Abstract
Objective To examine prospective relationships between caregiver's depressive symptoms and child asthma morbidity among inner-city African American families. Methods Phone surveys were conducted 6 months apart with 262 African American mothers of children with asthma. Cross-lagged structural path analysis was used for data analyses. Results Using goodness-of-fit indices, the final model for asthma symptoms had a good fit to the data. Time 1 (T1) maternal depressive symptoms predicted T2 child asthma symptoms (β =.16, p <.01); however, T1 asthma symptoms did not predict T2 maternal depressive symptoms (β =.03, non-significant). In contrast, in the final model for emergency department (ED) visits there was no predictive association between maternal depressive symptoms and ED visits. Conclusion Maternal depressive symptoms may have a detrimental effect on child asthma morbidity among inner-city African American families, rather than vice versa. Ameliorating maternal depressive symptoms may result in better asthma outcomes for inner-city children.
Keywords: African American, asthma, depressive symptoms, inner-city
Asthma is a major cause of childhood morbidity and mortality in the USA, and ethnic minority and inner-city children with asthma are disproportionately affected by adverse asthma outcomes. African American children are 2.6 times more likely to visit the emergency department (ED), 2.5 times more likely to be hospitalized, and 5 times more likely to die as a result of asthma compared to their non-Hispanic White counterparts (Akinbami, 2006). Latino children as a whole are twice as likely to visit the ED (Akinbami, Moorman, Garbe, & Sondik, 2009) due to asthma as non-Hispanic White children.
To reduce asthma disparities among children, it is critical to identify the modifiable factors associated with asthma morbidity among inner-city ethnic minority children. Studies have identified environmental, cultural, and psychosocial factors that may contribute to inner-city asthma disparities. Environmental factors linked to an increase in asthma morbidity include inadequate access and quality medical care (Lara et al., 2002), exposure to secondhand smoke (U.S. Department of Health and Human Services, 2006), and indoor asthma allergen exposures due to poor housing stock (Rosenstreich et al., 1997; Eggleston, 2000).
Culturally specific asthma beliefs and treatment practices (Koinis-Mitchell et al., 2008) and stress associated with adapting to the language and mainstream American cultural norms (Koinis-Mitchell et al., 2007) may pose additional barriers in reducing asthma disparities among ethnic minority families. For example, African American and Latino families are more likely to use complementary and alternative therapies (CAM) to treat asthma than White families; however the type of CAM used varies by ethnic group (Adams, Murdock, & McQuaid, 2007). Aggregating findings across ethnic groups could potentially mask distinct predictors of child asthma morbidity. Thus, it is critical to understand culturally specific predictors of asthma morbidity within the unique sociocultural context of an ethnic group.
Psychosocial stressors such as maternal depression (Shalowitz et al., 2006), lack of social support (Wade et al., 1997), stressful life events (Turyk et al., 2008), and exposure to neighborhood violence (Wright et al., 2004) have been linked to asthma disparities. Given that low-income minority families experience these risk factors at higher rates than other populations, they are important to consider when evaluating asthma disparities in these high-risk populations. Thus, our study focused on the prospective relationships between maternal depressive symptoms and child asthma morbidity among African American inner-city families.
Maternal Depressive Symptoms and Pediatric Asthma Morbidity
Mothers of children with asthma experience higher rates of depressive symptoms than mothers of children without asthma (Shalowitz et al., 2006). The rate of clinically significant levels of depressive symptoms ranges from 34% (Siefert, Finlayson, Williams, Delva, & Ismail, 2007) among inner-city mothers in general to 47% among mothers of children with asthma (Bartlett et al., 2001). This is noteworthy, given that mothers as primary caregivers play an important role in managing pediatric asthma (Kaugars, Klinnert, & Bender, 2004). Moreover, in the National Cooperative Inner-City Asthma Study, the caregiver's mental health status was the strongest predictor of asthma hospitalizations (Wade et al., 1997). Thus, maternal depressive symptoms among caregivers of children with asthma are important factors to consider when discussing asthma management and increased asthma morbidity among at-risk children.
Several studies have demonstrated an association between maternal depressive symptoms and increased child asthma morbidity (Weil et al., 1999; Bartlett et al., 2001; Shalowitz, Berry, Quinn, & Wolf, 2001; Brown et al., 2006). However, the directionality of this relationship remains unknown. The presence of depressive symptoms may impair a mother's ability to adhere to treatment (Bartlett et al., 2004) and make appropriate decisions about seeking medical care (Bartlett et al., 2001), which may negatively impact the child's asthma morbidity (Weil et al., 1999; Kaugars et al., 2004). In contrast, having a child with high asthma morbidity may contribute to a caregiver's distress and risk of mental illness (Shalowitz et al., 2001; Bartlett et al., 2004) due to the additional burden of existing social stressors from living in the inner city (Shalowitz et al., 2006). Finally, a reciprocal relationship between a mother's depressive symptoms and child asthma morbidity may exist whereby maternal depressive symptoms lead to increased child asthma morbidity, while concurrently high asthma morbidity perpetuates and potentially exacerbates the maternal depressive symptoms.
Although several prospective studies have been conducted in this area, no studies explicitly tested the reciprocity and/or the directionality of the relationship between maternal depressive symptoms and child asthma morbidity among inner-city families. Understanding reciprocity or the directionality of the relationship between depressive symptoms and asthma morbidity is critical to identifying targets of intervention to reduce asthma disparities. For instance, if the influence of maternal depressive symptoms on child asthma morbidity is confirmed, pediatric psychologists could help reduce asthma morbidity among inner-city children by targeting maternal depressive symptoms. Alternatively, if the influence of child asthma morbidity on maternal depressive symptoms is confirmed, effective management of the child's asthma could reduce maternal depressive symptoms. It may, however, be necessary to address both maternal depressive symptoms and child asthma management concurrently or sequentially to have a lasting impact on asthma morbidity. To address this gap in knowledge, we examined the potential reciprocal relationship between maternal depressive symptoms and child asthma morbidity with a sample of inner-city African American children with asthma in a prospective cohort study.
Hypotheses
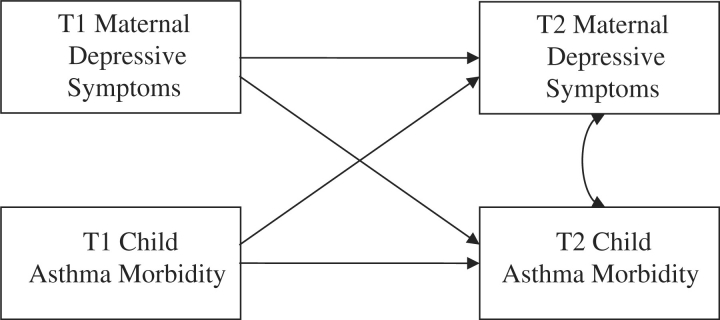
We tested four competing models to determine the directionality of the relationship between maternal depressive symptoms and child asthma morbidity. In all of the models, we statistically controlled for stability of the constructs over time (“stability coefficients model”). First, the “reciprocal effects model” specified that both maternal depressive symptoms and child asthma morbidity at Time 1 (T1) would simultaneously predict subsequent (T2) child asthma morbidity and maternal depressive symptoms, respectively (Figure 1). Second, the “depressive symptoms effect model” specified that only maternal depressive symptoms would predict subsequent child asthma morbidity. Third, the “asthma morbidity effects model” specified that only child asthma morbidity would predict subsequent maternal depressive symptoms. We hypothesized that for each outcome the reciprocal effects model would provide a better fit to the data than either depressive symptoms effects alone or asthma morbidity effects alone. We repeated the tests of these models separately for two morbidity outcomes: frequency of asthma symptoms (Hypothesis 1) and ED visits (Hypothesis 2).
Figure 1.
Full analytic model for the longitudinal relationship between maternal depressive symptoms and child asthma morbidity.
Methods
Procedures
This study is based on the secondary analysis of a dataset from a randomized control trial to reduce ED use among high-risk inner-city children with asthma. The intervention and the outcomes of this study are described elsewhere (Otsuki et al., in press). The aim of this randomized controlled trial was to test the efficacy of asthma education combined with medication adherence feedback intervention and an asthma education alone in reducing asthma morbidity, compared to usual care among inner-city children with asthma who were recruited from the Pediatric ED. All participants completed surveys at baseline and 6 months after randomization. We obtained informed consent from eligible mothers who completed phone surveys at a baseline assessment (T1) and 6 months later (T2). The selection of the observation period (6 months) was chosen to permit sufficient time to administer the intervention and allow for increased medication adherence to have an effect on symptoms. The 6-month observation period also allowed for sufficient time to document changes in healthcare utilization. The Johns Hopkins Medical Institutions Institutional Review Board reviewed and approved the study.
Participants
We recruited children with asthma from a large mid-Atlantic urban pediatric ED by weekly review of ED records between January 2001 and March 2003. Children were eligible to participate in the study if they had physician-diagnosed asthma, had two ED visits or one hospitalization due to asthma in the preceding 6 months, and were between the ages of 2 and 12 years. Study design considerations, recruitment procedures, intervention, and participant characteristics are described elsewhere (Otsuki et al., in press). Of the 377 families (65% of those eligible) who completed the T1 survey, 302 (80%) completed T2 surveys. Of these, 262 (87%) had both surveys completed by the child's mother and were included in the final analyses. Demographic characteristics of the participants are summarized in Table I.
Table I.
Demographic Characteristics (N = 262)
| Characteristic | n (%) |
|---|---|
| Child age in years, M (SD) | 6.68 (3.38) |
| Child gender, percentage male | 162 (61.8) |
| Child ethnicity, percentage African American | 262 (100.0) |
| Health insurance type, percentage Medicaid | 221 (84.4) |
| Maternal age in years, M (SD) | 30.17 (7.35) |
| Maternal education, percentage completed high school or beyond | 180 (68.7) |
| Household income | |
| <$10,000 | 102 (40.3) |
| $10–19,999 | 58 (22.9) |
| $20–29,999 | 42 (16.6) |
| $30–39,999 | 26 (10.3) |
| >$40,000 | 25 (9.9) |
| NAEPP guideline-based severity | |
| Mild–intermittent | 116 (44.3) |
| Mild–persistent | 20 (7.6) |
| Moderate–severe persistent | 126 (48.1) |
Measures
Asthma Morbidity
We calculated the number of asthma symptoms per month by averaging the caregiver-reported number of days of restricted activity due to asthma and number of nights with asthma symptoms in the past 6 months; this method is described in detail elsewhere (Bartlett et al., 2001). Asthma severity levels were derived from the 2007 NAEPP guideline criteria (National Heart & National Asthma Educationand Prevention Program, 2007) using daytime and nighttime asthma symptoms frequency. Caregivers also reported the number of ED visits in the past 6 months due to a child's asthma. Prior research has found that maternal recall of their child's acute healthcare events within the last 12 months was high: 75–96% agreement with medical record information and was not associated with maternal depression (D'Souza-Vazirani, Minkovitz, & Strobino, 2005).
Maternal Depressive Symptoms
We assessed maternal depressive symptoms using an abridged, 11-item version of the Center for Epidemiological Studies Depression (CES-D) Scale, as described elsewhere (Bartlett et al., 2001; Smith et al., 2006). The CES-D is widely used in general and psychiatric populations and the abridged version has been found to have reliability and validity comparable to the full scale (Irwin, Artin, & Oxman, 1999; Bartlett et al., 2001). The internal consistency for the current study was satisfactory (α =.82 at T1; α =.79 at T2).
Statistical Analyses
The objective of this study was to investigate the relationship between maternal depressive symptoms and asthma morbidity, as measured by the number of asthma symptoms per month and ED visits in the last 6 months. Cross-lagged path models were specified to examine this prospective relationship using AMOS 6.0 (Arbuckle, 2005). We used separate models to estimate asthma symptoms and ED visits because these variables were correlated.
Nested model comparisons were used to evaluate the model fit. First, we specified the hypothesized full reciprocal-effect model with one degree of freedom. Then, we compared the alternative models (one removing the path from T1 child asthma morbidity to T2 maternal depressive symptoms, and the other removing the path from T1 maternal depressive symptoms to T2 child asthma morbidity) against the full model. Finally, the model without cross-lags (i.e. stability coefficients only) was compared to one of the alternative models that provided a better fit to the data. We used the following criteria to examine model fit: significant χ2 values indicating poor model fit; Tucker-Lewis Index (TLI) (Tucker & Lewis, 1973) and Comparative Fit Index (CFI) (Bentler, 1990) with values >.95 representing a good fit (Hu & Bentler, 1999); root mean square error of approximation (RMSEA) with values <.05 indicating a good fit (Browne & Cudeck, 1992); and smaller values on Akaike's Information Criterion (AIC) (Akaike, 1987) representing a good fit.
Because half of our participants received an asthma self-management educational intervention, we used multigroup analysis (Bollen, 1989) to explore whether the final models were equivalent across intervention and non-intervention groups. The final best-fit models were simultaneously fit for intervention and non-intervention groups, while all path coefficients were constrained to be equal across these groups; then we estimated the unconstrained model allowing all the estimates to be different for each group (Bollen, 1989)
To reduce potential bias in the findings due to incomplete data, we conducted all path analyses using the full-information maximum likelihood estimation method. However, listwise deletion for missing data was used when conducting t-tests. With respect to statistical power, Kline (2005) recommends 10 times as many cases as freely estimated parameters. The maximum numbers of parameters estimated in this study were 13. Given the final sample size (N = 262), the ratios between the maximum numbers of parameter estimates were 20:1 for nested model comparisons, representing sufficient power to produce reliable estimates.
Results
Descriptive Statistics
Table II presents correlations, item means, and standard deviations for study variables. Maternal depressive symptoms, asthma symptoms, and ED visits decreased significantly over time, t(256) = 4.41, t(261) = 4.13, and t(252) = 10.70, p <.001, respectively. However, these variables were moderately stable over time, suggesting that rank-ordering of the individuals on these variables did not vary. Cross-sectional correlations showed that maternal depressive symptoms were associated with child asthma symptoms and ED visits at T2 but not at T1. Correlations between T1 and T2 variables indicated that maternal depressive symptoms were significantly associated with subsequent asthma symptoms, but not with ED visits. Neither frequency of asthma symptoms nor ED visits were prospectively associated with maternal depressive symptoms. Table III shows the relationship between demographic variables and the variables included in the model; as expected lower socioeconomic status (i.e. lower income and maternal education) was significantly associated with maternal depressive symptoms.
Table II.
Intercorrelations and Descriptive Statistics for Study Variables (N = 262)
| 1 | 2 | 3 | 4 | 5 | M | SD | Range | |
|---|---|---|---|---|---|---|---|---|
| 1. T1 maternal depressive symptoms | – | 17.80 | 11.79 | 0.00–49.14 | ||||
| 2. T1 asthma symptoms per month | –0.03 | –- | 6.57 | 7.16 | 0.00–30.33 | |||
| 3. T1 ED visits in the last 6 months | 0.04 | 0.26*** | – | 2.54 | 1.97 | 0.00–10.00 | ||
| 4. T2 maternal depressive symptoms | 0.51*** | –0.01 | 0.03 | – | 14.63 | 10.61 | 0.00–54.60 | |
| 5. T2 asthma symptoms per month | 0.14* | 0.38*** | 0.33*** | 0.24*** | – | 4.72 | 5.73 | 0.00–30.33 |
| 6. T2 ED visits in the last 6 months | 0.06 | 0.15* | 0.43*** | 0.14* | 0.42*** | 1.35 | 1.65 | 0.00–10.00 |
*p <.05; **p <.01; ***p <.001.
Table III.
Descriptive Statistics for the Study Variables by the Baseline Demographic Variables and Randomized Groups
| T1 Depression M (SD) | T1 Symptoms M (SD) | T1 ED visits M (SD) | T2 Depression M (SD) | T2 Symptoms M (SD) | T2 ED visits M (SD) | |
|---|---|---|---|---|---|---|
| Age | ||||||
| 2–5 (n = 124) | 19.62 (11.63) | 6.70 (7.12) | 2.95 (2.12) | 15.19 (9.96) | 4.81 (5.75) | 1.62 (1.82) |
| 6–12 (n = 138) | 16.16 (11.74) | 6.46 (7.22) | 2.16 (1.76) | 14.12 (11.17) | 4.64 (5.73) | 1.12 (1.44) |
| p-value | .02 | .62 | .001 | .42 | .97 | .01 |
| Gender | ||||||
| Male (n = 162) | 17.49 (11.57) | 6.41 (7.17) | 2.67 (2.06) | 14.76 (10.20) | 5.13 (5.76) | 1.48 (1.80) |
| Female (n = 100) | 18.32 (12.20) | 6.84 (7.18) | 2.32 (1.82) | 14.41 (11.29) | 4.04 (5.66) | 1.15 (1.34) |
| p-value | .58 | .56 | .16 | .80 | .07 | .16 |
| Income | ||||||
| <$10,000 (n = 102) | 20.34 (11.62) | 6.74 (7.16) | 2.51 (1.76) | 16.89 (11.87) | 5.29 (6.57) | 1.46 (1.69) |
| ≥$10,000 (n = 151) | 15.77 (11.45) | 6.45 (7.21) | 2.54 (2.11) | 13.09 (9.60) | 4.23 (5.02) | 1.25 (1.61) |
| p-value | .002 | .57 | .54 | .006 | .35 | .35 |
| Caregiver education | ||||||
| <High school (n = 82) | 22.32 (11.27) | 6.40 (7.15) | 2.54 (1.77) | 18.11 (11.62) | 5.74 (6.65) | 1.44 (1.43) |
| ≥High school (n = 180) | 15.76 (11.49) | 6.65 (7.18) | 2.54 (2.06) | 13.04 (9.75) | 4.25 (5.21) | 1.31 (1.74) |
| p-value | .001 | .75 | .61 | .0001 | .13 | .33 |
| Intervention group | ||||||
| No intervention (n = 128) | 17.71 (11.46) | 5.82 (7.22) | 2.30 (1.61) | 14.91 (10.60) | 4.69 (5.49) | 1.31 (1.54) |
| Intervention (n = 134) | 17.89 (12.16) | 7.30 (7.06) | 2.76 (2.25) | 14.36 (10.65) | 4.74 (5.98) | 1.48 (1.75) |
| p-value | .90 | .09 | .06 | .68 | .93 | .66 |
Path Analyses
The results of nested model comparisons for models for asthma symptoms and ED visits are summarized in Table IV. Because the covariances between T1 depressive symptoms and T1 asthma morbidity (asthma symptoms or ED visits) were not statistically significant, they were removed from specifying the models for both asthma symptoms and ED visits.
Table IV.
Nested Model Comparison Results for Asthma Symptoms and ED Visits (N = 262)
| Model | χ2 | Number of parameters | TLI | CFI | RMSEA (90% CI) | AIC | Comparison | Δχ2 | df | p |
|---|---|---|---|---|---|---|---|---|---|---|
| Asthma symptoms | ||||||||||
| Reciprocal effects | .25 | 13 | 1.06 | 1.00 | .00 (.00–.13) | 26.25 | – | – | 1 | .62 |
| Asthma morbidity effects | .27 | 12 | 1.07 | 1.00 | .00 (.00–.06) | 24.27 | M2–M1 | .02 | 2 | .99 |
| Depressive symptoms effect | 7.23 | 12 | 0.79 | 0.96 | .10 (.03–.18) | 31.23 | M3–M1 | 6.98 | 2 | .008 |
| Stability coefficients | 7.25 | 11 | 0.89 | 0.97 | .07 (.00–.14) | 29.25 | M4–M2 | 6.98 | 3 | .008 |
| ED visits | ||||||||||
| Reciprocal effects | .22 | 13 | 1.06 | 1.00 | .00 (.00–.13) | 26.22 | – | – | 1 | .64 |
| Asthma morbidity effects | .27 | 12 | 1.07 | 1.00 | .00 (.00–.06) | 24.26 | M2–M1 | .05 | 2 | .82 |
| Depressive symptoms effect | 1.36 | 12 | 1.03 | 0.99 | .00 (.00–.11) | 25.36 | M3–M1 | 1.14 | 2 | .28 |
| Stability coefficients | 1.40 | 11 | 1.04 | 1.00 | .00 (.00–.08) | 23.40 | M4–M2 | 1.13 | 3 | .29 |
M1: Model 1.
Test of Hypothesis 1: Asthma Symptoms
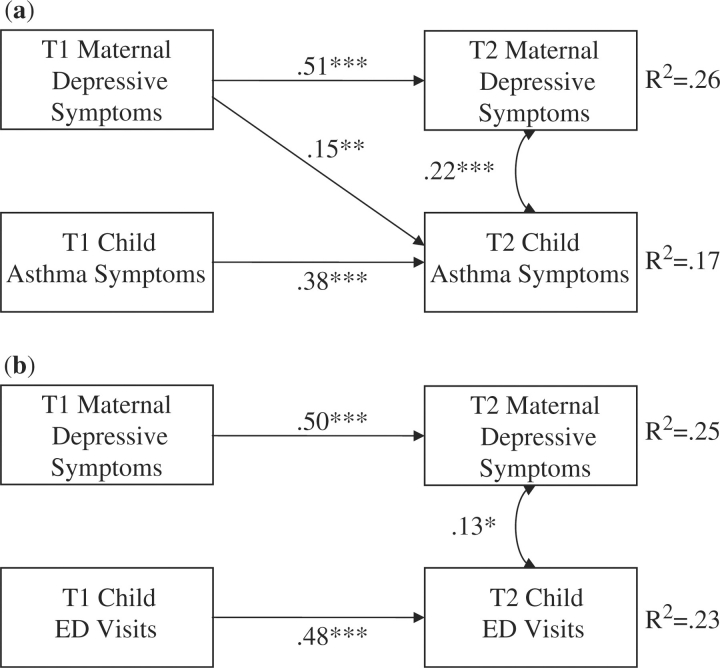
We constructed the full model with cross-lags (representing the reciprocal effects model, or Model 1) for asthma symptoms, and found that all paths were significant except the path linking T1 child asthma symptoms and T2 maternal depressive symptoms (β =.01). To test for the most parsimonious model fit, alternative models were constructed. In Model 2, the path from T1 child asthma symptoms to T2 caregiver depressive symptoms (representing asthma morbidity effect) was removed. Statistically non-significant chi-square test of difference suggested that we should not include this path in further model testing. In Model 3, the path from T1 caregiver depressive symptoms to T2 child asthma symptoms (representing depressive symptoms effect) was removed while keeping the path from T1 asthma symptoms to T2 depressive symptoms in the model. Chi-square test comparing Model 1 and Model 3 was statistically significant, suggesting that Model 3 is a worse fit to the data. Thus, Model 2 was considered to provide a better fit to the data. Finally, in Model 4, both cross-lag paths were removed and only stability paths remained in the model. The statistically significant chi-square difference test comparing the Model 4 and Model 2 suggested that the path from T1 caregiver depressive symptoms and T2 child asthma symptoms should be kept in the final model. In the final model (Model 2), T1 maternal depressive symptoms predicted T2 child asthma symptoms (β =.15, p <.01) above and beyond the stability of both maternal depressive symptoms and child asthma symptoms (Figure 2a).
Figure 2.
(a) Final prospective path model with standardized path coefficients and correlations for the significant paths between maternal depressive symptoms and child asthma symptoms. (b) Final prospective path model with standardized path coefficients and correlations for the significant paths between maternal depressive symptoms and child ED visits. *p <.05; **p <.01; *** p <.001.
Test of Hypothesis 2: ED Visits
In the full model with cross-lags for ED visits, both stability coefficients were statistically significant. The paths linking (a) T1 depressive symptoms and T2 ED visits and (b) T1 ED visits and T2 depressive symptoms were not significant (β =.06 and.01, respectively). We followed the same procedure described above to test the final model. Neither the depressive symptoms effect only model (Model 2) nor the asthma morbidity effect model (Model 3) had significantly better model fit than the reciprocal effect model (Model 1). Removing both cross-lags (Model 4) did not worsen the model fit. Thus, when using ED visits as a measure of asthma morbidity, only stability coefficients (Model 4) were statistically significant (Figure 2b).
Testing the Moderating Effect of Exposure to Intervention
As described above we tested whether the final models were equivalent between the intervention and non-intervention groups using a multigroup analysis. For the asthma symptoms final model, the fit indices were as follows: (a) constrained model: χ2(3) = 1.93, p =.96; CFI = 1.00, TLI = 1.12, RMSEA (90% CI) =.00 (.00–.04), AIC = 43.93; and (b) unconstrained model: χ2(4) =.38, p =.98; CFI = 1.00, TLI = 1.15, RMSEA (90% CI) =.00 (.00–.04), AIC = 48.38. Therefore, the unconstrained model did not provide superior fit to the data than the constrained model, ▵χ2(3) = 1.55, p =.67, indicating that the final asthma symptoms models were equivalent across the intervention and non-intervention groups. Similarly, for the ED visits final model, the unconstrained model—χ2(6) = 3.27, p =.77; CFI = 1.00, TLI = 1.08, RMSEA (90% CI) =.00 (.00–.05), AIC = 47.27—did not provide significantly better fit to the data than did the constrained model—χ2(8) = 4.04, p =.85; CFI = 1.00, TLI = 1.09, RMSEA (90% CI) =.00 (.00–.04), AIC = 44.04; ▵χ2(2) =.77, p =.68—indicating that the final ED visits models were equivalent across intervention and non-intervention groups. In summary, final models did not differ between intervention and non-intervention groups, and thus treating these groups as a single sample was warranted.
Discussion
This study is the first to examine the reciprocal relationship between maternal depressive symptoms and child asthma morbidity. Previous research has investigated the relationship from only one direction Bartlett et al., 2001; Shalowitz et al., 2001; Bartlett et al., 2004; Shalowitz et al., 2006; Wolf, Miller, & Chen, 2008), prohibiting evaluation of the reciprocal relationship. Understanding the directionality of the relationship between maternal depressive symptoms and child asthma morbidity is critical to identify patients who may be at risk for increased asthma morbidity or mothers who may need additional support to manage their child's asthma due to their depressive symptoms. In this study, maternal depressive symptoms prospectively predicted child asthma symptoms above and beyond the stability of these constructs over time among high-risk inner-city African American children. In contrast, maternal depressive symptoms did not prospectively predict child asthma ED visits beyond the stability of these constructs. We failed to find a prospective association between maternal depressive symptoms and child asthma ED visits, perhaps because we recruited participants during a period of high asthma morbidity (i.e. soon after an ED visit). Other studies that recruited participants from the community rather than the ED have found mixed results between maternal depressive symptoms and asthma ED visits, with some studies finding a prospective association (Bartlett et al., 2004; Minkovitz et al., 2005; Logan, Riley, & Barker, 2008), while others did not (Bender & Zhang, 2008).
Contrary to our hypothesis, neither child asthma symptoms nor ED visits predicted maternal depressive symptoms. Again, because of our recruitment approach, it is unclear if the reciprocal relationship between asthma symptoms and maternal depressive symptoms differs among children with stable asthma. Interestingly, our results were not moderated by the provision of an asthma self-management intervention, suggesting that the relationship between maternal depression and child asthma symptoms did not change by the receipt of an intervention.
These findings indicate that among this sample of children recruited after seeking care for asthma in an ED, maternal depressive symptoms are more likely to influence a child's asthma symptoms than the child's asthma is to influence the caregiver's mental health over time. One possible explanation for this finding is that depressed mothers may have more difficulty managing their children's asthma appropriately. Daily asthma management requires caregivers to recognize and appropriately treat the symptoms of an asthma attack and to ensure that their child adheres to the prescribed medication regimen, attends follow-up clinic visits, and avoid asthma triggers. Indeed, depressive symptoms have been associated with lower rates of adherence to asthma medications (Smith et al., 2006; Bender & Zhang, 2008).
Alternatively, as predicted by the depression–distortion hypothesis (De Los Reyes A. & Kazdin, 2005), our findings may indicate that mothers with depressive symptoms have heightened sensitivity to negative events and therefore inaccurate recall. A recent study indicated that increased symptoms reporting was linked to negative affect but not related to medication adherence, suggesting that the subjective report of asthma symptoms may be influenced by the emotional state of the respondent (Bender & Zhang, 2008). Support for the depression–distortion hypothesis is mixed, with some studies finding that depressed mothers provide distorted reports of subjective events, such as child psychiatric symptoms (Hood, 2009) but accurate reports of objective events, such as healthcare utilization (D'Souza-Vazirani et al., 2005). Further studies are needed to clarify the type of events that are prone to depression distortion.
Despite the limitation of parental report of asthma morbidity, there is growing evidence that treating maternal depression may not only benefit the mother's psychological well-being, but may also indirectly improve child health outcomes. Beyond the health benefit to the child, it may be economically advantageous to treat maternal depression. Using Medicaid claims, Perry (2008) found that 6 months following the initiation of maternal depression treatment, there was a net average reduction in asthma spending of $798 per child.
Limitations
Limitations of our study include the reliance on a self-report by the mother of both her own depressive symptoms and the child's asthma symptoms and ED visits. Future studies would be strengthened by including alternate informant reports of symptom control and objective measures, such as archival medical record data for healthcare utilization and asthma control data. Additionally, this study only used two time points. This relationship should be examined at multiple time points to better understand the potentially cyclical and dynamic relationship between maternal depression and asthma outcomes. This would also aid in addressing the seasonal nature of asthma, which could have an impact on morbidity measure, and which were not accounted for in our analyses. We had a restricted range of asthma morbidity in our sample and therefore the results may not generalize to children with stable asthma. The 11-item version of the CES-D does not have an established cutpoint for clinically significant depressive symptoms; therefore we cannot comment on the prevalence of depression in our sample. Finally, we included only urban African American children in our sample so the results may not generalize to other ethnic groups or children living in suburban or rural areas. However, our sample of predominantly low-income minority children recruited from the ED represents a high-risk group that is often targeted for specialized intervention to reduce known health disparities.
Clinical Implications
Previous research has shown that providing case management, education, and self-management training to parents improves their children's asthma morbidity (Evans, III, et al., 1999). What is unknown is whether children of depressed mothers benefit equally from asthma management interventions. Although emerging evidence suggests that treating maternal depression is associated with improved pediatric asthma outcomes (Perry, 2008), the mechanism of this association needs further investigation.
Healthcare teams have long been encouraged to integrate mental health treatment for families into their care of children with chronic illnesses (Zimmer & Minkovitz, 2003). However, a recent study found that only 57% of pediatricians felt responsible for diagnosing maternal depression and only 45% reported that they felt confident in their ability to diagnose it (Olson et al., 2002). At minimum, these results argue for the need to focus on family-based intervention to address maternal depressive symptoms as a barrier for optimal pediatric asthma management. This is particularly important for inner-city mothers, who often lack their own source of regular primary care and the pediatrician is often the mother's most frequent contact with the healthcare system (Pascoe & Stolfi, 2004). Pediatric psychologists are uniquely positioned to raise the healthcare teams’ awareness of the impact of maternal depression on child health outcomes, provide training in assessing maternal psychological well-being, and assist their physician colleagues in developing a cost-effective strategy for identifying maternal depression during clinic visits and establishing links to appropriate referral sources.
Future Directions
In light of these results and previous research linking maternal depressive symptoms, asthma morbidity, and medication non-adherence, research is needed to assess the value and cost-effectiveness of incorporating pediatrician assessment of maternal depressive symptoms and provision of adequate treatment referrals into standard pediatric primary care. Clinical trials are needed to assess the added value of integrating maternal depression assessments and intervention into more traditional asthma self-management and education interventions to improve child asthma outcomes. This may not only improve the mother's well-being, but may also decrease the child's asthma morbidity.
Funding
National Heart Lung Blood Institute (HL063333 to C.S.R.).
Conflict of interest: None declared.
References
- Adams SK, Murdock KK, McQuaid EL. Complementary and alternative medication (CAM) use and asthma outcomes in children: an urban perspective. Journal of Asthma. 2007;44:775–782. doi: 10.1080/02770900701645835. [DOI] [PubMed] [Google Scholar]
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- Akinbami L. The state of childhood asthma, United States, 1980–2005. Advance Data. 2006;381:1–24. [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123:S131–S145. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. Amos 6.0 user's guide. Chicago, IL: SPSS, Inc; 2005. [Google Scholar]
- Bartlett SJ, Kolodner K, Butz AM, Eggleston P, Malveaux FJ, Rand CS. Maternal depressive symptoms and emergency department use among inner-city children with asthma. Archives of Pediatirc and Adolescent Medicine. 2001;155:347–353. doi: 10.1001/archpedi.155.3.347. [DOI] [PubMed] [Google Scholar]
- Bartlett SJ, Krishnan JA, Riekert KA, Butz AM, Malveaux FJ, Rand CS. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113:229–237. doi: 10.1542/peds.113.2.229. [DOI] [PubMed] [Google Scholar]
- Bender B, Zhang L. Negative affect, medication adherence, and asthma control in children. Journal of Allergy and Clinical Immunology. 2008;122:490–495. doi: 10.1016/j.jaci.2008.05.041. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bollen KA. A new incremental fit index for general structural equation models. Sociological Methods and Research. 1989;17:303–316. [Google Scholar]
- Brown ES, Gan V, Jeffress J, Mullen-Gingrich K, Khan DA, Wood BL, et al. Psychiatric symptomatology and disorders in caregivers of children with asthma. Pediatrics. 2006;118:e1715–e1720. doi: 10.1542/peds.2006-1119. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods and Research. 1992;21:230–258. [Google Scholar]
- D'Souza-Vazirani D, Minkovitz CS, Strobino DM. Validity of maternal report of acute health care use for children younger than 3 years. Archives of Pediatirc and Adolescent Medicine. 2005;159:167–172. doi: 10.1001/archpedi.159.2.167. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Eggleston PA. Environmental causes of asthma in inner city children. The National Cooperative Inner City Asthma Study. Clinical Reveiws in Allergy and Immunology. 2000;18:311–324. doi: 10.1385/CRIAI:18:3:311. [DOI] [PubMed] [Google Scholar]
- Evans R, III, Gergen PJ, Mitchell H, Kattan M, Kercsmar C, Crain E, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. Journal of Pediatrics. 1999;135:332–338. doi: 10.1016/s0022-3476(99)70130-7. [DOI] [PubMed] [Google Scholar]
- Hood KK. The influence of caregiver depressive symptoms on proxy report of youth depressive symptoms: a test of the depression-distortion hypothesis in pediatric type 1 diabetes. Journal of Pediatric Psychology. 2009;34:294–303. doi: 10.1093/jpepsy/jsn090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Archives of Internal Medicine. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Kaugars AS, Klinnert MD, Bender BG. Family influences on pediatric asthma. Journal of Pediatric Psychology. 2004;29:475–491. doi: 10.1093/jpepsy/jsh051. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd. New York: The Guilford Press; 2005. [Google Scholar]
- Koinis-Mitchell D, McQuaid EL, Friedman D, Colon A, Soto J, Rivera DV, et al. Latino caregivers' beliefs about asthma: causes, symptoms, and practices. Journal of Asthma. 2008;45:205–210. doi: 10.1080/02770900801890422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koinis-Mitchell D, McQuaid EL, Seifer R, Kopel SJ, Esteban C, Canino G, et al. Multiple urban and asthma-related risks and their association with asthma morbidity in children. Journal of Pediatric Psychology. 2007;32:582–595. doi: 10.1093/jpepsy/jsl050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara M, Rosenbaum S, Rachelefsky G, Nicholas W, Morton SC, Emont S, et al. Improving childhood asthma outcomes in the United States: a blueprint for policy action. Pediatrics. 2002;109:919–930. doi: 10.1542/peds.109.5.919. [DOI] [PubMed] [Google Scholar]
- Logan JE, Riley AW, Barker LE. Parental mental and pain-related health and pediatric ambulatory care sensitive emergency department visits and hospitalizations. Health Services Research. 2008;43:656–674. doi: 10.1111/j.1475-6773.2007.00790.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkovitz CS, Strobino D, Scharfstein D, Hou W, Miller T, Mistry KB, et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115:306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- National Heart, L. a. B. I. and National Asthma Educationand Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. US Department of Health and Human Services, National Institutes of Health. [Electronic version]; 2007. [Google Scholar]
- Olson AL, Kemper KJ, Kelleher KJ, Hammond CS, Zuckerman BS, Dietrich AJ. Primary care pediatricians' roles and perceived responsibilities in the identification and management of maternal depression. Pediatrics. 2002;110:1169–1176. doi: 10.1542/peds.110.6.1169. [DOI] [PubMed] [Google Scholar]
- Otsuki M, Eakin MN, Rand CS, Butz AM, Hsu VD, Zuckerman IH, et al. Medication adherence feedback to improve asthma outcomes among inner-city children: a randomized controlled trial. Pediatrics. in press doi: 10.1542/peds.2008-2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe JM, Stolfi A. Maternal depression and the pediatrician. Pediatrics. 2004;113:424. doi: 10.1542/peds.113.2.424. [DOI] [PubMed] [Google Scholar]
- Perry CD. Does treating maternal depression improve child health management? The case of pediatric asthma. Journal of Health Economics. 2008;27:157–173. doi: 10.1016/j.jhealeco.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. The New England Journal of Medicine. 1997;336:1356–1363. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- Shalowitz MU, Berry CA, Quinn KA, Wolf RL. The relationship of life stressors and maternal depression to pediatric asthma morbidity in a subspecialty practice. Ambulatory Pediatrics. 2001;1:185–193. doi: 10.1367/1539-4409(2001)001<0185:trolsa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Shalowitz MU, Mijanovich T, Berry CA, Clark-Kauffman E, Quinn KA, Perez EL. Context matters: a community-based study of maternal mental health, life stressors, social support, and children's asthma. Pediatrics. 2006;117:e940–e948. doi: 10.1542/peds.2005-2446. [DOI] [PubMed] [Google Scholar]
- Siefert K, Finlayson TL, Williams DR, Delva J, Ismail AI. Modifiable risk and protective factors for depressive symptoms in low-income African American mothers. American Journal of Orthopsychiatry. 2007;77:113–123. doi: 10.1037/0002-9432.77.1.113. [DOI] [PubMed] [Google Scholar]
- Smith A, Krishnan JA, Bilderback A, Riekert KA, Rand CS, Bartlett SJ. Depressive symptoms and adherence to asthma therapy after hospital discharge. Chest. 2006;130:1034–1038. doi: 10.1378/chest.130.4.1034. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. The reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Turyk ME, Hernandez E, Wright RJ, Freels S, Slezak J, Contraras A, et al. Stressful life events and asthma in adolescents. Pediatric Allergy and Immunology. 2008;19:255–263. doi: 10.1111/j.1399-3038.2007.00603.x. [DOI] [PubMed] [Google Scholar]
- U.S.Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: A report of the Surgeon General. Atlanta, GA: U.S Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [Google Scholar]
- Wade S, Weil C, Holden G, Mitchell H, Evans R, III, Kruszon-Moran D, et al. Psychosocial characteristics of inner-city children with asthma: a description of the NCICAS psychosocial protocol. National Cooperative Inner-City Asthma Study. Pediatric Pulmonology. 1997;24:263–276. doi: 10.1002/(sici)1099-0496(199710)24:4<263::aid-ppul5>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Weil CM, Wade SL, Bauman LJ, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104:1274–1280. doi: 10.1542/peds.104.6.1274. [DOI] [PubMed] [Google Scholar]
- Wolf JM, Miller GE, Chen E. Parent psychological states predict changes in inflammatory markers in children with asthma and healthy children. Brain, Behavior, and Immunity. 2008;22:433–441. doi: 10.1016/j.bbi.2007.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the Inner-City Asthma Study. American Journal of Public Health. 2004;94:625–632. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmer KP, Minkovitz CS. Maternal depression: an old problem that merits increased recognition by child healthcare practitioners. Current Opinion in Pediatrics. 2003;15:636–640. doi: 10.1097/00008480-200312000-00016. [DOI] [PubMed] [Google Scholar]