Abstract
Introduction
Integrated care solutions need supportive financial incentives. In this paper, we describe the financial architecture and operative details of the integrated pilot Gesundes Kinzigtal.
Description of integrated care case
Located in Southwest Germany, Gesundes Kinzigtal is one of the few population-based integrated care approaches in Germany, organising care across all health service sectors and indications. The system serving around half of the population of the region is run by a regional health management company (Gesundes Kinzigtal GmbH) in cooperation with the physicians' network in the region (MQNK), a German health care management company with a background in medical sociology and health economics (OptiMedis AG) and with two statutory health insurers (among them is the biggest health insurer in Southwest Germany: AOK Baden-Württemberg).
Discussion and (preliminary) conclusion
The shared savings contract between Gesundes Kinzigtal GmbH and the two health insurers, providing financial incentives for managers and health care providers to realize a substantial efficiency gain, could be an appropriate contractual base of Gesundes Kinzigtal's population health gain approach. This approach is based on the assumption that a more effective trans-sector organization of Germany's health care system and increased investments in well-designed preventive programmes will lead to a reduction in morbidity, and in particular to a reduced incidence and prevalence of chronic diseases. This, in turn, is to lead to a comparative reduction in health care cost. Although the comparative cost in the Kinzigtal region has been reduced from the onset of Gesundes Kinzigtal Integrated Care, only future research will have to demonstrate whether—and to what extent—cost reduction may be attributed to a real population health gain.
Keywords: German managed care approach, population-based integrated care, health care management company, shared health gain
Background: cost and quality problems of a fragmented health care system and the concept of an integrated care solution in the Kinzigtal region
A key feature of the German health service system is its institutional fragmentation: public health services, primary and secondary ambulatory care (outpatient care), and hospital (inpatient) care are organized and financed largely independently from each other. The separation between office-based (ambulatory) and hospital-based (inpatient) physicians is stricter than in other countries, and only recent changes in German health care legislation have moderated this somewhat by allowing for example day-surgery in hospitals or a limited amount of ambulatory-based pre- and post-inpatient care [1]. This historically strict division of health services is connected to a reimbursement system without incentives for outcome-oriented health care or prevention so that quality- and value-based incentives have been virtually non-existent [1].
The shortcomings of such a fragmentation into health care sectors have often been noticed. Probably, the most obvious are problems of an insufficient follow-up care after patients' discharge from hospitals or rehabilitation clinics: very often, medication is diverging prior, during, and post hospitalization, which not only irritates the patients but is also a notorious ‘bone of contention between hospitals and primary care providers’ [1, p. 3]. As a rule, it takes more than two weeks for German primary care physicians to ‘receive a full report from a hospital once their patient has been discharged’ (ibid.). Insufficient communication of providers is however a problem which is not restricted to one sector or to inter-sector communication only. Insufficient communication leads many providers to perform redundant services and, therefore, to unnecessary cost. For the concerned patients, these redundant services imply not only a waste of time but also—at least in some cases, such as X-raying—unnecessary risks. The idea of implementing mutually compatible electronic means of communication and data processing for cooperating providers has remained a utopia for German normal care, with 68% of primary care physicians working in solo practice and another 31% in small group practice [1]. The same holds for the idea of creating a system of electronic patient files accessible to all providers treating a given patient (patients' informed consent provided). Sometimes the shortcomings of a fragmented health care system are exacerbated by specific reimbursement schemes, leading to blatant inefficiency. For example in a fee-for-service system it makes an economic sense for a provider to render as many services as possible by himself—regardless whether other providers are possibly better qualified or may render a given service at a much lower cost. On the other hand, in a reimbursement system with budgets it may be economically sensible for a provider to transfer services to another sector despite a considerably higher overall cost. To cite a prime example: quite often, a patient is hospitalized on Friday regardless of the fact that an intensive ambulatory care over the weekend would have rendered the necessary services, too—and at a much lower cost [2, p. 154]. One of the most severe problems of most current health service systems is that there are no effective incentives for health promotion and prevention: health care providers are rewarded for their efforts in treating diseases but not for preventing them successfully. In general, many current health service systems lack an effective system of incentives that would lead providers to consider a kind of ‘systemic’ or ‘macro-rationality’ in their actions.
Considering such inefficiencies, health care legislation in Germany initiated some innovations from 2000 and—with growing intensity—from 2004, implying more favourable conditions for integrated care solutions [1]. According to the Statutory Health Insurance Modernization Act (‘GKV-Modernisierungsgesetz’, abbreviation GMG) [3] adopted in 2004, Germany's health insurance companies were allowed to spend 1% of their total expenditure on integrated care programmes. This act was in effect from 2004 to 2008. Contrary to the expectations of responsible health politicians, however, the overwhelming majority of integrated care projects which have come into being since 2004 have focused only on a few specific indications (e.g. hip or knee surgery) and have usually integrated two sectors (e.g. inpatient care and rehabilitation) and occasionally three sectors (e.g. inpatient care, rehabilitation, and pre- and post-surgery ambulatory care). Only a tiny minority of integrated care contracts attempted to realize a population-based integrated care system, covering all sectors and indications of care for a given population. One of the few population-based integrated care systems is located in the Kinzig valley in the Southwest of Germany; it is called ‘Integrierte Versorgung Gesundes Kinzigtal’ (‘Healthy Kinzigtal Integrated Care’). Gesundes Kinzigtal Integrated Care is coordinated and managed by Gesundes Kinzigtal GmbH (‘Healthy Kinzigtal Ltd.’), a regional integrated care management company. The company was founded in September 2005 by two organizations: the local physicians' network MQNK (‘Medizinisches Qualitätsnetz—Ärzteinitiative Kinzigtal e.V.’) and OptiMedis AG, a German health care management company with a background in medical sociology and integrated care management. MQNK provides medical expertise and its members, being familiar with the region and its people, are aware of the strengths and shortcomings of the region's health care system. OptiMedis AG brings into this partnership prevention and health economic as well as management know-how and the ability to provide monetary investment. Some 66.6% of Gesundes Kinzigtal GmbH's shares are owned by MQNK members; thus it is ensured that the interests of local physicians remain dominant. The remaining shares are held by OptiMedis AG. According to its mission statement, Gesundes Kinzigtal GmbH aims to establish a more efficient and better-organized health care for the residents of the Kinzigtal area “in cooperation with patients, health professionals and health insurers”. At the same time, Gesundes Kinzigtal Integrated Care aims to provide state-of-the-art, i.e. best-practice health care to all its patients [4].
In the following section, we first outline the contract concluded by Gesundes Kinzigtal GmbH and the concerning health insurers as well as its implications on providers' incentives (Sections A–B). Afterwards, we present some operative aspects of Gesundes Kinzigtal Integrated Care in greater detail (Sections C–E).
The strategy of Gesundes Kinzigtal Integrated Care: improving population health by a shared health gain approach
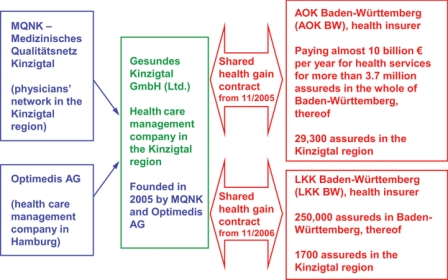
The total population within the western and central Kinzigtal region—the service area of the Gesundes Kinzigtal integrated care system—amount to about 60,000 inhabitants. Slightly more than half of these (31,000) are insured by AOK Baden-Württemberg (about 29,300 assureds) and by LKK Baden-Württemberg (about 1700 assureds). Both are statutory health insurers (sickness funds); AOK BW is open to anyone whereas LKK BW is open only to farmers and their dependents. Gesundes Kinzigtal GmbH is in charge of the health care budget of these 31,000 assureds (see Figure 1).
Figure 1.
Corporate structure of the Kinzigtal shared health gain contract.
One of the reasons why many well-meant reform attempts and integrated care initiatives of the past have not prevailed is—in our opinion—that its initiators refrained from proving the economic sustainability of their projects. The founders of Gesundes Kinzigtal Integrated Care seem to have learnt this lesson: the shared health gain approach and the corresponding shared savings contract of Gesundes Kinzigtal Integrated Care should be considered an answer to this shortcoming of past integrated care initiatives. Accordingly, it is crucial for our argument in total that we first explicate the economic and contractual foundations of Gesundes Kinzigtal's integrated care (Sections A and B).
Section A: Realizing a shared health gain approach by means of a shared savings contract: an outline of the principle
The initiators of Gesundes Kinzigtal Integrated Care are confident that enhancing patients' self-management capabilities in combination with intensifying health promotion and preventive programmes will lead—at least in the mid- and long-term—to an improved population health in comparison with normal care, i.e. to a lower incidence and prevalence of diseases. In economic respects, this health gain should result in considerable comparative savings in relation to normal care. Furthermore, the founders of Gesundes Kinzigtal GmbH are convinced that there are lots of potential sources of efficiency gains that will pay off even in the short-term: thus, e.g. a more economic pharmacotherapy might be realized within a comparably short-time period without sacrificing service quality—e.g. by avoiding me-too-products, concentrating on generic drugs, and buying from fewer drug manufacturers so as to realize increased discounts. The real challenge is to create a sufficiently accurate system of incentives that motivate providers and managers to bring in their knowledge and to act accordingly. Without appropriate incentives, individual providers will certainly not invest their time and money, e.g. in effective preventive services and a better coordination of care if the resulting comparative savings pay off exclusively in the cash balance of others, regardless if this is a health insurer or a management company. Still in 2005, the biggest statutory health insurer in Southwest Germany, AOK Baden-Württemberg, quickly took the courage to make considerable investments in providing the necessary resources and prerequisites of such an innovative project which claimed to reward the population's health gain. In this process of establishing the new integrated care system, AOK Baden-Württemberg benefited from their former experience with other physicians' networks and their experience with management tools for integrated care solutions—particularly as regards data management, data exchange, and data protection. Shortly after, in late 2006, LKK Baden-Württemberg joined the contract. The contract between Gesundes Kinzigtal GmbH and the two statutory health insurers was termed until the end of 2014 (and will—if it is not explicitly cancelled in 2014—be continued beyond that year) so as to reward even those improvements in population health which will pay off in the long-term only. To explain how this contract rewards a population health gain, we will explicate the essential details of this contract in the following paragraphs.
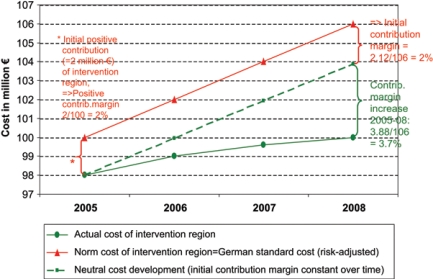
According to the contract, the financial result of Gesundes Kinzigtal GmbH is calculated within the framework of a health insurer's contribution and profitability analysis: the financial result achieved by Gesundes Kinzigtal GmbH equals the change in the Kinzigtal region's contribution margin, with the change being measured in relation to the region's contribution margin before the intervention started. By relying on fictitious figures, Figure 2 illustrates a model case which conforms to Gesundes Kinzigtal's ‘philosophy’, i.e. to the assumption that an investment in health promotion and preventive programmes will pay off in the mid- and long-term, and that a better coordination of health services and a more rational pharmacotherapy will pay off even in the short-term, thus compensating for initial investment cost. As a result, the actual cost of the fictitious intervention region illustrated in Figure 2 increase at a lower rate that its norm cost, resulting in an increasing contribution margin in the subsequent years 2006–2008.
Figure 2.
Calculation model of an integrated care management company's financial results within the framework of a health insurers' contribution margin analysis—model case I: increasing contribution margin after the start of the intervention in 2006 (figures are fictitious—for demonstrational purpose only).
Explication of Figure 2: In general, the contribution margin of a given region (precisely speaking: of the assureds living in the region) equals the difference between its norm cost and its actual cost. If we assume that the norm cost1 of a given region—as illustrated in Figure 2—amount to 100 million € per year and its actual cost to only 98 million, a positive contribution volume of 2 million € results. This corresponds to a positive contribution margin of 2 million €/100 million €=2% (in 2005). If we assume in model case I (see Figure 1) that an integrated care project starts in this region by January 1, 2006, the financial results of the project in subsequent years (in Figure 1: 2006, 2007, 2008) equal the change in contribution margin, measured in relation to the time before the project started. In our model case, we have illustrated an increasing contribution margin in 2006–2008. For 2008, e.g. the increase in contribution margin amounts to 3.7%. This is because in 2008 the norm cost of the intervention region amount to 106 million € and its actual cost to 100 million €, resulting in an overall contribution margin of 6 million €/106 million €=5.7%. In relation to the contribution margin before the start of the project (2% in 2005), the increase in contribution margin which may be attributed to the integrated care project amounts to 5.7%–2%=3.7%.
An explication of the term ‘norm cost’ may be useful here because it sheds more light on the management company's strategy of action. The German norm cost of an assured with given risk characteristics (age, sex, income, reduction in earning capacity2) equals the cost of the German (risk-adjusted) standard. Standard costs, i.e. norm costs are calculated in Germany by the Federal Insurance Agency (‘Bundesversicherungsamt’) within the context of managing the German risk structure compensation system (‘Risikostrukturausgleich’) [5]. This has an important implication for Gesundes Kinzigtal GmbH's action strategy: as the norm cost of the Kinzigtal assureds are ‘given’ by the German standard, i.e. cannot be influenced by Gesundes Kinzigtal GmbH, the management company's strategy must consist in reducing the Kinzigtal assureds' comparative actual cost in order to realize its financial goal. To cite a typical situation: the management company realizes its financial goal if, e.g. the actual cost of the Kinzigtal assureds increase at a lower rate as compared with their German standard (such a case has been illustrated in Figure 2). Hence the ‘shared health gain’ approach of Gesundes Kinzigtal GmbH and the contracting health insurers is based on a shared-savings contract.
Section B: A shared health gain approach in action: factual details of the shared savings contract between Gesundes Kinzigtal GmbH and health insurers AOK BW and LKK BW
After having outlined in Section A how to calculate an integrated care company's financial result within a health insurer's profitability analysis in principle (and by relying on fictitious figures—as in Figure 2), we shall now proceed to reporting the actual details of the contract between Gesundes Kinzigtal GmbH and the concerned health insurers.
The change in contribution margin—the indicator of financial success—is determined in relation to the Kinzigtal region's contribution margin in the reference period 2003–2005 with an above-average emphasis on the year 2004 because it is the last entire year without any intervention by Gesundes Kinzigtal GmbH.
Actually, the Kinzigtal region's contribution margin during the reference period 2003–2005—with an above-average weight of 2004—amounted to 1.56%; this figure serves then as a starting point against which the subsequent change in contribution margin will be measured. Thus, e.g. a hypothetical overall contribution margin of the Kinzigtal region of, say, 4.0% in 2008 implies that the change in contribution margin which may be attributed to Gesundes Kinzigtal GmbH's activities amounts to 4.0%–1.56%=2.44.
Up until June 30, 2007, Gesundes Kinzigtal GmbH benefited from the start-up funding according to the above-mentioned Statutory Health Insurance Modernization Act (see section Background). From July 2007, however, the management company derives its income exclusively from increasing the contribution margin of the Kinzigtal assureds, i.e. from realizing comparative savings.
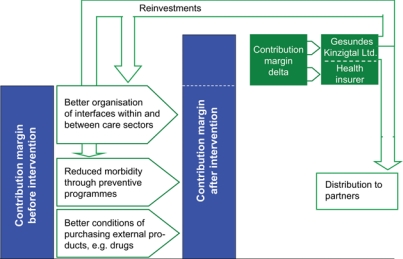
An increase in contribution margin—relative to the starting point of 1.56%—in subsequent years means a profit for the concerned health insurer, with the profit being attributed to Gesundes Kinzigtal GmbH's activities. This profit will be distributed between Gesundes Kinzigtal GmbH and the concerned health insurer according to an agreement made beforehand. As a for-profit company, Gesundes Kinzigtal GmbH may reinvest its profit into more preventive programmes and/or health promotion facilities or distribute a part of the profit to its shareholders (see Figure 3).
A decrease in the Kinzigtal region's contribution margin (relative to the starting point of 1.56%) means a loss for the integrated care intervention for which the concerned health insurer is liable. Such a loss means that Gesundes Kinzigtal GmbH obtains no returns on its investment. At the same time a loss opens up an exit option for the contracting health insurers.
The contracting health insurers may pursue an exit option in some other cases, too, which they deem to harm their interests. This applies when, e.g. Gesundes Kinzigtal GmbH may succeed in making a profit, but only by lowering the quality of its health care or by making an extraordinary number of assureds to contract out.
Figure 3.
Financial architecture of the Kinzigtal shared health gain contract.
Summarizing the preceding paragraphs (Sections A and B), Gesundes Kinzigtal GmbH's financial goal consists—by contract—in increasing the contracting health insurers' contribution margin within the Kinzigtal region. To increase the health insurers' contribution margin implies to realize comparative savings within the Kinzigtal region which are to be achieved in relation to German standard cost and to the reference period 2003–2005. Therefore, the contract between the management company and health insurers AOK BW and LKK BW may be conceived in its economic essence a shared-savings contract. This contract provides the incentives that are necessary to make health care providers and managers get involved in creating more effective and more efficient health services. Thus, the shared-savings contract may be considered an appropriate contractual base of Gesundes Kinzigtal's ambition to realize a substantial population health gain compared with normal care. This argument rests however on the assumption that an improved population health will result in comparative savings—an assumption which is at the core of Gesundes Kinzigtal GmbH's business philosophy and which will be tested in the course of a comprehensive evaluation performed by independent research institutions (see section Evaluation).
Section C: Key characteristics and prerequisites of Gesundes Kinzigtal's preventive and care management programmes
In view of Gesundes Kinzigtal's basic assumption regarding the prominent role of a population health gain, it is logical that at the core of the company's interventions are several preventive and health promotion programmes. Before describing the substance of these programmes in greater detail (see Section D), we will characterize some of their process and performance characteristics which seem to be equally important.
Individual treatment plans and goal-setting agreements between doctor and patient: whenever an enrolled patient has been identified of being at risk for a certain disease—e.g. in the course of a comprehensive health check-up which is routinely performed after a patient's enrolment—doctor and patient are to develop an individual treatment plan and agree upon mutual treatment goals. Gesundes Kinzigtal GmbH supports the physicians with case management know-how, offers financial incentives to them (see below) and provides additional services for the patients such as, e.g. patient education programmes.
Patient self-management and shared decision-making: until now, social institutions supporting patients' self-help and self-management activities are not yet well developed in the rural Kinzigtal area. By supporting self-help initiatives and by affording training programmes in shared decision-making to doctors, Gesundes Kinzigtal GmbH attempts to support patients' active participation on the micro level. Correspondingly, on an institutional level (macro level) a patient ombudsman and a patient advisory board have been established so as to ensure that patients' perspectives are carefully considered before important decisions are taken by the management company. The initiators of Gesundes Kinzigtal are convinced that patients' self-management capabilities and their active participation in treatment decision are an important prerequisite for patients to become ‘co-producers’ of their health, and thus for sustained gains in overall population health.
Follow-up care and case management: as explicated in the first section (Background), the lack of coordination of follow-up care after patients' discharge from hospital or rehabilitation is one of the most obvious shortcomings of Germany's health care system. By facilitating the cooperation of hospitals with other providers—e.g. by jointly developed care pathways, synchronizing medications and electronic patient records across the sectors of care (see below)—Gesundes Kinzigtal aims to create the preconditions for a better-coordinated follow-up. Relying on these newly institutionalized means, the patient's ‘doctor of trust’ (any physician or psychotherapist contracting with Gesundes Kinzigtal may be chosen by an enrolled patient as his/her ‘doctor of trust’) and his/her assistant take charge of a seamless follow-up care. By increasing the quality of follow-up care, unnecessary—and costly—readmissions shall be prevented.
Right care at the right time: when structural service bottlenecks have been identified—e.g. in some parts of the Kinzigtal region waiting periods of several months for an appointment with a psychotherapist are common—Gesundes Kinzigtal aims to provide tailored solutions. Thus, e.g. when psychotherapeutic services might seem to be urgent, Gesundes Kinzigtal offers the possibility of immediate short interventions by psychotherapists and psychiatrists so as to provide the required care in time. In return for holding these emergency services in readiness, providers receive an extra fee by the management company.
System-wide electronic patient record: partner providers of Gesundes Kinzigtal Integrated Care may have access to electronic patient records. This information is stored in a highly encrypted manner and is then delivered to each provider whom a key card had been offered by the patient. Thus the patient is the owner of his data and has the exclusive right of disposal. Provided that patients consent a provider's access, the provider will have access to all relevant diagnoses and treatment information. This implies a swift and accurate data communication between providers which is an important precondition for increasing the quality of care by, e.g. reducing medication interactions and avoiding costly—and sometimes risky—redundant services.
The specific care and preventive programmes that have been developed and implemented so far will be characterized briefly in the following paragraphs (Section D).
Section D: A brief description of Gesundes Kinzigtal's care management and preventive programmes
All specific care and preventive programmes shall be performed in compliance with the above-mentioned key characteristics. The primary goal of these programmes is to improve patients' overall health status and increase their quality of life. To achieve maximum effectiveness, Gesundes Kinzigtal's care and preventive programmes target common chronic diseases with high impact on patients' health status and against which effective interventions are available. For patients who have been identified in the initial health check-up of being at risk for certain diseases, Gesundes Kinzigtal offers programmes to prevent (or at least postpone the onset of) these diseases. For patients with chronic diseases—such as e.g. diabetes—programmes are offered to prevent (or postpone the onset of) long-term consequences of the disease, such as e.g. the occurrence of a diabetic foot. All these programmes are constantly checked and developed further after their implementation (according to the ‘plan-do-check-act’ scheme); moreover, further programmes concerning indications that have not yet been covered by the hitherto existing programmes will be developed. The following list contains a brief description of those programmes that have been implemented until May 2010.
Active health promotion for the elderly (‘Aktive Gesundheitsförderung im Alter’—Agilthe AGil programme consists of a half-day patient education for people from 60 years. Its focus is on health literacy with respect to nutrition, physical exercise and social participation. Furthermore, support in health-related decision-making is provided. The courses are to enhance patients' self-management capabilities and impart a basic knowledge on how to begin and stick to effective health behaviour. After the initial half-day course there is continuing support of participants by regular letters and refresher workshops. Until now (May 2010), 511 seniors have been trained. The outcome-evaluation of this programme is supported by the Federal Ministry of Education and Research.3
Two variants of an intervention programme for patients with chronic heart failure (‘Starkes Herz’)—both variants of the treatment programme rely on the same evidence-based treatment guidelines. The variants differ in how patients' supervision is organized: in variant (A) patients are supervised by phone calls; additionally, patients' health is controlled through telemonitoring performed by a professional telemonitoring service company. In variant (B) specialised teams, mainly consisting of doctor's assistants or practice nurses, are in charge of managing patients' health by regular personal contact (case management by house visits or phone calls).4
‘Healthy body weight’ (‚Gesundes Gewicht‘)—an intervention programme for patients with high blood sugar level, high body-mass index and lipid metabolic disorder (metabolic syndromethe programme combines lifestyle interventions as to nutrition and physical exercise with regular checks of patients' blood sugar level (to be performed either by physicians or by patients themselves).
An intervention programme for patients who are at risk of osteoporosis (‘Starke Muskeln, fest Knochen’)—the programme offers a screening test—occasionally including a state-of-the-art measurement of patients' bone density—to find out whether patients are at risk of osteoporosis. Patients at risk receive counselling sessions with respect to nutrition and preventive activities in general and vitamin D and medication depending on their risk score. Moreover, physiotherapists and specialised fitness trainers have developed a tailored physical exercise programme that may be performed by patients either in a physiotherapist's practice or in fitness studios and gym clubs. Depending upon their risk score these exercise programmes are paid by GK and are offered to enrolled patients of Gesundes Kinzigtal for free. Until now (May 2010), 455 patients have participated in this programme.
‘Smoke-free Kinzigtal’ (‘Rauchfreies Kinzigtal’) is a physician-conducted smoke cessation programme for people who are willing to quit smoking. Enrolled patients may choose one of four cessation programme variants: medical therapy (relying on new drugs supporting smoke cessation), acupuncture, hypnosis, and group behaviour therapy. Furthermore, Gesundes Kinzigtal supports enterprises in creating a smoke-free work environment and in encouraging employees to quit smoking by offering specific incentives (such as e.g. vouchers for wellness programmes).
A programme providing immediate short interventions by psychotherapists or psychiatrists in case of a personal crisis (‘Psychotherapie Akut’)—this programme offers immediate psychotherapeutic care with up to seven sessions to patients who have incurred an acute personal crisis, showing symptoms of e.g. depression, panic or anxiety disorders. As outlined above in section C (4), in normal care waiting periods of several months are common in rural areas, often leading to an—avoidable—exacerbation of disorders which does not only aggravate patients' sufferings but may also result in a costly hospitalization.
Social case management (‘Sozialer Dienst’)—patients with complex social problems or addictive disorders may be supported by social workers. These social workers work with AOK BW (that initiated this programme) and cooperate closely with the concerning ‘doctors of trust’ [see Section C (3)].
Strengthening medical care for the elderly in nursing homes (‘ÄrztePlusPflege’)—nursing homes inhabitants quite often experience the need for emergency care in the evenings or during the weekend, when their doctors are not on duty. Unfortunately, the physicians from the ambulance have no knowledge of the patient and his history; normally they have to take the elderly to the hospital. This programme developed joint guidelines for nurses and physicians, financed the mobile availability of primary care physicians beyond the office hours and helped nursing facilities to prevent fractures and infections.
These eight care management and preventive programmes have been developed by Gesundes Kinzigtal Integrated Care and its contracting partners. Furthermore, enrolled patients are encouraged by Gesundes Kinzigtal to participate in the nation-wide disease management programmes (DMPs) as to diabetes, coronary heart diseases, breast cancer, asthma, and COPD (see Table 1).
Table 1.
Care management and preventive programmes in Gesundes Kinzigtal Integrative Care
| Subject/name of the programme | Year of implementation | Number of patients enrolled in the programme (as of May 2010) |
|---|---|---|
| Chronic heart failure (‘Starkes Herz’) | 2006 | 67 |
| Lifestyle intervention for patients with metabolic syndrome (‘Gesundes Gewicht’) | 2007 | 122 |
| Smoking Cessation Programme (‘Smoke-free Kinzigtal’) | 2007 | 128 |
| Active health promotion for the elderly (‘AGil’) | 2007 | 511 |
| Intervention by psychotherapists/psychiatrists in case of acute personal crises (‘Psychotherapie akut’) | 2007 | 126 |
| Prevention of osteoporosis/osteoporotic fractures (‘Starke Muskeln, feste Knochen’) | 2008 | 455 |
| Social case management (‘sozialer Dienst’) | 2008 | 78 |
| DMP diabetes mellitus type II | 2006 | 830 |
| DMP coronary heart disease | 2007 | 288 |
| DMP breast cancer | 2006 | 18 |
| DMP asthma | 2008 | 100 |
| DMP COPD | 2008 | 154 |
| Patient university | 2007 | 1.070 |
| Medical care for the elderly in nursing homes (‘ÄrztePlusPflege’) | 2009 | 124 |
Besides these classical preventive and disease management programmes Gesundes Kinzigtal promotes some other programmes. Among these is, e.g. ‘Healthy Kinzigtal moving’ (‘Gesundes Kinzigtal bewegt’Gesundes Kinzigtal supports active membership in sports and gym clubs (including dance and glee clubs) by giving vouchers and membership discounts to patients. Furthermore, there are aqua-fitness courses for enrolled patients, programmes for health promotion at work, health promotion activities in collaboration with schools, programmes to improve medical services in nursing homes, and—last but not least—a ‘patient university’ consisting of regular health education and patient counselling presentations by medical experts. These ‘patient university’ classes are very popular: until now (May 2010), more than a 1000 people have taken part in classes and courses. The development of more preventive and care management programmes is underway concerning major depression, rheumatic disorders, hypertension, asthma in adolescents, and a generic programme to improve medication adherence of patients with chronic diseases (by distributing dose blisters prepared for a whole week).
Section E: Management tools
The information base for re-engineering health care provision by Gesundes Kinzigtal GmbH is health insurers' cost and utilisation data for the entire Kinzigtal population. By now a joint database has been computed (conforming to privacy legislation) which contains the contracting health insurers' data of their members:
basic claims data (age, sex, residence, periods of insurance),
data on diagnoses and services in ambulatory care,
data on prescriptions made by office-based physicians,
hospital data (admission/discharge diagnoses, further diagnoses, length of stay, OPS, DRG, etc.)
sick leave data,
data on therapeutic appliances, and
data on nursing care/long-term care.5
These data are used by the management company for planning its intervention programmes and for monitoring and improving the quality of services including health outcomes. In detail, the following techniques are applied:
predictive modelling and other data analysis techniques (such as regression and logistic regression) are used to identify groups of high-risk patients [10]. The results of these analyses allow for targeted early interventions;
disease costs are cluster-analysed and prioritized so as to design cost-effective intervention programmes using evidence-based intervention strategies;
regional variances of prevalence or utilization figures are analysed and discussed with the providers, and
providers get benchmark reports containing utilization and care history data of their patients.
Having outlined the relationship between Gesundes Kinzigtal GmbH and the contracting health insurers (Sections A–B) and the company's strategies to increase population health by various interventions and management techniques (Sections C–E), we shall now characterize the contractual relations and obligations between enrolled patients, individual health care providers, and Gesundes Kinzigtal GmbH.
Contractual relations and obligations between patients, health care providers, and the management company
The relationship between Gesundes Kinzigtal GmbH and individual providers
It is important to note that the normal reimbursement schemes and financial flows between statutory health insurers6 and individual physicians are not replaced by Gesundes Kinzigtal GmbH, i.e. the reimbursement schemes of normal care remain unchanged. These normal reimbursement payments, then, continue to be the bulk of individual providers' income. Only in addition to these payments, Gesundes Kinzigtal GmbH reimburses some special services not covered by the normal reimbursement schemes but deemed necessary to realize a higher quality of care.7 Currently, providers receive such additional payments by the management company for comprehensive check-ups of patients' health (routinely performed after patients have enrolled), calculation of patients' prognoses and development of individualized treatment plans including goal-setting agreements with patients, participation in project group meetings, development and implementation of preventive programmes (see Section D), and case management of patients with chronic diseases [usually performed by doctors' assistants—see Section D (2)]. Furthermore, Gesundes Kinzigtal GmbH bears providers' additional IT costs which result from establishing providers' prerequisites and equipment for data exchange and for (reading and writing) patients' electronic health records. All of the above-mentioned additional reimbursements and payments by the management company amount to about 10–15% of providers' other income.
As of May 2010, Gesundes Kinzigtal GmbH has concluded provider contracts with 52 physicians' practices (22 general practitioners, 5 paediatricians, 3 psychotherapists, 22 specialists), 6 hospitals, 3 pharmaceutical manufacturers, 9 nursing homes, 4 ambulatory home health agencies, 5 physiotherapists, 14 pharmacies, 22 health and sports clubs, and 6 gyms. Negotiations with additional providers are underway. The details of cooperation between an individual provider and Gesundes Kinzigtal GmbH are stated in the provider contract: therein providers agree, e.g. to adhere to consented guidelines, standards and procedures as well as to the charter of patients' rights within Gesundes Kinzigtal Integrated Care. Furthermore, the contract specifies for which extra services providers receive separate reimbursement payments by the management company.
To avoid an undue financial burden for the management company during the first years of the integrated care system—i.e. until the expected increase in population health begins to pay off—the company's shareholders [whose majority consists of individual physicians, see Section B (4)] have agreed that:
reimbursement levels for special services must not exceed the usual amount of fees for equivalent services; this means reimbursement levels should merely amount to expense allowances;
all providers should get an additional share in the company's profit depending on individual provider performance measured by appropriate quality indicators, referring to e.g. patients' health outcome or patient satisfaction;
the shareholders' share in the company's profit shall not be distributed to them until the fourth year of the integrated care project, i.e. until a sustainable profit is expected.8
The relationship between Gesundes Kinzigtal GmbH and enrolled patients
As mentioned above, Gesundes Kinzigtal GmbH is in charge of the health care budget for all 31,000 assureds of AOK BW and LKK BW in the Kinzigtal region. These 31,000 people are entitled to actively enrol as members of Gesundes Kinzigtal Integrated Care and thus benefit from special services and programmes which are reserved for enrolled assureds. Nonetheless, the non-enrolled, too, benefit from many of Gesundes Kinzigtal GmbH's activities, such as its efforts for a better care coordination in the region or a more rational pharmacotherapy. However, only the enrolled assureds are entitled to elect the members of the patients' advisory board—an institution which is to voice the interests of the patients in Gesundes Kinzigtal GmbH's decision-making process.
Until May 2010, 6870 assureds of AOK BW and LKK BW have enrolled,9 with an increasing speed of enrolment in 2008 and 2009. In 2008, the number of active integrated care members increased from 1998 (December 31, 2007) to 4402 (December 31, 2008), rising to 6335 at the end of 2009. Whereas thousands of assureds joined Gesundes Kinzigtal Integrated Care, only very few members withdrew from their membership: in 2009, only 0.8% withdrew all in all, with only 0.2% being ‘real’ withdrawals, whereas 0.4% moved out of the Kinzigtal region (and, consequently, withdrew from their integrated care membership) or withdrew from AOK BW membership altogether (and, consequently, had to withdraw from their integrated care membership, too—these amounted to 0.2%). Enrolment is strictly voluntary. There are no additional premiums or fees for the assureds to enrol, and enrolled assureds may contract out at the end of each calendar quarter. At the same time there are no immediate financial incentives for assureds to enrol. Thus, consumers' choice for or against enrolment relies on the expected health outcome and on service quality arguments and not on financial interest. This means that Gesundes Kinzigtal GmbH and the cooperating providers must convince the assureds to enrol by referring solely to the argument of a higher service quality and a comparative health gain to be expected by integrated care. The management company perceives such an unrestricted consumer choice as a valuable incentive for health care providers to improve their skill in convincing the patient by rational arguments instead of trying to ‘buy’ his/her compliance by relying on financial incentives. Patients' material service benefits, which are free of any additional charge, may be summarized as follows:
improved care coordination over all sectors of care,
a ‘doctor of trust’ (or doctor's assistants respectively) ready to conduct additional case management services,
care providers who have been trained in shared decision-making,
a more intensive patient–physician relationship through individual and mutually agreed-upon treatment plans,
additional health check-ups compared with normal care,
additional preventive programmes compared with normal care (see Section D)—and mostly for free,
access to consultations with physicians outside normal opening hours,
discounts for fitness classes and sports club membership fees,
immediate accessibility for providers to one's own electronic patient files containing all diagnoses, treatment and prescription records.
It is essential to note that a patients' free choice of health care providers remains unrestricted in Gesundes Kinzigtal's integrated care system: patients may seek care services from any legally accredited provider, regardless if this concerns hospitals, office-based specialists, general practitioners, or psycho- and physiotherapists, and regardless whether the concerning provider does or does not have a provider contract with Gesundes Kinzigtal GmbH. Nonetheless, the management company encourages enrolled patients to use the service of contracting partner providers; the final decision is however left to the patients. Thus, contrary to gate-keeping models which are en vogue in Germany at the moment, the Kinzigtal ‘doctor of trust’ is not in charge of keeping any gate closed or of benevolently opening this or that gate to a subjected patient. In Gesundes Kinzigtal's integrated care system, patients are treated as self-responsible co-producers of their own health who must be convinced by rational arguments—and not as ignorant consumers whose free choice must be bought out in order to realize goals set by external agents.
Evaluation of Gesundes Kinzigtal by independent institutions
In the history of Managed Care approaches it sometimes happened that positive financial results of Managed Care organizations were achieved not only by a more efficient trans-sector coordination of care but also by a policy risk selection. As been shown elsewhere, in the Kinzigtal integrated care case risk selection has successfully been prevented by a series of institutions and precautions that have been consciously implemented by the founders of Gesundes Kinzigtal Integrated Care [13]. Contrary to traditional risk selection, Gesundes Kinzigtal Integrated Care has enrolled first and foremost those assureds whose morbidity and whose cost is clearly above average (cf. ibid.). Gesundes Kinzigtal has, consequently, realised a kind of ‘inverted risk selection’ (cf. ibid.).
Another potential source of ‘positive’ financial results, such as e.g. an increased contribution margin would be—in theory—to postpone or withhold necessary services and therapies. In such a case comparative savings would be realised by under-use of medical and therapeutic services. To gain independent evidence on a potential under-use of services, Gesundes Kinzigtal GmbH and the two cooperating health insurers provided a remarkable budget for the evaluation of the system by independent research institutions. In 2006–2007, several independent evaluation projects have started, investigating different quality aspects of the Kinzigtal system. A key project in investigating a potential under-use of services is a study on ‘over-, under- and mis-use of health services’ (in short: OUM study). The OUM study conforms to the rules of a quasi-experimental, population-based controlled cohort trial. Its central question is whether certain diseases, selected health service utilization figures indicating service quality, as well as over-, under- and mis-use of services are (or become) comparatively less or more prevalent (resp. incident) in the intervention region (Kinzigtal region) compared with ‘normal care’. The OUM study relies on administrative data of the concerned statutory health insurers AOK BW and LKK BW: of all assureds living in the Kinzigtal region (n=31,000), a person-related (but pseudonymous) dataset was delivered to the research group, containing assureds':
basic claims data (age, sex, residence, periods of insurance),
data on diagnoses and services in ambulatory care,
data on prescriptions made by office-based physicians,
hospital data (admission/discharge diagnosis, further diagnoses, length of stay, OPS, DRG etc.),
sick leave data,
data on therapeutic appliances, and
data on nursing care, long-term care.
An analogous dataset has been made available by AOK BW and LKK BW for a large random sample of their assureds living outside the Kinzigtal region, i.e. in the rest of Baden-Württemberg. This latter sample, comprising the (pseudonymised) data of about 500,000 AOK BW and LKK BW members, serves as the control group. When incidence or prevalence figures are calculated, the control group's results will be standardised to the Kinzigtal group according to age and sex. In some other cases—e.g. when service quality indicators in both groups are compared (such as the prescription prevalence of, say, beta-blockers in CHD-patients)—a matched-pairs-technique will be applied so that every CHD patient in the intervention region will be compared with CHD patients in the control region (1:5 matching).
In both samples (intervention and control group) only those AOK BW or LKK BW assureds are considered who have been insured continuously in 2004–2006. New members who joined AOK BW or LKK BW after 2004 will be excluded from the OUM study. The assureds' data of the year 2004 are conceived as the baseline data as they reflect the state of affairs before the Kinzigtal integrated care intervention started; the years 2005–2011 are considered as follow-up years reflecting a gradually growing ‘dose’ of integrated care intervention by Gesundes Kinzigtal GmbH.
The OUM study seems to be appropriate to demonstrate how service quality develops in the Kinzigtal region over time in comparison with normal care. Furthermore, the OUM study delivers evidence whether Gesundes Kinzigtal succeeds in reducing the incidence and prevalence of diseases in the region compared with the remaining regions in Southwest Germany, i.e. whether Gesundes Kinzigtal delivers a comparative health gain in the region.
Discussion and preliminary conclusion
The regional management company Gesundes Kinzigtal GmbH and the statutory health insurers AOK BW and LKK BW have set up one of the first large-scale population-based integrated care systems in Germany. Without replacing the previous reimbursement schemes and financial flows between health insurers and individual health care providers, Gesundes Kinzigtal GmbH takes charge of the whole (i.e. trans-sector) health care service budget for all AOK BW and LKK BW assureds living in the Kinzigtal region. Cooperating closely with the two health insurers and the contracting health care providers (whose majority are at the same time shareholders of Gesundes Kinzigtal GmbH), the management company has implemented a series of preventive and care management programmes as well as other trans-sector measures to realize a substantial population health gain in the mid- and long-term (see Section C and D).
The expected health gain is to lead in turn to a substantial comparative reduction of health care cost in the Kinzigtal region (compared with the German standard). Some other measures such as, e.g. a more rational pharmacotherapy and a better trans-sector coordination of health care services are to lead to comparative efficiency gains even in the short-term, thus compensating for initial investment cost as to the above-mentioned care management and preventive programmes.
The shared savings contract between Gesundes Kinzigtal GmbH and the two health insurers, providing financial incentives for managers and health care providers to realize a substantial efficiency gain, could be an appropriate contractual base of Gesundes Kinzigtal's population health gain approach (see Section A and B). At the same time, the founders of Gesundes Kinzigtal Integrated Care seem to have taken effective precautions that managers' and providers' new interest in savings will not result in under-provisioning of services or risk selection [4, 13].
Indeed, the contract between Gesundes Kinzigtal GmbH and AOK BW as well as LKK BW seems to be an innovative and appropriate institution aligning—at least partially—the interests of health care providers and health insurers, thus providing the preconditions of a ‘value-based competition on results’ [14]. In German normal care with its fee-for-service system capped by budgets, financial interests of providers are as a rule opposed to the interests of health insurers: whereas providers strive in direction for higher reimbursement amounts for given services and for increasing the number of services performed by oneself (until the ceiling of one's budget is reached), the shared savings contract realized by Gesundes Kinzigtal GmbH brings in a completely new aspect that could work out in the reverse direction: the shared savings component creates an incentive for providers to realize increasing comparative savings in relation to the German standard, thus contributing to an (at least partial) harmonisation of their interests with those of the contracting health insurers. This harmonisation is however still ‘partial’ because the basic fee-for-service reimbursement system continues to be the main foundation of providers' income for the time being.
The first question that may be discussed controversially is: does the shared savings contract unfold sufficiently strong incentives so that health care providers get deeply involved in contributing to a more efficient regional health service system—despite the fact that the ‘old’ incentives, arising from a fee-for-service system capped by budgets, still exist? The answer of the promoters of Gesundes Kinzigtal Integrated Care could be two-fold: first, those health care providers who are members of the local physicians' network MQNK and who cooperate with Gesundes Kinzigtal GmbH, do not seem to act in a strictly utilitarian manner, which means they do not try to realize a maximum individual profit at every opportunity, regardless of the moral dimension of their action. Realistically, those health care providers—like many other groups of people—do not only strive for a high income but also for social approval and a good reputation10, even more so as a kind of ‘social control’ prevails among the partner providers of Gesundes Kinzigtal Integrated Care. (The number of office-based partner providers is still below 55 so that an effective social control is probably still at work [2, p. 158]). In short: because of the moral dimension of health care providers' self-esteem and because of the social control among Gesundes Kinzigtal's partner providers, even comparably small incentives may get health care providers involved in contributing their due share to more efficient health services in the region. The second answer is less theoretical and very simple: the first financial results of Gesundes Kinzigtal's integrated care system regarding the years 2006–2007 have invalidated the suspicion that the new incentives arising out of the shared savings contract might be too weak: already in 2007 Gesundes Kinzigtal GmbH has realized an increase in the overall region's contribution margin (as to AOK BW assureds) of 3.38%— which has surprised even the most optimistic promoters of integrated care [16].
As surprising as these first financial results might have been, it is not yet evident from which sources they have originated. It seems clear, however, that they do not have resulted primarily from a substantive population health gain limited to the enrolled assureds: by December 2007 only 1900 assureds had actively enrolled in Gesundes Kinzigtal Integrated Care, and still much fewer people had enrolled in the specific care management or preventive programmes described above in Section D. Rather, the comparative savings of 2006 and 2007 seem to have resulted from those actions of Gesundes Kinzigtal GmbH that are not limited to the enrolled patients but are focused on realizing efficiency gains in the short-term (see Section B) such as, e.g. a more rational pharmacotherapy or a more economic reorganization of trans-sector health services (including a lower hospitalisation ratio). Moreover, the introduction of goal setting techniques in treatments, the implementation of individual treatment plans for enrolled risk patients, and the additional health check-ups might have contributed to an enhanced ‘health mindfulness’ on the part of both physicians and patients which then again might have lead to lower costs.
Nonetheless, it still remains to be proven in detail whether the core of Gesundes Kinzigtal GmbH's philosophy is valid: that substantive comparative savings will be brought about by a substantial population health gain which may be realized by patients' enhanced self-management capabilities combined with intensified health promotion and prevention within an integrated care framework. In any case, the outlook for getting a comprehensive and reliable answer to this question seems to be very good: as outlined in the section Evaluation, Gesundes Kinzigtal and the contracting health insurers have provided a considerable budget for a comprehensive evaluation by independent research institutions, and several research projects focus on the issue of how service quality and health outcomes develop under conditions of Gesundes Kinzigtal Integrated Care in comparison with normal care.11
Until now we may conclude that Gesundes Kinzigtal Integrated Care seems to be a promising approach to realize the twofold goal of a substantial population health gain on the one hand and substantive comparative savings in relation to normal care on the other hand. Currently, some other (similar) integrated care projects are built up in several parts of Germany, and it will be exciting to watch whether they will be successful. In case of success these initiatives might develop into a role model for large parts of the German health service system. A detailed discussion of these other initiatives and a consideration of the newly unfolding discussion in the US on ‘Accountable Care Organizations’ [17] and the need for ‘integrators…an entity that accepts responsibility for all three components of the Triple Aim for a specified population’ [18] however have to be left to a future paper.
Footnotes
The calculation of ‘norm cost’ in Germany will be explicated shortly below.
From 1994 until 2008 these risk characteristics were the key variables for determining risk structure compensation payments of Germany's statutory health insurers. From 2002, the variable ‘participation in a national disease management programme (DMP)’ was added. From 2009, participation in a DMP was dropped again as a key variable. Simultaneously, new compensation regulations as to the morbidity risk structure of health insurers' members were introduced [5].
The evaluation is conducted by Prof. von dem Knesebeck (Institute of Medical Sociology, University Hospital Hamburg-Eppendorf, Hamburg University).
In their case management activities practice nurses or doctor's assistants rely on short standardized questionnaires developed in cooperation with the University of Heidelberg [6].
In the last years, a new branch of academic public health research has been developing which relies primarily on the investigation of health insurers' administrative data (as outlined above). For a detailed description of this health services utilization research [7–9].
In Germany, the reimbursement of providers' services by statutory health insurers is mediated by the association of statutory health insurance physicians (‘Kassenärztliche Vereinigung’). The main function of this intermediate organization consists in negotiating on reimbursement levels with health insurers and in distributing reimbursement payments to individual physicians [11, pages 40ff, 209ff; 12, 183ff].
Thus, even though the management company does not perform the bulk of reimbursement payments to individual providers, it virtually takes charge of the whole reimbursement budget for all services delivered to AOK BW and LKK BW assureds in the Kinzigtal region.
Luckily (from the management company's perspective), a considerable profit has been realized even during in the first years of the integrated care system's existence. See in greater detail the section Evaluation below.
Contrary to some Managed Care organizations in other countries, the founders of Gesundes Kinzigtal Integrated Care have consciously attempted to avoid incentives for risk selection towards the fit and healthy people (for more details see Hermann et al. 2006 [4, p. 5–7, 19–21] and Siegel et al. 2008 [13, p. 230–4]). Using the health insurers' contribution margin not for the enrolled but for all their assureds in the region as economic measure, Gesundes Kinzigtal GmbH must look for improving care especially for those who are in need and may have higher costs as it is the norm. Consequently, the mean age among the enrolled is considerably higher than among the non-enrolled, and the health insurers' per capita expenditure for an enrolled person exceeds their expenditure for a non-enrolled person by about 50% (more on this topic in greater detail: Siegel et al. 2008 [13, p. 230–4]). This testifies even to a kind of inverted risk selection by Gesundes Kinzigtal Integrated Care.
See in detail the subtle but striking critique of the utilitarian (i.e. strictly economist) conception of man shared by many economists, in Amitai Etzioni's ‘The moral dimension. Toward a new economics’ (1988) [15].
The evaluation is coordinated and supervised by the department of medical sociology at Freiburg University which periodically reports preliminary evaluation results in the (free-of-charge) EKIV Newsletter (http://www.ekiv.org/en/newsletter.php). From 2010, there will be also an abbreviated English version.
Contributor Information
Hildebrandt H., Hamburg, Germany and CEO of Gesundes Kinzigtal GmbH, Hauptstr. 7, 77716, Haslach, Germany.
Hermann C., Heilbronner Str. 184, 70191 Stuttgart, Germany.
Knittel R., Vogelrainstrasse 25, 70199 Stuttgart, Germany.
Richter-Reichhelm M., Borsteler Chaussee 53, D-22453 Hamburg, Germany.
Siegel A., Department of Medical Sociology, Hebelstr. 29. D-79104 Freiburg, Germany.
Witzenrath W., Appointed by the Physicians' Network MQNK (Medizinisches Qualitätsnetz—Ärzteinitiative Kinzigtal e.V.), Am Krähenäckerle 1, 77723 Gengenbach, Germany.
Reviewers
Volker Amelung, Univ.-Prof. Dr., Hannover Medical School, Institute for Epidemiology, Social Medicine and Health Systems Research, Hannover, Germany
Frances Cunningham, ScD., BA., Senior Research Fellow, Centre for Clinical Governance Research in Health, Australian Institute of Health Innovation, Faculty of Medicine, University of New South Wales, Sydney, Australia
Daniel K. Zismer, PhD., Associate Professor, Chair and Director, MHA and Health Administration Executive Studies Programs, School of Public Health, University of Minnesota, USA
References
- 1.Schlette S, Lisac M, Blum K. Integrated primary care in Germany: the road ahead. International Journal of Integrated Care [serial online] 2009 Apr 20;9 doi: 10.5334/ijic.311. Available from: http://www.ijic.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hildebrandt H, Richter-Reichhelm M, Trojan A, Glaeske G, Hesselmann H. Die Hohe Kunst der Anreize: Neue Vergütungsstrukturen im Deutschen Gesundheitswesen und der Bedarf für Systemlösungen. [The art of setting the right incentives: new reimbursement structures in German health care and the need for systemic solutions]. Sozialer Fortschritt. 2009;58(7):154–60. [in German] [Google Scholar]
- 3.Deutsche Bundestag. Gesetz zur Modernisierung der gesetzlichen Krankenversicherung (GKV-Modernisierungsgesetz-GMG) [Statutory Health Insurance Modernisation Act]. 2003. Available from: http://www.buzer.de/gesetz/7332/index.htm. [in German] [Google Scholar]
- 4.Hermann C, Hildebrandt H, Richter-Reichhelm M, Schwartz FW, Witzenrath W. Das Modell „Gesundes Kinzigtal“. Managementgesellschaft organisiert Integrierte Versorgung einer definierten Population auf Basis eines Einsparcontractings. [The „Gesundes Kinzigtal“ model: A management company organises a population-based integrated care system on the base of a shared-savings approach]. Gesundheits- und Sozialpolitik. 2006;(5–6):11–29. [in German] [Google Scholar]
- 5.Göpffarth D, Greß S, Jacobs W, Wasem J, editors. Jahrbuch Risikostrukturausgleich 2008. [Yearbook Risk Structure Compensation System 2008]. St. Augustin: Morbi-RSA; 2008. [Google Scholar]
- 6.Peters-Klimm F, Müller-Tasch T, Schellberg D, Gensichen J, Muth C, Herzog W, et al. Rationale, design and conduct of a randomised controlled trial evaluating a primary care-based complex intervention to improve the quality of life of heart failure patients: HICMan (Heidelberg Integrated Case Management) BMC Cardiovascular Disorders. 2007;7:25. doi: 10.1186/1471-2261-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schubert I, Köster I, Küpper-Nybelen J, Ihle P. Versorgungsforschung mit GKV-Routinedaten Nutzungsmöglichkeiten versichertenbezogener Krankenkassendaten für Fragestellungen der Versorgungsforschung. [Health services research on the base of health insurers' administrative data (claims dataHow to use health insurers' data for the purpose of health service research]. Gesundheitsblatt – Gesundheitsforschung – Gesundheitsschutz. 2008;51(10):1095–105. doi: 10.1007/s00103-008-0644-0. [in German] [DOI] [PubMed] [Google Scholar]
- 8.Ihle P, Köster I, Herholz H, Rambow-Bertram P, Schardt T, Schubert I. Versichertenstichprobe AOK Hessen/KV Hessen – Konzeption und Umsetzung einer personenbezogenen Datenbasis aus der Gesetzlichen Krankenversicherung. [How to create a sample of person-related but pseudonymised patient data from claims data of statutory health insurers and of the association of statutory health physicians]. Gesundheitswesen. 205;67:638–45. doi: 10.1055/s-2005-858598. [in German] [DOI] [PubMed] [Google Scholar]
- 9.Swart E, Ihle P, editors. Routinedaten im Gesundheitswesen. Handbuch Sekundäranalyse: Grundlagen, Methoden und Perspektiven. [Claims data in German health care: A handbook on the foundations of claims data-related health service research, its methods and perspectives]. Bern: Huber; 2005. [Google Scholar]
- 10.Schreyögg J, Plate A, Busse R. Identifizierung geeigneter Versichertengruppen für die integrierte Versorgung mit Hilfe von GKV-Routinedaten. [How to identify insured people as potential clients of integrated care providers with the aid of claims data]. Gesundheitsökonomie und Qualitätsmanagement. 2005;10:349–55. [in German] [Google Scholar]
- 11.Busse R, Riesberg A. Gesundheitssysteme im Wandel: Deutschland. [Changing health service systems: the case of Germany]. Copenhagen/Berlin: Medizinisch-Wissenschaftliche Verlagsgesellschaft; 2006. [in German] [Google Scholar]
- 12.Simon M. Das Gesundheitssystem in Deutschland. Eine Einführung in Struktur und Funktionsweise. [The health service system in Germany: An introduction to its structure and operation]. Bern: Huber; 2008. [in German] [Google Scholar]
- 13.Siegel A, Stößel U, Geßner D, Knittel R, Beckebans F, Hildebrandt H. Kooperation und Wettbewerb im integrierten Versorgungssystem „Gesundes Kinzigtal“. In: Amelung VE, Sydow J, Windeler A, et al., editors. Vernetzung im Gesundheitswesen. Wettbewerb und Kooperation. [Networking in health care: cooperation and competition]. Stuttgart: Kohlhammer; 2005. pp. 223–35. [in German] [Google Scholar]
- 14.Porter ME, Teisberg EO. Redefining health care: creating value-based competition on results. Boston: Harvard Business School Press; 2006. [Google Scholar]
- 15.Etzioni A. The moral dimension. Toward a new economics. New York: The Free Press; 1988. [Google Scholar]
- 16.Rabatta S. Integrierte Versorgung: Kooperation im Kinzigtal spart Kosten. [Integrated Care: cooperation in the Kinzig valley saves costs]. Deutsches Ärzteblatt. 2009;106(20) A-966/B-827/C-802. [in German] [Google Scholar]
- 17.Miller HD. How to create accountable care organizations. Pittsburgh: Center for Healthcare Quality and Payment Reform; 2009. Available from: http://www.CHQPR.org. [Google Scholar]
- 18.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Affairs. 2008 May-Jun;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]