Abstract
Context
Recent trends in hours worked by physicians may affect workforce needs but have not been thoroughly analyzed.
Objectives
To estimate trends in hours worked by US physicians and assess for association with physician fees.
Design, Setting, and Participants
A retrospective analysis of trends in hours worked among US physicians using nationally representative workforce information from the US Census Bureau Current Population Survey between 1976 and 2008 (N=116 733). Trends were estimated among all US physicians and by residency status, sex, age, and work setting. Trends in hours were compared with national trends in physician fees, and estimated separately for physicians located in metropolitan areas with high and low fees in 2001.
Main Outcome Measure
Self-reported hours worked in the week before the survey.
Results
After remaining stable through the early 1990s, mean hours worked per week decreased by 7.2% between 1996 and 2008 among all physicians (from 54.9 hours per week in 1996–1998 to 51.0 hours per week in 2006–2008; 95% confidence interval [CI], 5.3%–9.0%; P<.001). Excluding resident physicians, whose hours decreased by 9.8% (95% CI, 5.8%–13.7%; P<.001) in the last decade due to duty hour limits imposed in 2003, nonresident physician hours decreased by 5.7% (95% CI, 3.8%–7.7%; P<.001). The decrease in hours was largest for nonresident physicians younger than 45 years (7.4%; 95% CI, 4.7%–10.2%; P<.001) and working outside of the hospital (6.4%; 95% CI, 4.1%–8.7%; P<.001), and the decrease was smallest for those aged 45 years or older (3.7%; 95% CI, 1.0%–6.5%; P=.008) and working in the hospital (4.0%; 95% CI, 0.4%–7.6%; P=.03). After adjusting for inflation, mean physician fees decreased nationwide by 25% between 1995 and 2006, coincident with the decrease in physician hours. In 2001, mean physician hours were less than 49 hours per week in metropolitan areas with the lowest physician fees, whereas physician hours remained more than 52 hours per week elsewhere (P<.001 for difference).
Conclusion
A steady decrease in hours worked per week during the last decade was observed for all physicians, which was temporally and geographically associated with lower physician fees.
The potential expansion of health insurance coverage and associated reform of the delivery system, combined with recent forecasts of physician shortages (particularly in primary care), have catapulted issues related to the adequacy of the physician workforce high up on the health policy agenda.1–8 Whether the workforce is equipped to handle the demand for physician services depends on both the quantity and specialty distribution of physicians and the number of hours worked per physician. Most research and policy debate on the physician workforce, however, has focused on the numbers of current and future physicians and has largely ignored the hours worked by physicians.
This uneven focus likely stems from the availability of data on numbers of physicians and because the supply of new physicians can be more readily influenced by actions of private or government entities to alter the numbers of medical schools and residency positions, and funding of graduate medical education. In contrast, data on hours worked by physicians have not been reported by the American Medical Association (AMA) since 2001,9 and data up to that time did not suggest significant shifts in hours worked. Consequently, other than adjusting for changes in the composition of the workforce (eg, accounting for the growing proportion of female physicians and the increase in physician retirements10), most projections of the physician workforce assume hours worked by physicians remain constant.5
However, a 2006 report on trends in physician incomes based on snapshots of the physician workforce in 1995, 1999, and 2003, and a special survey commissioned by the Health Resources and Services Administration covering 2002, suggest that assumptions about steady hours worked may no longer be warranted.11,12 Moreover, recent projections of physician supply from the Health Resources and Services Administration and other organizations have begun to raise concerns about changing work hours of physicians.11,13,14 In this study, we examined trends in hours worked by physicians using data from the US Census Bureau for each year between 1976 and 2008.We also examined whether trends in physician hours were associated with concurrent trends in physician fees both nationally and by geographic region within the United States.
METHODS
Current Population Survey Data
Data on physician hours were obtained from the Current Population Survey (CPS), a household-based survey administered monthly by the US Census Bureau that covers a nationally representative sample of more than 100 000 individuals. In addition to demographic information collected in each month of the survey, the survey asks detailed questions about employment, including occupation and hours worked. The sample in each month was a representative cross-section of households. Each housing unit was included in the sample 8 times over the course of 16 months, with new housing units rotating in and out of the sample each month; therefore, some individuals appeared multiple times in the sample. Data from the CPS are used extensively by researchers and by the US Department of Labor to estimate trends in employment and hours.
Data from the CPS were obtained for all individuals employed as a “physician or surgeon” in the week of the survey between January 1976 and December 2008. This occupation category in the CPS includes osteopathic physicians as well as physicians in all specialties (including residents), but excludes other health care practitioners, such as chiropractors, dentists, optometrists, and podiatrists. Approximately 6.5% of physicians in the CPS work primarily in industries outside of health care services, most commonly educational services, public administration, and scientific research, and were excluded from the analysis. Data on physician work hours were based on reported hours worked at all jobs in the previous week. Physicians reporting zero or missing hours were excluded from the sample. The final sample included 116 733 monthly surveys of physicians obtained from 27 874 unique households spread over 33 years. To compare trends in physician work hours to other professions, we used the same procedures to obtain data from the CPS for attorneys, engineers, and registered nurses.
Information on the physician’s work setting (hospital or not), self-employment status, age, sex, and metropolitan area of residence was also obtained from the CPS survey. One limitation of the CPS survey is that it includes no questions about physician specialty or resident status. We identified physicians as residents if they were younger than 35 years and working in a hospital, because data from the AMA Physician Masterfile for 2007 indicate that 97% of hospital-based physicians younger than 35 years were residents, while among all other physicians involved in patient care only 3% were residents.15 A second limitation is that the CPS does not count many physicians in group practice as self-employed and, before 1989, also did not count any physicians who were incorporated as self-employed. Thus, the definition of a self-employed physician in our data is restrictive, and estimates for self-employed physicians before 1989 may not be directly comparable with later years.
Trends in Physician Fees
To examine whether trends in physician fees were associated with hours worked, we constructed an inflation-adjusted physician fee index that captures how payments to physicians have changed over time. Conceptually, the index represents mean prices paid by Medicare and by private insurance for a representative bundle of physician services provided in any given year. For the Medicare portion of the index, we used the reported fee index contained in the trustees’ reports on the Medicare program. 16–18 Private-sector fees were derived using published estimates of the ratio of private fees to Medicare fees.19,20 Our fee index is the weighted average of the Medicare and private-sector fee index, where the weight was the proportion of total spending on physician services accounted for by the Medicare program as reported in the National Health Accounts.21 Data on fees paid by Medicaid and other payers such as the Veterans Administration were unavailable; however, these sources represent only approximately 10% of physician reimbursements.22 Data on private fees were not available before 1989 or after 2006. Therefore, we constructed the fee index only for the the years between 1989 and 2006. Finally, we adjusted the index for inflation using the Consumer Price Index for All Urban Consumers.
To examine whether differences in fees across geographic areas were associated with trends in hours, we used a physician fee index constructed by the Government Accountability Office (GAO) that captures how payments to physicians by the Federal Employees Health Benefits program differed across 319 metropolitan areas in 2001, holding constant the cost of doing business and the mix of services provided.23 The average fees in each metropolitan area were adjusted by the GAO using methods similar to that used by Medicare to account for geographic differences in the cost of providing care. Between 1989 and 2008, 84%of the physicians in our sample lived in 1 of 319 metropolitan statistical areas (MSAs) (before 1989, MSAs were not consistently identified in the CPS). Physicians were designated as living in an MSA with low fees (vs high fees) if the GAO fee index from 2001 in their MSA was below the median in our sample.
Institutional Review Board Approval
This study used publicly available data and was exempt from institutional review board review.
Statistical Analysis
Mean hours worked by physicians (and comparison occupations) were estimated for each year and reported as 3-year moving averages to smooth fluctuations in the data. We analyzed trends separately for residents and nonresidents, because forces determining hours of work were likely to differ for residents. In particular, hours of residents were largely determined by their training program and affected by duty hour limits imposed in July 2003,24 whereas physicians in private practice were freer to choose hours based on their own preferences and financial incentives. To estimate trends in hours of residents, we excluded data from 2003 because duty hour limits were imposed mid-year. For nonresident physicians, we estimated trends overall and for subgroups of physicians by age (<45 vs ≥45 years), sex, work setting (hospital vs nonhospital), whether the physician reported being self-employed, and whether the physician lived in an MSA that had high or low fees in 2001. These subgroups were chosen after examining the overall trend in hours to explore whether changes in hours were concentrated in particular demographic groups or among physicians in particular work settings.
Analysis of variance models were used to test whether mean hours were equal across all the years in our sample, and to test the hypothesis that mean hours were equal across subgroups (eg, men vs women) in each year. All estimates were weighted by sampling weights provided by the CPS, making them representative of the US noninstitutionalized population. Unweighted estimates were similar (see eTable 1, eTable 2, eTable 3, and eTable 4 at http://www.jama.com). Standard errors for these estimates were calculated in a manner that accounted for the use of sampling weights and the existence of multiple observations in the sample for some individuals and households. 25 Ninety-five percent confidence intervals (CIs) for the 3-year averages and for the percentage change over time in these estimates were based on the delta method. Given the sample size available, and a 2-sided α=.05, our study had the power to detect a change over time in mean hours among all physicians of 2.7%, with a probability of 80%. To test for an association over time between mean hours of nonresident physicians and the physician fee index, we calculated the simple correlation between 1989 and 2006 (the years in which the fee index was available) and tested whether the correlation was equal to zero. To test whether hours trends were the same in MSAs with high and low fees in 2001, analysis of variance models were used to test the hypothesis that mean hours were equal across the 2 groups in each year between 1989 and 2008 (MSA was not consistently identified before 1989). All tests were 2-sided, withP<.05 considered statistically significant. Statistical analyses were performed by using STATA version 10.1 (Stata Corp, College Station, Texas).
RESULTS
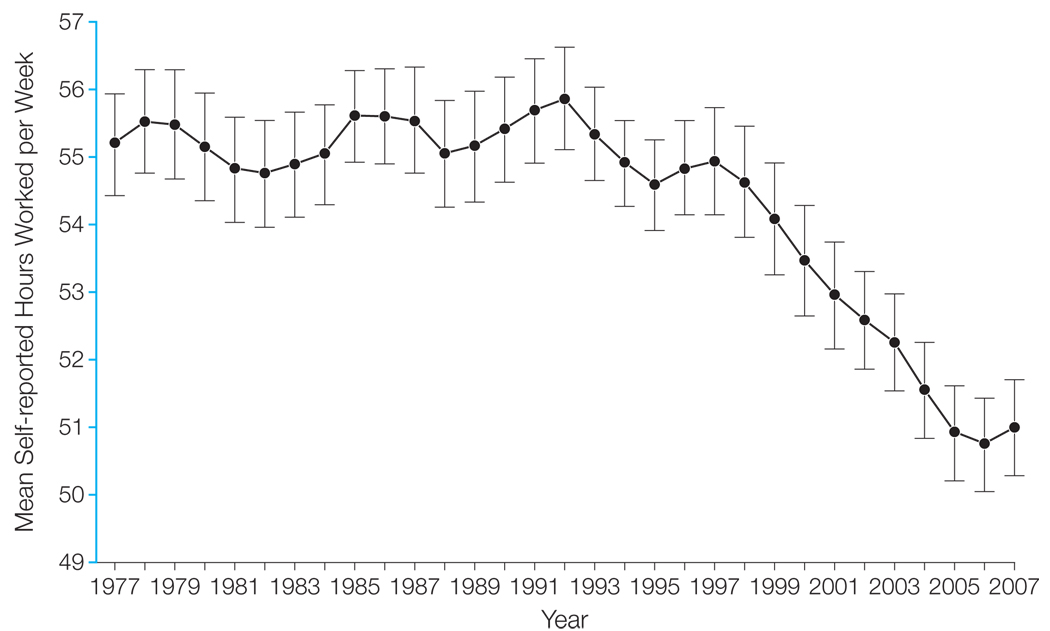
Mean hours worked per week among all physicians, plotted as a 3-year moving average in Figure 1 and reported at 10-year intervals in the Table, changed significantly during the sample period (P<.001). Physician hours were fairly stable at approximately 55 hours per week between 1977 and 1997, showing no trend and ranging from a low of 54.6 hours per week to a high of 55.9 hours per week. However, between 1997 and 2007, hours per week decreased steadily, decreasing nearly 4 hours per week to 51 hours per week (7.2%; 95% CI, 5.3%–9.0%; P<.001).
Figure 1. Mean Self-reported Hours Worked per Week by Physicians Between 1977 and 2007.
Current Population Survey data based on hours worked in the previous week. Data represent 3-year moving averages for each year plotted (eg, 1977 represents 1976–1978 and 2007 represents 2006–2008) and are weighted using sampling weights. Error bars indicate 95% confidence intervals.
Table 1.
Mean Self-reported Hours Worked per Week by Physicians for Selected Years by Resident Status, Sex, Age, and Work Settinga
| Mean Hours per Week (95% CI) |
||||||
|---|---|---|---|---|---|---|
| Characteristics | Total No. of Observationsb |
1976–1978 (n = 7812) |
1986–1988 (n = 9763) |
1996–1998 (n = 10 247) |
2006–2008 (n = 12 469) |
% Change Between 1996–1998 and 2006–2008 (95% CI) |
| All physicians | 40 291 | 55.2 (54.4–55.9) | 55.6 (54.8–56.3) | 54.9 (54.2–55.7) | 51.0 (50.3–51.7) | −7.2 (−5.3 to −9.0) |
| Nonresident physiciansc | 33 625 | 53.6 (52.8–54.4) | 53.3 (52.5–54.1) | 52.6 (51.9–53.4) | 49.6 (48.9–50.4) | −5.7 (−3.8 to −7.7) |
| Resident physiciansc | 6666 | 60.8 (59.0–62.6) | 65.0 (63.1–66.9) | 65.7 (63.7–67.8) | 59.3 (57.4–61.1) | −9.8 (−5.8 to −13.7) |
| Excluding resident physicians | ||||||
| Age <45 y | 15 155 | 55.9 (54.7–57.0) | 55.3 (54.2–56.4) | 54.2 (53.2–55.3) | 50.2 (49.1–51.3) | −7.4 (−4.7 to −10.2) |
| Age ≥45 y | 18 470 | 51.7 (50.7–52.8) | 51.1 (50.0–52.2) | 51.2 (50.1–52.3) | 49.3 (48.3–50.2) | −3.7 (−1.0 to −6.5) |
| Men | 26 682 | 54.6 (53.8–55.4) | 54.4 (53.6–55.2) | 54.4 (53.6–55.3) | 51.7 (50.9–52.6) | −5.0 (−2.8 to −7.2) |
| Women | 6943 | 44.2 (41.9–46.4) | 47.0 (45.1–48.9) | 46.7 (45.2–48.3) | 44.4 (43.2–45.5) | −5.1 (−1.0 to −9.1) |
| Hospital | 8089 | 50.2 (48.7–51.7) | 52.0 (50.5–53.4) | 52.2 (50.8–53.6) | 50.1 (48.8–51.4) | −4.0 (−0.4 to −7.6) |
| Nonhospital | 25 536 | 54.4 (53.5–55.3) | 53.6 (52.7–54.5) | 52.8 (51.9–53.7) | 49.4 (48.5–50.3) | −6.4 (−4.1 to −8.7) |
| Self-employed | 12 539 | 54.3 (53.1–55.4) | 52.8 (51.4–54.1) | 54.2 (53.0–55.4) | 50.9 (49.6–52.2) | −6.0 (−2.9 to −9.2) |
| Non–self-employed | 21 086 | 53.1 (52.1–54.1) | 53.5 (52.6–54.4) | 51.5 (50.5–52.4) | 49.0 (48.2–49.9) | −4.7 (−2.3 to −7.1) |
| Nonphysicians | ||||||
| Lawyers | 56 608 | 45.2 (44.7–45.6) | 46.3 (45.9–46.7) | 45.9 (45.5–46.4) | 44.9 (44.5–45.3) | −2.4 (−1.0 to −3.6) |
| Engineers | 114 276 | 42.5 (42.3–42.6) | 42.9 (42.7–43.1) | 43.6 (43.4–43.8) | 43.0 (42.8–43.2) | −1.4 (−0.7 to −2.1) |
| Registered nurses | 129 545 | 35.6 (35.3–35.9) | 36.4 (36.2–36.7) | 36.7 (36.4–36.9) | 37.3 (37.1–37.5) | 1.6 (0.7 to 2.6) |
Abbreviation: CI, confidence interval.
Data were derived from the Current Population Survey data based on hours worked in the previous week. Data represent 3-year averages as indicated and are weighted using sampling weights.
For the 12 years shown.
Resident physicians are defined as physicians younger than 35 years and working in a hospital. Nonresident physicians are all others.
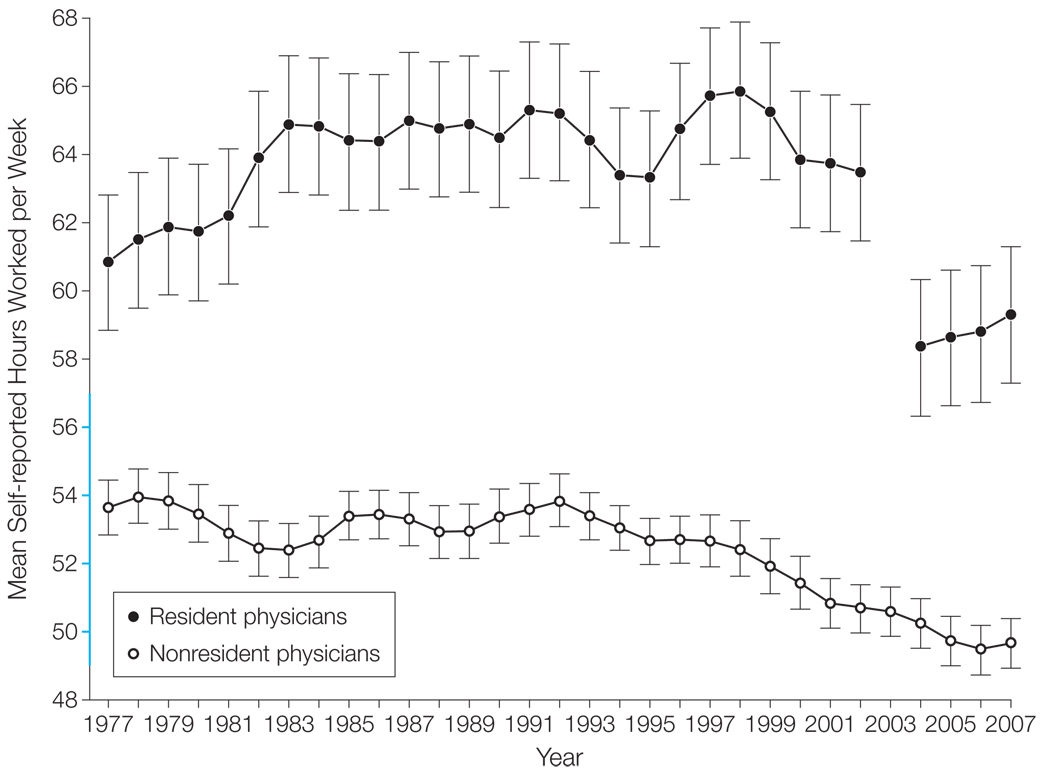
Trends in hours per week differed significantly (P<.001) between physicians who were residents (<35 years and working in the hospital) and those who were not residents (≥35 years or working outside the hospital). During the last decade (between 1996–1998 and 2006– 2008), hours decreased significantly for both residents (9.8%; 95% CI, 5.8%–13.7%; P<.001) and nonresidents (5.7%; 95% CI, 3.8%–7.7%; P<.001). However, as shown in Figure 2, resident hours remained high through 2002 and then decreased sharply following the imposition of work-hour limits in 2003, whereas hours of all other physicians decreased more steadily during the last decade.
Figure 2. Mean Self-reported Hours Worked per Week by Resident and Nonresident Physicians Between 1977 and 2007.
Current Population Survey data based on hours worked in the previous week. Data represent 3-year moving averages for each year plotted (eg, 1977 represents 1976–1978 and 2007 represents 2006–2008) and are weighted using sampling weights. Error bars indicate 95% confidence intervals. The 2003 data for residents are excluded and are also not used in the 2002 and 2004 moving averages, because duty hour restrictions for residents went into effect on July 1, 2003 (80-hour work week was implemented). The blue portion of the y-axis indicates 49 to 57 self-reported hours worked per week, the range for all physicians (Figure 1).
The decrease in hours worked by nonresident physicians during the last decade was broad-based and not concentrated among physicians with particular demographic characteristics or working in particular settings (Table). Between 1996–1998 and 2006–2008, hours worked decreased significantly (P<.05) among younger and older physicians, male and female physicians, physicians employed in hospital and nonhospital settings, and among self-employed and non–self-employed physicians. The decrease in hours during this period was largest for nonresident physicians younger than 45 years (7.4%; 95% CI, 4.7%–10.2%; P<.001) and those working outside of the hospital (6.4%; 95% CI, 4.1%–8.7%; P<.001), and the decrease was smallest for those aged 45 years or older (3.7%; 95% CI, 1.0%–6.5%; P=.008) and those working in the hospital (4.0%; 95% CI, 0.4%–7.6%; P=.03). In contrast, mean weekly hours of other professionals such as lawyers, engineers, and registered nurses changed very little during the past 30 years, which is consistent with national trends in mean weekly hours among all workers published by the US Bureau of Labor Statistics.26,27
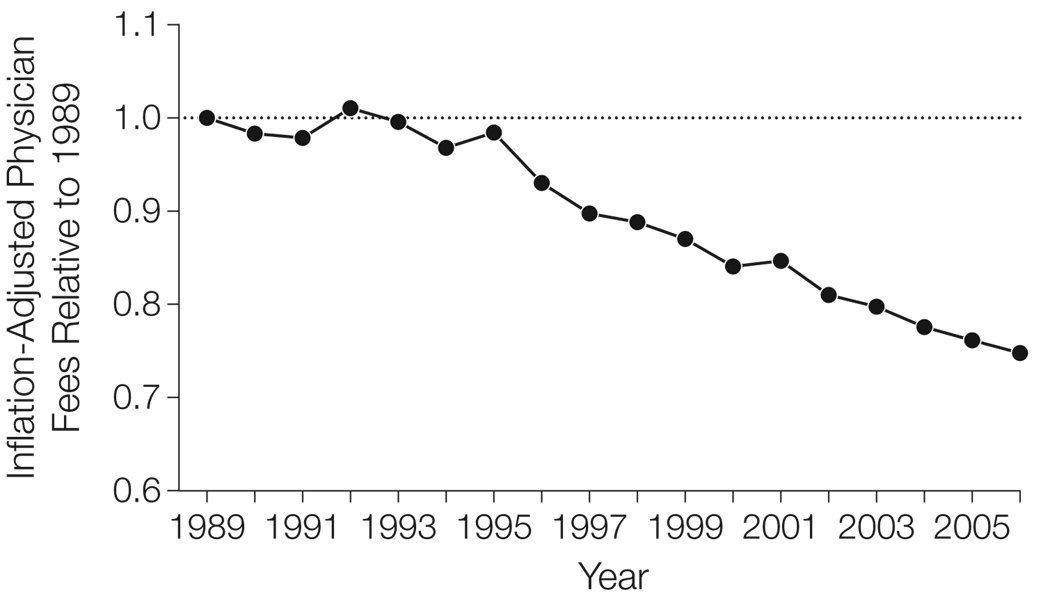
The decrease in hours worked by physicians coincided with a decrease in physician fees, measured by the national inflation-adjusted physician fee index (Figure 3). Inflation-adjusted physician fees changed little between 1989 and 1995, but then decreased substantially during the next 10 years. By 2006, physician fees were 25% lower than their inflation-adjusted 1995 levels. The timing of the decrease in fees closely matched the observed decrease in nonresident physician hours worked (Figure 2). Mean hours worked by nonresident physicians were strongly associated with the fee index (correlation= 0.965, P<.001) and even more strongly associated with the fee index from the prior year (correlation=0.969, P<.001).
Figure 3. Inflation-Adjusted Physician Fees Between 1989 and 2006.
Fee index is a weighted average of Medicare and private-sector fees compiled from several sources. Medicare fees are based on Medicare trustees’ reports. Private-sector fees are derived from combining the Medicare fees and independent estimates of the ratio of private fees to Medicare fees published by MedPAC for 1999–2006, by Direct Research LLC from 1989–1996, and interpolated for 1997–1998, when that ratio was not available. The proportion of physician services that Medicare comprises comes from the Centers for Medicare & Medicaid Services. The Consumer Price Index for All Urban Consumers was used to convert nominal to real. Medicaid or other services outside of Medicare or private are excluded.
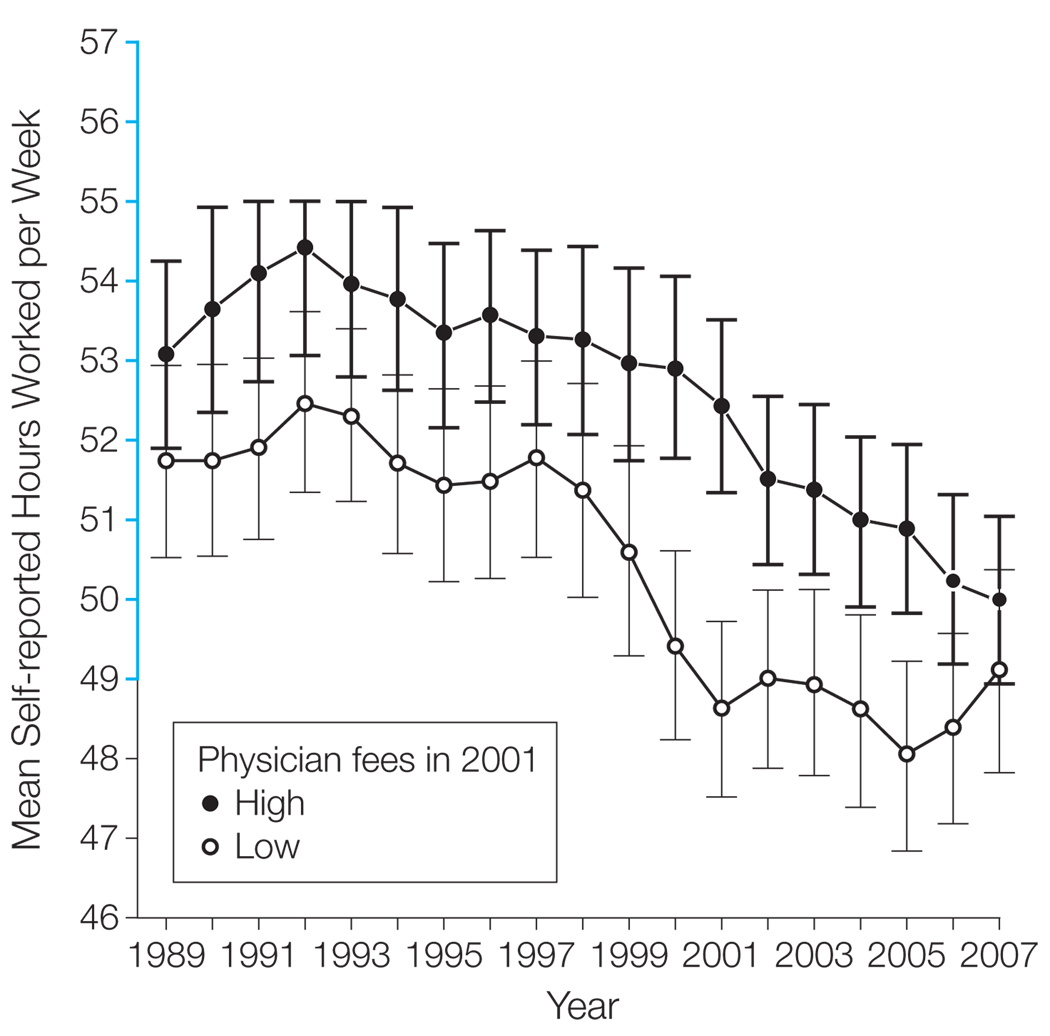
Trends in hours worked were significantly different (P<.001) for physicians living in MSAs that had the lowest fees in 2001 compared with physicians living in MSAs with high fees, measured by GAO’s metropolitan fee index (Figure 4). According to this index, fees in 2001 were approximately 18% lower on average in low-fee MSAs compared with high-fee MSAs. Correspondingly, physicians living in the low-fee MSAs already worked less than 49 hours per week by 2001, whereas physicians in high-fee MSAs continued to work more than 52 hours per week (P<.001 for difference from low-fee MSAs in 2001). The national trend toward lower hours occurred before 2001 in MSAs that had the lowest fees in 2001, and occurred after 2001 in the remaining MSAs.
Figure 4. Mean Self-reported Hours Worked per Week by Physicians in Metropolitan Statistical Areas (MSAs) With High and Low Physician Fees in 2001.
Current Population Survey (CPS) data based on hours worked in the previous week. Data represent 3-year moving averages for each year plotted (eg, 1989 represents 1988–1990 and 2007 represents 2006–2008) and are weighted using sampling weights. Error bars indicate 95% confidence intervals. Physicians were designated as living in a low-fee (vs high-fee) MSA if the Government Accountability Office fee index from 2001 in their MSA was below the median in our sample. Years before 1989 are excluded because MSA is not consistently identified before 1989 in the CPS data. The blue portion of the y-axis indicates 49 to 57 self-reported hours worked per week, the range for all physicians (Figure 1).
COMMENT
After remaining stable for 2 decades, there was a significant decrease in hours worked per week by physicians during the last decade. Among resident physicians, hours changed little through the 1980s and 1990s, until decreasing dramatically in 2003 following the implementation of work-hour limits. Among physicians who were not residents, hours have decreased steadily since the mid-1990s. This decrease was broad-based, occurring among physicians in different demographic groups and in different employment settings. During the same period, there were no similar decreases in hours worked by other professions, suggesting that forces responsible for the observed reduction in work hours were unique to physicians.
The decrease in nonresident physician work hours likely reflects a combination of economic and noneconomic factors. The observed decrease in physician fees is a potential economic factor behind the decrease in physician hours. As indicated in our analysis, mean physician fees adjusted for inflation decreased by 25% between 1996 and 2006, coinciding with the decrease in physician hours. Additionally, physician hours were lower and decreased first in MSAs where fees were lowest in 2001. Although there were no data on fees in these MSAs in other years, it is reasonable to infer that the national trend toward lower fees occurred before 2001 in the MSAs that had low fees in 2001, and occurred after 2001 in the remaining MSAs.
When fees decrease, a physician earns less for working an additional hour, all else equal, and may have less incentive to work long hours. However, the evidence on the relationship between fees and work hours is mixed, with some studies finding that lower fees encourage physicians to work more hours to achieve a target income.28 Because fees have decreased, some physicians have undertaken other activities to offset the loss in income, such as reducing the proportion of time spent in non–patient care activities,12 increasing ownership stake in ancillary services,29 and increasing the intensity of services provided,30 or spending less time per patient.31 Therefore, although mean physician income adjusted for inflation decreased by 7% between 1995 and 2003,12 it is less than would be expected based on the 19% decrease in fees and 5% decrease in hours we observed during this period if there had been no offsetting behavior by physicians. Nevertheless, such activities by physicians may make work less satisfying and only partially offset the decrease in fees, thereby reducing the incentives for physicians to work long hours.
A third factor associated with lower fees may also have been responsible for the decrease in physician hours. Several developments among both public and private payers occurred in the mid-to late 1990s (increasing managed care penetration, insurer consolidation, and Medicare’s implementation of the Resource-Based Relative Value Scales for physicians’ payment). Similarly, the GAO found that MSAs with lower physician fees in 2001 tended to have greater competition and managed care penetration.23 Therefore, greater competition and managed care penetration may have been associated with lower fees, but at the same time weakened physician autonomy and reduced job satisfaction, which in turn could have led to fewer hours. However, despite anecdotal reports, data from physician surveys suggest that, after declining during the 1980s and early 1990s, there has been no systematic decrease in physician satisfaction since the mid-1990s.32–35 Improvements in physician productivity driven by these market changes, resulting from the adoption of information technology and other practice innovations,36 could also have allowed physicians to reduce both fees and hours while at the same time increase their billing rate. However, inflation-adjusted physician income either decreased12 or was stagnant30 during this period, which would be surprising if these changes were driven solely by increased productivity.
Several noneconomic explanations might account for the recent decrease in physician hours, but none are fully consistent with our findings. For example, although female physicians work fewer mean hours and represent an increasing proportion of physicians, decreases in hours were observed for both male and female physicians. Similarly, limits on resident work hours were imposed in 2003, but decreases in work hours were observed for nonresident physicians and began before 2003. Decreases in hours were larger for younger physicians, which might suggest that preferences for balanced lifestyles among younger cohorts are a partial explanation. Although the Council on Graduate Medical Education has raised concerns that such preference may affect the hours of physicians in the future, we are unaware of any evidence that intrinsic preference for a balanced lifestyle, all else equal, has changed among physicians during the last decade. Moreover, we observed decreases in hours in the same years for physicians of all ages, and decreases in hours did not occur earlier among young physicians (as would be expected if only recent cohorts had such preferences). Although there has been a shift in physician employment toward larger practices and institutional settings,37 we found decreases in hours for both self-employed physicians and physicians working in hospitals. Finally, while changing specialty choice of physicians could contribute to a change in hours, data from the AMA Physician Masterfile indicate that the proportion of physicians working in relatively low-hour specialties, such as dermatology, pathology, and emergency medicine, changed by less than 1% during the last decade.15,38
Our study had some limitations. It was not designed to assess the possibility of a causal relationship between the observed trends in both hours and fees. As discussed above, it is likely that a third factor that was associated with lower fees, such as growing managed care penetration or market competition, may have contributed to the decrease in physician hours. Moreover, the lack of fee data before 1989 leaves open the possibility that trends observed to have begun in the 1990s may have already been underway. Finally, the lack of physician specialty in our data is an important limitation. The effect of both economic and noneconomic factors on physician work hours undoubtedly differs by medical specialty, particularly for primary care physicians. Other more focused data sources should be explored to further understand the relationship between specialty, fees, and trends in hours worked.
CONCLUSION
Our results have implications for how reform efforts and market forces may affect the future physician workforce. 39 Our findings are consistent with the possibility that economic factors such as lower fees and increased market pressure on physicians may have contributed, at least in part, to the recent decrease in physician hours. Further reductions in fees and increased market pressure on physicians may, therefore, contribute to continued decreases in physician work hours in the future.
Whatever the underlying cause, the decrease in mean hours worked among US physicians during the last decade raises implications for physician workforce supply and overall health care policy. A 5.7% decrease in hours worked by nonresident physicians in patient care, out of a workforce of approximately 630 000 in 2007,15 is equivalent to a loss of approximately 36 000 physicians from the workforce, had hours worked per physician not changed. Although the number of physicians has nearly doubled during the last 30 years,10 many workforce analysts and professional organizations are concerned about the adequacy of the size of the future physician workforce. This trend toward lower hours, if it continues, will make expanding or maintaining current levels of physician supply more difficult, although increases in the number of practicing physicians either through increases in the size of domestic medical school classes or further immigration of international medical graduates would mitigate those concerns. Moreover, if this trend toward lower physician hours continues, it could frustrate stated goals of health reform,4 which may require an expanded physician workforce to take on new roles and enhanced functions in a reformed delivery system.
Acknowledgments
Funding/Support: This work was supported by grant 2 P01 AG19783-06 from the National Institute on Aging (Dr Staiger).
Role of the Sponsor: The National Institute on Aging played no role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Staiger had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Staiger, Auerbach, Buerhaus.
Acquisition of data: Staiger, Auerbach.
Analysis and interpretation of data: Staiger, Auerbach, Buerhaus.
Drafting of the manuscript: Staiger, Auerbach, Buerhaus.
Critical revision of the manuscript for important intellectual content: Auerbach, Buerhaus.
Statistical analysis: Staiger, Auerbach.
Administrative, technical, or material support: Staiger, Buerhaus.
Study supervision: Buerhaus.
Financial Disclosures: None reported.
Disclaimer: The views expressed in this article are those of the authors and should not be interpreted as those of the US Congressional Budget Office.
Online-Only Material: eTables 1 through 4 are available at http://www.jama.com.
Contributor Information
Douglas O. Staiger, Department of Economics, Dartmouth College, Hanover, New Hampshire, and National Bureau of Economic Research, Cambridge, Massachusetts.
David I. Auerbach, Health and Human Resources Division, Congressional Budget Office, Washington, DC.
Peter I. Buerhaus, School of Nursing, Center for Interdisciplinary Health Workforce Studies, Institute for Medicine and Public Health, Vanderbilt University Medical Center, Nashville, Tennessee.
REFERENCES
- 1.Medicare Payment Advisory Commission. Report to the Congress: improving incentives in the Medicare program. [Accessed January 21, 2010]; http://www.medpac.gov/documents/Jun09_EntireReport.pdf.
- 2.US Congressional Budget Office. Key issues in analyzing major health insurance proposals. [Accessed January 21, 2010]; http://www.cbo.gov/ftpdocs/99xx/doc9924/12-18-KeyIssues.pdf.
- 3.US Government Accountability Office. Testimony before the Committee on Health, Education, Labor, and Pensions, US Senate: primary care professionals: recent supply trends, projections, and valuation of services. [Accessed January 21, 2010]; http://www.gao.gov/new.items/d08472t.pdf.
- 4.Senate Finance Committee. Call to action: health reform 2009. [Accessed January 21, 2010]; http://finance.senate.gov/healthreform2009/finalwhitepaper.pdf.
- 5.US Department of Health and Human Services, Health Resources and Services Administration. Physician supply and demand: projections to 2020. [Accessed January 21, 2010]; ftp://ftp.hrsa.gov/bhpr/workforce/PhysicianForecasting-Paperfinal.pdf.
- 6.Sandy LG, Bodenheimer T, Pawlson LG, Starfield B. The political economy of U.S. primary care. Health Aff (Millwood) 2009;28(4):1136–1145. doi: 10.1377/hlthaff.28.4.1136. [DOI] [PubMed] [Google Scholar]
- 7.Bodenheimer T, Grumbach G, Berenson RA. A lifeline for primary care. N Engl J Med. 2009;360(26):2693–2696. doi: 10.1056/NEJMp0902909. [DOI] [PubMed] [Google Scholar]
- 8.Iglehart JK. Grassroots activism and the pursuit of an expanded physician supply. N Engl J Med. 2008;358(16):1741–1749. doi: 10.1056/NEJMhpr0800058. [DOI] [PubMed] [Google Scholar]
- 9.American Medical Association. Socioeconomic monitoring system public use files. [Accessed January 21, 2010]; http://www.ama-assn.org/ama1/pub/upload/mm/363/sefile.pdf.
- 10.Staiger DO, Auerbach DI, Buerhaus PI. Comparison of physician workforce estimates and supply projections. JAMA. 2009;302(15):1674–1680. doi: 10.1001/jama.2009.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services; Health Resources and Services Administration. The physician workforce: projections and research into current issues affecting supply and demand. [Accessed January 21, 2010]; ftp://ftp.hrsa.gov/bhpr/workforce/physicianworkforce.pdf.
- 12.Tu HT, Ginsberg PB. Losing ground: physician income, 1995–2003: Tracking Report No. 15. [Accessed January 21, 2010];2006 June; http://www.hschange.org/CONTENT/851/ [PubMed]
- 13.Dill MJ, Salsberg ES. The complexities of physician supply and demand: projections through 2025. [Accessed January 21, 2010]; https://services.aamc.org/publications/showfile.cfm?file=version122.pdf&prd_id=244&prv_id=299&pdf_id =122.
- 14.Council on Graduate Medical Education. Physician Workforce Policy Guidelines for the United States, 2000–2020. Sixteenth Report. Washington, DC: Health Resources and Services Administration; 2005
- 15.Physician Characteristics and Distribution in the US. Chicago, IL: American Medical Association; 2009. [Google Scholar]
- 16.Centers for Medicare & Medicaid Services. Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. Baltimore, MD: Centers for Medicare & Medicaid Services; 1997 1997.
- 17.Centers for Medicare & Medicaid Services. Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. [Accessed January 21, 2010];2002 http://www.cms.hhs.gov/ReportsTrustFunds/downloads/tr2002.pdf.
- 18.Centers for Medicare & Medicaid Services. Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. [Accessed January 21, 2010];2008 http://www.cms.hhs.gov/ReportsTrustFunds/downloads/tr2008.pdf.
- 19.MedPAC: Report to the Congress: Medicare payment policy. Section 2B: physician services: assessing payment adequacy and updating payments. [Accessed January 21, 2010]; http://www.medpac.gov/chapters/Mar08_Ch02b.pdf.
- 20.MedPAC: Medicare Payment Advisory Commission. Medicare physician payment rates compared to rates paid by the average private insurer, 1999–2001. [Accessed January 21, 2010]; http://www.medpac.gov/publications/contractor_reports/Aug03_PhysPayRates(cont)Rpt.pdf.
- 21.Centers for Medicare&Medicaid Services. National health expenditure data: historical. [Accessed January 21, 2010]; http://www.cms.hhs.gov/NationalHealthExpendData/02_NationalHealthAccountsHistorical.asp#TopOfPage.
- 22.Lasser KE, Woolhandler S, Himmelstein DU. Sources of U.S. physician income: the contribution of government payments to the specialist-generalist income gap. J Gen Intern Med. 2008;23(9):1477–1481. doi: 10.1007/s11606-008-0660-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Government Accountability Office. Report to the Honorable Paul Ryan, House of Representatives: federal employees health benefits program: competition and other factors linked to wide variation in health care prices. [Accessed January 21, 2010]; http://www.gao.gov/new.items/d05856.pdf.
- 24.American Council on Graduate Medical Education. Statement of justification/impact for the final approval of common standards related to resident duty hours. [Accessed January 21, 2010]; http://www.acgme.org/DutyHours/impactStatement.pdf.
- 25.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. chap 7. Cambride, MA: MIT Press; 2002. [Google Scholar]
- 26.Rones PL, Ilg RE, Gardner JM. Trends in hours of work since the mid-1970s. Mon Labor Rev. 1997;120(4):3–14. [Google Scholar]
- 27.Bureau of Labor Statistics. Household data annual averages: Table 23: persons at work by occupation, sex, and usual full- or part-time status. [Accessed January 21, 2010]; http://www.bls.gov/cps/cpsaat23.pdf.
- 28.McGuire TG, Pauly MV. Physician response to fee changes with multiple payers. J Health Econ. 1991;10(4):385–410. doi: 10.1016/0167-6296(91)90022-f. [DOI] [PubMed] [Google Scholar]
- 29.Pham HH, Devers KJ, May JH, Berenson R. Financial pressures spur physician entrepreneurialism. Health Aff (Millwood) 2004;23(2):70–81. doi: 10.1377/hlthaff.23.2.70. [DOI] [PubMed] [Google Scholar]
- 30.Bodenheimer T, Berenson RA, Rudolf P. The primary care-specialty income gap: why it matters. Ann Intern Med. 2007;146(4):301–306. doi: 10.7326/0003-4819-146-4-200702200-00011. [DOI] [PubMed] [Google Scholar]
- 31.US Government Accountability Office. Testimony before the Subcommittee on Health, Committee on Energy and Commerce, House of Representatives: Medicare physician payments: trends in service utilization, spending, and fees prompt consideration of alternative payment approaches. [Accessed January 21, 2010]; http://www.gao.gov/new.items/d061008t.pdf.
- 32.Landon BE, Reschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians. JAMA. 2003;289(4):442–449. doi: 10.1001/jama.289.4.442. [DOI] [PubMed] [Google Scholar]
- 33.Blumenthal D. New steam from an old cauldron: the physician-supply debate. N Engl J Med. 2004;350(17):1780–1787. doi: 10.1056/NEJMhpr033066. [DOI] [PubMed] [Google Scholar]
- 34.Mechanic D. Physician discontent: challenges and opportunities. JAMA. 2003;290(7):941–946. doi: 10.1001/jama.290.7.941. [DOI] [PubMed] [Google Scholar]
- 35.Zuger A. Dissatisfaction with medical practice. N Engl J Med. 2004;350(1):69–75. doi: 10.1056/NEJMsr031703. [DOI] [PubMed] [Google Scholar]
- 36.Grossman JM, Reed MC. Clinical Information Technology Gaps Persist Among Physicians. Issue Brief No. 106. Washington, DC: Center for Studying Health System Change; 2006. [PubMed] [Google Scholar]
- 37.Isaacs SL, Jellinek PS, Ray WL. The independent physician: going, going…. N Engl J Med. 2009;360(7):655–657. doi: 10.1056/NEJMp0808076. [DOI] [PubMed] [Google Scholar]
- 38.Physician Characteristics and Distribution in the US. Chicago, IL: American Medical Association; 1999. [Google Scholar]
- 39.Iglehart J. Reform and the health care workforce: current capacity, future demand. [Accessed January 21, 2010]; doi: 10.1056/NEJMp0909521. Published October 21, 2009 http://healthcarereform.nejm.org/?p=2129&query=TOC. [DOI] [PubMed]