Abstract
The prevalence and incidence of both obesity and disability are projected to increase in the coming decades. The authors examined the relation between obesity and disability in older adults from 6 Latin American cities participating in the Health, Well-Being and Aging in Latin America and the Caribbean (SABE) Study (1999–2000). The sample included 6,166 participants aged 65 years or more. Data on sociodemographic factors, smoking status, medical conditions, body mass index (BMI; weight (kg)/height (m)2), and self-reported activities of daily living (ADL) were obtained. The prevalence of obesity (BMI ≥ 30) ranged from 13.3% in Havana, Cuba, to 37.6% in Montevideo, Uruguay. Using a BMI of 18.5–<25 as the reference category and controlling for all covariates, the lowest odds ratio for ADL limitation was for a BMI of 25–<30 (odds ratio = 1.10, 95% confidence interval: 0.93, 1.30), and the highest odds ratio for ADL limitation was for a BMI of 35 or higher (odds ratio = 1.63, 95% confidence interval: 1.26, 2.11). The results indicated that obesity is an independent factor contributing to ADL disability in these populations and should be included in future planning to reduce the impact of disability on global health.
Keywords: activities of daily living, adult, aged, Caribbean region, disabled persons, Latin America, obesity
The World Health Organization (WHO) estimates that 650 million people live with a disability or impairment (1). The WHO International Classification of Functioning, Disability and Health describes disability as “the outcome or result of a complex relationship between an individual's health condition and personal factors, and the external factors that represent the circumstances in which the individual lives” (2, p. 17).
The number of people with disabilities is increasing because of population growth, aging, a rise in chronic diseases, and improvements in medical care. The prevalence of disability is a particular concern in developing countries, where access to rehabilitation services and treatment programs is limited. The WHO reports that 80% of persons with disabilities live in low-income nations and that most are poor (3). Latin America is experiencing a significant increase in the proportion of persons aged 65 years or older (4). Colombia, Costa Rica, Mexico, Guatemala, Peru, Brazil, and Chile are projected to experience increases of more than 200% in the number of persons over 65 years of age between 2008 and 2040 (5). Persons aged 65 years or older are at highest risk for disability (5).
Obesity is also a health concern in both developed and developing countries (6). At a recent symposium on obesity in developing countries, Uauy et al. described “the rapid demographic and nutritional transition” (7, p. 893S) occurring in Latin America and indicated that the trend of increasing obesity would produce a corresponding rise in chronic disease and disability.
The association between obesity and mortality has been extensively investigated (8, 9). The relation between obesity and disability is less understood, particularly in the developing world. Recent research has demonstrated relations between obesity, as measured by body mass index (BMI), and disability in older adults (10–13). Additional research is needed to better understand the association between obesity and disability in order to plan future prevention and service-delivery programs. This need is especially urgent in developing areas, such as Latin America, where substantial demographic changes in the number of older adults, the number of persons with disabilities, and the prevalence of obesity are occurring (4).
We examined the relation between obesity and disability in older adults from 6 Latin American cities in the Salud, Bienestar y Envejecimiento en América Latina y el Caribe [Health, Well-Being and Aging in Latin America and the Caribbean] (SABE) Study (14). We hypothesized that there would be a significant association between obesity and disability and that the association would be mediated by medical conditions.
MATERIALS AND METHODS
Sample
The SABE Study (14) was a cross-sectional representative survey of noninstitutionalized older adults living in 7 Latin American cities: Buenos Aires, Argentina; Bridgetown, Barbados; São Paulo, Brazil; Santiago, Chile; Havana, Cuba; Mexico City, Mexico; and Montevideo, Uruguay (15, 16). Participants were selected on the basis of multistage cluster sampling. In each city, the primary sampling unit was a cluster of independent households within predetermined geographic areas. In all countries except Barbados and Brazil, the sample was chosen in 3 selection stages. In Barbados and Brazil, 2 selection stages were applied. Each sample consisted of 1,500–2,000 persons aged 60 years or older and their spouses. In total, 10,970 elderly men and women were interviewed during 1999–2000. The objective of SABE was to produce databases to evaluate demographic, socioeconomic, and health variables related to the emerging older population. Participants from Argentina were not included in our analyses, since anthropometric measurements needed to compute BMI were not taken there. The response rate for the cities varied from 65.3% in Montevideo to 95.3% in Havana, and the percentage of interviews completed by a proxy varied from 1.4% in Montevideo to 13.1% in São Paulo (15).
We analyzed SABE data for subjects aged 65 years or older from 6 cities (n = 7,371). Participants with complete data on measures of disability, BMI, and relevant covariates were included. We excluded 1,205 participants from the 7,371 interviewed; 830 had missing information on BMI or a BMI less than 15, and 375 had missing information on covariates. Excluded participants were older and more likely to be unmarried, to have less education, to have a lower BMI, and to have arthritis, stroke, or ADL disability. The final numbers of persons included in the analyses were 1,075 in Bridgetown, 1,352 in São Paulo, 859 in Santiago, 1,221 in Havana, 683 in Mexico City, and 976 in Montevideo, for a total of 6,166 participants.
Measurements
Disability was assessed using Katz et al.’s activities of daily living (ADL) scale (17). Interviewers asked participants whether they had experienced difficulty with or needed assistance in performing the following activities: walking across a small room, bathing, dressing, eating, getting into and out of bed, and using the toilet. ADL limitations were dichotomized as having difficulty or no difficulty in performing 1 or more of the 6 activities.
BMI was computed by dividing weight in kilograms by height in meters squared. BMIs were grouped according to the following standards: <18.5 = underweight, 18.5–24.9 = normal weight, 25.0–29.9 = overweight, 30.0–34.9 = obesity category I, 35.0–39.9 = obesity category II, and ≥40.0 = extreme obesity (18, 19). For the analyses, a BMI of 18.5–24.9 (normal weight) was used as the reference category.
Covariates
Sociodemographic variables included age (continuous), gender, years of formal education (continuous), and marital status (married = 1, not married/widowed/separated = 0). Smoking status was assessed by asking whether participants were current smokers, were former smokers, or had never smoked. The presence of chronic medical conditions was assessed by asking participants whether they had ever been told by a doctor or nurse that they had arthritis, diabetes, heart attack, hypertension, stroke, or cancer.
Statistical analysis
Data on participant characteristics were stratified by city and examined using descriptive statistics. Univariate comparisons based on continuous variables were conducted with 1-way analysis of variance, and comparisons involving categorical variables were conducted with chi-square tests. Logistic regression analysis was used to estimate the odds ratio for any ADL disability as a function of BMI, controlling for age and gender, for each city. We collapsed all participants with BMIs of 35 or more into 1 group because of the small number in each city. The homogeneity of BMI across cities, controlling for the effects of age and gender on ADL limitation, was assessed using Dyer's approach (20). After the homogeneity effect was established (P = 0.64), the relation between disability and BMI was tested jointly for all cities.
Two models were examined using the combined data. Model 1 included disability as the dependent variable with BMI as the independent variable and age, gender, education, marital status, smoking status, and city as covariates. In model 2, chronic medical conditions (arthritis, diabetes, hypertension, stroke, heart attack, and cancer) were added to the predictors included in model 1. To test whether the relation between BMI and ADL disability was mediated by medical conditions, we estimated the percentage reduction in the odds ratio (OR) in models with and without the proposed mediators (i.e., % reduction = [(OR without mediators − OR with mediators/OR without mediators − 1) × 100]) (21, 22). To test whether ADL disability increased from normal weight to extreme obesity, we created linear orthogonal contrasts under logistic regression models for each city and tested them using the Wald chi-square test. To test the U-shaped relation between BMI and ADL disability for each city, we performed a quadratic contrast on BMI categories and quadratic functional form analysis on BMI as a continuous variable. Multiple imputation with the Markov chain Monte Carlo method was used to account for the nonresponse variables (23).
To adjust for the sampling weights and design effects used in the SABE Study, we employed SAS survey procedures (SAS Institute Inc., Cary, North Carolina). All analyses were performed using SAS for Windows, version 9.1.3 (SAS Institute Inc.).
RESULTS
Table 1 shows the sociodemographic and personal characteristics of participants. Mean ages ranged from 72.7 years (standard error, 0.42) in São Paulo to 74.8 years (standard error, 0.22) in Bridgetown. Female participants outnumbered males in every sample. The prevalence of ADL limitation ranged from 12.8% (Bridgetown) to 24.5% (Santiago). The mean BMI ranged from 24.2 (Havana) to 28.3 (Montevideo). The prevalence of category I obesity (BMI 30–<35) ranged from 10.4% (Havana) to 22.9% (Santiago), and the prevalence of category II and extreme obesity (BMI ≥35) ranged from 2.9% (Havana) to 15.7% (Montevideo). Arthritis and hypertension were the most prevalent medical conditions across all cities, with the exception of heart attack being more prevalent in Santiago. Females consistently reported significantly more ADL limitation and had higher rates of obesity than males.
Table 1.
Characteristics of Participants in the Health, Well-Being and Aging in Latin America and the Caribbean (SABE) Study (n = 6,166), by City, 1999–2000a
| Explanatory Variable | Bridgetown, Barbados (n = 1,075) |
São Paulo, Brazil (n = 1,352) |
Santiago, Chile (n = 859) |
Havana, Cuba (n = 1,221) |
Mexico City, Mexico (n = 683) |
Montevideo, Uruguay (n = 976) |
||||||
| % or Mean | 95% CI | % or Mean | 95% CI | % or Mean | 95% CI | % or Mean | 95% CI | % or Mean | 95% CI | % or Mean | 95% CI | |
| Mean age, years | 74.8 | 74.4, 75.3 | 72.7 | 71.8, 73.5 | 73.7 | 72.9, 74.3 | 74.3 | 73.9, 74.7 | 72.9 | 72.5, 73.5 | 73.2 | 72.7, 73.7 |
| Female gender | 60.7 | 57.7, 63.6 | 61.4 | 58.4, 64.4 | 61.9 | 56.1, 67.9 | 60.0 | 56.9, 63.0 | 59.6 | 55.7, 63.4 | 63.6 | 60.3, 66.8 |
| Any limitation in activities of daily livingb | 12.8 | 10.8, 14.9 | 18.9 | 16.0, 21.8 | 24.5 | 20.8, 28.3 | 17.9 | 15.8, 20.2 | 21.4 | 18.2, 24.7 | 16.9 | 14.5, 19.3 |
| Mean BMIc | 26.9 | 26.4, 27.3 | 26.4 | 26.1, 26.7 | 27.7 | 27.2, 28.2 | 24.2 | 23.9, 24.5 | 27.5 | 27.1, 27.8 | 28.3 | 27.9, 28.8 |
| BMI category | ||||||||||||
| <18.5 | 5.9 | 4.4, 7.3 | 3.1 | 2.1, 4.2 | 1.3 | 0.6, 2.0 | 12.3 | 10.3, 14.3 | 1.2 | 0.3, 2.1 | 3.5 | 1.9, 4.9 |
| 18.5–<25 | 37.8 | 34.9, 40.7 | 31.8 | 29.1, 34.4 | 23.1 | 19.4, 26.9 | 43.9 | 41.0, 46.9 | 26.4 | 23.0, 29.8 | 26.4 | 23.5, 29.3 |
| 25–<30 | 31.2 | 28.4, 33.9 | 41.5 | 38.4, 44.5 | 44.5 | 38.6, 50.3 | 30.5 | 27.7, 33.3 | 43.7 | 39.9, 47.6 | 32.4 | 29.4, 35.5 |
| 30–<35 | 15.2 | 13.1, 17.4 | 17.6 | 15.5, 19.8 | 22.9 | 20.1, 25.8 | 10.4 | 8.4, 12.4 | 21.3 | 18.2, 24.4 | 21.9 | 18.5, 25.3 |
| ≥35 | 9.9 | 8.2, 11.7 | 6.0 | 4.5, 7.5 | 8.2 | 5.1, 11.2 | 2.9 | 1.9, 3.8 | 7.4 | 5.4, 9.4 | 15.7 | 13.5, 17.9 |
| Mean education, years | 5.1 | 4.9, 5.3 | 3.0 | 2.6, 3.5 | 6.2 | 5.1, 7.3 | 6.7 | 6.4, 6.9 | 4.4 | 4.1, 4.8 | 6.0 | 5.6, 6.5 |
| Married marital status | 34.2 | 31.3, 37.0 | 52.6 | 48.9, 56.3 | 52.2 | 46.7, 57.6 | 33.9 | 31.1, 36.7 | 49.5 | 45.7, 53.4 | 45.5 | 41.8, 49.2 |
| Smoking status | ||||||||||||
| Never smoker | 72.1 | 69.5, 74.9 | 54.4 | 51.0, 57.8 | 55.8 | 50.5, 60.9 | 49.3 | 46.2, 52.4 | 58.1 | 54.3, 61.9 | 59.1 | 55.4, 62.7 |
| Former smoker | 21.8 | 19.3, 24.2 | 31.6 | 28.6, 34.7 | 33.3 | 29.0, 37.6 | 22.8 | 20.1, 25.5 | 25.4 | 22.0, 28.7 | 28.3 | 25.0, 31.6 |
| Current smoker | 6.0 | 4.6, 7.4 | 13.9 | 11.7, 16.2 | 10.9 | 8.5, 13.3 | 27.9 | 25.2, 30.6 | 16.5 | 13.6, 19.5 | 12.6 | 10.3, 14.9 |
| Chronic medical condition | ||||||||||||
| Arthritis | 49.5 | 46.5, 52.5 | 36.4 | 33.5, 39.4 | 32.6 | 29.2, 35.9 | 56.3 | 53.1, 59.4 | 26.4 | 23.0, 29.9 | 49.0 | 44.8, 53.2 |
| Diabetes | 19.8 | 17.4, 22.2 | 19.2 | 16.4, 21.9 | 12.9 | 8.3, 17.4 | 15.3 | 13.0, 17.6 | 21.6 | 18.5, 24.8 | 14.7 | 12.0, 17.4 |
| Hypertension | 48.3 | 45.3, 51.3 | 55.7 | 51.8, 59.5 | 51.3 | 45.1, 57.5 | 42.1 | 39.0, 45.1 | 44.8 | 40.9, 48.6 | 45.3 | 42.3, 48.4 |
| Stroke | 5.2 | 3.8, 6.5 | 5.9 | 4.6, 7.3 | 6.2 | 4.2, 8.2 | 9.5 | 7.5, 11.4 | 6.2 | 4.3, 8.2 | 3.3 | 2.1, 4.5 |
| Heart attack | 12.8 | 10.8, 14.8 | 21.6 | 18.9, 24.2 | 34.2 | 27.6, 40.8 | 25.5 | 22.7, 28.3 | 11.6 | 9.1, 14.1 | 26.1 | 23.2, 29.0 |
| Cancer | 3.1 | 2.1, 4.2 | 3.9 | 2.8, 5.0 | 3.8 | 2.5, 5.1 | 2.9 | 1.9, 3.9 | 1.9 | 0.9, 2.9 | 6.1 | 4.5, 7.7 |
Abbreviations: BMI, body mass index; CI, confidence interval.
Results were obtained after adjusting for sampling weights and design effects used in the SABE Study.
Assessed using Katz et al.’s activities of daily living scale (17).
Weight (kg)/height (m)2.
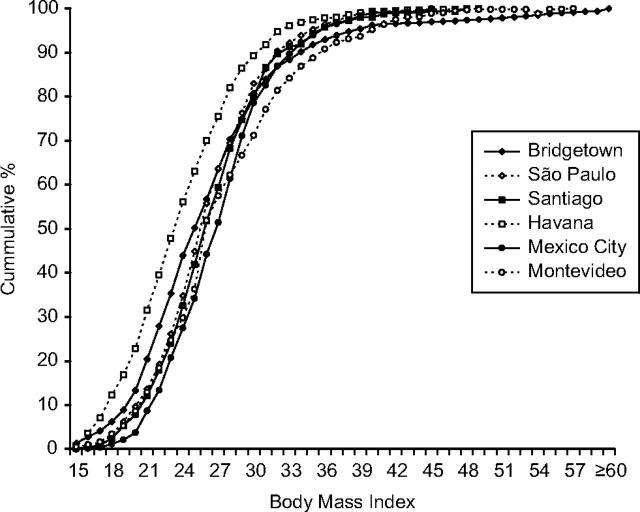
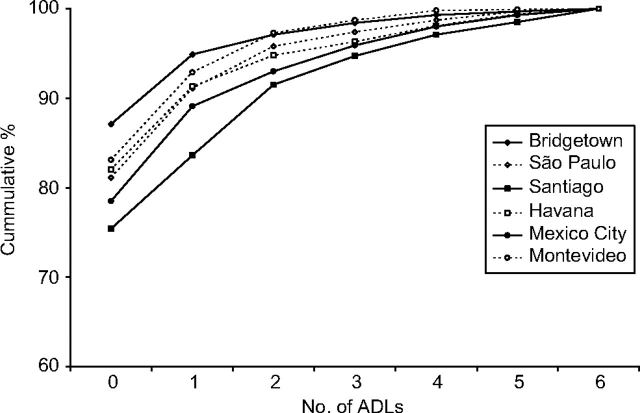
Figure 1 shows the BMI cumulative percentage for each city. The figure reveals similar patterns for each sample, with Havana showing a larger percentage of participants at lower levels of BMI. For example, 63% of participants from Havana had a BMI of 25 or less as compared with 50% of participants from Bridgetown. The cumulative percentage of ADL limitation for each city is shown in Figure 2. Santiago had the highest proportion of subjects with ADL limitation, while Bridgetown had the lowest.
Figure 1.
Body mass index (weight (kg)/height (m)2) cumulative percentage among elders from 6 Latin American cities (n = 6,166), Health, Well-Being and Aging in Latin America and the Caribbean (SABE) Study, 1999–2000. Percentages were obtained after adjusting for sampling weights and design effects used in the SABE Study.
Figure 2.
Cumulative percentage of number of limitations in activities of daily living (ADLs) among elders from 6 Latin American cities (n = 6,166), Health, Well-Being and Aging in Latin America and the Caribbean (SABE) Study, 1999–2000. Percentages were obtained after adjusting for sampling weights and design effects used in the SABE Study.
Figure 3 displays the percentage of ADL limitation by BMI category for each city. The percentage of any ADL limitation for a BMI less than 18.5 ranged from 14.9% (Bridgetown) to 49.9% (Santiago); for a BMI greater than or equal to 35, the percentage of ADL limitation varied from 17.9% (Bridgetown) to 36.5% (São Paulo). In some samples (Bridgetown, São Paulo, Santiago, and Havana), there was a U-shaped relation between BMI and ADL limitation, with higher levels of disability among persons with low and high BMIs. However, this U-shaped relation was not statistically significant. The relations in data from Mexico City and Montevideo were characterized by flatter curves between BMIs of 18.5 and 35.0.
Figure 3.
Percentage of persons with any limitation in activities of daily living (ADLs) by body mass index (weight (kg)/height (m)2) category among elders from 6 Latin American cities (n = 6,166), Health, Well-Being and Aging in Latin America and the Caribbean (SABE) Study, 1999–2000. Percentages were obtained after adjusting for sampling weights and design effects used in the SABE Study.
Table 2 presents odds ratios for ADL limitation as a function of BMI category, controlling for age and gender. Participants from Havana and São Paulo with BMIs of 30 or higher and participants from Bridgetown with BMIs of 35 or higher were more likely to report ADL limitation. There was a statistically significant trend for increasing disability with increasing BMI only among participants from São Paulo and Havana.
Table 2.
Odds Ratio for Any Disability in Activities of Daily Living as a Function of Body Mass Index Category Among Elders From 6 Latin American Cities (n = 6,166), Health, Well-Being and Aging in Latin America and the Caribbean (SABE) Study, 1999–2000a
| Body Mass Indexb Category | Bridgetown, Barbados (n = 1,075) |
São Paulo, Brazil (n = 1,352) |
Santiago, Chile (n = 859) |
Havana, Cuba (n = 1,221) |
Mexico City, Mexico (n = 683) |
Montevideo, Uruguay (n = 976) |
||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| <18.5 | 0.93 | 0.40, 2.12 | 1.14 | 0.49, 2.65 | 2.57 | 0.65, 10.13 | 1.08 | 0.62, 1.85 | 0.89 | 0.08, 10.06 | 2.22 | 0.88, 5.62 |
| 18.5–<25 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 25–<30 | 1.20 | 0.76, 1.89 | 1.27 | 0.88, 1.85 | 1.32 | 0.85, 2.05 | 1.28 | 0.85, 1.93 | 1.10 | 0.67, 1.79 | 1.40 | 0.88, 2.24 |
| 30–<35 | 0.97 | 0.52, 1.81 | 1.64 | 1.15, 2.33 | 1.29 | 0.78, 2.14 | 1.79 | 1.07, 2.99 | 1.16 | 0.65, 2.09 | 1.33 | 0.69, 2.55 |
| ≥35 | 1.89 | 1.02, 3.51 | 3.66 | 2.01, 6.66 | 1.83 | 0.88, 3.83 | 2.47 | 1.04, 5.90 | 1.69 | 0.77, 3.71 | 1.10 | 0.64, 1.91 |
| P valuec | 0.17 | 0.003 | 0.79 | 0.03 | 0.57 | 0.23 | ||||||
Abbreviations: CI, confidence interval; OR, odds ratio.
Results were controlled for age and gender using the sampling weights and design effects of the SABE Study.
Weight (kg)/height (m)2.
Contrast for a linear increase from 18.5 to ≥35 based on the Wald chi-square test.
We examined the homogeneity of the effect of BMI on ADL limitation (20). The results indicated that the effect was homogeneous across all study sites. On the basis of this analysis, we examined the relation of BMI to ADL limitation in the combined SABE samples. The results from these analyses are presented in Table 3. Model 1 included age, gender, marital status, education, smoking status, and city. In model 2, medical conditions were added to the predictors in model 1. Using a BMI of 18.5–<25 as the reference category, the smallest odds ratio associated with ADL limitation was found in participants with BMIs of 25–<30, and the highest odds ratio for ADL limitation was evident in participants with BMIs less than 18.5 or greater than or equal to 35, after controlling for all covariates (model 2). The mediating effect of medical conditions on the relation between BMI and ADL disability was significant only for a BMI of 35 or more (reduction of 23.2% in the odds ratio; P < 0.0001). To test the stability of this finding, we replicated the analyses using more conservative levels for ADL limitation based on difficulty in completing 2 of 6 ADL items and then 3 of 6 ADL items. Similar relations were found. Older age, female gender, former smoking, arthritis, heart attack, stroke, and cancer were factors significantly associated with ADL limitation, while participants with higher levels of education were less likely to report ADL limitation. Logistic regression analysis with imputed data was performed as a function of BMI category. The findings were similar to those obtained using original data without imputation, where participants with BMIs greater than or equal to 35 were at higher risk for ADL disability.
Table 3.
Odds Ratio for Any Disability in Activities of Daily Living as a Function of Body Mass Index Category and Other Variables Among Elders From 6 Latin American Cities (n = 6,166), Health, Well-Being and Aging in Latin America and the Caribbean (SABE) Study, 1999–2000a
| Explanatory Variable | Model 1b |
Model 2c |
||
| OR | 95% CI | OR | 95% CI | |
| Body mass index categoryd | ||||
| <18.5 | 1.22 | 0.90, 1.66 | 1.25 | 0.91, 1.71 |
| 18.5–<25 | 1.00 | 1.00 | ||
| 25–<30 | 1.17 | 0.99, 1.37 | 1.10 | 0.93, 1.30 |
| 30–<35 | 1.24 | 1.02, 1.52 | 1.11 | 0.89, 1.36 |
| ≥35 | 1.82 | 1.42, 2.34 | 1.63 | 1.26, 2.11 |
| Age, years | 1.07 | 1.06, 1.08 | 1.07 | 1.06, 1.08 |
| Female gender | 1.54 | 1.29, 1.82 | 1.28 | 1.07, 1.53 |
| City | ||||
| Bridgetown, Barbados | 1.00 | 1.00 | ||
| São Paulo, Brazil | 1.74 | 1.38, 2.20 | 1.87 | 1.47, 2.38 |
| Santiago, Chile | 2.62 | 2.06, 3.35 | 2.87 | 2.22, 3.70 |
| Havana, Cuba | 1.72 | 1.35, 2.19 | 1.48 | 1.15, 1.90 |
| Mexico City, Mexico | 1.97 | 1.51, 2.57 | 2.46 | 1.87, 3.25 |
| Montevideo, Uruguay | 1.43 | 1.10, 1.84 | 1.46 | 1.12, 1.90 |
| Married marital status | 1.01 | 0.86, 1.17 | 0.99 | 0.85, 1.16 |
| Education, years | 0.96 | 0.94, 0.97 | 0.95 | 0.94, 0.97 |
| Smoking status | ||||
| Never smoker | 1.00 | 1.00 | ||
| Former smoker | 1.30 | 1.10, 1.53 | 1.20 | 1.01, 1.41 |
| Current smoker | 1.06 | 0.85, 1.32 | 1.06 | 0.84, 1.33 |
| Chronic medical condition | ||||
| Arthritis | 2.05 | 1.78, 2.36 | ||
| Diabetes | 1.16 | 0.97, 1.38 | ||
| Hypertension | 1.12 | 0.97, 1.29 | ||
| Stroke | 2.83 | 2.25, 3.57 | ||
| Heart attack | 1.52 | 1.31, 1.77 | ||
| Cancer | 1.41 | 1.02, 1.94 | ||
Abbreviations: CI, confidence interval; OR, odds ratio.
This table shows unweighted data.
Model 1 included age, gender, marital status, education, smoking status, and city.
In model 2, chronic medical conditions were added to the predictors in model 1.
Weight (kg)/height (m)2.
DISCUSSION
The incidence and prevalence of obesity and disability are projected to increase significantly in the coming decades (4, 24). A recent report entitled An Aging World: 2008 (5) provided evidence that population aging has emerged as the major global demographic trend in the first decade of the 21st century. Seven of the 14 nations with the largest projected increases in numbers of persons aged 65 years or older are in Latin America.
The world's population aged 80 years or older is expected to increase 233% between 2008 and 2040, as compared with 160% for the population aged 65 or over and 33% for the total population of all ages (5). The increase in chronic disease and disability associated with the aging of the population, along with rising rates of obesity, will present major challenges to health care and social services worldwide.
Our results reflect these emerging challenges. We found rates of disability, as indicated by difficulty in performing basic ADLs, in 12.8%–24.5% of the people surveyed in 6 cities. The proportion of participants with a BMI greater than 30 ranged from 13.3% (Havana) to 37.6% (Montevideo). Multivariable logistic regression using the combined samples produced statistically significant odds ratios for ADL limitation of 1.63 for persons with a BMI greater than 35, after adjustment for sociodemographic variables, smoking status, medical conditions, and city. The odds ratio associated with a BMI greater than 35 was reduced by 23.2% (P < 0.0001) when medical conditions were added. This finding was not surprising given the established connection of obesity with diabetes, hypertension, stroke, and heart attack.
Our results suggest a multifaceted relation with disability involving age, gender, obesity, city, and other health conditions. The findings have implications for the development of prevention and intervention programs and suggest that attempts to reduce disability or obesity in isolation are likely to have limited success.
In 2005, the World Health Assembly approved the resolution “Disability, Including Prevention, Management and Rehabilitation” (25). The WHO has also organized initiatives related to obesity and aging (3). In planning future programs for preventing or reducing disability, it will be important to include system-based interventions that recognize the complex nature of aging, obesity, and disability. The WHO initiatives for promoting community-based rehabilitation are positioned to address the multiple factors contributing to disability (25). To maximize their effectiveness, community-based rehabilitation programs should incorporate factors contributing to disability in different settings and cultures.
Our findings suggest that community-based rehabilitation programs in developing nations should include a nutritional component to prevent/reduce obesity. Practitioners in these programs must be familiar with the social and cultural factors associated with obesity and disability in each country. For example, we found lower levels of obesity among older adults living in Havana as compared with persons from other SABE sites. If the lower level of obesity in Havana is found to be reliable, studies should be conducted to determine whether a similar pattern exists in younger persons and what factors are contributing to the lower BMI for participants in Cuba (more exercise, etc.).
Another area of potential interest is the prevalence of diabetes across countries. The prevalence of self-reported diabetes in this study ranged from 12.9% (Santiago) to 21.6% (Mexico City). Diabetes is directly related to diet and obesity and has a strong association with disability. The incorporation of diabetes management as a part of prevention programs or efforts to reduce disability is an important component of community-based rehabilitation programs and requires continued research.
This study had some limitations. First, because this was a cross-sectional study, it was not possible to determine the temporal sequence of BMI and ADL limitation. Second, information on disability was obtained by self-report and was subject to recall bias, particularly for the oldest participants. Third, data on comorbid conditions were obtained by self-report. However, other investigators have found good agreement between self-reported medical events and comorbid diseases or conditions (26, 27).
The study's strengths included the collection of information from large, well-defined samples of persons living in 6 capital cities, generalizable to all older adults in the cities of origin. Most older people in Latin America and the Caribbean live in urban areas (28). Over 70% of the older population in the region lives in cities (28). Survey measures were similar across the data collection sites, allowing for direct comparisons. Data were collected by different groups of interviewers/examiners. However, all interviewers received similar training in the data collection and assessment procedures, and the procedures for measurement of BMI and disability were identical in each setting.
There is controversy in the literature regarding the most appropriate and sensitive measure of body mass and obesity in older adults and in persons from different racial and ethnic groups (29). We selected BMI to assess obesity because it is the most commonly used measure and has been applied in prior studies examining Latinos (4, 6). Other measures of obesity, including waist circumference and waist-to-hip ratio, may be more sensitive in older adults or persons with disabilities (29). The ideal measure for use in older adults and persons with variation in anthropometric characteristics is a subject that requires continued research.
World Health Assembly resolution 58.23 supports the “WHO member states in collecting more reliable data and to promote studies of incidence and prevalence of disabilities as a basis for the formulation of strategies for prevention, treatment and rehabilitation” (25, p. 3). The results of this investigation contribute to the WHO resolution by providing information on disability and obesity from a broad international sample of Latino older adults. The findings will assist in planning future research designed to address the mission of the WHO Disability and Rehabilitation Action Plan for 2006–2011 (30): to improve the quality of life for persons with disabilities and their families.
Acknowledgments
Author affiliations: Division of Rehabilitation Sciences, University of Texas Medical Branch, Galveston, Texas (Soham Al Snih, James E. Graham, James S. Goodwin, Kenneth J. Ottenbacher); Sealy Center on Aging, University of Texas Medical Branch, Galveston, Texas (Soham Al Snih, Yong-Fang Kuo, James S. Goodwin, Kyriakos S. Markides, Kenneth J. Ottenbacher); Division of Geriatrics, Department of Internal Medicine, University of Texas Medical Branch, Galveston, Texas (Soham Al Snih, Yong-Fang Kuo, James S. Goodwin, Kenneth J. Ottenbacher); and Department of Preventive Medicine and Community Health, University of Texas Medical Branch, Galveston, Texas (Yong-Fang Kuo, James S. Goodwin, Kyriakos S. Markides, Kenneth J. Ottenbacher).
This study was supported by grants R03-AG029959, R01-AG017638, R01-AG010939, and P30-AG024832 from the National Institute on Aging. Dr. Soham Al Snih was supported by a research career development award (no. K12HD052023) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Institute of Allergy and Infectious Diseases; and the Office of the Director, National Institutes of Health.
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funding institutes or the National Institutes of Health. The funding agencies did not influence the study design, analysis, or interpretation of the results.
Conflict of interest: none declared.
Glossary
Abbreviations
- ADL
activities of daily living
- BMI
body mass index
- SABE
Salud, Bienestar y Envejecimiento en América Latina y el Caribe
- WHO
World Health Organization
References
- 1.World Health Organization. Geneva, Switzerland: World Health Organization; 2009. Disability and Rehabilitation. ( http://www.who.int/disabilities/en/). (Accessed July 16, 2009) [Google Scholar]
- 2.World Health Organization. ICF: International Classification of Functioning, Disability and Health. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 3.World Health Organization. What Is Being Done to Improve the Daily Lives of People With Disabilities? Geneva, Switzerland: World Health Organization; 2010. ( http://www.who.int/features/qa/16/en/index.html). (Accessed March 2, 2010) [Google Scholar]
- 4.Filozof C, Gonzalez C, Sereday M, et al. Obesity prevalence and trends in Latin-American countries. Obes Rev. 2001;2(2):99–106. doi: 10.1046/j.1467-789x.2001.00029.x. [DOI] [PubMed] [Google Scholar]
- 5.Kinsell K, He W. An Aging World: 2008. (International Population Report no. P95/09-1). Washington, DC: Bureau of the Census, US Department of Commerce; 2009. [Google Scholar]
- 6.Monteiro CA, Moura EC, Conde WL, et al. Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ. 2004;82(12):940–946. [PMC free article] [PubMed] [Google Scholar]
- 7.Uauy R, Albala C, Kain J. Obesity trends in Latin America: transiting from under- to overweight. J Nutr. 2001;131(3):893S–899S. doi: 10.1093/jn/131.3.893S. [DOI] [PubMed] [Google Scholar]
- 8.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Prospective Studies Collaboration. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 10.Al Snih S, Ottenbacher KJ, Markides KS, et al. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med. 2007;167(8):774–780. doi: 10.1001/archinte.167.8.774. [DOI] [PubMed] [Google Scholar]
- 11.Bender R, Jöckel KH, Trautner C, et al. Effect of age on excess mortality in obesity. JAMA. 1999;281(16):1498–1504. doi: 10.1001/jama.281.16.1498. [DOI] [PubMed] [Google Scholar]
- 12.Chen H, Guo X. Obesity and functional disability in elderly Americans. J Am Geriatr Soc. 2008;56(4):689–694. doi: 10.1111/j.1532-5415.2007.01624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walter S, Kunst A, Mackenbach J, et al. Mortality and disability: the effect of overweight and obesity. Int J Obes (Lond) 2009;33(12):1410–1418. doi: 10.1038/ijo.2009.176. [DOI] [PubMed] [Google Scholar]
- 14.Albala C, Lebrão ML, León Díaz EM, et al. The Health, Well-Being, and Aging (“SABE”) survey: methodology applied and profile of the study population. Rev Panam Salud Publica. 2005;17(5-6):307–322. doi: 10.1590/s1020-49892005000500003. [DOI] [PubMed] [Google Scholar]
- 15.Palloni A, Pelaez M. Survey of Health and Well-Being of Elders. Final Report. Washington, DC: Pan American Health Organization; 2002. [Google Scholar]
- 16.Palloni A, Pinto-Aguirre G, Pelaez M. Demographic and health conditions of ageing in Latin America and the Caribbean. Int J Epidemiol. 2002;31(4):762–771. doi: 10.1093/ije/31.4.762. [DOI] [PubMed] [Google Scholar]
- 17.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The Index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 18.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: Evidence Report. National Heart, Lung, and Blood Institute Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. (NIH publication no. 02-4084). Bethesda, MD: National Heart, Lung, and Blood Institute; 2002. [Google Scholar]
- 19.World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. (WHO Technical Report Series no. 894). Geneva, Switzerland: World Health Organization; 1998. [PubMed] [Google Scholar]
- 20.Dyer AR. A method for combining results from several prospective epidemiologic studies. Stat Med. 1986;5(4):303–317. doi: 10.1002/sim.4780050403. [DOI] [PubMed] [Google Scholar]
- 21.Szklo M, Nieto FJ. Epidemiology: Beyond the Basics. Gaithersburg, MD: Aspen Publications; 2000. [Google Scholar]
- 22.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 23.Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8(1):3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 24.Arterburn DE, Crane PK, Sullivan SD. The coming epidemic of obesity in elderly Americans. J Am Geriatr Soc. 2004;52(11):1907–1912. doi: 10.1111/j.1532-5415.2004.52517.x. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. WHA Resolution 58.23. Disability, Including Prevention, Management and Rehabilitation. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- 26.Haapanen N, Miilunpalo S, Pasanen M, et al. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997;145(8):762–769. doi: 10.1093/aje/145.8.762. [DOI] [PubMed] [Google Scholar]
- 27.Simpson CF, Boyd CM, Carlson MC, et al. Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc. 2004;52(1):123–127. doi: 10.1111/j.1532-5415.2004.52021.x. [DOI] [PubMed] [Google Scholar]
- 28.Population, Ageing and Development. San Juan, Puerto Rico: United Nations; 2004. United Nations Economic Commission for Latin America and the Caribbean. [Google Scholar]
- 29.Visscher TL, Seidell JC, Molarius A, et al. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: the Rotterdam Study. Int J Obes Relat Metab Disord. 2001;25(11):1730–1735. doi: 10.1038/sj.ijo.0801787. [DOI] [PubMed] [Google Scholar]
- 30.Disability and Rehabilitation: WHO Action Plan 2006–2011. Geneva, Switzerland: World Health Organization; 2005. Disability and Rehabilitation Team, World Health Organization. ( http://www.who.int/disabilities/publications/action_plan/en/index.html). (Accessed July 25, 2009) [Google Scholar]