Abstract
Pediatricians understand their role as promoting both the physical and mental health of children from birth until adulthood. Within the context of this long-term relationship, parents approach clinicians to address a full range of behavioral concerns ranging from variations of normal development to major mental illness. In this commentary that builds upon the earlier manuscripts in this collection, we explore the pediatrician’s role in mental health care through the example of attention-deficit hyperactivity disorder (ADHD). ADHD is an ideal prototype for the exploration of partnership in mental health care because ADHD is the most common neurobehavioral disorder in childhood, it is commonly treated in primary care settings, multiple evidence-based treatments exist, personal values strongly influence the acceptability of treatment, treatment adherence is often poor, and effective treatment relies on the collaboration of pediatricians with families, schools, and the mental health system. Through the use of the Chronic Care Model for Child Health that emphasizes the importance of optimizing and coordinating systems of care for effective partnership, the following manuscript reviews the challenges and opportunities for pediatricians partnering with families and schools to address mental health problems. Strategies highlighted in the preceding papers are discussed within the context of this model.
Keywords: Pediatrics, Partnership, Mental health
Introduction
Pediatricians broadly define their role as focusing on health promotion and disease prevention in collaboration with parents, other health professionals, schools, mental health systems, and the broader community (Hagan, Shaw, & Duncan, 2008). This perspective is particularly relevant to developmental, behavioral, and mental health concerns that impact children in multiple settings and often require resources from multiple systems to be effectively treated. Such efforts are especially important, given that more than 20% of children and adolescents have mental health problems, the mental health of family members impacts children’s behavioral health, and emotional problems are more common among those with chronic illness, a population central to many pediatric practices (Committee on School Health, 2004; Lesesne, Visser, & White, 2003; Weiland, Pless, & Roghmann, 1992). The manuscripts in this collection have discussed the impact of diverse conditions including ADHD, childhood cancer, and anxiety on parents, siblings, and affected children. The following paragraphs highlight the role of pediatricians as care coordinators, treating multiple members of the same family and working with experts from the health, mental health, and school systems to minimize the impact of mental health problems. Partnership is central to the success of these efforts.
Among conditions impacting mental health for children, attention-deficit/hyperactivity disorder (ADHD) is an ideal prototype to examine how pediatricians partner with families, schools, and other systems of care. ADHD is the most common neuro-developmental disorder in children and adolescents with prevalence estimates in the United States between 3 and 16% depending upon the sample and measurement techniques used (U.S. Department of Health and Human Services, 1999; American Academy of Pediatrics [AAP], 2000). Treatment is especially important since those affected often have decreased self-esteem, struggle with interpersonal relationships, and have lower academic achievement including reduced rates of high school graduation (Loe & Feldman, 2007). For ADHD, stimulant medication and behavior therapy (at home and school), and school-based interventions have been widely studied, shown to improve symptoms, and are currently recommended, alone or in combination, as the first-line treatment (AAP, 2001; Jensen et al., 2001; MTA Cooperative Group, 1999, 2004; Pliszka et al., 2006). Because ADHD is seen as a medical disorder, decisions are often negotiated between pediatricians and families. While the care of children with ADHD is distributed across multiple settings, prior work has shown that physicians are a primary source of information on ADHD, the majority of visits for ADHD and most medication prescriptions come from pediatric primary care, and ADHD is the most common behavioral complaint to pediatricians (Bussing, Schoenberg, & Perwien, 1998; Leslie & Wolraich, 2007; Rushton, Fant, & Clark, 2004).
National guidelines from the American Academy of Pediatrics (AAP) stress that pediatricians treating ADHD should partner with families in consultation with schools to jointly determine a treatment plan (AAP, 2000, 2001). This family-centered approach is necessary in ADHD and other prevalent mental health conditions since cultural differences as well as personal values shape attitudes regarding the recognition of abnormal behavior (Achenbach et al., 1990; Crijnen, Achenbach, & Verhulst, 1999), decisions to seek help (Eiraldi, Mazzuca, Clarke, & Power, 2006), and treatment selection (Bussing, Gary, Mills, & Wilson Garvan, 2003; dosReis et al., 2003). For example, African Americans have been found to be more likely to prefer behavior therapy to medication than whites even if they receive care in the same setting (dosReis et al., 2003). This preference, at least in part, reflects fears regarding later drug abuse, a general mistrust of the medical system, and concerns regarding the stigma of having a behavioral disorder (dosReis et al., 2006; Olaniyan et al., 2007). In addition, some families may be more likely to view ADHD initially as a parenting or discipline as opposed to a biomedical problem (Olaniyan et al., 2007). Alternatively, some families see ADHD as primarily a problem only within the school setting and prioritize school-based interventions (Leslie, Plemmons, Monn, & Palinkas, 2007). These studies suggest that partnership between well-informed families, clinicians, and schools informs treatment decisions and improves the acceptability of and adherence to ADHD treatment.
Recent studies focused on the outcomes of ADHD treatment underscore the importance of assembling a team that incorporates members of the health, school, and mental health systems in order to best help affected children. Follow-up 6 and 8 years post-enrollment in The National Institute of Mental Health (NIMH) Collaborative Multisite Multimodal Treatment Study of Children with ADHD (MTA), the largest randomized trial of ADHD treatment conducted to date, found that while initial symptom trajectories on treatment predicted symptoms in the long-term for children with combined type ADHD, significant impairment persisted in adolescence (Molina et al., 2009). This work is supported by studies in real-world practice settings that indicate while symptoms respond to treatment, functional impairments including peer relationships, academic performance, and organizational skills fail to improve (Epstein et al., 2010.). Since treatment is generally targeted to symptoms, these results have profound implications for treating ADHD in childhood: innovative strategies, likely encompassing multiple systems and individuals involved in children’s lives, may be needed if health care is to minimize the burden of ADHD on the lives of families as children age. The work by Power et al. (2010) presented in this collection provides one model for how pediatricians, psychologists, and schools may partner in ADHD to improve outcomes with at risk families.
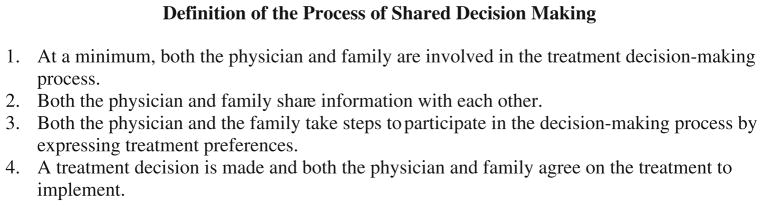
Framework: The Chronic Care Model
The Care Model for Child Health, modified by the National Initiative for Children’s Healthcare Quality (NICHQ) from the Wagner et al. (2000) Chronic Care Model, provides a conceptual framework for developing interconnected systems to promote childhood mental health (see Fig. 1). While this model is primarily focused on the doctor–patient–family partnership, it also highlights the role of community resources such as schools. Strengthening the areas specified in the model may be an ideal way to assemble the type of partnerships that may ultimately be able to guide sustained and coordinated intervention to address child mental health needs. As described above, findings from the long-term follow-up of children in the MTA Study highlight the importance of treating ADHD as a chronic illness requiring sustained intervention. Consistent with this finding, the Care Model for Child Health is based on the premise that the usual exchange of symptoms and diagnosis leading to a defined, time-limited treatment does not fit the complexities of care for a chronic disorder. In addition, the model recognizes that ability to self-manage a chronic disorder develops with age and maturity and parents act as an important proxy for the child throughout most of childhood. Thus, patient-centered care for pediatric patients is best defined as family-centered care.
Fig. 1.
National initiative for children’s healthcare quality (NICHQ) care model for child health in a medical home
Similar to the models described by Shapiro et al. in their introduction to this collection that emphasize the importance of partnership with the community, the Care Model features three clearly identified and overlapping domains: the health system, patient/family, and community, including schools (Shapiro, DuPaul, Barnabas, Benson, & Slay 2010). With examples from work on ADHD, the following paragraphs address distinct aspects of the Care Model as they apply to the delivery of mental health services to children. Through this review of the Care Model, we illustrate both the scope of the problem of providing comprehensive mental health care to children and the importance of strategies to develop partnerships to maintain patient, family, and school engagement in care.
Elements of the Chronic Care Model and Their Implications for Child Mental Health
The Informed, Activated Patient/Family
The Care Model revolves around the informed, activated family as the center of interactions that ultimately influence health outcomes. Multiple studies provide an evidence-base for this approach. For example, results from family medicine indicate that patients arriving at visits having received communication skills training are more likely to adhere to behavioral treatments (Cegala, Marinelli, & Post, 2000). Similarly, in the pediatric setting, parent training has decreased inappropriate use of antibiotics in the emergency department (McWilliams, Jacobson, Van Ho-uten, Naessens, & Ytterberg, 2008). Specific to the care of children with ADHD, Power et al. (2010) in this collection demonstrate that the quantity of telephone contact between families and pediatric clinicians, a setting to both activate and inform families, predicts treatment initiation for affected children.
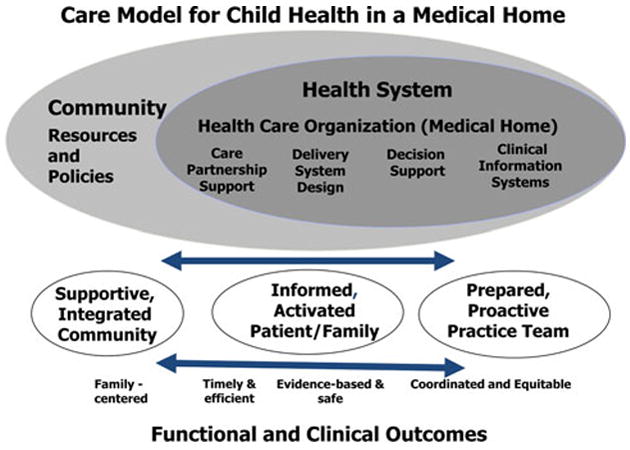
More broadly, the literature on shared decision making (SDM) has described a set of approaches that create and maintain a high level of partnership directed at achieving families’ treatment goals. For the following discussion, we will use the most commonly cited definition of SDM published by Charles (see Fig. 2) that considers SDM in the context of medical encounters and is relevant to chronic mental health conditions such as ADHD (Charles, Gafni, & Whelan, 1997; Charles, Gafni, & Whelan, 1999). SDM is distinguished from both paternalistic models in which practitioners make treatment decisions and convey them to families and informed patient-models in which patients and families reach their own healthcare decisions with information from clinicians or other sources (Charles et al., 1999). Unlike paternalistic and informed approaches that focus primarily on medical facts, SDM emphasizes the exchange of personal in addition to medical information (Charles et al., 1999), an aspect of care particularly relevant to value-laden mental health problems.
Fig. 2.
The process of shared decision making
A primary focus of work to promote SDM has been the development of decision aids, defined as interventions to help people make specific and deliberative choices among options by providing information about the options and outcomes that is relevant to a person’s health status (Barry, 2002; O’Connor et al., 2003). These tools are designed to both bolster knowledge and clarify values through questionnaires, instructional videos, and/or coaching from a trained health professional. Meta-analyses of controlled randomized trials indicate that these tools are effective in improving knowledge and realistic expectations, enhancing participation in decision making, decreasing decisional conflict (uncertainty), increasing the proportion of people able to reach a decision, and improving agreement between values and choice (O’Connor et al., 2007). Based on the effectiveness of SDM tools, the World Health Organization Health Evidence Network has concluded that strategies to integrate these tools into practice for diverse populations should be developed (O’Connor & Stacey, 2005). Decision aids support the goals articulated by the NIMH in their report “Bridging Science and Service” which stresses the importance of developing approaches to better incorporate patient/consumer preferences explicitly into treatment protocols (National Advisory Mental Health Council Clinical Treatment and Services Research Workgroup, 1999). Despite this emphasis, few decision aids have been developed for pediatrics, and the tools developed have not been well integrated into pediatric practice or across systems caring for children. Given this gap in translating knowledge into practice, study is needed to determine optimal strategies for using decision aids to improve decision making, promote adherence, and provide a shared approach across settings in which children are served, including the home and school (O’Connor & Stacey, 2005; O’Connor et al., 2003). In pediatrics, the complexity of incorporating children who become increasingly autonomous with age as well as their parents/guardians into decision making requires additional consideration.
The Prepared, Proactive Practice Team
When parents approach pediatricians to address mental health concerns, they meet well-meaning practitioners who historically have not received robust training in pediatric mental health. As a profession, pediatrics has increasingly confronted this training gap. In particular, to effectively meet the needs of an informed and activated family, the AAP Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health developed a list of competencies for primary care pediatricians treating affected children (Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health, 2009). For pediatricians, a first step in being proactive is working with families to establish healthy lifestyles and prevent the escalation of social, emotional, or behavioral problems typical throughout childhood (Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health, 2009). This focus on prevention parallels the goals of the Family Check-Up described earlier in this collection (Stormshak, Fosco, & Dishion, 2010). In addition, the report argues that pediatricians must develop skills to help children with mental health problems who lack a formal diagnosis, the largest group of children with mental illness seen in primary care and also a group reflective of the population with mental health concerns in schools. As the work of Alderfer and Hodges in this collection shows, siblings of chronically ill children are one group that needs this support (Alderfer & Hodges, 2010).
Specific areas emphasized in the AAP report include developing a better understanding of how to establish partnerships across systems of mental health care delivery including schools; developing clinical skills to treat those with mental health conditions such as ADHD, anxiety, depression, and substance abuse; developing a better understanding of the science underlying the treatment of mental illness; and building skill sets that focus on interpersonal and communication skills, professionalism, and partnerships across systems. The article by Weems et al. 2010) highlights one potential mechanism by which schools could effectively partner with families and health care professionals to identify children and adolescents with anxiety, another chronic pediatric disorder. Efforts to address test anxiety in the school setting could be linked to primary care and mental health comanagement of related anxiety and depression, particularly for those youth who are severely impaired by their symptoms.
In addition, mechanisms for reaching families that are often more difficult to engage in care need to be developed. For these families, the engagement issue often extends across settings to include the school and the pediatric office. Two of the interventions in 2010, Power et al. telephone intervention in the pediatric office setting and Stormshak et al. (2010) Family Check-up Model, based in the school setting, provide examples of simple and effective interventions for engaging families more directly in service provision. Finding mechanisms for copartnering to improve engagement could be an important strategy in the comanagement of youth with conditions that affect health, mental health, and school participation and performance.
A Supportive, Integrated Community
The AAP has emphasized that competence in treating mental health problems depends upon collaboration within primary care offices and between primary care clinicians and educators, as well as professionals in any other systems in which an individual child is served including mental health specialists, case managers, social service workers, and juvenile justice staff (Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health, 2009). More broadly, success in treating mental health problems depends upon pediatricians understanding prevalent concerns in the community, ensuring that both parents and children receive the support needed to address the challenges of treating mental illness, and determining how best to provide that support through partnerships with other professionals. These relationships are especially important because chronic medical conditions impact children daily at home and school, while contact with the medical system is often far less frequent.
The example of ADHD is particularly helpful in understanding the importance of the community to children’s mental health. For example, in ADHD, many believe that poor behavior results from a parenting as opposed to a biomedical problem (Olaniyan et al., 2007). Such attitudes and the stigma they engender can lead families to avoid seeking medical help and receiving treatment for ADHD (Eiraldi et al., 2006). When parents do begin to consider medical help to address their child’s behavior, a high level of stress is common (Brinkman et al., 2009). In this setting, pediatricians frequently will refer families to support groups such as Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD) for both emotional support and education. Unfortunately, fewer support groups are available in urban settings that often have an increased burden of mental health problems. To augment services, efforts are underway in many areas to develop additional support groups for families in accessible settings; these may include schools, neighborhood churches, or community service organizations for families in underserved communities.
Pediatricians also have longstanding relationships with schools that include providing assessment forms to document health for enrolled children, established systems to assist school nurses in administering medication or other treatments to children at schools, and they support school nurses, psychologists, and teachers in preventing and addressing behavior problems. In the setting of ADHD, teachers regularly look to pediatricians to diagnose ADHD. At the same time, pediatricians look to teachers to complete behavioral rating scales to assist in the diagnostic process and monitor the response to medication. To more broadly address the behavioral health needs of children outside of the office setting, the AAP Committee on School Health has identified three areas for intervening to improve school health: (1) programs targeted to all students to promote resilience and foster the engagement of children and their families with school; (2) for those with a specific impairment, but who continue to function in the school settings, targeted behavioral interventions; and (3) a coordinated multidisciplinary team including the pediatrician for more severely affected children (Committee on School Health, 2004). To maximize the effectiveness and comprehensiveness of care provided, the AAP conceptualizes these school-based services as an extension of the “medical home” and has prioritized the integration of these two systems of care (Committee on School Health, 2004). However, work needs to be done to address barriers to integrating these two systems, including the challenges of timely information sharing within the context of confi-dentiality requirements under the Family Educational Rights and Privacy Act (FERPA) and the Health Insurance Portability and Accountability Act (HIPAA). In addition, the cultural differences in approach (e.g. strength-based versus diagnosis-based, educational codes versus medical codes), schedules, and missions must also be addressed.
Key Features of an Improved Delivery System
Care Partnership Support
Since chronic illness affects children daily but medical encounters are infrequent, the development of tools and educational programs to help patients and families manage children’s medical problems has increasingly been recognized as an important part of pediatric health care. In general pediatric practice, these tools have been much more thoroughly developed for physical as opposed to mental health conditions in children. In asthma, clinicians and families jointly develop care plans that specify daily treatment regimens as well as how to adjust therapy during flares or if symptoms arise with exercise (Loe & Feldman, 2007). Office-based education accompanies the review of the management plan. In the setting of asthma, such approaches have been shown to improve outcomes in adult settings (Lahdensuo et al., 1996). Research is needed to develop and test the benefit of teaching and self-management tools on outcomes in the treatment of childhood mental health problems. Also, the integration of these tools across primary care and schools needs further study.
Both Weems et al. (2010) paper on test anxiety prevention and intervention programs in school settings and Stormshak et al. (2010) Family Check-up Model also point out the possibility of providing family and/or self-management support about a mental health condition within schools. While not specific to ADHD, both demonstrate that schools are natural settings for delivering services to youth and families. The development of these types of programs and the ability to integrate those with interventions in primary care settings would promote better family and youth self-management skills and should be the focus of further research.
Delivery System Design/Care Coordination
The AAP has stressed the importance of pediatricians coordinating health care across multiple systems including schools, especially for children with chronic health conditions. As identified by the AAP, the tasks involved in this process include collaboratively planning treatment, monitoring outcomes and resource use, coordinating visits with other subspecialists or professionals, organizing care to avoid duplication of diagnostic tests and services, sharing information with the family and across systems of care, facilitating access to care, as well as the development and ongoing refinement of care plans (Committee on Children With Disabilities, 1999). Research suggests that effective care coordination improves outcomes for children with special health care needs, defined as those “with a chronic physical, behavioral, or emotional condition who require health and related services of a type or amount beyond that required by children generally” (Newacheck et al., 1998). Specifically, receiving “adequate” care coordination has been associated with improved satisfaction, decreased problems with referral to specialists, fewer emergency department visits, and fewer missed school days. In addition, with care coordination, out-of-pocket health care costs for families were reduced, and fewer parents had to stop work or decrease work hours (Turchi et al., 2009).
Despite these impressive findings, many pediatricians struggle to find time to manage care across systems. Recent work in ADHD has defined many of the challenges in care coordination: (1) a lack of consensus on which professional from what setting (e.g. primary care, mental health, school) is ultimately accountable for the success of treatment; (2) turnover of mental health professionals and teachers limiting the development of long-term collaboration; (3) a lack of resources to devote to the process; (4) distrust and blame when relationships across systems are not productive; and (5) a general lack of support from employers, systems, friends, or families to engage in collaborative care (Guevara et al., 2005). Given these barriers, many practices enlist members of their nursing and clerical staff to help in this process with unreimbursed costs for a practice of between $22,800 and $33,000 per year (Antonelli & Antonelli, 2004). To reimburse practices for this financial burden, many have called for the development of new mechanisms to support this process.
To address these concerns, practice models could increasingly incorporate pediatric psychologists or school psychologists within the primary care practice. These skilled professionals have the knowledge, background, and experience to understand both issues arising in the pediatrician’s office and the nature of partnership needed in schools, a perspective not traditionally part of pediatric training. The ability of psychologists to bridge primary care pediatrics and schools for the benefit of children and their families is demonstrated by the Partnering to Achieve School Success (PASS) Program featured in this collection (Power et al., 2010). Equally important, these individuals carry the necessary licensure credentials to provide the reimbursement required to sustain a private practice primary care office.
Decision Support and Clinical Information Systems
For pediatric clinicians managing complex conditions, gathering information then synthesizing it with the growing body of medical evidence during office-based encounters lasting as little as 15 min or less represents an ongoing challenge. Tools to support information gathering and decision making are increasingly available to help. The most widely studied toolkit for any mental health condition in pediatric primary care is the AAP/National Initiative for Children’s Healthcare Quality (NICHQ) toolkit for ADHD (AAP, 2000, 2001). Included are educational materials for parents regarding the condition and its treatment as well as tools to assist in the diagnosis, assess comorbidities, assess both symptom severity and impairment on treatment, and communicate across school and primary care settings. Early scholarship demonstrated the feasibility of using such tools in varied pediatric practice settings (Leslie, Weckerly, Plemmons, Landsverk, & Eastman, 2004; Polaha, Cooper, Meadows, & Kratochvil, 2005; Rushton et al., 2004), and more recent work suggests that clinicians using these tools may be able to work with families to markedly reduce children’s symptoms (Epstein et al., 2005). This work demonstrates the potential value of tools to strengthen partnerships in providing mental health care.
A growing body of literature in pediatrics has demonstrated benefits of health information technology in delivering decision support. In pediatrics, more than 20% of primary practices already have electronic health records (EHRs) in place and the proportion is growing (Kemper, Uren, & Clark, 2006). Our own work on immunization demonstrated improved outcomes for children cared for using these systems (Fiks, Grundmeier, Biggs, Localio, & Alessandrini, 2007). In ADHD, our group has developed structured order sets and visit templates to facilitate evidence-based care and collaboration between pediatric clinicians, families, and schools (see Fig. 3). Formal evaluation of such systems is underway, and their benefit should be increasingly understood in coming years. However, while these tools are structured to improve the quality of care delivered to children, they play only a small role in sustaining the ongoing partnership central to delivering optimal pediatric mental health care.
Fig. 3.
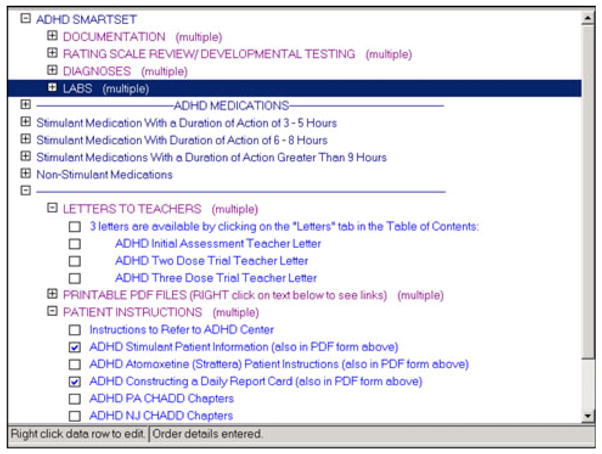
Electronic health record-based order set for ADHD to promote evidence-based care and partnership between clinicians, families, and schools
Perhaps the greatest promise of health information technology for mental health care is opening and maintaining lines of communication between the multiple systems involved in delivering mental health services and the family. Work thus far has centered on connecting pediatricians with families. Electronic health record-linked patient portals, tools that allow families to securely communicate with their clinicians and view their children’s health information over the internet, are innovative systems to facilitate the integration of patient preferences and goals into practice and support SDM on a large scale. While only 2.7% of the population now uses personal health records or patient portals, adoption is increasing, and public interest is high (Westin, 2008). Additionally, parents are receptive to electronic communication both inside and outside the medical office (Gerstle, 2004; Kleiner, Akers, Burke, & Werner, 2002; Rosen & Kwoh, 2007).
Results published to date demonstrate that despite fears that computers might compromise communication in the office setting, the use of health information technology has been associated with improved patient satisfaction, communication about health issues, and comprehension of decisions made during clinical encounters (Hsu et al., 2005). In addition, these systems have been used to capture information on families’ health concerns and formally structure the delivery of healthcare around them (Biondich, Downs, Anand, & Carroll, 2005; Porter, Forbes, Feldman, & Goldmann, 2006). Once data is captured on information relevant to care such as the preferences and goals of families, these systems are capable of delivering this content to clinicians at the appropriate stage in their workflow and changing practitioner performance (Garg et al., 2005). Since content may be updated over time, these systems can adapt to changes such as the known evolution in families’ preferred ADHD treatment over time or new clinical practice guidelines (Jensen et al., 2007; Leslie et al., 2007). Further, well-established approaches exist to maximize the effectiveness of these systems (Bates et al., 2003; Osheroff, Pifer, Teich, Sittig, & Jenders, 2005). However, while these types of tools will improve communication between parents and clinicians, they still do not fully address communication issues between the health system, community partners, and the schools. Effectively incorporating school professionals and those from other systems involved in a child’s care should be the focus of future work in this area.
Conclusion
Over the past decade, major breakthroughs have occurred supporting the partnership between families, pediatricians, and other professionals for children affected by mental health problems. Resources are increasingly available to help families become “activated” participants in care, and models for care coordination across health, school, and mental health systems are emerging from the literature on children with special healthcare needs and research on partnership models. For clinicians, a focus on improving communication skills is also likely to benefit children. In addition, as illustrated by the example of ADHD, toolkits developed and promulgated nationally are beginning to influence mental health outcomes. Approaches using health information technology to regularly elicit families’ preferences and goals and maintain open communication across systems of care should help guide coordinated care toward goals valued by families. For pediatricians and school professionals, many of these children with mental health problems will lack a formal medical diagnosis or may not qualify for a 504 plan or special education-developing, testing, and funding interventions for these at risk children, like those described by Weems et al. (2010), and Alderfer and Hodges (2010) will be critical. The impact of combining all of these approaches on outcomes for children with mental health problems will be increasingly well defined over the next 10 years.
Acknowledgments
We thank Cayce Hughes, MPH for his help in assembling this manuscript.
This paper was written with the support from Award Number K23HD059919 from the Eunice Kennedy Shriver National Institute of Children Health & Human Development (Dr. Fiks) and Award Number RC1 HL100546 from the National Heart Lung & Blood Institute (Dr. Leslie). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Alexander G. Fiks, Email: Fiks@email.chop.edu, The Pediatric Generalist Research Group & Center for Biomedical Informatics, University of Pennsylvania School of Medicine, Philadelphia, PA, USA. Department of Pediatrics, University of Pennsylvania School of Medicine, Philadelphia, PA, USA. The Children’s Hospital of Philadelphia, 34th Street and Civic Center Boulevard, Philadelphia, PA 19104, USA
Laurel K. Leslie, Aligning Researchers and Communities for Health, Boston, MA, USA. Tufts Medical Center/Floating Hospital for Children, Boston, MA, USA
References
- Achenbach TM, Bird HR, Canino G, Phares V, Gould MS, Rubio-Stipec M. Epidemiological comparisons of Puerto Rican and U.S. mainland children: Parent, teacher, and self-reports. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29(1):84–93. doi: 10.1097/00004583-199001000-00014. [DOI] [PubMed] [Google Scholar]
- Alderfer MA, Hodges J. Supporting siblings of children with cancer: A need for family-school partnerships. School Mental Health. 2010 doi: 10.1007/s12310-010-9027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics. Clinical practice guideline: Diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000;105(5):1158–1170. doi: 10.1542/peds.105.5.1158. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. Clinical practice guideline: Treatment of the school-aged child with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108(4):1033–1044. doi: 10.1542/peds.108.4.1033. [DOI] [PubMed] [Google Scholar]
- Antonelli RC, Antonelli DM. Providing a medical home: The cost of care coordination services in a community-based, general pediatric practice. Pediatrics. 2004;113(5):1522–1528. [PubMed] [Google Scholar]
- Barry MJ. Health decision aids to facilitate shared decision making in office practice. Annals of Internal Medicine. 2002;136(2):127–135. doi: 10.7326/0003-4819-136-2-200201150-00010. [DOI] [PubMed] [Google Scholar]
- Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Ten commandments for effective clinical decision support: Making the practice of evidence-based medicine a reality. Journal of the American Medical Informatics Association. 2003;10(6):523–530. doi: 10.1197/jamia.M1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biondich PG, Downs SM, Anand V, Carroll AE. Automating the recognition and prioritization of needed preventive services: Early results from the CHICA system. AMIA Annual Symposium of Proceedings; 2005. pp. 51–55. [PMC free article] [PubMed] [Google Scholar]
- Brinkman WB, Sherman SN, Zmitrovich AR, Visscher MO, Crosby LE, Phelan KJ, et al. Parental angst making and revisiting decisions about treatment of Attention-Deficit/Hyperactivity Disorder. Pediatrics. 2009;124(2):580–589. doi: 10.1542/peds.2008-2569. [DOI] [PubMed] [Google Scholar]
- Bussing R, Gary FA, Mills TL, Wilson Garvan C. Parental explanatory models of ADHD: Gender and cultural variations. Social Psychiatry and Psychiatric Epidemiology. 2003;38(10):563–575. doi: 10.1007/s00127-003-0674-8. [DOI] [PubMed] [Google Scholar]
- Bussing R, Schoenberg NE, Perwien AR. Knowledge and information about ADHD: Evidence of cultural differences among African-American and white parents. Social Science and Medicine. 1998;46(7):919–928. doi: 10.1016/s0277-9536(97)00219-0. [DOI] [PubMed] [Google Scholar]
- Cegala DJ, Marinelli T, Post D. The effects of patient communication skills training on compliance. Archives of Family Medicine. 2000;9(1):57–64. doi: 10.1001/archfami.9.1.57. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango) Social Science and Medicine. 1997;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: Revisiting the shared treatment decision-making model. Social Science and Medicine. 1999;49(5):651–661. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- Committee on Children With Disabilities. Care coordination: Integrating health and related systems of care for children with special health care needs. Pediatrics. 1999;104(4):978–981. [PubMed] [Google Scholar]
- Committee on Psychosocial Aspects of Child, Family Health, Task Force on Mental Health. The future of pediatrics: Mental health competencies for pediatric primary care. Pediatrics. 2009;124(1):410–421. doi: 10.1542/peds.2009-1061. [DOI] [PubMed] [Google Scholar]
- Committee on School Health. School-based mental health services. Pediatrics. 2004;113(6):1839–1845. doi: 10.1542/peds.113.6.1839. [DOI] [PubMed] [Google Scholar]
- Crijnen AAM, Achenbach TM, Verhulst FC. Problems reported by parents of children in multiple cultures: The child behavior checklist syndrome constructs. American Journal of Psychiatry. 1999;156(4):569–574. doi: 10.1176/ajp.156.4.569. [DOI] [PubMed] [Google Scholar]
- dosReis S, Butz A, Lipkin P, Anixt J, Weiner C, Chernoff R. Attitudes about stimulant medication for Attention-Deficit/Hyperactivity Disorder among African American families in an inner city community. The Journal of Behavioral Health Services and Research. 2006;33(4):423–430. doi: 10.1007/s11414-006-9038-y. [DOI] [PubMed] [Google Scholar]
- dosReis S, Zito JM, Safer DJ, Soeken KL, Mitchell JW, Jr, Ellwood LC. Parental perceptions and satisfaction with stimulant medication for attention-deficit hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics. 2003;24(3):155–162. doi: 10.1097/00004703-200306000-00004. [DOI] [PubMed] [Google Scholar]
- Eiraldi R, Mazzuca L, Clarke A, Power T. Service utilization among ethnic minority children with ADHD: A model of help-seeking behavior. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33(5):607–622. doi: 10.1007/s10488-006-0063-1. [DOI] [PubMed] [Google Scholar]
- Epstein RM, Franks P, Fiscella K, Shields CG, Meldrum SC, Kravitz RL, et al. Measuring patient-centered communication in patient-physician consultations: Theoretical and practical issues. Social Science and Medicine. 2005;61(7):1516–1528. doi: 10.1016/j.socscimed.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Epstein JN, Langberg JM, Lichtenstein PK, Altaye M, Brinkman WB, House K, et al. Attention-Deficit/Hyperactivity Disorder outcomes for children treated in community-based pediatric settings. Archives of Pediatrics and Adolescent Medicine. 2010;164(2):160–165. doi: 10.1001/archpediatrics.2009.263. [DOI] [PubMed] [Google Scholar]
- Fiks AG, Grundmeier RW, Biggs LM, Localio AR, Alessandrini EA. Impact of clinical alerts within an electronic health record on routine childhood immunization in an urban pediatric population. Pediatrics. 2007;120(4):707–714. doi: 10.1542/peds.2007-0257. [DOI] [PubMed] [Google Scholar]
- Garg AX, Adhikari NKJ, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: A systematic review. JAMA. 2005;293(10):1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- Gerstle RS. E-mail communication between pediatricians and their patients. Pediatrics. 2004;114(1):317–321. doi: 10.1542/peds.114.1.317. [DOI] [PubMed] [Google Scholar]
- Guevara JP, Feudtner C, Romer D, Power T, Eiraldi R, Nihtianova S, et al. Fragmented care for inner-city minority children with attention-deficit/hyperactivity disorder. Pediatrics. 2005;116(4):e512–e517. doi: 10.1542/peds.2005-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan JF, Shaw JS, Duncan PM. Bright futures: Guidelines for health supervision of infants, children, and adolescents. 3. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- Hsu J, Huang J, Fung V, Robertson N, Jimison H, Frankel R. Health information technology and physician-patient interactions: Impact of computers on communication during outpatient primary care visits. Journal of the American Medical Informatics Association. 2005;12(4):474–480. doi: 10.1197/jamia.M1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Arnold LE, Swanson JM, Vitiello B, Abikoff HB, Greenhill L, et al. 3-Year follow-up of the NIMH MTA Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(8):989–1002. doi: 10.1097/CHI.0b013e3180686d48. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Hinshaw SP, Swanson JM, Greenhill LL, Conners CK, Arnold LE, et al. Findings from the NIMH Multimodal Treatment Study of ADHD (MTA): Implications and applications for primary care providers. Journal of Developmental and Behavioral Pediatrics. 2001;22(1):60–73. doi: 10.1097/00004703-200102000-00008. [DOI] [PubMed] [Google Scholar]
- Kemper AR, Uren RL, Clark SJ. Adoption of electronic health records in primary care pediatric practices. Pediatrics. 2006;118(1):e20–e24. doi: 10.1542/peds.2005-3000. [DOI] [PubMed] [Google Scholar]
- Kleiner KD, Akers R, Burke BL, Werner EJ. Parent and physician attitudes regarding electronic communication in pediatric practices. Pediatrics. 2002;109(5):740–744. doi: 10.1542/peds.109.5.740. [DOI] [PubMed] [Google Scholar]
- Lahdensuo A, Haahtela T, Herrala J, Kava T, Kiviranta K, Kuusisto P, et al. Randomised comparison of guided self management and traditional treatment of asthma over one year. BMJ. 1996;312(7033):748–752. doi: 10.1136/bmj.312.7033.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesesne CA, Visser SN, White CP. Attention-Deficit/Hyperactivity Disorder in school-aged children: Association with maternal mental health and use of health care resources. Pediatrics. 2003;111(5):1232–1237. [PubMed] [Google Scholar]
- Leslie LK, Plemmons D, Monn AR, Palinkas LA. Investigating ADHD treatment trajectories: Listening to families’ stories about medication use. Journal of Developmental and Behavioral Pediatrics. 2007;28(3):179–188. doi: 10.1097/DBP.0b013e3180324d9a. [DOI] [PubMed] [Google Scholar]
- Leslie LK, Weckerly J, Plemmons D, Landsverk J, Eastman S. Implementing the American Academy of Pediatrics Attention-Deficit/Hyperactivity Disorder diagnostic guidelines in primary care settings. Pediatrics. 2004;114(1):129–140. doi: 10.1542/peds.114.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie LK, Wolraich ML. ADHD service use patterns in youth. Ambulatory Pediatrics. 2007;7(1, Supplement 1):107–120. doi: 10.1016/j.ambp.2006.05.002. [DOI] [PubMed] [Google Scholar]
- Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. Ambulatory Pediatrics. 2007;7(1, Supplement 1):82–90. doi: 10.1016/j.ambp.2006.05.005. [DOI] [PubMed] [Google Scholar]
- McWilliams DB, Jacobson RM, Van Houten HK, Naessens JM, Ytterberg KL. A program of anticipatory guidance for the prevention of emergency department visits for ear pain. Archives of Pediatrics and Adolescent Medicine. 2008;162(2):151–156. doi: 10.1001/archpediatrics.2007.30. [DOI] [PubMed] [Google Scholar]
- Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(5):484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999;56(12):1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: 24-month outcomes of treatment strategies for Attention-Deficit/Hyper-activity Disorder. Pediatrics. 2004;113(4):754–761. doi: 10.1542/peds.113.4.754. [DOI] [PubMed] [Google Scholar]
- National Advisory Mental Health Council Clinical Treatment and Services Research Workgroup. Bridging science and service: A report by the National Advisory Mental Health Council Clinical Treatment and Services Research Workgroup. Washington, DC: National Institute of Mental Health; 1999. [Google Scholar]
- Newacheck PW, Strickland B, Shonkoff JP, Perrin JM, McPherson M, McManus M, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):117–123. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Stacey D. Should patient decision aids (PtDAs) be introduced in the health care system? Copenhagen: WHO Regional Office for Europe; 2005. [Google Scholar]
- O’Connor AM, Stacey D, Barry MJ, Col NF, Eden KB, Entwistle V, et al. Do patient decision aids meet effectiveness criteria of the International Patient Decision Aid Standards Collaboration? A systematic review and meta-analysis. Medical Decision Making. 2007;27(5):554–574. doi: 10.1177/0272989X07307319. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003;2:CD001431. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- Olaniyan O, dosReis S, Garriett V, Mychailyszyn MP, Anixt J, Rowe PC, et al. Community perspectives of childhood behavioral problems and ADHD among African American parents. Ambulatory Pediatrics. 2007;7(3):226–231. doi: 10.1016/j.ambp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Osheroff JA, Pifer EA, Teich JM, Sittig DF, Jenders RA. Improving outcomes with clinical decision support: An implementer’s guide. Chicago: Healthcare Information and Management Systems Society; 2005. [Google Scholar]
- Pliszka SR, Crismon ML, Hughes CW, Corners CK, Emslie GJ, Jensen PS, et al. The Texas Children’s Medication Algorithm Project: Revision of the algorithm for pharmacotherapy of attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(6):642–657. doi: 10.1097/01.chi.0000215326.51175.eb. [DOI] [PubMed] [Google Scholar]
- Polaha J, Cooper SL, Meadows T, Kratochvil CJ. The assessment of attention-deficit/hyperactivity disorder in rural primary care: The portability of the American Academy of Pediatrics guidelines to the “real world”. Pediatrics. 2005;115(2):e120–e126. doi: 10.1542/peds.2004-1521. [DOI] [PubMed] [Google Scholar]
- Porter SC, Forbes P, Feldman HA, Goldmann DA. Impact of patient-centered decision support on quality of asthma care in the emergency department. Pediatrics. 2006;117(1):e33–e42. doi: 10.1542/peds.2005-0906. [DOI] [PubMed] [Google Scholar]
- Power TJ, Hughes CL, Helwig JR, Nissley-Tsiopinis J, Mautone JA, Lavin HJ. Getting to first base: Promoting engagement in family-school intervention for children with ADHD in urban, primary care practice. School Mental Health. 2010 doi: 10.1007/s12310-010-9029-2. [DOI] [Google Scholar]
- Rosen P, Kwoh CK. Patient-physician e-mail: An opportunity to transform pediatric health care delivery. Pediatrics. 2007;120(4):701–706. doi: 10.1542/peds.2007-1094. [DOI] [PubMed] [Google Scholar]
- Rushton JL, Fant KE, Clark SJ. Use of practice guidelines in the primary care of children with attention-deficit/hyperactivity disorder. Pediatrics. 2004;114(1):e23–e28. doi: 10.1542/peds.114.1.e23. [DOI] [PubMed] [Google Scholar]
- Shapiro ES, DuPaul GJ, Barnabas E, Benson JL, Slay PM. Facilitating school, family, and community partnerships: Enhancing student mental health: An overview of the special issue. School Mental Health. 2010 doi: 10.1007/s12310-010-9033-6. [DOI] [Google Scholar]
- Stormshak EA, Fosco GM, Dishion TJ. Implementing interventions with families in schools to increase youth school engagement: The family check-up model. School Mental Health. 2010 doi: 10.1007/s12310-009-9025-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turchi RM, Berhane Z, Bethell C, Pomponio A, Antonelli R, Minkovitz CS. Care coordination for CSHCN: Associations with family-provider relations and family/child outcomes. Pediatrics. 2009;124(Supplement_4):S428–S434. doi: 10.1542/peds.2009-1255O. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Agency for Health Care Policy and Research Publication No. 99–0050. Rockville, Md: US Department of Health and Human Services; 1999. Diagnosis of Attention-Deficit/Hyperactivity Disorder: Technical review 3. [Google Scholar]
- Wagner EH. The role of patient care teams in chronic disease management. BMJ. 2000;320(7234):569–572. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weems CF, Scott BG, Taylor LK, Cannon MF, Romano DM, Perry AM, et al. Test anxiety prevention and intervention programs in schools: Program development and rationale. School Mental Health. 2010 doi: 10.1007/s12310-010-9032-7. [DOI] [Google Scholar]
- Weiland SK, Pless IB, Roghmann KJ. Chronic illness and mental health problems in pediatric practice: Results from a survey of primary care providers. Pediatrics. 1992;89(3):445–449. [PubMed] [Google Scholar]
- Westin AF. Connecting for health: Americans overwhelmingly believe electronic personal health records could improve their health. New York: Markle Foundation; 2008. [Google Scholar]