Abstract
We present a case of hydrocephalus as the primary manifestation of neurosarcoidosis. Sarcoidosis is a rare disease in Korea and its incidence is much lower than that of tuberculosis. Diagnosis is made by pathologic findings and by exclusion of other granulomatous disorders. Neurosarcoidosis is observed in approximately 5% of sarcoidosis. Its common manifestations are facial palsy (50% of patients with neurosarcoidosis) and optic neuritis. Hydrocephalus is a very uncommon reported finding. Although the typical presentation of sarcoidosis such as facial palsy is not a diagnostic dilemma, more atypical presentations such as hydrocephalus with altered mentality in a tuberculosis patient can lead to a misdiagnosis.
Keywords: Sarcoidosis, Neurosarcoidosis, Tuberculosis, Hydrocephalus
INTRODUCTION
Sarcoidosis is a systemic granulomatous disease that primarily affects the lung and lymphatic systems of the body. It makes epitheloid, non-necrotizing granuloma in pulmonary parenchyma. The cause of this disorder is still unknown3). Neurologic complications develop in 5% of patients with sarcoidosis2,9). An initial diagnosis of neurosarcoidosis is made in 50% of patients with neurologic deficits. Neurosarcoidosis is diagnosed on the basis of neurologic complaints from the patient and de novo findings consistent with the disease8). Seventh nerve involvement with unilateral facial palsy, which usually occurs suddenly and transiently, is the most common finding (50% of patients with neurosarcoidosis). Optic neuritis is the second most common cranial nerve neuropathy5). Palate dysfunction, hearing abnormalities, vertigo, papilledema, hypothalamic and pituitary abnormalities, chronic aseptic meningitis, mass-lesion effect, psychiatric disturbances, myopathy and seizure are other common neurologic manifestations5,6). Hydrocephalus was involved in 6% of patients with neurosarcoidosis in a prospective study1). Both obstructive and communicating hydrocephalus occur with neurosarcoidosis, and the main cause of hydrocephalus is granulomatous meningitis3,4).
In Korea, sarcoidosis is a very rare disease. The incidence is 59 cases in 1998 (0.125/100,000)4). The most common symptom was respiratory symptoms (42%) and the most frequently involved organ was the lung (87%), followed by skin (31%)4). On the other hand, tuberculosis is an endemic disease and 34,157 new cases of tuberculosis patients were noted in 2007. Acid fast stain test of sputum was positive in just 11,048 cases. In Korea, there are few sarcoidosis patients and many tuberculosis patients whose laboratory test is negative. Therefore, physicians sometimes use antituberculous medication, if tuberculosis was suggested clinically without other evidence.
CASE REPORT
A 32-year-old woman visited the emergency department due to drowsiness. She also complained of poor oral intake and strabismus. Brain computed tomography (CT) revealed radiologic findings suggestive of hydrocephalus. The magnetic resonance imaging (MRI) suggested diffuse leptomeningeal enhancement, especially in the inferior portion of the fourth ventricle (Fig. 1). The patient was already diagnosed with pulmonary tuberculosis and has taken antituberculous medication for 11 months before this presentation. An initial diagnosis of tuberculous leptomeningitis, sarcoidosis leptomeningitis or neurocysticercosis was made. We performed Mycobacterium tuberculosis polymerase chain reaction (PCR)/culture, serum angiotensin converting enzyme and enzyme linked immunosorbent assay (ELISA) for cysticercosis, all of which showed negative results. According to the past history and laboratory result, we initially diagnosed the patients as tuberculosis leptomeningitis.
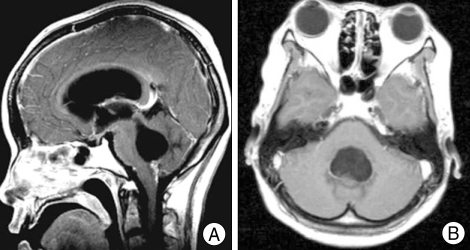
Fig. 1.
There are magnetic resonance images on admission. A : MRI image showed fourth ventricular mass and markedly dilated fourth ventricle. The mass in fourth ventricle enhanced by gadolinium. B : MRI image as axial cut at fourth ventricle showed leptomeningeal enhancement.
We obtained uncovered medical history belatedly. She had previously visited a regional hospital with a 4-year history of blurred vision. An ophthalmologist made a diagnosis of uveitis at that time. At presentation, she had a palpable neck mass and hilar lymphadenopathy. Prednisolone was administered for 11 months. Her uveitis was cured by steroid therapy. At the completion of steroid therapy, she complained of jaw pain and was diagnosed with sialadenitis. Cytological examination of the fine needle aspiration specimen showed chronic granulomatous inflammation without necrosis. She was transferred to the department of internal medicine. Although AFB staining results and Mycobacterium tuberculosis PCR results were inconsistent with tuberculosis, a pulmonologist made a diagnosis of tuberculous lymphadenitis and administered antituberculous medication.
Emergency extraventricular drainage was performed, and intravenous dexamethasone 4 mg was administered. Intravenous dexamethasone 4 mg was injected every 6 hours for 2 weeks. On follow-up MRI at 2 weeks, hydrocephalus resolved (Fig. 2). Based on the past medical history of uveitis, as well as sialadenitis, hilar lymphadenopathy, negative Mycobacterium tuberculosis PCR results and a good response to steroid therapy, she was ultimately diagnosed with sarcoidosis. We performed ventriculoperitoneal shunt operation and administered corticosteroids. The patient was discharged in a symptom-free state after treatment.
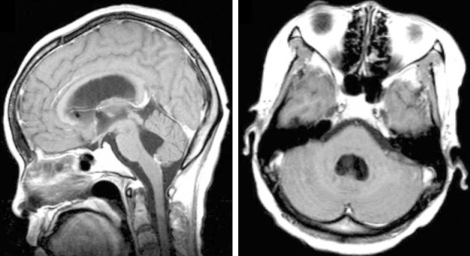
Fig. 2.
Follow-up MR images obtained 15 days after the treatment show improved venriculomegaly and regression in size of the enhanced mass.
DISCUSSION
The diagnosis of sarcoidosis requires compatible clinical features, pathologic findings and no possibility of alternative diagnosis. If the patient shows non-caseating granuloma affected organ and no alternative diagnosis is possible, the patient is diagnosed with sarcoidosis. If biopsy was impossible and laboratory tests showed compatibility with sarcoidosis, we can make a diagnosis of sarcoidosis. The diagnosis of sarcoidosis cannot be made with 100% certainty.
This case has aqueductal mass. Biopsy could not be performed because of surgical morbidity. She showed hilar adenopathy in chest roentgenogram, uveitis and granuloma in the salivary gland. The patient was given antituberculous medication for 11months. However, a new aqueductal mass occurred. It means she did not suffer from tuberculosis. We made a diagnosis of sarcoidosis caused by her clinical manifestation, biopsy and no alternative diagnosis.
In literature review, just one case of misdiagnosis of sarcoidosis in pulmonary tuberculosis was reported in 19857). In Korea, although sarcoidosis was formerly a very rare disease, its incidence has continuously been increasing4). Most granulomatous diseases in Korea have been diagnosed as tuberculosis rather than sarcoidosis. However, despite a high incidence of tuberculosis, we must consider the possibility of sarcoidosis in such cases to avoid unnecessary antituberculosis medication.
CONCLUSION
We report a case of hydrocephalus as the primary manifestation of neurosarcoidosis, which is very rare. She was misdiagnosed with tuberculosis and treated with antituberculous medication for a long period of time. We must consider the possibility of sarcoidosis before making a diagnosis of tuberculosis.
References
- 1.Allen RK, Sellars RE, Sandstrom PA. A prospective study of 32 patients with neurosarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2003;20:118–125. [PubMed] [Google Scholar]
- 2.Burns TM. Neurosarcoidosis. Arch Neurol. 2003;60:1166–1168. doi: 10.1001/archneur.60.8.1166. [DOI] [PubMed] [Google Scholar]
- 3.James DG, Neville E. Pathobiology of sarcoidosis. Pathobiol Annu. 1977;7:31–61. [PubMed] [Google Scholar]
- 4.Kim DS. Sarcoidosis in Korea : report of the Second Nationwide Survey. Sarcoidosis Vasc Diffuse Lung Dis. 2001;18:176–180. [PubMed] [Google Scholar]
- 5.Lower EE, Broderick JP, Brott TG, Baughman RP. Diagnosis and management of neurological sarcoidosis. Arch Intern Med. 1997;157:1864–1868. [PubMed] [Google Scholar]
- 6.Luke RA, Stern BJ, Krumholz A, Johns CJ. Neurosarcoidosis : the long-term clinical course. Neurology. 1987;37:461–463. doi: 10.1212/wnl.37.3.461. [DOI] [PubMed] [Google Scholar]
- 7.Rubinstein I, Baum GL, Hiss Y. [Misdiagnosis of sarcoidosis in active pulmonary tuberculosis] Harefuah. 1985;108:175–176. [PubMed] [Google Scholar]
- 8.Scott TF. Neurosarcoidosis : progress and clinical aspects. Neurology. 1993;43:8–12. doi: 10.1212/wnl.43.1_part_1.8. [DOI] [PubMed] [Google Scholar]
- 9.Stern BJ, Krumholz A, Johns C, Scott P, Nissim J. Sarcoidosis and its neurological manifestations. Arch Neurol. 1985;42:909–917. doi: 10.1001/archneur.1985.04060080095022. [DOI] [PubMed] [Google Scholar]