Abstract
Background:
The diabetes epidemic in China imposes an increasing burden on the health care system and the economy. We derived prospective diabetes prevalence rates in China until 2016 from a systematic review of the published literature in the period 1987–2007. The results could help to guide resources of the Chinese health care system in order to address the diabetes epidemic.
Methods:
We selected articles published in the English/Chinese languages from MEDLINE and the China Wanfang Digital Database using the keywords “China”, “diabetes mellitus”, “prevalence”, and “epidemiology” in order to estimate the current diabetes prevalence in China. For projecting future prevalence rates, we considered the population growth, and assumed that China’s diabetes prevalence in first tier cities in 2016 would equal Hong Kong’s diabetes prevalence in 2007.
Results:
The number of Chinese adults with diabetes is projected to rise from 53.1 million in 2009 to 76.1 million in 2016. The estimated diabetes prevalence rate in China in 2009 was 3.9% (urban 5.2%, rural 2.9%) and is projected to increase to 5.4% (urban 6.9%, rural 3.8%) in 2016, corresponding to an annual consolidated aggregate growth rate of 4.6%.
Conclusion:
We estimate a considerably higher diabetes prevalence in the adult Chinese population than that reported in previous studies. The diabetes prevalence will continue to rise in the future, which points to the importance of increasing awareness and better diagnosis of diabetes in China.
Keywords: diabetes, prevalence, epidemic, China, Chinese, systematic review
Introduction
Diabetes increases the risk of developing long-term microvascular and macrovascular complications and represents a major public health concern.1 The World Health Organization (WHO) estimates that more than 180 million people worldwide suffered from diabetes in 2008, a number which will be more than twice as high by 2030.2 Prevalence estimates of diabetes and impaired glucose tolerance in all Asian countries, adjusted to those for the world population, are high and are expected to increase further.3 China has one of the largest single diabetes populations worldwide, due to rapid westernization, with its associated changes in dietary habits and a sedentary lifestyle.4 Diabetes and its complications also have significant economic consequences for individuals, families, and health care systems. The WHO estimates that from 2006 to 2015 China will lose $558 billion of its national income due to heart disease, stroke, and diabetes.2 Therefore, adequate financial resources and structures of health care delivery are required to deal with the future diabetes burden, particularly in the context of continued rapid urbanization.5 Previous nationwide epidemiologic studies, conducted between 1997 and 2006, showed diabetes prevalence rates varying between 0.6%–6.8%.6–11 However, these studies were cross-sectional in nature and were carried out in different cities at various time points. Furthermore, estimation of future diabetes prevalence will allow us to understand and address better the diabetes burden in China. We carried out a systematic literature review of the published data for diabetes prevalence in China and tried to estimate prevalence rates of diabetes for the years 2009–2016 for the urban and rural populations.
Methodology
Search strategy
We conducted a systematic literature search of MEDLINE and the China Wanfang Digital Database12 for articles containing the keywords “China”, “diabetes mellitus”, “prevalence”, and “epidemiology”, published in the English or Chinese language for 1987–2007. Titles and abstracts of the resulting publications were screened for further articles that were possibly of interest for our review. The references in the relevant articles and review articles were checked for additional studies of interest. We included original articles of observational studies on diabetes prevalence for China published in peer-reviewed journals. We excluded randomized controlled trials, editorials, letters to the editor, and review articles.
Data extraction
The key parameter of interest was the prevalence of diabetes. On initial screening, articles were selected if they reported prevalence data on diabetes. The full texts of relevant articles were scrutinized, and the extracted data on coverage, study population, age group, year of study, and results (original/age-standardized prevalence rates) were organized in tables. The definitions and diagnostic measures used to define diabetes prevalence varied across studies. The population-based studies from China used the 1997 criteria from the American Diabetes Association (ADA) or the 1999 criteria from WHO to diagnose diabetes.6–9 In the present study, we selected publications using the WHO/ADA criteria for diabetes diagnosis (ie, fasting plasma glucose >7.0 mmol/L).
Estimation of diabetes prevalence
Estimates of the nationwide diabetes prevalence rate were derived from major diabetes epidemiologic surveys in China,6,7,9,11,13 and are summarized in Table 1. Table 2 presents prevalence rates as measured in studies of various Chinese populations.5,6,14–30 Differences in prevalence rates are most likely to be due to different survey methodologies, diagnostic criteria, time points of analyses, and the cities where the studies were conducted. Based on a database of 661 Chinese cities, the urban population was classified into four city tiers according to wealth distribution (Gross Domestic Product per capita) and population.31 The categorization into urban and rural segments was based on the definition provided in the China Statistics Yearbook.32 Since the patients’ ages differed significantly, the crude overall prevalence rates were corrected for age (see Table 3). We used the 2000 China National Census data for standardizing prevalence. For first tier cities, we selected a standardized prevalence of 7.6% from the most recently published report.15 For other city tiers, we calculated the prevalence rate for 2009 by taking an average of the age-standardized prevalence rates (fifth column in Table 3). This approach was confirmed to be reasonable by diabetes experts in China. We adjusted the average age-standardized prevalence rate by the difference between percentage of the adult population (>19 years) in 2000 (67.9%) and 2009 (72.3%) to calculate the prevalence rate in 2009 (eighth column in Table 3).33 We projected a prevalence rate increase for each forecast year thereafter (2010–2016) based on the trends suggested by the available data and assumptions for prevalence growth rate (Table 4). For first tier cities, we assumed that the 2016 diabetes prevalence in China would equal the 2007 diabetes prevalence in Hong Kong, where the population had the earliest exposure to risk factors for diabetes, in particular, a more sedentary lifestyle and a high-fat diet, but is of the same ethnic origin as the population in mainland China. The annual growth rate of diabetes prevalence was described as the consolidated aggregate growth rate (CAGR) from 2009–2016, and was calculated as the ending value/beginning value/number of years.
Table 1.
Major nationwide surveys on diabetes prevalence in China
| Reference | Sample | Sample size | Age (years) | Year of study | Prevalence (%) |
|---|---|---|---|---|---|
| Southern Research Institute of Medicine Economics DM prevalence survey, 200411 | Nationwide | NA | All | 1978 | 0.6 |
| 1990 | 1.2 | ||||
| 1995 | 1.5 | ||||
| 2000 | 2.4 | ||||
| Pan et al6 | 19 provinces, urban and rural | 224,251 | 25–64 | 1994 | 2.5 |
| Yang et al7 | 12 areas | 29,559 | 40–99 | 1998 | 5.9 |
| 12 urban areas | 6.8 | ||||
| 12 rural areas | 3.8 | ||||
| Gu et al9 | Nationwide | 15,540 | 35–74 | 2000 | 5.5 |
| Li et al13 | Nationwide | NA | ➢18 | 2002 | 2.6 |
| Urban | 4.5 | ||||
| Rural | 1.8 |
Abbreviation: NA, not available.
Table 2.
Studies on diabetes prevalence in China by city/province
| Reference | Tier | Region | Sample size | Age (years) | Year of survey | Prevalence (%) | Age-standardized prevalencea (%) |
|---|---|---|---|---|---|---|---|
| City level | |||||||
| Pan et al6 | 1 | Beijing | – | >25 | 1994 | 4.5 | 3.2 |
| Pan et al14 | 1 | Beijing | 29,859 | 30–64 | 1995 | – | 3.6 |
| Jia et al15 | 1 | Beijing | 2706 | >18 | 2005 | – | 7.6 |
| Zhu et al16 | 1 | Beijing | – | >15 | 2006 | 7.7 | – |
| Pan et al5 | 1 | Guangzhou | 775 | >20 | 2002 | 6.6 | 4.4 |
| Sheng et al17 | 1 | Shanghai | – | >30 | 1998 | 3.7 | 4.8 |
| Li et al18 | 1 | Shanghai | 11,589 | >15 | 2005 | 8.6 | 6.2 |
| Hu et al19 | 2 | Chengdu | 1445 | 20–74 | 2004 | 4.6 | 3.3 |
| Hu et al20 | 2 | Hangzhou | – | >15 | 2001 | 6.9 | 4.9 |
| Dong et al21 | 2 | Qingdao | 2634 | 20–74 | 2004 | – | 10.0 |
| Luo et al22 | 2 | Changsha | 5124 | 25–80 | 1994 | 6.1 | 5.4 |
| Huang et al23 | 3 | Nantong | 36,849 | >20 | 2006 | 4.8 | 3.4 |
| Zhong et al24 | 4 | Ganzhou | 2908 | >18 | 2006 | 4.4 | 3.1 |
| Feng et al25 | 4 | Jinzhong | 3000 | >20 | 2006 | 4.2 | 3.2 |
| Tan et al26 | 4 | Shaoyang | 786 | >20 | 2005 | 4.5 | 3.2 |
| Province level | |||||||
| Sun et al27 | Urban and rural | Hebei | 5892 | >25 | 2002 | 5.8 | – |
| Zhang et al28 | Urban and rural | Sichuan | 4641 | >3 | 2002 | 2.2 | 2.6 |
| Hu et al20 | Urban and rural | Zhejiang | 7417 | >35 | 2002 | 5.9 | – |
| Li et al29 | Urban and rural | Jilin | 1649 | All | 2005 | 3.5 | 2.5 |
| Ma et al30 | Urban and rural | Qinghai | 2276 | 20–74 | 2003 | 3.1 | 2.2 |
| Urban | Qinghai urban | – | – | 2003 | 4.5 | 4.7 | |
| Rural | Qinghai rural | – | – | 2003 | 1.5 | 1.0 |
Notes:
Age-standardized prevalence of diabetes was calculated if not reported in published study.
Table 3.
Estimation of baseline prevalence rate for 2009 based on analysis of available data
| City | Year of survey | Age-standardized prevalence (%) | Average of age-standardized prevalence (%) | Total population in 2009 (million) | Number of people with diabetes in 2009 (million) | Prevalence rate in 2009 (%) | |
|---|---|---|---|---|---|---|---|
| Urban | – | – | – | – | 596.945 | 31.410 | 5.2 |
| Tier 1 | Beijing | 2005 | 7.6 | 7.6 | 32.756 | 2.735 | 8.3 |
| Tier 2 | Chengdu | 2004 | 3.3 | 6.1 | 154.282 | 10.410 | 6.7 |
| Hangzho | 2006 | 4.9 | |||||
| Qingdao | 2004 | 10.0 | |||||
| Tier 3 | Nantong | 2005 | 5.4 | 5.4 | 113.857 | 6.903 | 6.0 |
| Tier 4 | Ganzhao | 2006 | 3.4 | 3.2 | 296.050 | 11.362 | 3.8 |
| Jinzhong | 2004 | 3.1 | |||||
| Shaoyang | 2006 | 3.2 | |||||
| Rural | – | – | – | 2.7a | 748.264 | 21.679 | 2.9 |
| Total | – | – | – | – | 1345.209 | 53.089 | 3.9 |
Notes:
Prevalence rate for rural area was assumed to be 80% of fourth tier prevalence rate in 2009.
Table 4.
Projections for the increase in prevalence rate in 2016 based on assumptions
| Age-standardized prevalence rate in 2009 (%) | Total population size in 2016 (million) | Assumptions | Number of people with diabetes in 2016 (million) | Growth (%/year) 2009–2016 | Prevalence rate in 2016 (%) | |
|---|---|---|---|---|---|---|
| Urban | 5.2 | 704.917 | – | 49.318 | 4.1 | 6.9 |
| Tier 1 | 8.3 | 38,751 | By 2016, the prevalence rate of tier 1 cities will reach the 2007 prevalence rate in Hong Kong | 3.790 | 2.3 | 9.8 |
| Tier 2 | 6.7 | 182,518 | By 2016, the prevalence rate of tier 2 cities will reach 90% of the 2007 prevalence rate in tier 1 cities | 15.008 | 2.9 | 8.2 |
| Tier 3 | 6.0 | 134,695 | By 2016, the prevalence rate of tier 3 cities will reach the 2007 prevalence rate in tier 2 cities | 9.902 | 2.8 | 7.3 |
| Tier 4 | 3.8 | 350,231 | By 2016, the prevalence rate of tier 4 cities will reach 90% of the 2007 prevalence rate in tier 3 cities | 20.618 | 6.3 | 5.8 |
| Rural | 2.9 | 701,624 | By 2016, the prevalence rate of rural area will reach the 2007 prevalence rate in tier 4 cities | 26.766 | 4.0 | 3.8 |
| Total | 3.9 | 1406.541 | – | 76.084 | 4.6 | 5.4 |
Results
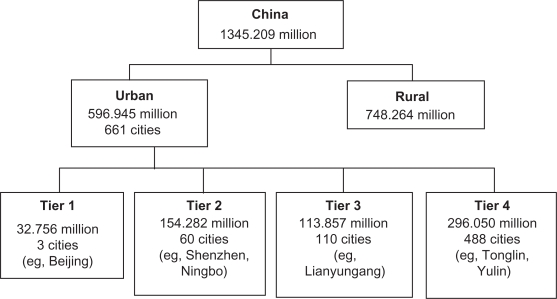
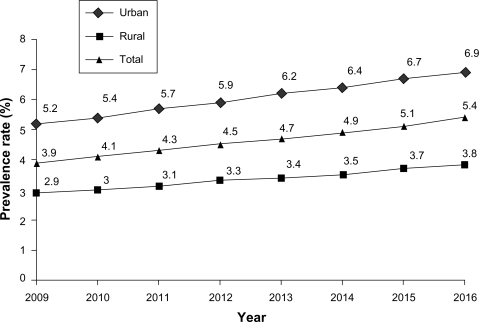
The literature search yielded 70 potentially relevant papers. Of these, 27 epidemiologic studies on diabetes prevalence rate in China were included, ie, five national studies with a large patient population and representative of entire China (Table 1) and 22 provincial/city level (Table 2) studies. Of the total Chinese population (1345 million), approximately 597 million resided in urban areas, while 748 million people resided in rural areas in 2009 (Figure 1). The estimated diabetes prevalence rates in China were 3.9% (urban 5.2%, rural 2.9%) in 2009 and were estimated to increase to 5.4% (urban 6.9%, rural 3.8%) in 2016. Accordingly, the total number of people suffering from diabetes is projected to rise from 53.1 million in 2009 to 76.1 million in 2016. From 2009 to 2016, the urban population is projected to increase more than the rural population (1.6-fold versus 1.2-fold). From 2009 to 2016, the number of diabetes cases in urban areas will increase from 31.4 million (59%) to 49.3 million (65%), while in rural areas it will increase from 21.7 million (41%) to 26.8 million (35%). The prevalent population, prevalence rates, and CAGR for all the four tiers are presented in Table 3. The CAGR calculated from 2009 to 2016 was 4.6%, describing the rate at which prevalence might grow, if it grew at a steady rate. The prevalence increase in the urban, rural, and total Chinese population by year is presented in Figure 2.
Figure 1.
Flow chart of the distribution of Chinese population in 2009.
Figure 2.
Projected rate of diabetes prevalence in China.
Discussion
We estimate the number of adult patients with diabetes in China to have been approximately 53.1 million in 2009 and that it will increase to about 76.1 million in 2016, with an annual growth rate of 4.6%. These numbers are much higher than the previous estimates of 39.8 million adult patients with diabetes in 2007 and 59.3 million in 2025.34 Because we used the same total population size as reported in previous papers for calculating 2009 and 2016 prevalence, demographic changes cannot account completely for the difference in estimated prevalence. However, the higher prevalence can potentially be explained by the inclusion of recent studies that reported a higher prevalence of diabetes, or has less stringent inclusion criteria (eg, studies considering only fasting plasma glucose >7.0 mmol/L) for diagnosis of diabetes. However, our data are confirmed by more recent data provided by the International Diabetes Federation.47
The present study shows that the prevalence of diabetes in China in 2009 is higher in urban areas (5.2%, 31.4 million people) than in rural areas (2.9%, 21.6 million people). In the urban population, the projected diabetes prevalence in first tier cities increased from 2.7 million (8.3%) to 3.7 million (9.8%), while that in fourth tier cities increased from 11.3 million (3.8%) to 20.6 million people (5.8%). These findings are in agreement with those of previous epidemiologic studies conducted in China.7–9,16,35 Furthermore, our findings also underscore the increasing importance of obesity as the strongest risk factor for the development of diabetes in China, which in turn is caused by excessive consumption of high-calorie food and declining physical activity, a phenomenon which is particularly evident in urban communities.36–39 The present study reported an estimated prevalence rate of 3.9% in 2009, which is comparable with an earlier reported prevalence rate of 3.9% for China in 2007.40 An earlier study showed that the diabetes prevalence rate in China is lower than that in Hong Kong and Singapore, where estimated rates are 9%–12%.38,41 Hong Kong, being one of the most cosmopolitan cities in the world, can be considered as the demographic prototype of China in the future.42 Rapid changes in lifestyle, such as an increasingly high-fat diet, physical inactivity, and psychosocial stress might unmask a genetic predisposition of some individuals to develop diabetes.43 Therefore, based on trends suggested by the available data, we predict that the diabetes prevalence rate in first tier Chinese cities will reach the level of Hong Kong’s 2007 prevalence by 2016. Although the present study suggests a high diabetes prevalence in China, our data likely still underestimates the real burden of diabetes, since many diabetic patients are undiagnosed or are diagnosed late.44,45 Our findings are in agreement with data from other large Asian countries. India, which is undergoing the same development as China, is facing an even higher and rapidly increasing burden of diabetes, with an estimated 50 million people suffering from diabetes today, and projected to increase to 87 million people by 2030.47 Thus, in the light of the expected high prevalence of diabetes in 2016, rigorous efforts are required to improve on prevention strategies and diagnosis of diabetes by putting in place effective public health policies. This would be important in light of the fact that Type 2 diabetes can be delayed or even prevented by lifestyle counseling or drug therapy in the primary care setting.46
The strength of our study is that that we analyzed data published during the past two decades, in both English and Chinese languages, representing adult populations from all over China, including rural and urban populations. The limitations of our study are that the prevalence of diabetes was based solely on the growth in Chinese population, no modifications were made for possible increases in age-specific prevalence over time, and we searched the selected papers from 1987 to 2007, hence more recent publications were not included in the analysis.
Taken together, our results predict a constant rise in the prevalence of diabetes in China from 2009 to 2016, at an annual growth rate of 4%–5%. The much higher current diabetes burden in China than that observed in earlier studies represents a serious concern for the Chinese health care system. Even though there are national education programs on diabetes in China (eg, Project HOPE), our findings point to the necessity for developing further strategies for diabetes prevention, awareness, and early diagnosis of the disease, in order to reduce the economic and societal burden of the disease and its long-term complications.
Acknowledgments
The authors would like to thank Yinuo Li for her support in the data analysis.
Footnotes
Disclosures
SS and MT are employees of Sanofi-aventis, China.
References
- 1.Gan D. Diabetes Atlas 2000. Brussels: International Diabetes Federation; 2001. [Google Scholar]
- 2.World Health Statistics 2008. Available from: http://www.who.int/mediacentre/factsheets/fs312/en/. Accessed Jan 5, 2010.
- 3.Sicree R, Shaw J, Zimmet P. Prevalence and projections. In: Gan D, editor. Diabetes Atlas. 3rd ed. Brussels: International Diabetes Federation; 2006. [Google Scholar]
- 4.Pan C. Diabetes care in China: Meeting the challenge. Diabetes Voice. 2005;50(11):9–12. [PubMed] [Google Scholar]
- 5.Pan B, Qiu X, Fang F, et al. The prevalence and risk factors of diabetes mellitus in residents of Dongshan and Yuexiu district of Guangzhou. Mod Prev Med. 2005;32:516–517. [Google Scholar]
- 6.Pan XR, Yang WY, Li GW, Liu J. Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care. 1997;20(11):1664–1669. doi: 10.2337/diacare.20.11.1664. [DOI] [PubMed] [Google Scholar]
- 7.Yang Z. A survey of diabetes prevalence in the middle-aged and elderly Chinese from 12 areas of China. Chin J Endocrinol Metabol. 2002;18:280–284. [Google Scholar]
- 8.Dong Y, Gao W, Nan H, et al. Prevalence of type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabet Med. 2005;22:1427–1433. doi: 10.1111/j.1464-5491.2005.01658.x. [DOI] [PubMed] [Google Scholar]
- 9.Gu D, Gupta A, Muntner P, et al. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: Results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia) Circulation. 2005;112(5):658–665. doi: 10.1161/CIRCULATIONAHA.104.515072. [DOI] [PubMed] [Google Scholar]
- 10.He Y, Jiang B, Wang J, et al. Prevalence of the metabolic syndrome and its relation to cardiovascular disease in an elderly Chinese population. J Am Coll Cardiol. 2006;47(8):1588–1594. doi: 10.1016/j.jacc.2005.11.074. [DOI] [PubMed] [Google Scholar]
- 11.State Food and Drug Administration . Analysis of Patient Population outside Japan. Southern Medicine Economic Research Institute; 2004. [Google Scholar]
- 12.Oxford Wanfang Digital Resources Available from: http://www1.wanfangdata.com/oxford.asp. Accessed Jan 5, 2010.
- 13.Li LM, Rao KQ, Kong LZ, et al. for The Technical Working Group of China National Nutrition and Health Survey A description on the Chinese National Nutrition and Health Survey in 2002. Chin J Epidemiol. 2005;26(7):478–484. [PubMed] [Google Scholar]
- 14.Pan C, Lu J, Tian H. Epidemiology of adult diabetes mellitus in a population of Capital Iron and Steel Company in Beijing. Zhonghua Yi Xue Za Zhi. 1995;75(7):409–413. [PubMed] [Google Scholar]
- 15.Jia J. Prevalence of diabetes mellitus for residence of Haidian district, Beijing. Mod Prev Med. 2007;34(20):3869–3871. [Google Scholar]
- 16.Zhu L. Issues in the treatment of diabetes mellitus in the community. Chinese Community Doctors. 2006;22(4):22. [Google Scholar]
- 17.Sheng Z, Liu M, Wang Y, et al. A survey of diabetes prevalence in 9376 urbanite adults of Shanghai. Chinese J Diabet. 2001;9(4):214–217. [Google Scholar]
- 18.Li R, Lu W, Jia WP, et al. Cross-sectional investigation of prevalence of type 2 diabetes in Shanghai. Zhonghua Yi Xue Za Zhi. 2006;86(24):1675–1680. [PubMed] [Google Scholar]
- 19.Hu R, Zhang Y. Prevalence survey of diabetes mellitus in Shuangliu, Chengdu. J Prevent Med Info. 2006;22(1):92–93. [Google Scholar]
- 20.Hu R, Han X, Zhong J, Yu M. Study on the morbidity of type 2 diabetes and risk factors among residents from two communities of Zhejiang province. Dis Surveill. 2005;20(3):151–153. [Google Scholar]
- 21.Dong Y, Nan H, Gao W, et al. Prevalence of the metabolic syndrome among adults aged 20∼74 years in Zhanshan community of Qingdao. Chinese J Diabet. 2004;12(3):177–181. [Google Scholar]
- 22.Luo H, Qu G, et al. Diabetes mellitus prevalence survey of 5124 residence in Changsha city. Bull Hun Med Univ. 1996;21(3):217–220. [Google Scholar]
- 23.Huang J, Wu G, Chen D, et al. Epidemiological survey of diabetes mellitus in Nantong city. Med J Comm. 2006;20(4):469–472. [Google Scholar]
- 24.Zhong G, Lu W, Dong M, et al. A survey on diabetes prevalence in 2908 public officials of Ganzhou city. J Gannan Med Univ. 2007;27(3):334–338. [Google Scholar]
- 25.Feng Y, Meng R, Fan Z. Survey of prevalence of diabetes mellitus among the population of Jin Zhong city. Shanxi Med J. 2007;36(9):803–804. [Google Scholar]
- 26.Tan W, Li Z, Liu H, et al. Type II diabetes risk factor analysis for residence of Shaoyang city. J Practical Diabetol. 2007;3(5):16–18. [Google Scholar]
- 27.Sun J, Zhang J, Cao L, et al. Prevalent state survey on adult residents with chronic metabolic diseases in the rural communities of Hebei province. Chinese General Pract. 2004;7:1584–1586. [Google Scholar]
- 28.Zhang N-M, Li D, Ping W, et al. The epidemic characteristics of diabetes among residents in rural and urban area in Sichuan. Chinese Chronic Dis Prevention Control. 2007;15:462–464. [Google Scholar]
- 29.Li Z-Y, Guan X, Ding D, et al. Epidemiological survey of diabetes mellitus in urban and rural communities in Jilin province. Chinese Tropical Med. 2007;7:806–808. [Google Scholar]
- 30.Ma X, Li Z, Zou L, et al. Survey of diabetes mellitus prevalence in Qinghai province. Qinghai J Med. 2004;34(2):57–59. [Google Scholar]
- 31.National Bureau of Statistics of China 1981–2006. Available from: http://liber8.stlouisfed.org/iesd/details/3075/. Accessed Jan 5, 2010.
- 32.China Statistics Press; 2007. China Population Statistics Yearbook 2007. [Google Scholar]
- 33.2000 China Population Census Data Assemblies. Available from: www.eastview.com/Files/EV%20CDC%20DataAssemblies.pdf. Accessed Jan 5, 2010.
- 34.International Diabetes Federation . Diabetes Atlas – Third Edition. Brussels: International Diabetes Federation; 2006. [Google Scholar]
- 35.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 36.Cheng TO. Epidemic of diabetes in China. Med J Aust. 2003;179(11–12):586. doi: 10.5694/j.1326-5377.2003.tb05706.x. [DOI] [PubMed] [Google Scholar]
- 37.Yoon K-H, Lee J-H, Kim J-W, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368(9548):1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 38.Wong KC, Wang Z. Prevalence of type 2 diabetes mellitus of Chinese populations in Mainland China, Hong Kong, and Taiwan. Diabetes Res Clin Pract. 2006;73(2):126–134. doi: 10.1016/j.diabres.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 39.Qiao Q, Hu G, Tuomilehto J, Nakagami T, et al. for DECODA Study Group Age- and sex-specific prevalence of diabetes and impaired glucose regulation in 11 Asian cohorts. Diabetes Care. 2003;26(10):1770–1780. doi: 10.2337/diacare.26.6.1770. [DOI] [PubMed] [Google Scholar]
- 40.Diabetes Global Prevalence Available from: www.boehringer-ingelheim.com/corporate/news/presspack/corporate/rd_2008/pdf/diabetes_prevalence.pdf. Accessed Jan 5, 2010.
- 41.World Diabetes Foundation . The Health of the Chinese. 2007. Available from: www.cdc.gov/TB/EthnographicGuides/China/chapters/chapter3.pdf. Accessed Jan 5, 2010. [Google Scholar]
- 42.Chan NN, Kong APS, Chan JCN. Metabolic syndrome and Type 2 diabetes: The Hong Kong perspective. Clin Biochem Rev. 2005;26(3):51–57. [PMC free article] [PubMed] [Google Scholar]
- 43.CUHK urges for comprehensive assessment and treatment for young onset diabetes. Press release. Available from: http://www.cuhk.edu.hk/ipro/000928e(1).htm. Accessed Jan 5, 2010.
- 44.Jia WP, Pang C, Chen L, et al. Epidemiological characteristics of diabetes mellitus and impaired glucose regulation in a Chinese adult population: The Shanghai Diabetes Studies, a cross-sectional 3-year follow-up study in Shanghai urban communities. Diabetologia. 2007;50:286–292. doi: 10.1007/s00125-006-0503-1. [DOI] [PubMed] [Google Scholar]
- 45.Hu D, Fu P, Xie J, et al. for the InterASIA Collaborative Group Increasing prevalence and low awareness, treatment and control of diabetes mellitus among Chinese adults: The InterASIA study. Diabetes Res Clin Pract. 2008;81(2):250–257. doi: 10.1016/j.diabres.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 46.Lauritzen T, Borch-Johnsen K, Sandbæk A. Is prevention of Type 2 diabetes feasible and efficient in primary care? A systematic PubMed review. Prim Care Diabetes. 2007;1(1):5–11. doi: 10.1016/j.pcd.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 47.International Diabetes Federation . Diabetes Atlas 2009. 4th ed. International Diabetes Federation; 2009. [Google Scholar]