Abstract
The current study explored longitudinal evidence for prodromal symptoms of depression episodes. A model based on previous findings of the relations between prodromal and residual symptoms was described and used to generate hypotheses tested in this study. Data were analyzed from 160 participants from the Cognitive Vulnerability to Depression (CVD) Project (Alloy & Abramson, 1999) who experienced an episode of depression during the prospective follow-up period and 60 CVD participants who did not. Congruent with the hypothesis, individuals who subsequently developed an episode of depression experienced significantly greater numbers of depression symptoms in the period of time leading up to the acute episode compared with those who did not develop a depressive episode. Seven depression symptoms were particularly likely to appear before the onset of an acute episode. Further, all three predictions from the model were supported: the durations of prodromal and residual phases were correlated, the prodromal and residual symptom profiles were quite similar, and the order of symptom onset was significantly and highly negatively correlated with the order of symptom remission. Additionally, residual symptom profiles were similar to subsequent prodromal symptom profiles in individuals who experienced more than one depressive episode. These findings are discussed in terms of the importance of understanding the earliest prodromal symptoms to appear and their relation to the symptomatic course of depression episodes. Implications for early intervention are also discussed.
Keywords: Depression, prodrome, symptoms, course
Researchers and clinicians have long recognized the benefit of understanding the natural course of psychological disorders. Understanding how a disorder, especially an episodic one, will unfold and eventually remit over time can be invaluable for estimating prognosis and planning treatment. In the field of depression research, such understanding most often has been sought through studies of the number, severity and duration of episodes over time (i.e., Iacoviello et al., 2006). Far less attention has been paid to the symptomatic course of depressive episodes (i.e., the progression of symptom presentation and remission).
Relatively recently, the depressive symptoms appearing earliest, often before the acute episode, have garnered attention as possible prodromal symptoms (early symptoms or signs of an impending episode; e.g., Fava et al., 1990). Several preliminary studies investigating prodromal symptoms of depression have been conducted (see Jackson, Cavanaugh & Scott, 2003 for a review). In these studies, anxiety/tension, irritability, loss of interest, sleep disturbance, decreased drive or motivation, emotional distance, depressed mood, gastrointestinal problems, fatigue, impaired concentration and decreased energy are reported as prodromal symptoms occurring in a significant proportion of their samples. Additionally, among the studies reporting on the duration of unipolar depressive prodromes, the findings are mixed. The mean prodromal duration ranged from 6 weeks to 23 months. Taken together, there is a good deal of inconsistency across studies, both in terms of the prodromal symptom profiles experienced and their durations. One major limitation of these preliminary studies involves their retrospective nature. Longitudinal studies utilizing assessments sensitive to capture prodromal symptom presentation are thus warranted.
Consistency of depression symptoms across successive episodes, and across phases of individual episodes, is also an important area ripe for investigation. Identifying such symptom patterns could highlight some of the underlying pathological processes that are contributing to the onset and maintenance of depression episodes. Indeed, consistency of symptoms experienced within individuals across episodes of depression has been suggested (e.g., Paykel, Prusoff &Tanner, 1976), but these findings are mixed as other studies have not found a significant consistency of symptoms between episodes (e.g., Young et al., 1987) or only demonstrated consistency when the severity of the episodes were taken into account (e.g., Young et al., 1990). In terms of the prodromal phase of depression episodes, consistency within individuals across prodromes has been suggested in several preliminary studies of unipolar and bipolar depression (e.g., Fava et al., 1990; Molnar, Feeney & Fava, 1988; Smith & Tarrier, 1992; Keitner et al., 1996). Consistency in the early symptom presentation across individuals with the same subtype of depression has also been demonstrated for depressive episodes in seasonal affective disorder (SAD), where the core symptoms of SAD (hypersomnia, appetite increase and fatigue) were observed to typically be the earliest symptoms to appear (e.g., Young et al., 1991). Taken together, these studies could offer preliminary evidence that for a given individual or subtype of depression, depressive episodes might tend to begin according to consistent symptom sequences. However, longitudinal studies using assessments sensitive to prodromal symptom presentation have not been conducted to adequately address this question.
There is also preliminary evidence that the prodromal and residual symptoms of an episode of depression can be quite similar. Fava and colleagues (1994) found that the majority of residual symptoms present after treatment were also present in the prodromal phase of the disorder. Similarly, Mahnert and colleagues (1997) reported that in a sample of 15 individuals, prodromal and residual symptoms were similar within individuals based on retrospective recall. The applicability of these findings to our understanding of the relation between prodromal and residual symptoms in depression is tempered by the treatment received in these samples and the retrospective reporting. Still, they highlight the possibility that prodromal and residual symptoms are related.
Relations between early symptoms to appear and the latest to remit have been hypothesized in several theories of depression. Hopelessness theory of depression (Abramson, Metalsky & Alloy, 1989) and the dual vulnerability theory of seasonal affective disorder (see Young et al., 1991; 2008) both posit that the core symptoms of hopelessness depression (HD) and SAD would be the earliest symptoms to present in episodes of HD and SAD, respectively, and secondary symptoms would appear as a response to the core symptoms. Indeed, evidence has been presented to support the notion that the core symptoms of SAD (hypersomnia, appetite increase and fatigue) tend to appear before secondary symptoms (Young et al., 1991; 2008). Moreover, these theories both posit that the core symptoms would be the first to remit, then triggering the remission of the secondary symptoms. To our knowledge, no studies of the order of symptom remission in HD or SAD have been conducted to validate these hypotheses.
These theories are in contrast to the process proposed in “the rollback phenomenon” (Detre & Jarecki, 1971). According to the rollback phenomenon, as depression remits it will repeat, in reverse order, many of the stages and symptoms experienced as the episode developed. Accordingly, the prodromal symptoms of the disorder, representing the early stage, would be the last symptoms to remit, potentially explaining the relation between prodromal and residual symptomatology. Fava and colleagues (1994) argue that their findings, and those of Manhert and colleagues (1997), provide support for the rollback phenomenon. The rollback phenomenon hypothesis further presupposes a temporal relation between the period of development of the disorder and the duration of the recovery phase, suggesting that the duration of prodromal and residual phases would be similar. The rationale being that a long run-up to the acute phase would be indicative of a more chronic course of depression, including a longer residual phase. Studies of this relation have not been conducted to date.
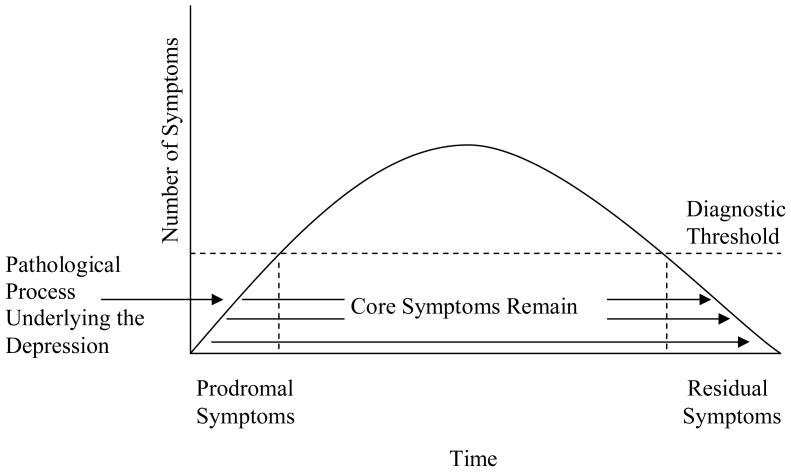
Piecing together the preliminary evidence for the occurrence of prodromal symptoms in depression episodes with the preliminary evidence for the rollback phenomenon reviewed above, a model for the relation between prodromal and residual symptoms and phases of depressive episodes can be generated (Figure 1). In this model, the prodromal symptoms form the core syndrome of the disorder, remain through the depressive episode, and are likely to remain as the last, potentially residual, symptoms. Episodes represent the more pronounced peaks of symptomatology.
Figure 1.
Model for the Development of Prodromal Symptoms and Their Relation to the Symptomatic Course of Depressive Episodes.
Taken together, the literature involving patterns of symptom presentation and remission in depression indicates that studying the early course of depression holds the potential to inform our understanding of the pathological processes underlying depression. However, empirically-based, theoretical conceptualizations of the depressive prodrome have not been generated or tested as yet, and are sorely needed. In addition, previous studies of the depressive prodrome used retrospective designs. The current study had two goals: 1) to enhance understanding of the early course of depression by identifying prodromal symptoms present in a longitudinal study of the course of depression, and 2) to test hypotheses regarding the relation between prodromal and residual symptoms and phases of depressive episodes.
It was hypothesized that individuals who developed an acute episode of depression would exhibit significantly more depressive symptoms in the run-up to the acute phase (prodromal symptoms) compared with a similar period of time for individuals who do not go on to develop an acute episode. Analyses were conducted to test this hypothesis, and to identify specific depressive symptoms that were particularly likely to appear before the acute phase of an episode of depression.
Three specific hypotheses predicted by the model outlined above (Figure 1) were also tested: 1) Individuals will display similar prodromal and residual symptom profiles for a given episode of depression; 2) Individuals will display similar durations of the period of prodromal and residual symptomatology for a given episode; and 3) the sequence of prodromal symptom presentation will appear, in reverse, as the symptoms of depression remit. Two additional, exploratory hypotheses about the relation between prodromal and residual symptom profiles were also tested: 4) Within individuals, the prodromal symptom profiles across successive episodes of depression will be similar; and 5) Within individuals who experience more than one episode of depression, the residual symptom profile of one episode will be similar to the subsequent prodromal symptom profile.
Method
Participants
This study used data from the Cognitive Vulnerability to Depression (CVD) Project (Alloy & Abramson, 1999), a prospective study of cognitive and psychosocial factors in the development of depressive disorders among college freshmen at high and low cognitive risk for depression. Details of the selection procedures are in Alloy et al. (2000). In Phase I, the Cognitive Style Questionnaire (CSQ; Alloy et al., 2000) and Dysfunctional Attitudes Scale (DAS; Weissman & Beck, 1978) were given to 5,378 freshmen. Those who scored in the highest or lowest quartiles on both the CSQ composite for negative events and the DAS were considered the high-risk (HR) and low-risk (LR) groups, respectively. In Phase II, a random subset of participants who met the Phase I criteria for the HR or LR groups were given an expanded Schedule for Affective Disorders and Schizophrenia-Lifetime interview (SADS-L; Endicott & Spitzer, 1978) by interviewers who were blind to risk status. Based on DSM-III-R (American Psychiatric Association, 1987) and Research Diagnostic Criteria (RDC; Spitzer et al., 1978) criteria, participants were excluded if they exhibited any current Axis I disorder, psychotic symptoms, or any serious medical illness. Participants were retained if they met diagnostic criteria for a past depressive disorder but had remitted for at least 2 months (to insure that any depression onsets during the prospective phase were new episodes and not relapses). On average, the most recent past episode of depression was 2.31 years (SD = 2.44 yrs.) before Phase I. The final CVD sample included 172 HR and 175 LR participants (see Alloy et al., 2000 for the sample demographics and representativeness).
The present study was based on a subset of 160 CVD Project participants who experienced at least one depressive episode (DSM-IV major depressive episode, RDC major episode or minor episode (definite) and no dysthymia) during the first 2.5 years of prospective follow-up, for a total of 331 episodes of depression included in the current report. Table 1 presents the demographic characteristics and cognitive risk status of the overall sample. Additionally, for the preliminary analyses, 60 of these participants were matched post-hoc on the basis of age, gender, ethnicity, study site, prior history of depression and cognitive risk status with 60 CVD participants who did not develop an acute episode of depression during the follow-up, to compare rates and patterns of prodromal symptom presentation between these groups. Table 2 provides the demographic and cognitive style characteristics of the matched participants in this subsample. For the primary hypotheses tested in this study, the larger sample of 160 depressed participants (331 episodes of depression) was utilized.
Table 1.
Demographic and Cognitive Risk Characteristics of the Sample
| High Risk | Low Risk | |
|---|---|---|
| Temple Site | ||
| Sample Size | 37 | 27 |
| Age | 18.59 (1.52) | 19.37 (2.23) |
| Ethnicity | 78.4% Caucasian | 70.3% Caucasian |
| Gender | 64.9% Female | 77.8% Female |
| Prior History of Depression | 24 | 15 |
| Wisconsin Site | ||
| Sample Size | 59 | 37 |
| Age | 18.44 (.50) | 18.68 (1.55) |
| Ethnicity | 98.3% Caucasian | 91.9% Caucasian |
| Gender | 72.4% Female | 75.6% Female |
| Prior History of Depression | 38 | 18 |
Note. Standard deviations in parentheses.
Table 2.
Demographic and Cognitive Risk Characteristics of the Match-Controlled Subsample
| Depressed Participants | Control Participants | |
|---|---|---|
| Temple Site | ||
| Sample Size | 26 | 26 |
| Age | 18.42 (0.76) | 18.42 (0.76) |
| Ethnicity | 76.9% Caucasian | 76.9% Caucasian |
| Gender | 88.5% Female | 88.5% Female |
| Cognitive Risk Status | 17 HR, 9 LR | 17 HR, 9 LR |
| Mean # Episodes Experienced | 1.62 (1.17) | 0 |
| Prior History of Depression | 15 | 15 |
| Wisconsin Site | ||
| Sample Size | 34 | 34 |
| Age | 18.24 (0.43) | 18.24 (0.43) |
| Ethnicity | 97.1% Caucasian | 97.1% Caucasian |
| Gender | 70.6% Female | 70.6% Female |
| Cognitive Risk Status | 12 HR, 22 LR | 12 HR, 22 LR |
| Mean # Episodes Experienced | 1.91 (1.19) | 0 |
| Prior History of Depression | 23 | 23 |
Note: Standard deviations in parentheses.
Measures
The Schedule for Affective Disorders and Schizophrenia- Lifetime version
(SADS-L; Endicott & Spitzer, 1978) is a widely used structured diagnostic interview that assesses current and past psychopathology according to the Research Diagnostic Criteria. The SADS-L was used in this study as part of the phase II screening procedure (described above). The SADS has demonstrated high inter-rater reliability across interview sessions and high test-retest reliability (Endicott & Spitzer, 1978).
For the purposes of the CVD project, the SADS was modified and expanded in several ways (Alloy & Abramson, 1999). First, additional questions were included to allow DSM-III-R diagnoses to be made. Second, a more precise set of initial “probes” was included to assess the persistence of depressed mood. Third, components of the Anxiety Disorders Interview Schedule (ADIS; DiNardo et al., 1985) were included in the anxiety section of the SADS. Fourth, some reorganization of the items was conducted such that all items relevant to a particular disorder, first current then past, were presented together. Last, questions were included to assess two cognitive subtypes of depression according to the hopelessness theory (Abramson, Metalsky, & Alloy, 1989) and Beck’s (1967) theory. The expanded version of the SADS-L, like the original version, has demonstrated high levels of inter-rater reliability, with kappas for all diagnoses ≥ .90 (Alloy et al., 2000). As regards validity, HR participants in the CVD project were found to have significantly greater lifetime prevalence and prospective incidence and recurrence of DSM-III-R, DSM-IV, and RDC major depression and RDC minor depression as assessed by the Exp-SADS-L than LR participants (Alloy et al., 2000; 2006).
To assess change in depression over the course of the study, the onset or offset of an episode and for tracking symptoms, an expanded SADS-Change (SADS-C) interview was conducted. The SADS-C expansion allowed for DSM-IV as well as RDC diagnoses. The SADS-L and SADS-C differ in that the “L” version was administered to assess current and past depressive experiences, whereas the “C” version was given every 6 weeks throughout the course of the first 2.5 years of follow-up to assess symptoms and episodes of depression during the prospective phase of the study. When an item was endorsed on the SADS-C, several examples were required before a positive rating was made, and strict dating of symptoms (onset and offset) was recorded. For the current study, the onset, severity, and duration of depressive symptoms, as well as the onset and offset of DSM-IV and RDC major and RDC minor depressive episodes, were obtained from this interview.
In the CVD project, inter-rater reliability of the expanded SADS-C was high for all diagnoses (kappas ≥ .90; Abramson et al., 1998; Alloy et al., 2006) as well as for day-by-day rating of individual SADS-C depressive symptoms (r = .89). This was based on an interrater reliability study of 80 SADS-C interviews (40 from each site) in which 2 different interviewers interviewed the same participant within 2 days of each other for the same 6-week interval.
For the current study, the following 29 depressive symptoms were assessed via the SADS-L and SADS-C and included in the analyses: sad mood, decreased appetite, weight loss, increased appetite, weight gain, initial insomnia, middle insomnia, early waking, hypersomnia, decreased energy, decreased interest or pleasure, self blame, difficulty concentrating, indecision, suicidal ideation, psychomotor agitation, psychomotor retardation, crying more, inability to cry, hopelessness, brooding/worry, decreased self-esteem, irritability, dependency, self-pity, somatic complaints, decreased effectiveness, helplessness, and decreased initiation of voluntary responses.
The Cognitive Style Questionnaire (CSQ; Alloy et al., 2000) was developed from the original and revised versions of the Attributional Style Questionnaire (ASQ; Seligman, Abramson, Semmel, & von Baeyer, 1979; Peterson & Villanova, 1988) to assess depressogenic inferences for positive and negative events, although only the composite score for negative events was used in the CVD project. The CSQ consists of 24 hypothetical situations representing equal numbers of positive and negative, interpersonal and achievement events. In the ASQ, participants are asked to identify the cause of an event, to assess its degree of importance and to make attributions as to the internality, stability and globality of the cause using a 1–7 rating scale. In creating the CSQ, Alloy and colleagues (2000) added inferences concerning characteristics about the self and event consequences and adapted the hypothetical situations to better suit a college population. Examples of the negative hypothetical situations from the CSQ include “You take an exam and receive a low grade on it” and “You go to a party with some friends and throughout the whole party people don’t act interested in you.” The CSQ composite for negative events consists of the total stability, globality, consequences and self-ratings for the 12 negative hypothetical events.
Within the CVD project, internal consistency of the CSQ was good for both negative and positive events (alphas= .88 and .86, respectively; Alloy et al., 2000). The 1-year test-retest reliability was also good (r= .80 for both negative and positive events; Alloy et al., 2000). With respect to validity, Abramson, Alloy and colleagues (Abramson et al., 1998; Alloy et al., 2000; 2006) have shown that the CSQ in combination with the Dysfunctional Attitudes Scale significantly predicted depressive episodes and suicidality.
The Dysfunctional Attitudes Scale (DAS; Weissman & Beck, 1978) is a 40-item self-report questionnaire measuring depressogenic attitudes on a 7-point scale that ranges from “totally agree” to “totally disagree.” The DAS assesses perfectionistic expectations of performance, concerns about disapproval, pessimism, and causal attributions. In the CVD project, 24 additional achievement- and interpersonally-oriented items were included. Examples of items on the DAS include “I can be happy if I’m not popular at all” and “If I do poorly in school or work, other people will think I’m dumb.”
In the CVD project, internal consistency for the expanded DAS was high (alpha = .90) and test-retest reliability for 1-year was good (r= .79; Alloy et al., 2000). As regards validity, Weissman and Beck (1978) found the correlation of the DAS with the BDI to range from .48 to .55 in a college sample. Dysfunctional attitudes as measured by the DAS have also been shown to differentiate a group of patients who were depressed from a non-depressed, mixed psychiatric or a non-depressed, normal control group (Hamilton & Abramson, 1983). Finally, risk group status in the CVD project, based on the CSQ and DAS, predicted lifetime history and prospective incidence of depressive disorders (Alloy et al., 2000; 2006).
Procedures
Participants in the CVD project provided informed consent and were randomly assigned to interviewers after the Phase II assessment using the Exp-SADS-L, They were interviewed every 6 weeks for the first 2.5 years of the study and every 4 months for the remaining 3 years. Each of these subsequent interviews included the Exp-SADS-C, among other assessments. Interviews were conducted in person, when possible; otherwise, interviews were conducted via telephone. Interviews were tape-recorded, providing an opportunity for independent tape reviews by other interviewers. This allowed for the assessment of inter-rater reliability.
Operational definition of prodromal, acute and residual phases and symptoms
In this study, the acute phase was marked by meeting diagnostic criteria for a DSM-IV major depressive episode or RDC criteria for a major or minor episode of depression, and ended when these diagnostic criteria were no longer met. Consistent with prior investigations, a symptom was identified as prodromal if it appeared at any time before the acute phase and remained consistently present into the acute phase. Accordingly, the prodromal phase was operationally defined as the period of time before the acute phase during which at least 1 symptom was continuously present. A symptom that was present at any time during the acute phase and continued beyond the acute phase was identified as a residual symptom. The residual phase was operationally defined as the period of time after the acute phase during which at least 1 symptom from the acute phase remained.
For 14 episodes of depression analyzed in this study, residual symptoms remained consistently into the next episode. In such cases, the residual symptom(s) that consistently remained into the subsequent episode were considered to also represent prodromal symptoms of the next episode, and we designated the halfway point between episodes as the end of the residual phase for episode one and the beginning of the prodromal phase for episode two. This was admittedly an imprecise method for distinguishing residual vs. prodromal symptoms and phases in these cases. However, it is noteworthy that this happened in only a small subsample of participants (14 episodes out of the larger sample of 331 episodes), so we do not believe that these symptoms significantly alter any of our analyses given the much larger overall sample size.
Results
Initial analyses
To support the existence and relevance of the prodromal phase of a depressive episode, the number of SADS-C symptoms present immediately before and leading into the acute phase of a depressive episode for 60 CVD participants that experienced a depressive episode was compared, using a t-test, to the number of slight or clinically significant SADS-C symptoms present during the corresponding period of time for the 60 matched participants without a depressive episode. Table 2 provides the demographic and cognitive risk characteristics of the 60 depressed CVD participants and the 60 matched, nondepressed participants.
Congruent with the hypothesis, depressed participants had a significantly greater number of symptoms during the prodromal period than non-depressed, matched participants (mean= 3.46 vs. 1.40 symptoms; t(118)= −2.043, p < .043). Further, χ2 analyses were conducted to identify symptoms significantly more likely to be present during the prodromal period among the depressed participants than the non-depressed participants. To adjust for multiple testing, only results with p < .01 were regarded as significant. These analyses identified seven symptoms: depressed mood (χ2 (1) = 6.992, p< .008), decreased interest in or pleasure from activities (χ2 (1) = 6.602, p< .01), decreased concentration (χ2 (1) = 6.755, p< .009), hopelessness (χ2 (1) = 8.818, p< .003), worrying/brooding (χ2 (1) = 7.500, p< .006), decreased self-esteem (χ2 (1) = 8.100, p< .004) and irritability (χ2 (1) = 6.600, p< .01).
Hypothesis 1
To test the hypothesis that individuals would display similar prodromal and residual symptom profiles for a given episode of depression, the prodromal and residual symptom profiles for each individual in the study, for each of 331 episodes of depression experienced, were compared by calculating Cohen’s kappa (κ; Cohen, 1960). Cohen’s kappa, a measure of homogeneity or agreement across rating periods which adjusts for the magnitude of agreement expected by chance, was calculated based on the presence or absence of the 29 SADS-C depression symptoms in each episode’s prodromal and residual phases. Such an analytic strategy has been employed previously in studies of the concordance of symptoms present during episodes of depression (e.g., Young et al., 1990). Specifically, to assess the concordance of prodromal and residual symptom occurrence for a given episode, the presence of prodromal and/or residual symptoms rated as “slight” or “clinically significant” on the SADS-C was coded for each period. Cohen’s κ was calculated as a measure of concordance of prodromal and residual symptoms for each episode of depression. Given that the distribution of κ’s was influenced by a number of 1.0 scores (indicating perfect concordance) and a Shapiro-Wilk test of departure from normality yielded p< .001, the median is presented as a more robust measure of the central tendency of the data than the mean. Across all episodes, the median κ= .605 (mean= 0.585, mode= 1.0).
To evaluate the effect of episode severity on symptom consistency across prodromal and residual phases, the sample was split into high and moderate severity groups (using a median split of the number of symptoms experienced during an episode, with the median being 7 symptoms) and the median kappa was calculated for each group. The moderate severity group demonstrated a lower symptom consistency across phases (n=101 episodes, median κ= .501) compared to the high severity group (n=230, median κ= .651).
Hypothesis 2
The correlation between the durations of prodromal and residual phases was computed for the 331 episodes in the sample. The mean duration of the prodromal phase was 44.75 days (s.d. = 39.73 days) and of the residual phase was 36.39 days (s.d = 27.05 days). Exploration of the data revealed that there were numerous outliers among both the prodromal and residual duration variables and their distributions were found to be non-normal (Shapiro-Wilk test of departure from normality yielded p< .001 for both variables). Accordingly, the nonparametric Spearman rank correlation (ρ), was computed to assess the significance of the correlation of the ranks of the data. The correlation was found to be moderate and significant, with ρ (329)= .486, p< .001.
Hypothesis 3
To test the hypothesis that the sequence of prodromal symptom presentation would appear, in reverse, as the symptoms of depression remit, Spearman’s rho (ρ) was computed on the order (ranks) of symptom onset and offset for a given episode. Symptoms of a given episode were ranked and coded in their order of onset and remission, with ties given to symptoms that appeared or remitted on the same day, and a value for ρ was calculated for each episode. Accordingly, a negative correlation would be expected if the early symptoms were the last symptoms to remit. The distribution of these correlation coefficients was not normally distributed, with a substantial number of −1.0 correlations and a Shapiro-Wilk test of departure from normality yielding p< .001. As such, the median is presented as a more robust measure of the central tendency of these data, as opposed to the mean. The median correlation of the order of symptom onset and remission was ρ= −0.642 (mean= −0.564, mode= −1.0).
Hypotheses 4 and 5
Eighty-one participants experienced more than 1 episode of depression during the prospective assessment period of the CVD Project, yielding a total of 252 episodes of depression. Fifty-seven of the 81 (70.0%) were classified as cognitive HR participants.
Cohen’s Kappa (κ) was calculated as a measure of the concordance of prodromal symptom profiles for each pair of successive episodes of depression for each participant. Kappas for each pair of successive episodes were then averaged for each participant. Participant mean kappas ranged from−.258 to 1.0 and the scores were normally distributed without any significant outliers. Across participants, the mean value for the concordance of prodromal symptom profiles across successive episodes of depression was κ= .40 (median= .338, mode= 1). When episode severity was taken into account, by comparing only pairs of episodes with similar intensities (i.e., the difference in the number of symptoms experienced during the episodes did not exceed 3 symptoms), the concordance of prodromal symptom profiles across successive episodes of depression was higher (n= 82 pairs of episodes; mean κ= .52, mode= 1.0).
Cohen’s kappa was also calculated as a measure of the concordance between residual symptoms and the subsequent prodromal symptom profile among participants experiencing more than one episode of depression. Kappas for each residual-prodromal phase pairing were averaged within each participant. Participant mean kappas ranged from −.031 to 1.0, but the distribution of these scores was not normally distributed, with a substantial number of 1.0 scores and a Shapiro-Wilk test of departure from normality yielding p< .001. As such, the median is presented as a more robust measure of the central tendency of these data, as opposed to the mean. Across participants, the median value for the concordance of residual and prodromal symptom profiles across successive episodes of depression was κ= .613 (mean= .593, mode= 1.0). When episode severity was taken into account by only comparing episodes of similar severity, the concordance of residual and prodromal symptom profiles across successive episodes of depression was higher (n= 82 pairs of episodes; mean κ= .67, mode= 1.0).
Discussion
An important preliminary finding of this study was that there does appear to be a discernable prodromal phase to depressive episodes, as well as several symptoms that appear to be common to the depressive prodrome across individuals. Seven symptoms were identified as being more likely to be present among individuals entering a depressive episode compared to individuals matched on age, gender, ethnicity, study site, prior history of depression and cognitive risk status, who did not develop an episode of depression. These included sad mood, decreased interest in or pleasure from activities, difficulty concentrating, hopelessness, worrying/brooding, decreased self-esteem and irritability. These symptoms appeared to be related to the prodromal phase and thus could represent early warning signs that an individual could be developing an acute episode of depression. The results of this study also suggest that indicators from this prodromal phase could highlight the expected course of the depressive episode, including the order of symptom offset and the duration of the remission phase. Moreover, the specific symptoms experienced in the prodrome could highlight some of the processes underlying the depression. Thus, this phase of the depressive experience is ripe for further study.
Three general hypotheses were tested in this study regarding the relations between prodromal and residual symptoms and phases of an episode of depression. First, the hypothesis that the profiles of the symptoms present in the prodromal and residual phases would be similar received substantial support, especially when taking episode severity into account. Additionally, results indicated that the order of symptom onset and remission was found to be substantially, negatively correlated, suggesting that the order of symptom remission was similar to the reverse of the order of onset. The earliest symptoms were among the very last to remit. These results provide strong evidence that prodromal symptoms are most likely to remain present throughout the depressive experience, and support the notion that these “primary” symptoms could represent the core syndrome of the disorder. The hypothesis that the durations of prodromal and residual phases would be correlated was also supported with a moderate, significant correlation. This is in line with predictions from the rollback theory, and suggests that the duration of the prodromal phase could be an indicator of how chronic the course of depression will be, including the amount of time symptoms might linger after the acute phase.
Taken together, the support for each of these three hypotheses begins to paint a picture of the relation between the earliest and latest, or the prodromal and residual, phases of a depressive episode. Figure 1 presents a graphical depiction of the relations supported in the current investigation, and suggests a model of the depressive episode whereby the prodromal symptoms are influenced by particular pathological processes underlying the depression (which could include stressful life events, biological processes, cognitive processes, etc.), form the core syndrome of the disorder, remain through the depressive episode, and are likely to remain as the last, potentially residual, symptoms. Episodes represent the more pronounced peaks of symptomatology.
The exploratory hypothesis that prodromal symptom profiles would be similar across episodes of depression was not strongly supported by the analyses conducted in this study. It would appear from these findings that individuals do not demonstrate a great degree of consistency in the earliest symptoms that present across episodes of depression. Similar results were obtained in a study of symptom consistency across episodes, which found that the degree of correlation observed between symptom profiles of subsequent episodes of depression was low; the agreement observed was largely that to be expected by chance (Young et al., 1990). However, Young and colleagues also demonstrated that when the total number of symptoms experienced was taken into account, and episodes are only compared with episodes that include similar numbers of symptoms overall, the concordance of symptom presentation was high. In the current study, accounting for episode severity did appear to result in a higher concordance of prodromal symptoms across episodes, although still not reaching a substantial level.
The exploratory hypothesis that the residual symptom profile would be similar to the subsequent prodromal symptom profile among participants who experienced more than one episode of depression was supported by the analyses conducted in this study. This finding is in line with previous studies, suggesting that the residual symptoms remaining after the acute phase of a depressive episode might eventually function as prodromal symptoms of the following episode (e.g., Fava et al., 1994).
The results of the current investigation are in line with prior theory as well as some preliminary investigations. The current results provide support for the rollback phenomenon proposed by Detre and Jarecki (1971). According to the rollback phenomenon, as a depression remits it will repeat, in reverse order, many of the stages and symptoms experienced as the episode developed. Accordingly, the earliest symptoms to appear would be the latest symptoms to remit, which was, in fact, the case in these data. This is also in line with previous findings by Fava and colleagues (1994) and Manhert and colleagues (1997), who also found that the earliest symptoms to appear (described as prodromal symptoms in these studies) were generally the latest to remit. Although these results do suggest that the earliest symptoms to appear are similar to those that remain and remit latest, the mechanisms responsible for such a phenomenon were beyond the scope of this investigation. These results do appear to support the rollback phenomenon, but this does not necessarily discount the processes hypothesized by competing theories such as hopelessness theory and the dual vulnerability theory. Taking from hopelessness theory and the dual vulnerability theory, perhaps the core symptoms need only begin to weaken to trigger the remission of secondary symptoms, and the primary symptoms, as the core of the episode, remain and remit latest. Further investigation of the mechanisms relating prodromal (primary) and secondary symptoms, especially as regards symptom onset and remission, are warranted.
An important implication of these findings is that they lend support to the staging method of conceptualizing depressive episodes, and specifically for the inclusion of prodromal and residual stages of depression in such models. Recently, Hetrick and colleagues (2008) have argued that the prodromal phase be considered as the earliest stage of the depressive experience, and the results of the current study support this. These results appear to indicate that current categorical definitions of onset and offset of depressive episodes may not adequately describe other significant aspects of depression, namely the prodromal and residual phases, which appear to be important indicators of an episode’s course and future prognosis. Importantly, these results highlighting the importance of the residual phase and symptoms also support the possible utility of sequential treatments for depression, whereby one form of therapy (e.g., pharmacotherapy) targeted at symptoms of the acute phase is followed by another therapeutic modality (e.g., psychotherapy) targeted at residual symptoms and relapse prevention (e.g., Fava, Ruini & Rafanelli, 2005).
In addition, the results of the current study indicating particular symptoms that were likely prodromal symptoms are in line with prior investigations. In particular, Fava et al. (1994) reported generalized anxiety and irritability as two symptoms that were particularly likely to appear before the acute phase of illness. The results of the current study also indicate that irritability is a likely prodromal symptom. The symptom of worry/brooding assessed in this study can also be likened to generalized anxiety, however, it is important to note that the worry/brooding symptom used in this study is broader than generalized anxiety and this should be taken into account when trying to compare across studies. Moreover, there has been increasing interest in the recent literature on subjective incompetence as a hallmark of demoralization, which can be thought of as a subclinical symptom and potential early indicator of depression (e.g., Cockram, Doros & de Figueiredo, 2009). In the context of the current study, subjective incompetence was not explicitly assessed. However, the symptoms of “dependency” and “decreased self-esteem”, as assessed by the SADS used in this study, could be thought to encompass individuals’ beliefs about themselves as incompetent or otherwise unworthy, and needing others for everyday things. Interestingly, dependency was not found to be a likely prodromal symptom in these data, whereas decreased self-esteem was. Although extrapolation from these data to other studies is difficult because the symptoms of dependency and decreased self-esteem are broader than subjective incompetence, these data might be thought to support the importance of subjective incompetence in the pathogenesis of depression, as evidenced by decreased self-esteem being a likely prodromal symptom.
These data also support one component of the etiological process hypothesized in hopelessness theory of depression (Abramson, Metalsky & Alloy, 1989). Specifically, hopelessness theory hypothesizes that particular cognitive vulnerabilities (i.e., a negative inferential style for the causes and consequences of life events) in the face of negative life events render one prone to developing hopelessness, which, in turn, serves as a proximal cause for the development of other depression symptoms and the subtype of hopelessness depression in particular. This implicates hopelessness as a potential prodromal symptom of depression. Indeed, the results of the current study suggest that hopelessness was one of the most common prodromal symptoms in this sample. Future research is warranted to evaluate the specificity of this prodromal symptom among individuals with the aforementioned cognitive vulnerabilities, as well as investigating the role of hopelessness in the development of other symptoms and acute episodes of depression.
It is important to note that individual differences in symptom presentation exist, and the appearance of these symptoms will not always indicate that an episode of depression is forthcoming. Certainly, there is a risk in overpathologizing the presentation of prodromal symptoms. It is thus important for individuals, as well as their treatment providers, to be mindful of the specific symptoms that are salient to them, across episodes of depression, before ascribing too much importance to the emergence of specific symptoms of depression.
This study has several strengths. First, the longitudinal design enabled the onset and remission of depression symptoms to be chronicled in real time, minimizing the effects of retrospective reporting to several weeks. The frequent (every 6 weeks) assessments increased the validity of the data regarding the onset and offset of symptoms. Moreover, the broad range of symptoms assessed, and the sensitive nature of the measures, allowed for the study of many potential depressive symptoms at subclinical levels. These are all improvements over the methodologies of previous studies of depressive prodromes. One particular limitation of the current study involves the sample analyzed, which was not especially diverse with respect to ethnicity and gender, included some participants who had a prior history of depression and consisted primarily of college students, who tend to exhibit a relatively restricted range of psychopathology. Additionally, participants were selected for the CVD Project based on high or low cognitive vulnerability to develop depression, which also could limit the generalizability of the current findings to the larger population. Another limitation of the current study is that the analyses conducted did not allow for investigation of third variables (beyond episode severity) that could influence symptom patterns or the consistency of symptoms across phases, such as life stress, personality variables, etc. Future investigations would do well to include these variables to determine their effects on symptom presentation and consistency.
In conclusion, the current study provided support for the concept of a prodromal phase of depressive episodes. Several hypotheses regarding relations between the early and late course, or prodromal and residual phases, of depression were also supported. Namely, the duration of the prodromal and residual phases of depressive episodes are significantly correlated. The symptoms to present earliest, during the depressive prodrome, are also likely to remit latest, often remaining as residual symptoms. Further, the order of symptom onset is strongly related to the order of symptom offset, in reverse. Although the prodromal phases of subsequent episodes did not demonstrate a compelling degree of similarity in this study, it was demonstrated that the residual symptoms lingering after an acute episode do appear to remain or reemerge as prodromal symptoms of the next episode. These symptoms that present earliest and remit latest are important insofar as they might be thought to comprise the core syndrome of the depressive episode. Their nature could potentially highlight processes underlying the depression, and they could represent important treatment targets if they are, in fact, the core syndrome of the episode. Future research should investigate further the role of prodromal symptoms in the course of a depressive episode. Moreover, research is warranted into the specific treatment of prodromal symptoms of depression. Such early intervention could help thwart the development of an acute episode of depression. Or, when an acute episode has already developed, understanding the core pathology, as reflected by the early course of the episode, might help in focusing more effective treatments.
Table 3.
Frequency of Symptom Presentation in the Prodromal, and Residual Phases (N= 331 episodes)
| Symptom | Prodromal Frequency | Residual Frequency |
|---|---|---|
| Depressed mood | 95 | 79 |
| Decreased appetite | 42 | 40 |
| Weight loss | 13 | 12 |
| Increased appetite | 10 | 12 |
| Weight gain | 20 | 17 |
| Initial insomnia | 29 | 30 |
| Middle insomnia | 13 | 10 |
| Early waking | 11 | 14 |
| Hypersomnia | 23 | 22 |
| Decreased energy | 38 | 35 |
| Decreased interest or pleasure | 82 | 75 |
| Self blame | 51 | 55 |
| Decreased concentration | 78 | 75 |
| Indecision | 6 | 8 |
| Suicidality | 6 | 5 |
| Psychomotor agitation | 6 | 5 |
| Psychomotor retardation | 10 | 7 |
| Crying more frequently | 34 | 31 |
| Inability to cry | 4 | 2 |
| Hopelessness | 195 | 201 |
| Worrying/Brooding | 104 | 118 |
| Decreased self-esteem | 195 | 199 |
| Irritability | 85 | 72 |
| Dependency | 45 | 46 |
| Self-pity | 24 | 28 |
| Somatic complaints | 5 | 4 |
| Decreased effectiveness | 38 | 37 |
| Helplessness | 35 | 28 |
| Decreased initiation of voluntary responses | 19 | 23 |
Acknowledgments
The research reported in this article was supported by National Institute of Mental Health Grant MH 48216 to Lauren B. Alloy and Grant MH 43866 to Lyn Y. Abramson. This article was prepared with support from the VA VISN3 Mental Illness Research, Education and Clinical Center.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ABN
Contributor Information
Brian M. Iacoviello, VA VISN3 Mental Illness Research, Education and Clinical Center (MIRECC) and Mount Sinai School of Medicine
Lauren B. Alloy, Department of Psychology, Temple University
Lyn Y. Abramson, Department of Psychology, University of Wisconsin-Madison
Jimmy Y. Choi, Department of Psychology, Temple University
References
- Abramson L, Alloy L, Hogan M, Whitehouse W, Cornette M, Akhavan S, Chiara A. Suicidality and cognitive vulnerability to depression among college students. Journal of Adolescence. 1998;21:473–487. doi: 10.1006/jado.1998.0167. [DOI] [PubMed] [Google Scholar]
- Abramson L, Metalsky G, Alloy L. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Alloy L, Abramson L. The Temple-Wisconsin Cognitive Vulnerability to Depression Project: Conceptual Background, Design, and Methods. Journal of Cognitive Psychotherapy: An International Quarterly. 1999;13:227–262. [Google Scholar]
- Alloy L, Abramson L, Hogan M, Whitehouse W, Rose D, Robinson M, Kim R, Lapkin J. The Temple-Wisconsin Vulnerability to Depression Project: Lifetime history of Axis I psychopathology in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2000;109:403–418. [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, Rose D. Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2006;115:145–156. doi: 10.1037/0021-843X.115.1.145. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: Author; 1987. [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Harper & Row; 1967. [Google Scholar]
- Cockram CA, Doros G, de Figueiredo JM. Diagnosis and Measurement of Subjective Incompetence: The Clinical Hallmark of Demoralization. Psychotherapy and Psychosomatics. 2009;78:342–345. doi: 10.1159/000235737. [DOI] [PubMed] [Google Scholar]
- Cohen J. A coefficient of agreement for nominal tables. Educational and Psychological Measurement. 1960;20:37–46. [Google Scholar]
- Detre P, Jarecki H. Modern Psychiatric Treatment. Philadelphia: Lippincott; 1971. [Google Scholar]
- DiNardo P, Barlow D, Cerny J, Vermilyea B, Vermilyea J, Himadi W, Waddell M. Anxiety Disorders Interview Schedule-Revised (ADIS-R) Albany, NY: Phobia and Anxiety Disorders Clinic, State University of New York at Albany; 1985. [Google Scholar]
- Endicott J, Spitzer R. A diagnostic review of the Schedule for Affective Disorders and Schizophrenia. American Journal of Psychiatry. 1978;135:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Fava G, Grandi S, Canestrari R, Molnar G. Prodromal symptoms in primary major depressive disorder. Journal of Affective Disorders. 1990;19:149–152. doi: 10.1016/0165-0327(90)90020-9. [DOI] [PubMed] [Google Scholar]
- Fava G, Grandi S, Zilezny M, Canestrari R, Morphy M. Cognitive behavioral treatment of residual symptoms in primary major depressive disorder. American Journal of Psychiatry. 1994;151:1295–1299. doi: 10.1176/ajp.151.9.1295. [DOI] [PubMed] [Google Scholar]
- Fava G, Kellner R. Prodromal symptoms in affective disorders. American Journal of Psychiatry. 1991;148:823–830. doi: 10.1176/ajp.148.7.823. [DOI] [PubMed] [Google Scholar]
- Fava G, Ruini C, Rafanelli C. Sequential treatment of mood and anxiety disorders. Journal of Clinical Psychiatry. 2005;66:1392–400. doi: 10.4088/jcp.v66n1108. [DOI] [PubMed] [Google Scholar]
- Hamilton E, Abramson L. Cognitive patterns and major depressive disorder: A longitudinal study in a hospital setting. Journal of Abnormal Psychology. 1983;92:173–184. doi: 10.1037//0021-843x.92.2.173. [DOI] [PubMed] [Google Scholar]
- Hetrick SE, Parker AG, Hickie IB, Purcell R, Yung AR, McGorry PD. Early Identification and Intervention in Depressive Disorders: Towards a Clinical Staging Model. Psychotherapy and Psychosomatics. 2008;77:263–270. doi: 10.1159/000140085. [DOI] [PubMed] [Google Scholar]
- Iacoviello BM, Alloy LB, Abramson LY, Whitehouse WG, Hogan ME. The course of depression in individuals at high and low cognitive risk for depression: A prospective study. Journal of Affective Disorders. 2006;93:61–69. doi: 10.1016/j.jad.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Jackson J, Cavanagh J, Scott J. A systematic review of manic and depressive prodromes. Journal of Affective Disorders. 2003;74:209–217. doi: 10.1016/s0165-0327(02)00266-5. [DOI] [PubMed] [Google Scholar]
- Keitner G, Solomon D, Ryan C, Miller I, Mallinger A, Kupfer D, Frank E. Prodromal and residual symptoms in bipolar I disorder. Comprehensive Psychiatry. 1996;37:362–367. doi: 10.1016/s0010-440x(96)90018-8. [DOI] [PubMed] [Google Scholar]
- Manhert F, Reicher H, Zalaudek K, Zapotoczky H. Prodromal and residual symptoms in recurrent depression. European Neuropsychopharmacology. 1997;7(supplement 2):s159–s160. [Google Scholar]
- Molnar G, Feeney G, Fava G. Duration and symptoms of bipolar prodromes. American Journal of Psychiatry. 1988;145:1576–1578. doi: 10.1176/ajp.145.12.1576. [DOI] [PubMed] [Google Scholar]
- Paykel E, Prusoff B, Tanner J. Temporal stability of symptom patterns in depression. British Journal of Psychiatry. 1976;128:369–374. doi: 10.1192/bjp.128.4.369. [DOI] [PubMed] [Google Scholar]
- Peterson C, Villanova P. An expanded attributional style questionnaire. Journal of Abnormal Psychology. 1988;97:87–89. doi: 10.1037//0021-843x.97.1.87. [DOI] [PubMed] [Google Scholar]
- Seligman M, Abramson L, Semmel A, von Baeyer C. Depressive attributional style. Journal of Abnormal Psychology. 1979;88:353–357. doi: 10.1037//0021-843x.88.3.242. [DOI] [PubMed] [Google Scholar]
- Smith J, Tarrier N. Prodromal symptoms in manic depressive psychosis. Social Psychiatry and Psychiatric Epidemiology. 1992;27:245–248. doi: 10.1007/BF00788937. [DOI] [PubMed] [Google Scholar]
- Spitzer R, Endicott J, Robins E. Research Diagnostic Criteria: Rationale and reliability. Archives of General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Weissman A, Beck A. Development and validation of the Dysfunctional Attitudes Scale: A preliminary investigation. Paper presented at the meeting of the American Educational Research Association; Toronto, Ontario, Canada. 1978. [Google Scholar]
- Young M, Fogg L, Scheftner W, Fawcett J. Concordance of symptoms in recurrent depressive episodes. Journal of Affective Disorders. 1990;20:79–85. doi: 10.1016/0165-0327(90)90120-w. [DOI] [PubMed] [Google Scholar]
- Young M, Keller M, Lavori P, Scheftner W, Fawcett J, Endicott J, Hirschfeld R. Lack of stability of the RDC endogenous subtype in consecutive episodes of major depression. Journal of Affective Disorders. 1987;12:139–143. doi: 10.1016/0165-0327(87)90006-1. [DOI] [PubMed] [Google Scholar]
- Young M, Reardon A, Azam O. Rumination and vegetative symptoms: A test of the Dual Vulnerability Model of seasonal depression. Cognitive Therapy and Research. 2008;32:567–576. [Google Scholar]
- Young M, Watel L, Lahmeyer H, Eastman C. The temporal onset of individual symptoms in winter depression: differentiating underlying mechanisms. Journal of Affective Disorders. 1991;22:191–197. doi: 10.1016/0165-0327(91)90065-z. [DOI] [PubMed] [Google Scholar]