Abstract
Background
The aim of this prospective randomized clinical trial was to investigate the efficacy of a home-based program of isometric strengthening exercises for the treatment of the lateral epicondylitis (LE) of the distal humerus. We hypothesized that 1) use of isometric strengthening exercises would result in clinical benefits similar to those provided by medication and pain relief and 2) functional improvements after exercise would be time-dependent.
Methods
Patients were assigned to one of two groups: 1) an immediate physical therapy group (group I), or 2) a delayed physical therapy group (group D). Group I patients (n = 16) were instructed how to do the exercises at their first clinic visit and immediately carried out the exercise program. Group D patients (n = 15) learned and did the exercises after being on medications for 4 weeks.
Results
Outcomes at the 1-month clinic visit indicated that pain (measured using a visual analogue scale [VAS]) had been significantly reduced in group I compared to group D (p < 0.01). However, significant differences between groups were not found at 3-, 6-, and 12-month follow-up for either VAS scores or Mayo elbow performance scores. For modified Nirschl/Pettrone scores, a significant difference between groups was found only at the 1-month follow-up visit. By then, the number of participants who returned to all activities with no pain or occasional mild pain was six (37%) in Group I and two (13%) in Group D (p = 0.031). At the final follow-up visit, 88% of all participants performed physical activities without pain.
Conclusions
Isometric strengthening exercises done early in the course of LE (within 4 weeks) provides a clinically significant improvement.
Keywords: Lateral humeral epicondylitis, Muscle strengthening exercises, Isometric, Home based
Lateral epicondylitis (LE), or tennis elbow, is a degenerative or failed-healing tendon disease characterized by immature reparative tissue that resembles angiofibroblastic hyperplasia in the origin of the extensor carpi radialis brevis (ECRB).1) Although a diagnosis of LE can be easily arrived at by clinical examination, treatment has been a challenging problem.2) Based on the natural history of LE, some investigators have advocated a wait and watch policy without any intervention for relief of symptoms. Smidt et al.3) reported that 80 percent of persons with LE of longer than 4 weeks' duration had recovered after 1 year of waiting. However, there is a consensus among experts that a year is too long a time for the patient to wait, not only in terms of pain and disability, but also in terms of loss of economic productivity.4) To date, more than 40 different therapeutic interventions including physiotherapy have been described in the literature.5) Among these treatment modalities, exercise programs, home-based or supervised, are one of the most commonly suggested physiotherapies. However, as stated by Stasinopoulos et al.,2) one disadvantage of a home exercise program is a lack of compliance with the regimen. Furthermore, compliance is often decreased when patients exercise with pain.6) Since most studies regarding exercise programs have dealt with the efficacy of concentric or eccentric exercises, these disadvantages may not be as relevant to isometric strengthening exercise programs.
Isometric strengthening exercise programs have not been investigated well. To the authors' knowledge, only one study has mentioned its possibility as a treatment modality for the LE.6) Accordingly, we developed a simple isometric strengthening exercise program, which can be easily performed without any equipment or strict supervision of a physiotherapist. The aim of our prospective randomized clinical trial was to investigate the efficacy of home-based isometric strengthening exercise by comparing two different treatment regimens: 1) participants start exercising immediately vs. 2) participants begin exercise after receiving medications for the initial 4 weeks. We hypothesized that 1) the participants doing an isometric strengthening exercise program would experience clinical outcomes similar to those with medication and pain relief and 2) functional improvements after exercise would be time-dependent.
METHODS
Design
We conducted a prospective randomized study. Physical examination was done by the senior author. Assignment to one of the two groups was done using a random number generating program by the two clinical fellows: 1) an immediate physical therapy group (group I), 2) a delayed physical therapy group (group D). The exercise protocol was the same in both groups. Patients who were assigned to group I were instructed as to how to perform the exercises at the very first visit and then immediately carried out the exercise program. Group D patients did the exercises after 4 weeks of oral non-steroidal anti-inflammatory drug medications. Participants who did not exhibit reduced symptoms after 4 weeks of doing the exercise program were withdrawn from the study and received other treatments such as extracorporal shock wave therapy (ESWT), or surgery after confirming the pathologic lesions of the elbow using ultrasonography.
Participants
Patients in our study were selected using the following criteria: 1) clinical diagnosis of LE - tenderness on or near the extensor carpi radialis brevis (ECRB) origin site, which is located 5 mm distal and anterior from the lateral epicondyle of the humerus, and aggravation of symptoms with resisted middle finger extension with the elbow in an extended position; 2) persistent symptoms for at least 6 weeks despite non-strengthening conservative treatments including medication, brace application, and physical therapy; 3) ability to complete questionnaires. Exclusion criteria were as follows: 1) steroid injections at the lateral epicondyle within the last 3 months; 2) combined diseases such as rheumatoid arthritis, neurologic or muscular disorders; 3) a history of previous injury of the elbow; 4) arthritic changes or calcifications around the elbow joint on radiographs. Between August 2005 and June 2006, 31 consecutive patients who had LE diagnosed by the senior author and met criteria were invited to participate. There were no participants who received workers' compensation for their treatments. All patients were informed that they were going to be in a study.
Intervention
We adapted isometric muscle strengthening exercises (Figs. 1 and 2). The strengthening exercise program was composed of four sets of 50 repetitions daily. Instructions on performing strengthening exercises were given by the senior author. The participants were instructed to do exercises gently, without pain so as to increase compliance rate and to reduce the potential of further injury to the affected tissues.7) Each of the patients was given a calendar and asked to keep a record of the days when he did the exercises. Then compliance was measured as the ratio of the number of days when they did the exercises to the total number of days that they were supposed to do the exercises.
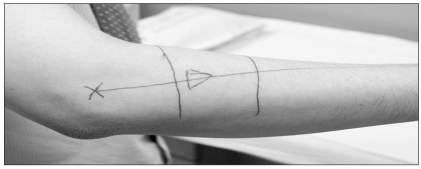
Fig. 1.
Picture showing the location of the lateral epicondyle (asterisk) and the direction of the extensor carpi radialis brevis (ECRB; arrowhead). Before providing instruction regarding the isometric strengthening exercise program, the anatomical location of the ECRB and the efficacy of isometric contraction of the ECRB were explained. By doing so, patients could understand the goal of the exercise treatment more easily.
Fig. 2.
The isometric strengthening exercise program was composed of four sets of 50 repetitions daily. Each static motion is performed for 10 seconds.
Outcome Measures
To evaluate the effectiveness of the treatment protocols, we used three self-report outcome measures: a pain visual analogue scale (VAS), the modified Nirschl/Pettrone score,8) and the Mayo elbow performance score (MEPS).9) The pain VAS is a horizontal line, 100 mm in length, anchored by word descriptors "no pain" at the left side and "very severe pain" at the right side. Participants were asked about elbow pain and function with the Modified Nirschl/Pettrone scoring system. For each item, there were five possible responses.
A. Full activity, no pain
B. No pain during normal daily activities, mild pain during sports/occupational activity
C. Occasional pain during normal daily activities, moderate pain during sports/occupational activity
D. Mild to moderate pain during normal daily activities, severe pain during sports/occupational activities
E. Pain at rest
The MEPS scale consisted of four categories: pain, range of motion, stability, and function, and total score was divided by 100, with higher scores indicating normal levels of elbow function. Clinical assessments were done at 1, 3, and 6 months. At 12 months, phone calls were made to participants to evaluate clinical outcomes and compliance with the home exercise program.
Statistical Analysis
Results for groups I and D were compared using the Mann-Whitney test for MEPS, a two-tailed unpaired Student's t-test for VAS, and a chi-square test for the modified Nirschl/Pettrone score. Statistical analysis was done using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). All tests were done using a 95% confidence level. The level of significance was set at p < 0.05.
RESULTS
Participant Demographics
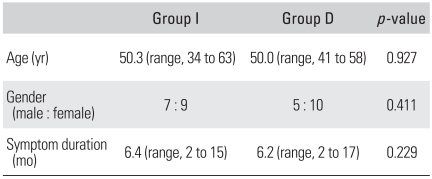
A total of 31 participants were enrolled in this study. Sixteen patients were in group I and fifteen in group D. The ratio of male to female was seven to nine in group I and five to ten in group D. The demographic data of the participants are listed in Table 1. No significant baseline differences were found between the groups regarding age, ratio of male to female, or duration of symptoms.
Table 1.
Epidemiologic Data
Compliance with the Exercise Program
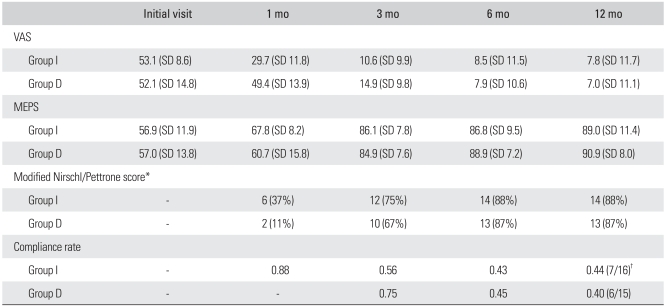
Inspection of participant diaries showed that at 3 months follow-up the compliance rate was 0.56 in group I and 0.75 in group D (p = 0.02) (Table 2). At 6 months, the compliance rate had decreased to 0.43 and 0.38 in groups I and D, respectively (p = 0.629) At 12 months, 52% of participants did not perform the exercises.
Table 2.
Results at Follow-up
VAS: Visual analogue scale, MEPS: Mayo elbow performance score, SD: Standard deviation.
*In Modified Nirschl/Pettrone score, we present the number of participants who answered A or B. †The compliance rate at 12 month is presented in the ratio of the number of participant who performed the exercise out of the total number of participants.
Effect of the Intervention
At the 1-month visit the average VAS score for group I was lower than for group D (p < 0.01) (Table 2). However, significant differences in VAS or MEPS were not found at 3- and 6-month follow-up. According to the evaluations through 12-month follow-up phone call, significant differences were not found in VAS and MEPS between the groups.
A significant difference between groups in Modified Nirschl/Pettrone scores was only found at 1-month follow-up. By then, the number of participants participants who returned to all activities with no pain or occasional mild pain was six (37%) in Group I and two (13%) in Group D (p = 0.031). At final follow-up, 88% of all participants performed activities without pain.
Withdrawn Participants
Five participants dropped out. Of these, two received ESWT in our hospital at the 1-month follow-up visit because they had not experienced reduced pain or improved function. The remaining three did not revisit our clinic after receiving instructions regarding how to do the strengthening exercises. A follow-up phone call revealed that the isometric strengthening exercise program had not led to substantial improvement in any of these three.
DISCUSSION
The present study was conducted to evaluate the effectiveness of a home-based isometric exercise strengthening program. In a clinical setting at a tertiary grade hospital, getting control data is not easy, which makes it difficult to determine the exact efficacy of the treatment independently of the natural course of improvement. Therefore, we only included patients who had more than 6 weeks of symptoms without improvement. In addition, by comparing groups with different exercise program starting points, we could observe the effectiveness of the isometric exercise program during the initial period. The findings of our study indicate that isometric exercise reduces pain and improves elbow function within a short period. After three-months of follow-up, except for a difference in compliance at three months, there were no differences in the other variables. One interesting finding was that none of the participants who dropped out showed improvement at the second visit. We assumed that this may be due to the limited efficacy of the isometric exercise in patients for whom the disease had progressed more. Actually, the mechanism by which a strengthening exercise program causes pain relief remains uncertain. Most studies regarding the efficacy of exercise investigated eccentric strengthening exercises in Achilles tendinopathy. Based on experimental studies, eccentric strengthening exercise causes tendon strengthening by stimulating mechanoreceptors in tenocytes to produce collagen, which is the key cellular mechanism that determines recovery from tendon injuries.10,11) Another reason for the positive effects of eccentric strengthening may be due to increased tensile strength in the muscle or decreased muscular strain during joint motion because of muscular lengthening.12,13) On the contrary, several authors have called into question the idea that the mechanism that produces positive effects in Achilles tendinopathy may not be applicable to LE. Martinez-Silvestrini et al.6) stated that, unlike Achilles tendinopathy, LE is often related to forceful grip activities requiring isometric contraction, which would be more beneficial than eccentric contraction in LE. In addition, following a supervised eccentric exercise protocol may not be convenient because patients should visit the hospital each time for exercise training and because this type of exercise often causes increased pain, which could result in abandonment of the exercises. In contrast, a home-based eccentric exercise program is convenient for the patients to perform without consideration of time, place, and supervision. However, patient compliance still remains a matter of concern. Judging from our clinical experience, compliance decreases when patients do exercise with pain or when the exercise protocol is not easy to follow. In this study, a simple isometric strengthening exercise program was used, which was easy to carry out without any equipment. In the early phase of the program (1 to 3 months), the compliance rate was over 70%. Because, most studies of home exercise programs have not mentioned participant compliance rates, we could not conclude whether our rate is appropriate or not. One interesting finding was that 48% patients continued doing the exercises at one-year follow-up regardless of symptoms, which reflects the acceptance of our treatment protocol.
Our study has several limitations that warrant review before drawing a definite conclusion. First, we could not find any theoretical evidence for the effectiveness of isometric exercise. Several authors only described the possibility of it conferring a benefit.6) Recently, eccentric strengthening exercise has gained attention for the treatment of LE.6,13) However, eccentric exercise often causes increase pain and some authors have emphasized that eccentric exercise should be performed without pain.14) Furthermore, to perform eccentric exercise, equipment such as a resistance band is necessary. In a review of the literature, we could not find compliance rates for home eccentric exercise programs. Considering that doing exercise with pain decreases compliance, enhancing compliance with eccentric exercises may be difficult. Second, although, the isometric strengthening exercises contributed to the reduction in symptoms, we do not know how much improvement the exercise caused because we did not compare the patient group with exercise to one without exercise. Third, to evaluate participants' compliance, at the beginning, we gave the subjects exercise calendars. However, in the intermediate to late period, some participants kept records that were only partially completed. Therefore, the compliance rate was not accurately measured in all participants. Fourth, we do not have enough clinical data to support this treatment protocol. Therefore, a future study will be required to investigate the most effective regimen. Fifth, the follow-up intervals in the initial period were not uniform between the groups due to the limitations of the outpatient clinical setting.
In conclusion, an isometric strengthening exercise program early in the course of LE (within 4 weeks) provides clinically significant improvement. A large-scale study will be required to determine whether an early response to the strengthening exercise program can be used as a prognostic factor.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow): clinical features and findings of histological, immunohistochemical, and electron microscopy studies. J Bone Joint Surg Am. 1999;81(2):259–278. [PubMed] [Google Scholar]
- 2.Stasinopoulos D, Stasinopoulou K, Johnson MI. An exercise programme for the management of lateral elbow tendinopathy. Br J Sports Med. 2005;39(12):944–947. doi: 10.1136/bjsm.2005.019836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smidt N, van der Windt DA, Assendelft WJ, Deville WL, Korthals-de Bos IB, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet. 2002;359(9307):657–662. doi: 10.1016/S0140-6736(02)07811-X. [DOI] [PubMed] [Google Scholar]
- 4.Tonks JH, Pai SK, Murali SR. Steroid injection therapy is the best conservative treatment for lateral epicondylitis: a prospective randomised controlled trial. Int J Clin Pract. 2007;61(2):240–246. doi: 10.1111/j.1742-1241.2006.01140.x. [DOI] [PubMed] [Google Scholar]
- 5.Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow: an attempted meta-analysis. J Bone Joint Surg Br. 1992;74(5):646–651. doi: 10.1302/0301-620X.74B5.1388172. [DOI] [PubMed] [Google Scholar]
- 6.Martinez-Silvestrini JA, Newcomer KL, Gay RE, Schaefer MP, Kortebein P, Arendt KW. Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther. 2005;18(4):411–419. doi: 10.1197/j.jht.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 7.Nirschl RP. Elbow tendinosis/tennis elbow. Clin Sports Med. 1992;11(4):851–870. [PubMed] [Google Scholar]
- 8.Stahl S, Kaufman T. The efficacy of an injection of steroids for medial epicondylitis: a prospective study of sixty elbows. J Bone Joint Surg Am. 1997;79(11):1648–1652. doi: 10.2106/00004623-199711000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Turchin DC, Beaton DE, Richards RR. Validity of observer-based aggregate scoring systems as descriptors of elbow pain, function, and disability. J Bone Joint Surg Am. 1998;80(2):154–162. doi: 10.2106/00004623-199802000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the "tendinitis" myth. BMJ. 2002;324(7338):626–627. doi: 10.1136/bmj.324.7338.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohberg L, Lorentzon R, Alfredson H. Eccentric training in patients with chronic Achilles tendinosis: normalised tendon structure and decreased thickness at follow up. Br J Sports Med. 2004;38(1):8–11. doi: 10.1136/bjsm.2001.000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med. 2000;29(2):135–146. doi: 10.2165/00007256-200029020-00005. [DOI] [PubMed] [Google Scholar]
- 13.Svernlov B, Adolfsson L. Non-operative treatment regime including eccentric training for lateral humeral epicondylalgia. Scand J Med Sci Sports. 2001;11(6):328–334. doi: 10.1034/j.1600-0838.2001.110603.x. [DOI] [PubMed] [Google Scholar]
- 14.Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res. 1986;(208):65–68. [PubMed] [Google Scholar]