Abstract
Objective
In cervico-thoracic junction (CTJ), the use of strong fixation device such as pedicle screw-rod system is often required. Purpose of this study is to analyze the anatomical features of C7 and T1 pedicles related to screw insertion and to evaluate the safety of pedicle screw insertion at these levels.
Methods
Nineteen patients underwent posterior CTJ fixation with C7 and/or T1 included in fixation levels. Seventeen patients had tumorous conditions and two with post-laminectomy kyphosis. The anatomical features were analyzed for C7 and T1 pedicles in 19 patients using computerized tomography (CT). Pedicle screw and rod fixation system was used in 16 patients. Pedicle violation by screws was evaluated with postoperative CT scan.
Results
The mean values of the width, height, stable depth, safety angle, transverse angle, and sagittal angle of C7 pedicles were 6.9 ± 1.34 mm, 8.23 ± 1.18 mm, 30.93 ± 4.65 mm, 26.42 ± 7.91 degrees, 25.9 ± 4.83 degrees, and 10.6 ± 3.39 degrees. At T1 pedicles, anatomic parameters were similar to those of C7. The pedicle violation revealed that 64.1% showed grade I violation and 35.9% showed grade II violation, overall. As for C7 pedicle screw insertion, grade I was 61.5% and grade II 38.5%. At T1 level, grade I was 65.0% and grade II 35.0%. There was no significant difference in violation rate between the whole group, C7, and T1 group.
Conclusion
C7 pedicles can withstand pedicle screw insertion. C7 pedicle and T1 pedicle are anatomically very similar. With the use of adequate fluoroscopic oblique view, pedicle screw can be safely inserted at C7 and T1 levels.
Keywords: Pedicle screw, Cervico-thoracic junction, Posterior fixation
INTRODUCTION
Pathologic processes in cervico-thoracic junction (CTJ) are relatively uncommon but can include trauma, degenerative disease, infection and tumor involvement. It is known that 15% of total spinal tumor is involved in the upper thoracic spine and 10% of spine metastases occur across T1 and T4 region2). The incidence of traumatic injuries at CTJ has been reported as 9% of all cervical injuries18). Neurologic involvement is commonly complicated in CTJ lesions, which can be as high as 80%26). The CTJ, as a unique area, is the crossing transitional area of lordotic cervical spine and kyphotic thoracic spine3). Because laminectomy for neural decompression in CTJ usually aggravates spinal instability, stabilization process should be accompanied2,7,13,23).
Various internal fixation techniques have been used for the stabilization of CTJ. Anterior fixation is mostly used for anterior column injuries or as an adjunct to posterior fixation for three-column injuries. However, there have been serious complications related to visceral and vascular injury during anterior approach. Posterior stabilization is generally preferred for posterior and three column injuries because anterior plating is estimated to be biomechanically the least rigid construct in all tests and significantly less stiff than any type of posterior stabilization5). Several kinds of posterior fixation have been suggested, for example, sublaminar wiring with rod/plate fixation, laminar hook with rod fixation, and pedicle screw with rod fixation system8,12,14,30). However, sublaminar wiring system has a restriction because the lower cervical laminae are smaller and weaker than upper thoracic vertebrae. And, laminar hook also has a limit due to the narrow spinal canal19). Lateral mass screw cannot provide strong fixation at C6, 7 levels of which lateral mass is smaller than other cervical levels15). Biomechanically, the transpedicular screw fixation system has the highest stability and is frequently considered, but it has a demerit of high possibility of pedicle violation4,5,28).
CTJ is a surgically challenging area because vertebral artery, small spinal canal, and tenuous blood supply to spinal cord may cause frequent neurovascular complications. Therefore, the understanding of the anatomical structure in CTJ is the most important factor in stabilization3,9). The purpose of this study is to analyze the anatomical features of C7 and T1 pedicles related to screw insertion and to evaluate the safety of pedicle screw insertion at these levels.
MATERIALS AND METHODS
Our study population consisted of 19 patients who had posterior fusion operation on CTJ from 2002 to 2009. Their C7 and/or T1 pedicles were included in fixation levels. Ten of them were males, nine were females and their average age was 55.5 years (range, 17-74 years). The operative diagnoses were tumorous condition in 17 [metastasis of lung cancer, colon cancer, mass of unknown origin (MUO) etc.] and post-laminectomy kyphosis in two patients. The anatomical features were analyzed in C7, T1 for these 19 patients. Pedicle screw system was used in 16 patients. Computerized tomography (CT) was used for morphological analysis of C7 and T1 pedicles regarding their linear and angular dimensions, as well as for pedicle violation detection following screw insertion.
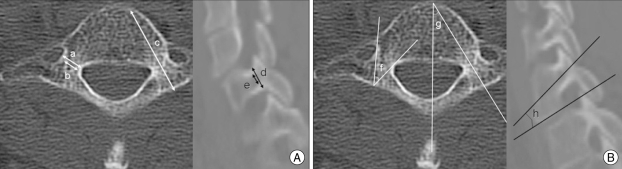
Twenty-nine pedicles of C7 and 27 pedicles of T1 were available for the morphological study. For each spine CT scan was performed with 1-2 mm slice thickness. Then measurement was taken on sagittal and coronal reconstructions of 1 mm thickness. Linear and angular dimensions of the pedicles were calculated in two planes, sagittal and transverse planes, with each crossing the central part of the pedicle and the entry point of transpedicular screw insertion. The width and height in pedicle isthmus of C7 and T1 were checked in division of outer and inner in linear dimension. Stable depth which is the distance from the lateral mass to the anterior inner cortex of vertebral body was also measured (Fig. 1A). Safety angle, a range of angle which does not make neurovascular injury during screw insertion in angular dimension, transverse angle, between the medial sagittal plane and longitudinal pedicle axis, and the sagittal angle, the angle between inferior end plate and pedicle, were measured (Fig. 1B).
Fig. 1.
A : Measurement of linear dimensions in C7 and T1 pedicle is done on CT images crossing through the central part of the pedicles. a : outer pedicle width, distance between medial and lateral outer cortex of pedicle, b : inner pedicle width, distance between medial and lateral inner cortex of pedicle, c : stable depth, distance from lateral mass to the anterior inner cortex, d : outer pedicle height, distance between superior and inferior outer cortex of pedicle, e : inner pedicle height, distance between superior and inferior inner cortex of pedicle. B : Measurement of angular dimensions in C7 and T1 pedicle is done on CT images crossing through the central part of the pedicles. f : safety angle, range of angle which does not make neurovascular injury, g : transverse angle, angle between medial sagittal plane and longitudinal pedicle axis, h : sagittal angle, angle between inferior end plate and pedicle.
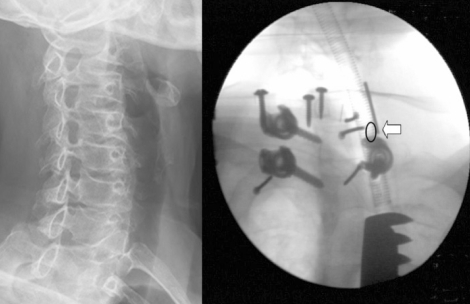
C7 pedicle screw insertion was done as follows; the entry point was selected on the spot of crossing point of 1 mm below the midline of transverse process and midline of C6/7 facet line. Then decortication of the lateral mass was done with a high-speed burr until the pedicle entry point could be identified confidently. The entry hole was created using an awl. The guide pins were inserted into the pedicle holes, and the accuracy of the created trajectory was confirmed on C-arm oblique view (Fig. 2). If a guide pin was located outside a pedicle, the probe was reinserted into the pedicle to create a correct pathway. Blunt tipped fine pedicle probe was inserted into the pedicle cavity with the inclination at 5 degrees down-wards pointing to the C7 end plate from the medial in 30 to 35 degrees from the sagittal plane4). Tapping was performed. After fluoroscopic confirmation was done again, final insertion of screws was performed.
Fig. 2.
C7 screw insertion with C-arm oblique view. The insertion point is selected for the guide pin (arrow) to be positioned at the lateral margin of pedicle (circle).
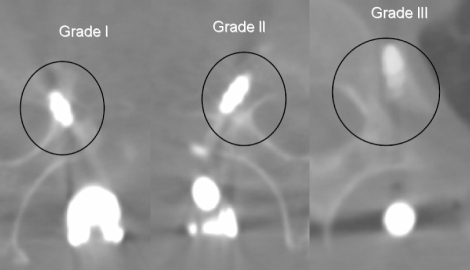
Pedicle violation by screws was graded from I to III according to the position of the inserted screws (Fig. 3). The occurrence of neurovascualr complication was not considered. Grade I violation was decided when screw centered in the pedicle caused only minor plastic deformation of the pedicle cortex at most. Grade II violation was judged when a half or less than half of the screw width penetrated the cortex without injuring the spinal cord, nerve roots, or vertebral artery. Finally, grade III violation was noted when more than half of the screw width penetrated the cortex.
Fig. 3.
Screw violation grading system depending on screw position. Grade I : screw centered in the pedicle caused only minor plastic deformation of the pedicle cortex at most. Grade II : a half or less than half of the screw width penetrated the cortex without injuring neurovascular structures. Grade III : more than half of the screw width penetrated the cortex.
RESULTS
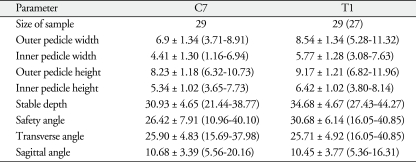
Morphological evaluation for C7 and T1 pedicles was done with preoperative CT images. Anatomical analysis for C7 pedicle was possible in 29 (Table 1). Pedicle width showed 6.9 ± 1.34 mm (outer) and 4.41 ± 1.30 mm (inner), pedicle height was 8.23 ± 1.18 mm (outer) and 5.34 ± 1.02 mm (inner), and stable depth was 30.93 ± 4.65 mm. In angular dimension, safety angle, transverse angle, and sagittal angle were 26.42 ± 7.91 degrees, 25.9 ± 4.83 degrees, and 10.6 ± 3.39 degrees, respectively. Similar measurements for T1 pedicle were done in 27 (Table 1). Pedicle width was 8.5 ± 1.34 mm (outer) and 5.77 ± 1.28 mm (inner), pedicle height was 9.17 ± 1.21 mm (outer) and 6.41 ± 1.02 mm (inner), and stable depth was 34.68 ± 4.67 mm. Safety angle, transverse angle, and sagittal angle were 30.68 ± 6.14 degree, 25.71 ± 4.92 degrees, and 10.45 ± 3.77 degrees respectively.
Table 1.
Anatomical features of C7 and T1
Each parameter was given as the mean ± standard deviation (range)
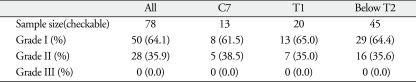
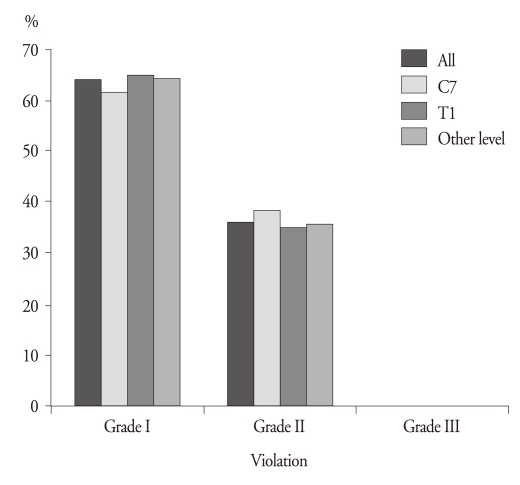
For a total of 16 operations, 94 pedicle screws were inserted; C7 instrumentation was performed in 14 pedicles of 8 patients and T1 instrumentation in 23 pedicles of 12 patients. Corpectomy was done in 13 patients and anterior plating was performed in 3 patients (Table 2). Pedicle violation by screws could be checked in 78 pedicles; C7 pedicle screw in 13 and T1 pedicle screw in 20. Overall review in 78 screws revealed that 64.1% (50 screws) showed grade I violation and 35.9% (28 screws) showed grade II violation but there was no case of grade III violation. As for C7 pedicle screw insertion, grade I violation was 61.5% (8 of 13 pedicle screw) and grade II violation 38.5% (5 of 13 pedicle screw). At T1 level, grade I violation was 65.0% (13 of 20 pedicle screw) and grade II violation 35.0% (7 of 20 pedicle screw). Grade III violation was not detected (Table 2). In cases with pedicle violation, there was no case of medial cortex violation while all of them penetrated the pedicle lateral cortex. When comparing these values with screws inserted at other levels, the violation rate of C7 and T1 was not higher than those of other levels (Table 3). Furthermore, there was no significant difference in violation rate between the whole group of 78 pedicles, C7, and T1 group (Fig. 4).
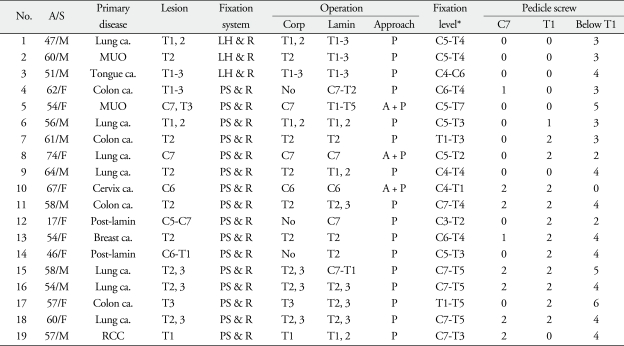
Table 2.
Patients' information
*Lateral mass screws were used for above C7 level fixation. M : males, F : females, Post-lamin : post-laminectomy kyphosis, LH & R : laminar hook and rod fixation, PS & R : pedicle screw and rod fixation, Corp : corpectomy level, Lamin : laminectomy level, P : posterior approach only, A+P : anteriorr with posterior approach, MUO : mass of unknown origin
Table 3.
Results of pedicle screw violation rate (%)
Grade I : screw centered in the pedicle caused only minor plastic deformation of the pedicle cortex at most. Grade II : a half or less than half of the screw width penetrated the cortex without injuring the neurovascular structures. Grade III : more than half of the screw width penetrated the cortex
Fig. 4.
Comparison of screw violation rate (%). There is no significant difference in violation rate between C7 pedicle, T1 pedicle, and whole group.
With regards to early complications after surgery, two cases of paraplegia developed due to acute hematoma collection and one wound infection was found, but they recovered soon. There was no neurovascular injury related to instrumentation. A case of anterior slippage of mesh cage on X-ray was observed at five months after surgery. This patient was operated with laminar hook and rod fixation system. No significant symptoms or signs were associated with slippage. With pedicle screw and rod fixation system, no instrument-related complication was detected. It was not possible to draw a conclusion whether which fixation system was more reliable, owing to the fact that most cases were fixed using pedicle screw-rod system with only three cases fixed using other system.
DISCUSSION
Bony destruction due to neoplasm is often accompanied by spinal instability. In addition, surgical intervention, such as corpectomy or laminectomy, can result in additional spinal instability. Especially in junctional region, e.g., cervicothoracic or thoracolumbar area, instability is a major concern in surgical treatment when destructive lesions develop. In CTJ, the change from cervical lordosis to thoracic kyphosis at C7 results in transfer of weight from the posterior aspect to the anterior aspect of the spinal column10). This transfer results in increased stress at this level, rendering instrumentation at CTJ a challenging procedure11). Because CTJ represents a transition zone, significant anatomical variations are common. Vertebral alignment represents a change from a mobile, cervical lordosis to a rigid, thoracic kyphosis. The lower cervical laminae are thinner and weaker compared with upper thoracic vertebrae. Together with a narrow spinal canal, this finding often limits the use of the hook/rod system for stabilization at CTJ19).
Three-column fixation offers a significant biomechanical advantage23). However, when choosing anterior versus posterior, posterior constructs prove superior to anterior plates for managing instabilities between C7 and T1. Bueff et al.5) compared three different fixation devices at the CTJ-an anterior plate, a posterior plate, and a posterior hook rod sytems. Anterior plates provided the least rigid construct in all tests and were significantly less stiff than posterior plates. Among several kinds of fixation device, transpedicular screw fixation has provided the highest stability in unstable lower cervical spine17). In our institution, sub-laminar wiring system was used before 2000, laminar hook system was applied on the patients from 2001 to 2003 and the pedicle screw system was adopted since 2004 (Fig. 5).
Fig. 5.
Various posterior fixation systems for cervico-thoracic junction. A : Sub-laminar wiring and rod fixation system. B : Laminar hook and rod fixation system.
From a morphological point of view, seventh cervical vertebra (C7) is a transitional vertebra, with characteristics of both cervical and thoracic vertebrae; this was the reason why Albrecht named C7 the "pseudo-cervical vertebra"4). Its particular morphology, especially its pedicle dimensions and lateral mass thickness, generate some specific findings when posterior fixation of C7 is required31). The vertebral artery usually penetrates the transverse canal at C6 level and it is not present within the C7 transverse foramen in 95% of cases4). This is a very important anatomical point when considering transpedicular screwing of C724). Thus, the risk of vascular injury in cases of pedicle violation is not so high at C7 as at other vertebral levels. It needs to be known that the presence of a C7 transverse foramen does not necessarily signify that there is the vertebral artery inside. The C7 foramen transverse may be small but it is seldom absent. It usually contains vascular and sympathetic nerve branches, fibrous and adipose tissues. It would be useful to carry out an injected CT scan preoperatively to verify the presence or absence of the vertebral artery inside C7 transverse foramen4,6,9,10).
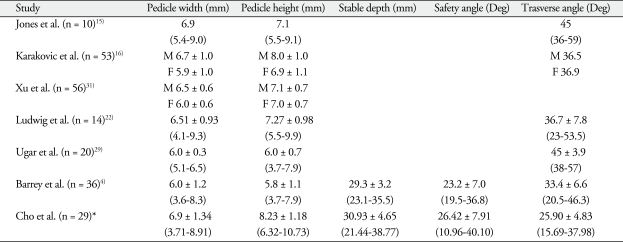
The previous investigations for C7 anatomical features revealed that pedicle width ranges from 6.0 mm to 7.0 mm, which is consistent with our data, however, the value of pedicle height showed wide variation from 5.8 to 8.23 mm15,16,22,29) (Table 4). These findings were due to the different measurement methods. In some studies, pedicle was checked in width and height with direct measurement in object of cadaver, however, in others, it was done using reconstructed CT images. In spite of the measurement errors, we can see that C7 pedicle is oval in shape with height exceeding width in the coronal view and the size of pedicle is not as small as it is thought of. In our study, C7 pedicle was a little smaller in size compared to T1 pedicle and no great differences were seen when the anatomical feature of C7 and T1 were compared (Table 1).
Table 4.
Review of the literatures and comparison of C7 anatomy
For each parameter the mean ± standard deviation (range) are given. *Our study. M : males, F : females, Deg : degrees
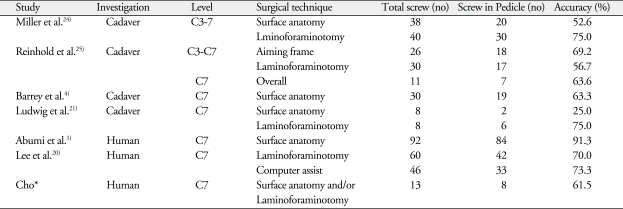
Although pedicle screw system is the strongest fixation system, it has a risk of pedicle violation1,4,16,22,24,25,27). So far several researches for pedicle violation when inserting screws have been done with object of cadaver or clinical human (Table 5). Miller et al.24) classified cadavers into two groups and checked the pedicle violation with two surgical techniques depending on the screw position after cervical spine pedicle screw insertion on C3-C7 level. It was performed along the surface landmark in one group and with window opening of laminoforaminotomy in the other group, which result showed 52.6% and 75% of accuracy respectively. Reinhold et al.25) compared two methods of cervical pedicle screw insertion, which were with laminoforaminotomy and aiming frame in cadavers, the accuracy was similar. On C7 pedicle level, Barrey et al.4) reported 63.3% of accuracy in 30 C7 pedicle screws in cadavers which was checked on postoperative CT scan. In clinical studies, Abumi et al.1) has reported the most extensive experience with transpedicular fixation of the cervical spine. They used surface landmarks and intraoperative fluoroscopy, and the remarkable accuracy of 91.3% was noted on postoperative CT images. Lee et al.20) reported C7 pedicle screw insertion along with anatomical reference using laminoforaminotomy, their accuracy was 70%.
Table 5.
Accuracy of pedicle screw placement of cervical spine
No : number, % : percentage. *Our study
Definitive conclusion regarding accuracy and safety of pedicle screw insertion using different surgical techniques cannot be drawn when comparing the pedicle violation rate among different studies. It is due to variations in standards of violation grading and the methods of checking the violation. Some studies considered minor cortical penetration as grade I violation, others linked violation to approaching neurovascular structures. Moreover, Miller et al.24) directly checked the position of screw in pedicles of cadavers, others checked the screw positions on CT scan1,4,20,21,25).
CONCLUSION
For posterior fixation at CTJ, C7 pedicle screw insertion is often required. Our data show that C7 pedicle is not small for screw insertion and C7 pedicle and T1 pedicle are anatomically very similar. When C7 pedicle screw insertion is tried, insertion angle can be referenced to T1 level. With the use of fluoroscopic oblique view, pedicle screw can be safely inserted at C7 and T1 levels.
References
- 1.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976) 2000;25:962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 2.An HS, Vaccaro A, Cotler JM, Lin S. Spinal disorders at the cervicothoracic junction. Spine (Phila Pa 1976) 1994;19:2557–2564. doi: 10.1097/00007632-199411001-00011. [DOI] [PubMed] [Google Scholar]
- 3.An HS, Wise JJ, Xu R. Anatomy of the cervicothoracic junction : a study of cadaveric dissection, cryomicrotomy, and magnetic resonance imaging. J Spinal Disord. 1999;12:519–525. [PubMed] [Google Scholar]
- 4.Barrey C, Cotton F, Jund J, Mertens P, Perrin G. Transpedicular screwing of the seventh cervical vertebra : anatomical considerations and surgical technique. Surg Radiol Anat. 2003;25:354–360. doi: 10.1007/s00276-003-0163-5. [DOI] [PubMed] [Google Scholar]
- 5.Bueff HU, Lotz JC, Colliou OK, Khapchik V, Ashford F, Hu SS, et al. Instrumentation of the cervicothoracic junction after destabilization. Spine (Phila Pa 1976) 1995;20:1789–1792. doi: 10.1097/00007632-199508150-00007. [DOI] [PubMed] [Google Scholar]
- 6.Cha SH, Kim C, Choi BK, Kim HJ, Baek SY. C-arm assessment of cervical pedicle screw : screw coaxial fluoroscopy and oblique view. Spine (Phila Pa 1976) 2007;32:1721–1727. doi: 10.1097/BRS.0b013e3180b9f29b. [DOI] [PubMed] [Google Scholar]
- 7.Chapman JR, Anderson PA, Pepin C, Toomey S, Newell DW, Grady MS. Posterior instrumentation of the unstable cervicothoracic spine. J Neurosurg. 1996;84:552–558. doi: 10.3171/jns.1996.84.4.0552. [DOI] [PubMed] [Google Scholar]
- 8.Choueka J, Spivak JM, Kummer FJ, Steger T. Flexion failure of posterior cervical lateral mass screws. Influence of insertion technique and position. Spine (Phila Pa 1976) 1996;21:462–468. doi: 10.1097/00007632-199602150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Ebraheim NA, Jabaly G, Xu R, Yeasting RA. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine (Phila Pa 1976) 1997;22:1553–1556. doi: 10.1097/00007632-199707150-00002. discussion 1557. [DOI] [PubMed] [Google Scholar]
- 10.Ebraheim NA, Xu R, Knight T, Yeasting RA. Morphometric evaluation of lower cervical pedicle and its projection. Spine (Phila Pa 1976) 1997;22:1–6. doi: 10.1097/00007632-199701010-00001. [DOI] [PubMed] [Google Scholar]
- 11.Graham AW, Swank ML, Kinard RE, Lowery GL, Dials BE. Posterior cervical arthrodesis and stabilization with a lateral mass plate. Clinical and computed tomographic evaluation of lateral mass screw placement and associated complications. Spine (Phila Pa 1976) 1996;21:323–328. doi: 10.1097/00007632-199602010-00014. discussion 329. [DOI] [PubMed] [Google Scholar]
- 12.Hong JT, Yi JS, Kim JT, Ji C, Ryu KS, Park CK. Clinical and radiologic outcome of laminar screw at C2 and C7 for posterior instrumentation-review of 25 cases and comparison of C2 and C7 intralaminar screw fixation. Surg Neurol. 2009 doi: 10.1016/j.surneu.2009.06.010. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Inoue A, Ikata T, Katoh S. Spinal deformity following surgery for spinal cord tumors and tumorous lesions : analysis based on an assessment of the spinal functional curve. Spinal Cord. 1996;34:536–542. doi: 10.1038/sc.1996.97. [DOI] [PubMed] [Google Scholar]
- 14.Jeanneret B, Magerl F, Ward EH, Ward JC. Posterior stabilization of the cervical spine with hook plates. Spine (Phila Pa 1976) 1991;16:S56–S63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 15.Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976) 1997;22:977–982. doi: 10.1097/00007632-199705010-00009. [DOI] [PubMed] [Google Scholar]
- 16.Karaikovic EE, Daubs MD, Madsen RW, Gaines RW., Jr Morphologic characteristics of human cervical pedicles. Spine (Phila Pa 1976) 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 17.Kotani Y, Cunningham BW, Abumi K, McAfee PC. Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine (Phila Pa 1976) 1994;19:2529–2539. doi: 10.1097/00007632-199411001-00007. [DOI] [PubMed] [Google Scholar]
- 18.Kreshak JL, Kim DH, Lindsey DP, Kam AC, Panjabi MM, Yerby SA. Posterior stabilization at the cervicothoracic junction. A biomechanical study. Spine (Phila Pa 1976) 2002;27:2763–2770. doi: 10.1097/00007632-200212150-00005. [DOI] [PubMed] [Google Scholar]
- 19.Le H, Balabhadra R, Park J, Kim D. Surgical treatment of tumors involving the cervicothoracic junction. Neurosurg Focus. 2003;15:E3. doi: 10.3171/foc.2003.15.5.3. [DOI] [PubMed] [Google Scholar]
- 20.Lee GY, Massicotte EM, Rampersaud YR. Clinical accuracy of cervicothoracic pedicle screw placement : a comparison of the "open" lamino-foraminotomy and computer-assisted techniques. J Spinal Disord Tech. 2007;20:25–32. doi: 10.1097/01.bsd.0000211239.21835.ad. [DOI] [PubMed] [Google Scholar]
- 21.Ludwig SC, Kowalski JM, Edwards CC, 2nd, Heller JG. Cervical pedicle screws : comparative accuracy of two insertion techniques. Spine (Phila Pa 1976) 2000;25:2675–2681. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 22.Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ. Placement of pedicle screws in the human cadaveric cervical spine : comparative accuracy of three techniques. Spine (Phila Pa 1976) 2000;25:1655–1667. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 23.Mazel C, Hoffmann E, Antonietti P, Grunenwald D, Henry M, Williams J. Posterior cervicothoracic instrumentation in spine tumors. Spine (Phila Pa 1976) 2004;29:1246–1253. doi: 10.1097/00007632-200406010-00015. [DOI] [PubMed] [Google Scholar]
- 24.Miller RM, Ebraheim NA, Xu R, Yeasting RA. Anatomic consideration of transpedicular screw placement in the cervical spine. An analysis of two approaches. Spine (Phila Pa 1976) 1996;21:2317–2322. doi: 10.1097/00007632-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 25.Reinhold M, Magerl F, Rieger M, Blauth M. Cervical pedicle screw placement : feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J. 2007;16:47–56. doi: 10.1007/s00586-006-0104-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sapkas G, Papadakis S, Katonis P, Roidis N, Kontakis G. Operative treatment of unstable injuries of the cervicothoracic junction. Eur Spine J. 1999;8:279–283. doi: 10.1007/s005860050174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Seo YJ, Song GS, Cho WH, Choi BK, Cha SH, Baek SY. Comparison of three different techniques in cervical transpedicular screw insertion. J Korean Neurosurg Soc. 2006;39:360–365. [Google Scholar]
- 28.Stulík J, Vyskocil T, Sebesta P, Kryl J, Pafko P. [Surgical treatment for disorders of the cervicothoracic junction region] Acta Chir Orthop Traumatol Cech. 2005;72:213–220. [PubMed] [Google Scholar]
- 29.Uğur HC, Attar A, Uz A, Tekdemir I, Egemen N, Cağlar S, et al. Surgical anatomic evaluation of the cervical pedicle and adjacent neural structures. Neurosurgery. 2000;47:1162–1168. doi: 10.1097/00006123-200011000-00029. discussion 1168-1169. [DOI] [PubMed] [Google Scholar]
- 30.Wang MY. Cervical crossing laminar screws : early clinical results and complications. Neurosurgery. 2007;61:311–315. doi: 10.1227/01.neu.0000303987.49870.7b. discussion 315-316. [DOI] [PubMed] [Google Scholar]
- 31.Xu R, Ebraheim NA, Yeasting R, Wong F, Jackson WT. Anatomy of C7 lateral mass and projection of pedicle axis on its posterior aspect. J Spinal Disord. 1995;8:116–120. [PubMed] [Google Scholar]