Abstract
This study directly compares total intrafascial laparoscopic (TAIL™) hysterectomy with vaginal (VH) and abdominal (AH) hysterectomy with regard to safety, operating time and time of convalescence. The study is a prospective cohort study (Canadian Task Force classification II-2), including data from patients of a single university-affiliated teaching institution, admitted between 1997 and 2008 for hysterectomy due to benign uterus pathology. Patient data were collected pre-, intra- and postoperatively and complications documented using a standardised data sheet of a Swiss obstetric and gynaecological study group (Arbeitsgemeinschaft Schweizerische Frauenkliniken, Amlikon/Switzerland). Classification of complications (major complications and minor complications) for all three operation techniques, evaluation of surgeons and comparison of operation times and days of hospitalisation were analysed. 3066 patients were included in this study. 993 patients underwent AH, 642 VH and 1,431 total intrafascial hysterectomy. No statistically significant difference for the operation times comparing the three groups can be demonstrated. The mean hospital stay in the TAIL™ hysterectomy, VH and AH groups is 5.8 ± 2.4, 8.8 ± 4.0 and 10.4 ± 3.9 days, respectively. The postoperative minor complications including infection rates are low in the TAIL™ hysterectomy group (3.8%) when compared with either the AH group (15.3%) or the VH group (11.2%), respectively. The total of minor complications is statistically significant lower for TAIL™ hysterectomy as for AH (O.R. 4.52, CI 3.25–6.31) or VH (O.R. 3.16, CI 2.16–4.62). Major haemorrhage with consecutive reoperation is observed statistically significantly more frequent in the AH group when compared to the TAIL™ hysterectomy group, with an O.R. of 6.13 (CI 3.05–12.62). Overall, major intra- and postoperative complications occur significant more frequently in the AH group (8.6%) when compared to the VH group (3%) and the TAIL™ hysterectomy group (1.8%). The incidence of major complications applying the standardised TAIL™ hysterectomy technique is not related to the experience of the surgeons. We conclude that a standardised intrafascial technique of total laparoscopic (TAIL™) hysterectomy using an anatomically developed special uterine device is associated with a very low incidence of minor and major intra- and postoperative complications. The direct comparison of complication rates with either vaginal or abdominal hysterectomy favours the total laparoscopic technique, and therefore, this technique can be recommended as a relatively atraumatic procedure. The operation times are comparable for all three techniques without any statistically significant differences. This technique for laparoscopic hysterectomy is shown to be equally safe when applied by experienced gynaecologic surgeons or by residents in training.
Electronic supplementary material
The online version of this article (doi:10.1007/s10397-010-0569-0) contains supplementary material, which is available to authorized users.
Keywords: Total intrafascial laparoscopic hysterectomy, TAIL™ hysterectomy, Vaginal hysterectomy, Abdominal hysterectomy, Uterine device, Postoperative complications
A recent Cochrane review of 27 randomised controlled trials with 3,643 patients [1] comparing different techniques of hysterectomy in benign gynaecologic disease has shown that patients undergoing laparoscopically assisted vaginal hysterectomy (LAVH) or total laparoscopic hysterectomy (LH) have significantly lower mean blood loss (smaller drop in haemoglobin), significantly less infections and a faster return to normal activities when compared to laparotomy. On the other hand, abdominal hysterectomy (AH) requires a significantly lower operating time, and the frequency of urinary tract injuries is significantly increased for LH or LAVH [1]. The laparoscopic technique had no advantage over vaginal hysterectomy (VH) since in all but two studies LAVH was performed. In this situation, the most important steps of the operation are identical with VH.
The importance of more frequent urinary tract injuries, especially ureteral lesions, when applying the LH or the LAVH technique is supported by a non-randomised but large published database [2]. It is therefore possible that fear of consecutive complications and technical difficulties are the reasons for the fact that the vast majority of hysterectomies of benign uterus disease are today still performed as abdominal laparotomies [3–6]. In contrast, recent published data of a series of 3,190 LH for benign uterus disease by Donnez et al. [7] clearly demonstrated that this technique is a safe alternative with no increase in major complications when applied by experienced surgeons. LH also was shown to be associated with less tissue trauma [8], less postoperative pain [9], lower morbidity and less stress response when compared to AH [10].
In 1992, we started the development of a device and a surgical technique with the aim to improve safety and to simplify total LH [11]. The instrument described is reusable. It has been developed further and is manufactured today by Storz AG, Tuttlingen/Germany. Preliminary experience with this instrument has been reported by different authors [12–14].
The study presented evaluates safety and feasibility of a standardised surgical technique for total intrafascial laparoscopic (TAIL™) hysterectomy using the developed surgical device. We compare data of TAIL™ hysterectomy with AH and VH in a large group of patients (3,066 patients) from one single teaching institution.
Material and methods
Patients
All patients admitted between 1997 and 2008 for hysterectomy with or without adnexectomy due to benign uterine disease were included in this prospective, cohort study. Patient data were collected prospectively pre-, intra- and postoperative. Complications were documented using a standardised data sheet of a Swiss obstetric and gynaecological study group (Arbeitsgemeinschaft Schweizerische Frauenkliniken, Amlikon/Switzerland) [15]. Inclusion and exclusion criteria as well as the outcome were defined. For the analysis, patient identification was removed.
The quality of the data recorded was ensured by a two-step control system. First, the completeness and exactness of all data were verified at our centre by a data controller and double checked by a senior gynaecologist. Then, the data were sent to the central registry of the Swiss study group, and there, the accuracy of all data entered in the database was assessed again by the data centre quality control group. In case of discrepancy, data were returned for verification and correction. Information on patient characteristics, surgical procedures, intra- and postoperative complications was documented in the database.
The choice of the operative procedure (AH, VH or TAIL™ hysterectomy) was based on patient preferences after a thorough discussion of risks and benefits. Complications were classified as previously reported [16] with some minor modifications.
Major complications were classified as follows:
Major haemorrhage: requiring transfusion or reoperation
Bowel, ureteric or bladder injury
Deep venous thrombosis and pulmonary embolus (diagnosed by ultrasound, angiography, perfusion/ventilation scintigraphy or CT scan)
Reoperation for postoperative bleeding or unintended laparotomy
Minor complications were defined as:
Infections (pelvic infection or fever >38°C, two consecutive days)
Abdominal or vaginal bleeding or haematoma not requiring reoperation
Ileus
Wound dehiscence
Significant bacteruria
The study was approved by the ethical committee of the Institutional Review Board, Kantonsspital Baden, Switzerland.
Surgical technique
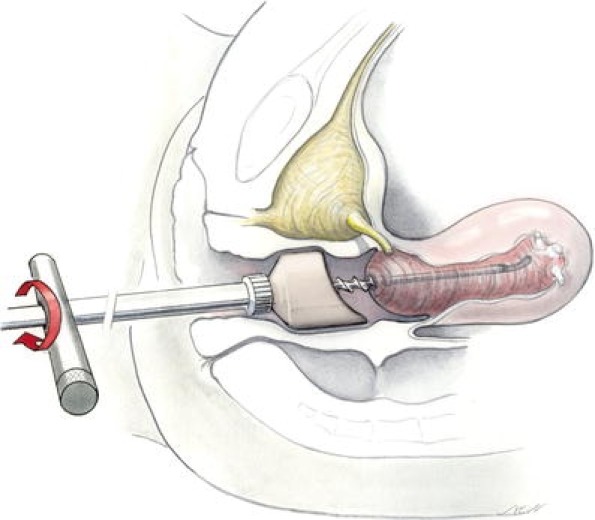
All vaginal and abdominal hysterectomies were performed with a standard surgical technique [17]. Patients in the LH group were operated by application of a step-by-step standardised operation technique, the so-called total atraumatic intrafascial laparoscopic hysterectomy (TAIL™ hysterectomy). A totally reusable instrument (Hohl Manipulator, Storz AG, Tuttlingen/Germany) with an anatomical design as a uterine device was used in all patients being operated by the LH technique. The instrument consists of a strong handle, manipulator rod, cervical cup platform in three different sizes for small, medium and large cervices, spiral threads in two sizes for a tight and secure endocervical fixation of the instrument and Hegar-type rod extensions for small and large uteri (Fig. 1 and Video 1). Tight endocervical fixation of the thread allows moving even a large uterus in all directions and applying strong tension to the tissue.
Fig. 1.

Uterine manipulator with cup, thread, extension, rod and handle
The cervical cup withstands electric and sonar energy and delineates exactly the border between the vagina and cervix. It serves as a surgical platform. Crucial surgical steps, e.g. bicoagulation of uterine vessels and intrafascial detachment of ligaments and vagina, are all performed in direct contact with the fringe of the cup (Video 2). These cups have a special design to adapt to the anatomy of the anterior and posterior vaginal fornices (Fig. 1).
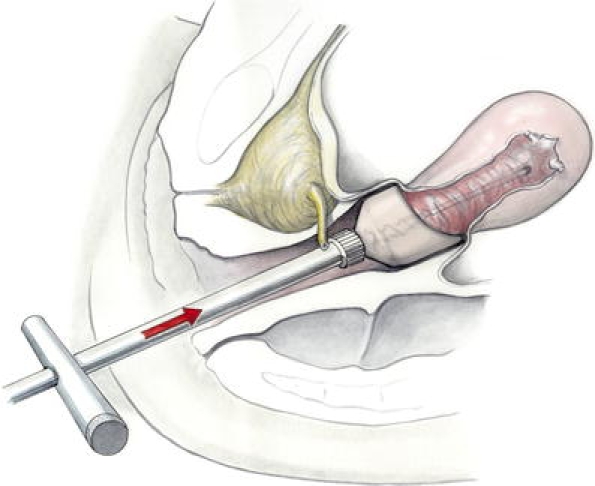
The patient is positioned in laparoscopic dorsal lithotomy position. Buttocks have to be positioned on the lower edge of the operation table to allow free manipulation with the instrument in all directions. The patient’s position is maintained by the use of shoulder supports and in recent years by special retraining mattresses on the operation table. Cranial sliding even in deep Trendelenburg position is thus mostly prevented. A tenaculum is placed on the anterior lip of the cervix and the cervix is dilated to Hegar 6. The length of the uterus cavity is measured. The size of the spiral thread is chosen according to the dimensions of the cervical canal (wide or narrow) and Hegar-type rod extensions according to uterine cavity length. Then, spiral threads are very tightly screwed into the endocervix to move even large uteri in all directions and apply strong tension to the tissues. The manipulator handpiece with an attached cup is gently introduced into the vagina with light rotating movements (Fig. 2). It has to be ensured that the extended side of the manipulator cup is located dorsally. Only after the manipulator handpiece has been advanced cranially as far as possible it is screwed to the manipulator probe. As a result, the edge of the manipulator cup is exactly located at the boundary of the cervix and the vagina (Video 1).
Fig. 2.
Application of the uterine device
A 10-mm port is placed in the umbilicus or even cranial to the umbilicus in cases of very large uteri. Three secondary 5-mm (two on the left side and one on the right side) ports are positioned very laterally for the application of surgical instruments. A 30° optical system is used for navigation in cases with large uteri. Using this optical system, better access to the ligaments is achieved. Bipolar or vapor pulse coagulation (VPC-Gyrus PlasmaKinetic®) applied with a grasping forceps with an integrated scalpel or bipolar and monopolar forceps or hooks are used for the dissection of the tissues.
-
Step 1.
The uterine device is pushed strongly to the contralateral side to create maximal tension. The left utero ovarian ligament, fallopian tube and the round ligament are grasped stepwise for dissection.
-
Step 2.
The anterior leaf of the peritoneum is incised and dissected stepwise in the direction of the cervix. The vesicovaginal peritoneum is opened and dissected. If there was no previous caesarean section, the dissection of the bladder from the cervix is obviated by strong pressure on the uterine instrument to push the uterus into the cranial direction (Fig. 3).
-
Step 3.
Steps 1 and 2 are performed on the right side in analogy to the left side.
-
Step 4.
With large uteri, access to the ligaments and posterior fornix is often blocked. Therefore, we approach the uterine arteries anteriorly. The manipulator cup is rotated to the contralateral side of the uterine artery (e.g. to the right side when the left uterine artery is dissected) which is then grasped whilst the back of the electric instrument touches the fringe of the cup (in safe distance from ureter and bladder, Fig. 4). Dissection of the uterine artery can therefore be performed safely even in difficult anatomical situations, e.g. frozen pelvis or advanced endometriosis. In this way, blood circulation to the uterus is completely stopped.
-
Step 5.
Thus, large uteri with blocked access to the lateral and posterior ligaments may then be reduced in volume without any further blood loss using an electrical morcellator before cervical detachment. Vaginal manipulation of the uterus in all directions greatly facilitates morcellation (sometimes pulling the uterus towards the vagina).
-
Step 6.
The fringe of the cup used serves as a platform to navigate around the cervix. If there are adhesions of the rectum cranial to the vaginal line of incision, they must be lysed first. This is facilitated by stretching tissues by applying strong pressure on the cup of the device.
-
Step 7.
Cardinal and sacrouterine ligaments are stretched to a maximum applying strong cranial pressure. The extraserosal pelvic fascia can be dissected at the level of the paracervix [18], keeping the “fascial ring” completely intact (Fig. 5). The vagina is dissected following exactly the fringe of the cup using monopolar blended current applied by scissors or a hook. The pneumoperitoneum is still maintained through maximal pressure on the vaginal walls by the device. After complete detachment of the uterus, it is partially removed from the vagina but left in the vaginal canal to maintain the pneumoperitoneum until laparoscopic suturing is accomplished.
-
Step 8.
Usually three to four Z-sutures, using 1–0 polydiaxonon (PDS, Ethicon), incorporating cardinal and sacrouterine ligaments as well as posterior and anterior endopelvic fascia are needed to close the vagina. The sutures are knotted extracorporally (Fig. 6). A “face-to-face” closure of the fascial plane is strived for. With our technique, we remove the uterus intrafascially, but during closure, a shortening of the ligaments can be achieved if the tissue is very lax by placing extra sutures on the sacrouterine ligaments and vagina. Bipolar coagulation should be avoided whenever possible. The peritoneum remains open. Hemostasis is checked and a copious lavage using warm ringer lactate is done.
Fig. 3.
Strong cranial pressure to the uterine device obviates the need for bladder dissection
Fig. 4.

Anterior approach to the uterine arteries. The back of the bicoagulation instrument touches the fringe of the cup
Fig. 5.
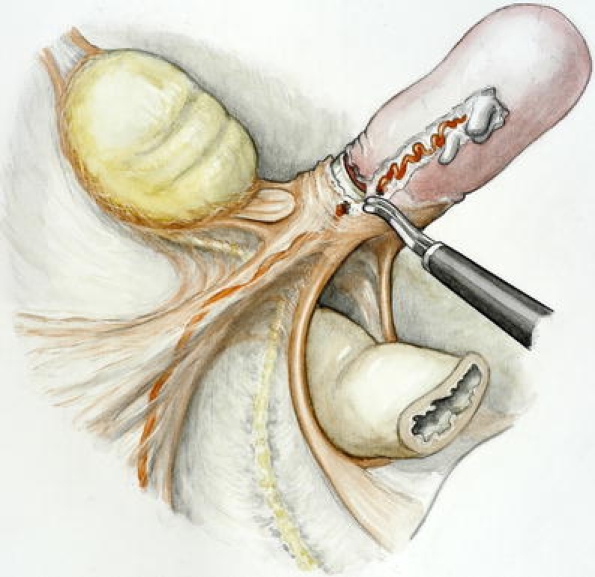
Intrafascial detachment of the uterus from ligaments and the vagina
Fig. 6.
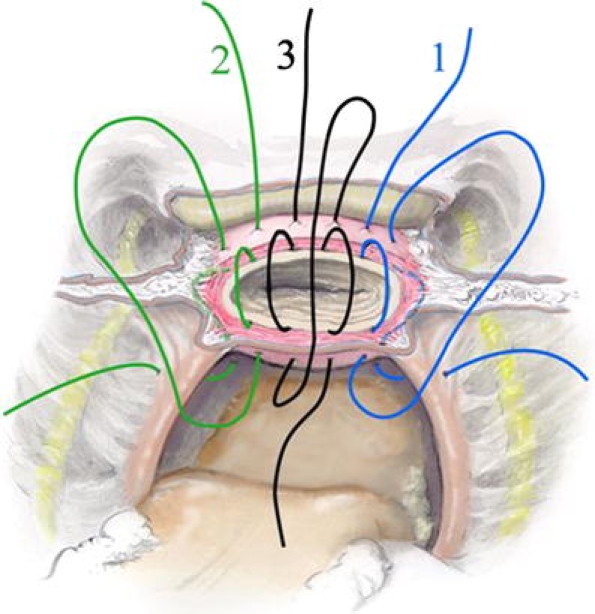
Closure of the vagina and reconstruction of the fascia by face-to-face closure
The stepwise operation procedure is documented by Video 1 and Video 2 added to this publication.
Statistical analysis
Data were evaluated for normal distribution by Kolmogorov–Smirnov test, and non-parametric tests were applied if required. Statistical significance level was placed at 0.025 by the Bonferroni correction for comparison of groups. Statistical evaluations were obtained by SPSS 10.0.7 Chicago Illinois, Medcalc 9.3.0.0 Belgium or Statcalc 5.0.
Results
A total of 3,066 patients fulfilled the inclusion criteria and could be included in this study. 993 of the total number of patients underwent AH, 642 VH and 1,431 TAIL™ hysterectomy. Table 1 shows the characteristics of the patients, including age, body mass index, operation times and duration of hospital stays. Mean age shows a difference between the groups. The women in the TAIL™ hysterectomy group are statistically significantly older when compared to the AH and VH groups. Mean body mass index also differs between the three groups. It is significantly lower in the TAIL™ hysterectomy group compared to the VH and AH groups. There is no statistically significant difference for the operation times comparing the three groups. The mean hospital stay in the TAIL™ hysterectomy, VH and AH groups is 5.8 ± 2.4, 8.8 ± 4.0 and 10.4 ± 3.9 days, respectively. Statistically significant differences are demonstrated.
Table 1.
Demographic and operative characteristics
| TAIL™ hysterectomy | AH (n = 642) | VH (n = 642) | Comparison | |||
|---|---|---|---|---|---|---|
| TAIL™-AH | Tail™-VH | AH-VH | ||||
| Age (years) | 56.4 ± 14.5 | 50.0 ± 11.1 | 46.9 ± 8.9 | p < 0.01 | p < 0.01 | p < 0.01 |
| Body mass index | 24.9 ± 2.8 | 26.7 ± 3.5 | 27.1 ± 2.9 | p < 0.01 | p < 0.01 | n.s. |
| Operation time (min) | ||||||
| 0–30 | 12 (0.8%) | 5 (0.5%) | 16 (2.5%) | n.s. | n.s. | n.s. |
| 31–60 | 272 (19%) | 165 (17%) | 167 (26%) | n.s. | n.s. | n.s. |
| 61–120 | 739 (52%) | 481 (48%) | 322 (50%) | n.s. | n.s. | n.s. |
| 121–180 | 333 (22%) | 264 (26.5%) | 112 (17%) | n.s. | n.s. | n.s. |
| >180 | 75 (5.2%) | 78 (8%) | 25 (3.9%) | n.s. | n.s. | n.s. |
| Hospital stay (days) | 5.8 ± 2.4 | 10.4 ± 3.9 | 8.8 ± 4.0 | p < 0.025 | p < 0.025 | p < 0.01 |
Data are reported as mean ± SD or number (%)
n.s.: p > 0.025
Table 2 shows the symptoms and diagnoses for the three groups of patients. Dysfunctional uterine bleeding, cervical intraepithelial neoplasia and genital prolapse are more frequent in the VH group as compared to the TAIL™ hysterectomy group, whereas the frequency of the diagnosis of postmenopausal bleeding, uterus myomatosus, benign adnexal tumours and endometrioses is higher in the TAIL™ hysterectomy group than in the VH group.
Table 2.
Symptoms and diagnoses
| TAIL (n = 1,431) | AH (n = 993) | VH (n = 642) | |
|---|---|---|---|
| Dysfunctional uterine bleeding | 655 (45.7%) | 412 (41.5%) | 349 (54.4%) |
| Postmenopausal bleeding | 109 (7.6%) | 69 (7%) | 31 (4.8%) |
| Cervical intraepithelial neoplasie | 65 (4.5%) | 32 (3.2%) | 64 (10%) |
| Adenomyosis | 221 (15.4%) | 141 (14.2%) | 82 (12.7%) |
| Uterus myomatosus | 758 (52.9%) | 506 (51%) | 240 (37.4%) |
| Benign adnexal tumours | 131 (9.2%) | 107 (10.8%) | 9 (1.4%) |
| Genital prolapse | 156 (10.9%) | 145 (14.6%) | 120 (18.7%) |
| Incontinence | 115 (8%) | 60 (6%) | 52 (8.1%) |
| Endometriosis | 122 (8.5%) | 88 (8.9%) | 10 (1.5%) |
| Dysmenorrhea | 241 (16.8%) | 70 (7%) | 128 (19.9%) |
| Dyspareunia | 62 (4.3%) | 47 (4.7%) | 30 (4.7%) |
| Abdominal pain | 25 (1.7%) | 21 (2.1%) | 11 (1.7%) |
| Miscellaneous | 45 (3.1%) | 29 (2.9%) | 21 (3.3%) |
Patients may have multiple symptoms and/or diagnoses
Major complications are shown in Table 3. Major haemorrhage with consecutive reoperation is observed to be statistically significantly more frequent in the AH group when compared to the TAIL™ hysterectomy group, with an O.R. of 6.13 (CI 3.05–12.62). An analogous observation is described when the AH group is compared to the VH group (O.R. 3.0, CI 1.45–6.39). For thromboembolic complications, a statistically significant difference is found: The AH group shows a statistically significantly higher incidence when compared to the TAIL™ hysterectomy group, with an O.R. of 16.0 (CI 2.06–124). The total rate of reoperations needed is significantly increased in the AH group when compared to the TAIL™ hysterectomy group (O.R. 4.47, CI 2.35–8.63), and also the AH group compared to the VH group shows a statistically significant difference (O.R. 2.42, CI 1.1–5.34).
Table 3.
Major complications
| TAIL™ hysterectomy | AH | VH | AH vs TAIL™ | VH vs TAIL™ | AH vs VH | |
|---|---|---|---|---|---|---|
| 1432 patients | 993 patients | 642 patients | O.R. ± 95% CI | O.R. ± 95% CI | O.R. ± 95% CI | |
| Major haemorrhage (reoperations) | 11 | 45 | 10 | 6.13 (3.05–12.62) | n.s. | 3.0 (1.45–6.39) |
| Bowel injury | 2 | 4 | 1 | n.s. | n.s. | n.s. |
| Ureteric injury | 1 | 3 | 0 | n.s. | n.s. | n.s. |
| Bladder injury | 8 | 8 | 5 | n.s. | n.s. | n.s. |
| Thromboembolic complications | 1 | 11 | 1 | 16.0 (2.06–124) | n.s. | n.s. |
| Reoperations | 3 | 14 | 2 | 4.47 (2.353–8.63) | n.s. | 2.42 (1.1–5.34) |
| Total of complications | 26 (1.8%) | 85 (8.6%) | 19 (3%) | 5.06 (3.17–8.12) | n.s. | 3.07 (1.8–5.3) |
| At least one major complication | 22 (1.5%) | 72 (7.3%) | 17 (2.7%) | 5.01 (3.02–8.38) | n.s. | 2.87 (1.63–5.11) |
Values are numbers (percentage) of patients
A patient may have more than one complication
Overall, major intra- and postoperative complications occur significantly more frequently in the AH group (8.6%) when compared to the VH group (3%) and the TAIL™ hysterectomy group (1.8%). No statistically significant difference is shown for the comparison of the VH group with the TAIL™ hysterectomy group. The odds ratios and confidence intervals for major complications are 5.06 (CI 3.17–8.12) for AH compared to TAIL™ hysterectomy and 3.07 (CI 1.8–5.3) for AH compared to VH, respectively.
Table 4 demonstrates minor complications observed for the three groups, including comparisons of the groups. The postoperative minor complications including infection rates (pelvic infections, fever and significant bacteruria) are low in the TAIL™ hysterectomy group (3.8%) when compared with either the AH group (15.3%) or the VH group (11.2%), respectively. The total of minor complications is statistically significantly lower for TAIL™ hysterectomy as for AH (O.R. 4.52, CI 3.25–6.31) or VH (O.R. 3.16, CI 2.16–4.62).
Table 4.
Minor complications
| TAIL™ hysterectomy | AH | VH | AH vs TAIL™ | VH vs TAIL™ | AH vs VH | |
|---|---|---|---|---|---|---|
| 1431 patients | 993 patients | 642 patients | O.R. ± 95% CI | O.R. ± 95% CI | O.R. ± 95% CI | |
| Infection | 14 | 42 | 15 | 4.47 (2.35–8.63) | 2.42 (1.10–5.34) | n.s. |
| Ileus | 1 | 3 | 1 | n.s. | n.s. | n.s. |
| Wound dehiscence | 1 | 2 | 1 | n.s. | n.s. | n.s. |
| Hematoma, bleeding (not requiring reoperation) | 6 | 7 | 9 | n.s. | 3.38 (1.16–9.53) | n.s. |
| Significant bacteruria | 33 | 98 | 46 | 4.64 (3.05–7.09) | 3.27 (2.02–5.59) | n.s. |
| Total | 55 (3.8%) | 152 (15.3%) | 72 (11.2%) | 4.52 (3.25–6.31) | 3.16 (2.16–4.62) | 1.43 (1.05–1.95) |
| At least one minor complication | 49 (3.4%) | 125 (12.6%) | 63 (9.8%) | 4.06 (2.95–5.8) | 3.07 (2.05–4.69) | n.s. |
| Total of major and minor complications | 81 (5.7%) | 237 (23.9%) | 91 (14.2%) | 5.22 (3.97–6.89) | 2.75 (1.98–3.82) | 1.90 (1.49–2.5) |
Values are numbers (percentage) of patients
Overall, the incidence of major and minor complications is lowest in the TAIL™ hysterectomy group compared to either AH or VH, respectively. The odds ratios and CI are 5.22 (3.97–6.89) for AH compared to TAIL™ hysterectomy, 2.75 (1.98–3.82) for VH compared to TAIL™ hysterectomy and 1.90 (1.49–2.50) for AH compared to VH.
The incidence of major complications applying the standardised TAIL™ hysterectomy technique is not related to the experience of the surgeons. No differences are found among residents in training and experienced staff surgeons for major complications. These data are summarised in Table 5.
Table 5.
Experience of surgeons and incidence of major complications with TAIL™ hysterectomy
| Major complications | Residents in training (620 patients) |
Staff surgeons (821 patients) | Statistic level |
|---|---|---|---|
| Major haemorrhage | 6 | 5 | n.s. |
| Bowel injury | 0 | 2 | n.s. |
| Ureter injury | 0 | 1 | n.s. |
| Bladder injury | 5 | 3 | n.s. |
| Thromboembolic complications | 1 | 0 | n.s. |
| Reoperations | 0 | 3 | n.s. |
| Total | 12 (1.9 ) | 14 (1.7%) | n.s. |
n.s.: p > 0.05
Discussion
The presented data are one of the largest prospective observational studies from a single institution. We describe and compare different techniques for total hysterectomy in benign uterus disease. Although there are statistically significant differences in age and body mass index, we feel that these are not in favour of total atraumatic intrafascial laparoscopic (TAIL™) hysterectomy since patients in this group are older. We demonstrate operation times not to vary statistically significantly for the three groups analysed. This observation is not in accordance with earlier published data of other authors [1]. If the standardised surgical technique for LH, as we describe it in this publication, is applied strictly, the operating procedure is straightforward and operation times are less as described for, e.g. LAVH procedures. Therefore, total laparoscopic hysterectomy does not consume longer operation times than either AH or VH, respectively. As it has been shown in earlier publications, LH is associated with less tissue trauma [8], less postoperative pain [9], lower morbidity and less stress response when compared to AH [10]. This leads to a better acceptance of the procedure and an improvement of quality of life.
Symptoms and diagnoses with regard to dysfunctional uterine bleeding, cervical intraepithelial neoplasia, genital prolapse, postmenopausal bleeding, uterus myomatosus, benign adnexal tumours and endometrioses are not equally balanced for the LH and the VH groups. This is in accordance with the published data by David-Montefiore et.al. [19] and also reflects that in the first years of this study, LH was not yet propagated and accepted as a standard of care for the symptoms and diagnoses mentioned.
Optimising health economics by the development of safe and time-saving operation techniques with reduced time of convalescence and hospital treatment days, we present the method of total relatively atraumatic intrafascial laparoscopic (TAIL™) hysterectomy. As a result of this study, we demonstrate that the operation time is equivalent when compared to AH and VH techniques. The mean hospital treatment days are reduced from 9 to 10 days below 6 days. As published evidence shows [1], reduced postoperative time of convalescence and earlier return to work and social life can be expected. The same is true for the quality of life of patients [20]. Therefore, shorter hospitalisation time, earlier convalescence, less lost work days and earlier return to social life achieved by the use of this operation technique support health economic aspects.
The main outcome results concerning intra- and postoperative complications are at variance with other published reports. The most dreaded complication—the risk of ureteric lesions—has repeatedly been shown to be increased applying the laparoscopic hysterectomy technique as compared to abdominal procedures [1, 2, 16, 21]. In contrast, we demonstrate that the laparoscopic approach is associated with a very low incidence of these complications discussed. We describe the development and consequent application of a uterine device designed to facilitate the single operation steps increasing especially the safety of the operation technique. The following step-by-step operation protocol as described here is essential to achieve the results presented for fast operation times with low incidences of complications. Every potential “dangerous” step of the operation procedure, e.g. the dissection of the uterine vessels, is performed in direct contact with the surgical platform. The device is designed to remove the bladder and ureter far away from the dissection plane. Our LH method is an intrafascial technique. This is also essential to increase the safety of the operation. Intrafascial detachment of the cervix decreases the risk for ureteral and/or bladder injuries even under difficult conditions, e.g. large uteri or the situation of a frozen pelvis. As described, there is no need for dissection of the bladder from the vagina; this is another advantage using this technique. In our study population, eight bladder lesions (0.6%) occurred in patients with scarring of the lower uterine segment after caesarean section. This is in accordance with published data for AH and VH and does, also in our study population, not show any statistically significant difference when compared to the AH and VH groups. Our results are also supported by the recent published data of a large series of LH demonstrating no association with an increase of major complication rates [7].
The analysed major complications include bleeding, defined as the need of reoperation and the requirement of blood transfusions. In our population, this complication is documented significantly more frequently for AH than for TAIL™ hysterectomy (OR 6.13 (CI 3.05–12.62). This observation can be explained by the anatomic dissection and the relatively atraumatic technique of the TAIL™ hysterectomy.
In contrast to Garry et al. [16] who found no significant differences for the postoperative minor complications including infection rates. In our study, these are significantly lower in the LH group (3.8%) as either in the AH (15.3%) or VH (11.2%) group. These data demonstrate that our LH technique is applicable and safe if the developed uterine device is applied correctly and used as a surgical platform and if the operation is followed step-by-step consequently as described. The face-to-face sutured endopelvic fascia at the vaginal level might help prevent postoperative ascending infections. Also, this tight approximation of fascial tissue might promote fibroblast proliferation and help in sealing the wound and probably prevents postoperative ascending infections. The short operation times and the avoidance of extensive coagulation seem to be important too.
With the technique of intrafascial dissection of the cervix, most parts of the cardinal and sacrouterine ligaments remain attached. The vaginal closure by the use of laparoscopic sutures unifies the ligaments, and during closure, a shortening of the ligaments can be achieved, if the tissue is very lax, by placing extra sutures on the sacrouterine ligaments and vagina. This operation step might contribute to a reduction of the indecency of post-hysterectomy vaginal vault prolapse. This hypothesis, however, needs to be confirmed by a long follow-up.
In summary, we observe, in contrast to others, a statistically significantly lower incidence of complications in the TAIL™ hysterectomy group when compared to either vaginal or abdominal procedures. We acknowledge that our results might be biased by the fact that our data represent a prospective observational study and not a randomised trial. However, the clinical importance of our findings is underlined by the large number of patients. In addition, our data are supported by the results of Donnez et al. [7] demonstrating no increased major complication rate for LH in a similar huge patient population as presented in our study. All our patient data were collected in a single institution, including staff surgeons and residents in training as gynaecologic surgeons. The analysis of the data presented shows no difference in the incidence of complications comparing residents in training as surgeons with experienced gynaecologic surgeons. This again is in contrast to the experience of other authors [22–24]. We postulate that the consequent following of the step-by-step operation procedure is crucial to guarantee a long-term high quality of outcome. The strict application of the standardised technique is a prerequisite for effective teaching and learning of this surgical technique.
The presented data will encourage and serve as a strong argument for better acceptance of the total laparoscopic hysterectomy technique among gynaecologists as discussed earlier in the literature [5]. Therefore, they serve as a fundament and raise the potential of this technique to popularise the minimal invasive approach. Thus, patients with benign uterus disorders may benefit from the proven advantages, e.g. less perioperative blood loss, reduction of postoperative pain, lower incidence of postoperative infections and shorter convalescence, respectively, without undergoing an increased risk for perioperative complications.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(MPG 6872 kb)
(WMV 103313 kb)
Acknowledgement
The authors acknowledge the work of Marc van den Bergh who did the statistical analysis of all data.
Conflict of interest
There have been no financial interest/arrangements with one or more organisations that could be perceived as a real or apparent conflict of interest in the context of the subject of this article.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, Garry R (2006) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev CP003677 [DOI] [PubMed]
- 2.Mäkinen J, Johansson J, Tomàs C. Morbidity of 10110 hysterectomies by type of approach. Hum Reprod. 2001;16:1473–1478. doi: 10.1093/humrep/16.7.1473. [DOI] [PubMed] [Google Scholar]
- 3.Reich H, Roberts L. Laparoscopic hysterectomy in current gynecological practice. Rev Gynaecol Pract. 2003;3:32–40. [Google Scholar]
- 4.Farquhar CM, Steiner CA. Hysterectomy rates in the United States 1990–1997. Obstet Gynecol. 2002;99:299–234. doi: 10.1016/S0029-7844(01)01723-9. [DOI] [PubMed] [Google Scholar]
- 5.Englund M, Robson S. Why has the acceptance of laparoscopic hysterectomy been slow? Results of an anonymous survey of Australian gynecologists. J Minim Invasiv Gynecol. 2007;14:724–728. doi: 10.1016/j.jmig.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Whiteman MK, Hillis SD, Jannieson DJ. In patient hysterectomy surveillance in the United States 2000–2004. Am J Obstet Gynecol. 2008;198:34–36. doi: 10.1016/j.ajog.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 7.Donnez O, Jadoul P, Squifflet J, Donnez J. A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: evaluation of complications compared with vaginal and abdominal procedures. BJOG. 2009;116:492–500. doi: 10.1111/j.1471-0528.2008.01966.x. [DOI] [PubMed] [Google Scholar]
- 8.Härkki-Sirén P, Sjöberg J, Toivonen J, Tiitinen A. Clinical outcome and tissue trauma after laparoscopic and abdominal hysterectomy: a randomized controlled study. Acta Onstet Gynecol Scand. 2000;79:866–871. [PubMed] [Google Scholar]
- 9.Roushdy M, Farag O, Mosaad M, Zayed M. Pain after hysterectomy: a comparison between four currently available procedures. Gynaecological Endoscopy. 1997;6:99–103. doi: 10.1046/j.1365-2508.1996.700493.x. [DOI] [Google Scholar]
- 10.Mo Yuen P, Mak T, Yim SF, Ngan Kee W, Lam C, Rogers M, Chang A. Metabolic and inflammatory responses after laparoscopic and abdominal hysterectomy. Am J Obstet Gynecol. 1998;179:1–5. doi: 10.1016/S0002-9378(98)70243-1. [DOI] [PubMed] [Google Scholar]
- 11.Hohl MK. Uterus manipulator für die intrafasziale laparoskopische hysterektomie. Frauenheilkunde aktuell. 1994;4:30–31. [Google Scholar]
- 12.Hohl MK, Häberle M (1998) The “Baden-manipulator” for bloodless total laparoscopic hysterectomy. 7th Congress of the European Society of Gynaecological endoscopy (abstract)
- 13.Müller A, Oppelt P, Ackermann S. The Hohl instrument for optimizing total laparoscopic hysterectomy procedures. J Minim Invasive Gynecol. 2005;12:432–435. doi: 10.1016/j.jmig.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Thiel F. Establishment of total laparoscopic hysterectomy (TLH) in a University Gynecology Department: results of the first 100 operations. Geburtsh Frauenheilkunde. 2006;66:665–669. doi: 10.1055/s-2006-924304. [DOI] [Google Scholar]
- 15.Huber AW, Mueller MD, Ghezzi F. Tubal sterilization: complications of laparoscopy and minilaparotomy. Eur J Obstet Gynecol Reprod Biol. 2006;134:105–109. doi: 10.1016/j.ejogrb.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 16.Garry R, Fountain J, Mason S. The eVALuate Study: Two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy. Br Med J. 2004;328:129–137. doi: 10.1136/bmj.37984.623889.F6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hirsch HA, Käser O, Iklé FA (1995) Atlas der Gynäkologischen Operationen. Thieme pp 121–130, 240–252
- 18.Eccoli A, Delmas V, Fanfani R. Terminologia Anatomica versus unofficial descriptions and nomenclature of the fasciae and ligaments of the female pelvis: a dissection based comparative study. Am J Obstet Gynecol. 2005;193:1565–1573. doi: 10.1016/j.ajog.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 19.David-Montefiore E, Rouzier R, Chapron C, Darai E. Surgical routes and complications of hysterectomy for benign disorders: a prospective observational study in French university hospitals. Hum Reprod. 2006;22:260–265. doi: 10.1093/humrep/del336. [DOI] [PubMed] [Google Scholar]
- 20.Kluivers KB, Johnson NP, Chien P. Comparison of laparoscopic and abdominal hysterectomy in terms of quality of life. A systematic review. Eur J Obstet Gynecol Reprod Biol. 2008;136:3–8. doi: 10.1016/j.ejogrb.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 21.McPherson K, Metcalfe MA, Herbert A. Severe complications of hysterectomy: the VALUE Study. BJOG. 2004;111:688–694. doi: 10.1111/j.1471-0528.2004.00174.x. [DOI] [PubMed] [Google Scholar]
- 22.Wattiez A, Joriano D, Cohen SB. The learning curve of total laparoscopic hysterectomy: comparative analysis of 1947 cases. J Am Assoc Gynecol Laparosc. 2002;9:339–345. doi: 10.1016/S1074-3804(05)60414-8. [DOI] [PubMed] [Google Scholar]
- 23.Altgassen C, Michels W, Schneider A. Learning laparoscopic-assisted hysterectomy. Obstet Gynecol. 2004;104:308–313. doi: 10.1097/01.AOG.0000132806.46344.05. [DOI] [PubMed] [Google Scholar]
- 24.Leminen A. Comparison between personal learning curves for abdominal and laparoscopic hysterectomy. Acta Obstet Gynecol Scand. 2000;79:1100–1104. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(MPG 6872 kb)
(WMV 103313 kb)


