Abstract
We here in report a case of bilateral endogenous endophthalmitis caused by Pantoea agglomerans (P. agglomerans) in a patient who had interstitial lung disease and was treated with oral corticosteroids. A 72-year-old man presented with decreased visual acuity in both eyes nine days after he received oral corticosteroids. He had marked uveitis, cataracts, and vitreous opacities. Cultures were taken of blood, aqueous humor, and vitreous. We initially suspected a fungal etiology and treated him with antifungal drugs; however, the intraocular disease progressed without improvement. Vitreous culture was positive for P. agglomerans. The patient underwent pars plana vitrectomy with cataract surgery bilaterally, followed by a 2-week course of antibiotics. The final visual acuity was 20/25 in the right eye and 20/200 in the left eye. This is the first report of bilateral endogenous endophthalmitis caused by P. agglomerans in Korea; it is also the first case reported outside of the United States.
Keywords: Endophthalmitis, Pantoea
Bilateral endogenous endophthalmitis is a rare but devastating disease. It results from hematogenous spread from a septic focus distant to the eye. Immunocompromised states such as diabetes mellitus, malignancy, and chemotherapy are associated with reduced host defense and are risk factors for developing endogenous endophthalmitis.
Pantoea agglomerans (P. agglomerans) belongs to the species Enterobacteriaceae, which are gram-negative facultative anaerobes. It is commonly found in plants, soil, water, and foods. It can cause epidemics among hospitalized patients when associated with the use of contaminated intravenous products due to its ability to grow in commercial infusion fluids [1,2] and is rarely recognized as an agent of endogenous nosocomial infections [3-5]. We report the first case of bilateral endogenous endophthalmitis caused by P. agglomerans in a patient who had interstitial lung disease and was treated with oral corticosteroids.
Case Report
A 72-year-old male patient with interstitial lung disease presented to a local clinic because of difficulty breathing and a subjective fever. He had a fever of 39℃. The fever went down to 37℃ with the administration of antibiotics; the patient was then given oral corticosteroids (predinisolone 60 mg/day). Nine days after admission to a local clinic he developed blurred vision in both eyes; however, ophthalmic examination was not performed initially. Three days after this decrease in visual acuity he was referred to our hospital. On initial examination, bilateral visual acuity was finger counting. There was no history of ocular trauma prior to admission. Anterior segment examination revealed severe conjunctival injection, severe anterior chamber reaction without hypopyon, and mild complicated cataracts in both eyes. Fundus examination revealed a vitreal reaction and multiple whitish-yellow exudates in both eyes. A single exudate was seen in the right macula and multiple exudates were observed in the left macula (Fig. 1).
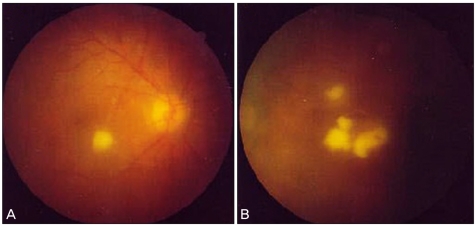
Fig. 1.
(A) Right eye. Exudate was round, whitish-yellow, and slightly elevated towards the vitreous cavity. (B) Left eye. Exudates were irregular, whitish-yellow, and slightly elevated towards the vitreous cavity.
We initially suspected a fungal infection, such as candida, given his history and fundus findings. Cytological examination and cultures of the blood, aqueous humor, and vitreous were ordered. Intravitreal vancomycin (1 mg), amikacin (200 µg), and amphotericin B (5 µg) were then injected into both eyes. Oral ketoconazole (400 mg/day) was given for the suspected ocular fungal infection. Despite this treatment, the anterior chamber reaction and fundus findings deteriorated. Five days after the initial intravitreal injection, visual acuity of the right eye had decreased to hand motion. A hypopyon had also developed in the right eye (Fig. 2).
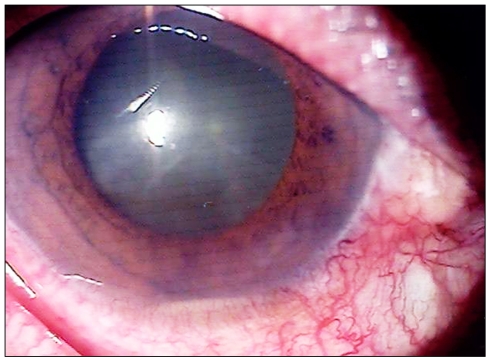
Fig. 2.
Hypopyon in the anterior chamber of the right eye.
Nine days after admission the patient underwent a pars plana vitrectomy with cataract surgery in the right eye. Intravitreal gentamicin (20 µg/mL), cefazolin (50 µg/mL), amphotericin B (1.0 µg/mL), vancomycin (1 mg), and ceftazidime (2 mg) were administered at the end of the surgery.
Five days after the initial ocular presentation, P. agglomerans was identified in the vitreous culture, but the aqueous humor and blood cultures were negative. Based on sensitivities, intravenous antibiotics (ciprofloxacin 200 mg every twelve hours and ampicillin sodium 500 mg every eight hours) were administered. The inflammation of the right eye gradually decreased in response to this therapy, but no response was observed in the left eye. On hospital day 24 the patient underwent a pars plana vitrectomy with cataract surgery in the left eye. All cultures of the vitrectomy specimens were negative. Ophthalmic findings in the left eye also improved. Six months after surgery the patient's final visual acuity improved to 25/20 in the right eye and 20/200 in the left eye. An exudative scar of the paramacular area in his left eye was noted, but his symptoms were markedly improved.
Discussion
Endogenous bacterial endophthalmitis is a rare disease that occurs when microorganisms spread to the eye from a source elsewhere in the body, usually through the bloodstream. It accounts for only 2 to 6% of all cases of endophthalmitis [6]. In this case we initially believed that the infection was fungal in origin because of the clinical features, no history of ocular trauma, the presence of interstitial lung disease with a fever, and the prior administration of immunosuppressive treatment. Early diagnosis and treatment were delayed and the inflammatory reaction worsened because this species of Enterobacteriace is refractory to antifungal agents. After aspiration of the vitreous, P. agglomerans was confirmed as the causative agent of the intraocular infection. Early detection of visual disturbances is important in patients who have received corticosteroids or immunosuppressive therapy.
P. agglomerans (formerly named Enterobacter agglomerans) is a rare cause of endogenous endophthalmitis. Zeiter et al. [7] reported the first case of endogenous P. agglomerans endophthalmitis in the United States. It is a gram-negative aerobic bacillus in the family Enterobacteriaceas. All species of the genus P. agglomerans can be isolated from feculent materials, plants, and soil; they can be either pathogens or commensals. Within the genus, P. agglomerans is the most commonly isolated species in humans, resulting in soft tissue or bone/joint infections following penetrating trauma by vegetation [8]. The organism also colonizes cotton and cotton plants and has been shown to cause a benign self-limited fever in intravenous drug abusers who filter drugs through cotton before injecting [9,10]. Tissue toxicity associated with gram-negative rods in endophthalmitis is known to generally have a poor outcome [11]. However, in our case the ocular infection subsided after vitrectomy, intravitreal injection, and tailored antibiotic treatment.
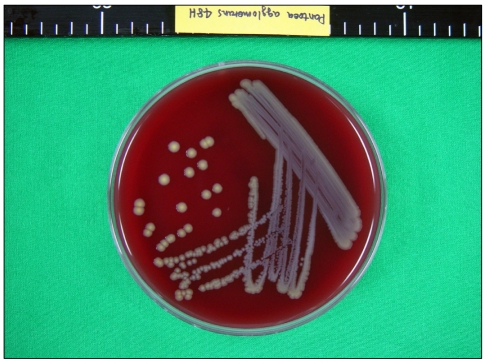
P. agglomerans produces yellow pigments that are typically only noticeable after delayed incubation at room temperature. This distinguishes it from other Enterobacter species. In our case, P. agglomerans was isolated in a vitreous culture. Yellow pigment-producing colonies that were 2 mm in size, nonhemolytic, and convex were detected on a blood agar plate (Fig. 3).
Fig. 3.
Pantoea agglomerans was isolated in the vitreous culture. Yellow pigment-producing colonies that were 2 mm in size, nonhemolytic, and convex were detected on a blood agar plate.
We believe that our case is the first report of bilateral endogenous endophthalmitis caused by P. agglomerans in Korea and the first case reported outside of the United States.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Maki DG, Martin WT. Nationwide epidemic of septicemia caused by contaminated infusion products. IV. Growth of microbial pathogens in fluids for intravenous infusions. J Infect Dis. 1975;131:267–272. doi: 10.1093/infdis/131.3.267. [DOI] [PubMed] [Google Scholar]
- 2.Maki DG, Rhame FS, Mackel DC, Bennett JV. Nationwide epidemic of septicemia caused by contaminated intravenous products. I. Epidemiologic and clinical features. Am J Med. 1976;60:471–485. doi: 10.1016/0002-9343(76)90713-0. [DOI] [PubMed] [Google Scholar]
- 3.Burchard KW, Barrall DT, Reed M, Slotman GJ. Enterobacter bacteremia in surgical patients. Surgery. 1986;100:857–862. [PubMed] [Google Scholar]
- 4.Chow JW, Fine MJ, Shlaes DM, et al. Enterobacter bacteremia: clinical features and emergence of antibiotic resistance during therapy. Ann Intern Med. 1991;115:585–590. doi: 10.7326/0003-4819-115-8-585. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher PG. Enterobacter bacteremia in pediatric patients. Rev Infect Dis. 1990;12:808–812. doi: 10.1093/clinids/12.5.808. [DOI] [PubMed] [Google Scholar]
- 6.Jackson TL, Eykyn SJ, Graham EM, Stanford MR. Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Surv Ophthalmol. 2003;48:403–423. doi: 10.1016/s0039-6257(03)00054-7. [DOI] [PubMed] [Google Scholar]
- 7.Zeiter JH, Koch DD, Park ED, 2nd, Font RL. Endogenous endophthalmitis with lenticular abscess caused by Enterobacter agglomerans (Erwinia species) Ophthalmic Surg. 1989;20:9–12. [PubMed] [Google Scholar]
- 8.Cruz AT, Cazacu AC, Allen CH. Pantoea agglomerans, a plant pathogen causing human disease. J Clin Microbiol. 2007;45:1989–1992. doi: 10.1128/JCM.00632-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferguson R, Feeney C, Chirurgi VA. Enterobacter agglomerans: associated cotton fever. Arch Intern Med. 1993;153:2381–2382. [PubMed] [Google Scholar]
- 10.Harrison DW, Walls RM. "Cotton fever": a benign febrile syndrome in intravenous drug abusers. J Emerg Med. 1990;8:135–139. doi: 10.1016/0736-4679(90)90222-h. [DOI] [PubMed] [Google Scholar]
- 11.Rowsey JJ, Newsom DL, Sexton DJ, Harms WK. Endophthalmitis: current approaches. Ophthalmology. 1982;89:1055–1066. doi: 10.1016/s0161-6420(82)34691-6. [DOI] [PubMed] [Google Scholar]