Abstract
Attenuated Yersinia pestis pgm strains, such as KIM5, lack the siderophore yersiniabactin. Strain KIM5 does not induce significant pneumonia when delivered intranasally. In this study, mice were found to develop pneumonia after intranasal challenge with strain KIM5 when they were injected intraperitoneally with iron dextran, though not with iron sulfate. KIM5-infected mice treated daily with 4 mg iron dextran died in 3 days with severe pneumonia. Pneumonia was less severe if 4 mg iron dextran was administered only once before infection. The best-studied experimental vaccine against plague currently consists of the Yersinia pestis capsular antigen F1 and the type 3 secreted protein LcrV. The F1 antigen was shown to be protective against KIM5 infections in mice administered iron dextran doses leading to light or severe pneumonia, supporting the use of an iron dextran-treated model of pneumonic plague. Since F1 has been reported to be incompletely protective in some primates, and bacterial isolates lacking F1 are still virulent, there has been considerable interest in identifying additional protective subunit immunogens. Here we showed that the highly conserved Psa fimbriae of Y. pestis (also called pH 6 antigen) are expressed in murine organs after infection through the respiratory tract. Studies with iron dextran-treated mice showed that vaccination with the Psa fimbrial protein together with an adjuvant afforded incomplete but significant protection in the mouse model described. Therefore, further investigations to fully characterize the protective properties of the Psa fimbriae are warranted.
Yersinia pestis, a Gram-negative bacterium belonging to the family Enterobacteriaceae, is the causative agent of plague, a disease that affects a variety of mammalian hosts and that can be transmitted by various arthropod vectors. Humans are susceptible to Y. pestis, whether transmitted by aerosol or by infected fleas, causing the highly lethal pneumonic plague or bubonic plague, respectively (53). Aerosol infections by Y. pestis remain a concern for public health (12). The only currently available tools for combating Y. pestis in the United States are antibiotics, since manufacture of the previously licensed formalin-killed Y. pestis vaccine that was used by the U.S. military during the Vietnam War (41) stopped in 1998. Although effective against bubonic plague, this vaccine was not efficiently protective against pneumonic plague and caused significant side effects (11). The emergence of multiple antimicrobial resistance in Y. pestis (72) and the lack of a safe and effective vaccine have been the impetus for the search for new inhibitory drugs as well as a better vaccine (48, 49).
Y. pestis has been classified as a Category A select agent (8) requiring special precautions, particularly because of the risk of pneumonic plague due to bacterial aerosolization. One of the major impediments to studying the biology and pathogenesis of Y. pestis is that many laboratories do not have access to the required biosafety level 3 (BSL-3) facilities and therefore must work with attenuated strains that were excluded from the CDC select-agents list. Such strains lack either the pgm locus (e.g., KIM5) or the virulence plasmid pCD1 (51). A major virulence component of the pgm locus is the yersiniabactin (Ybt siderophore)-dependent iron transport system, which is essential for plague infection from peripheral sites (52). The pCD1 plasmid encodes a type III secretion system (T3SS, or Yops regulon) that, upon contact with host cells (or in low calcium concentrations in vitro), produces an elaborate injection machinery used to transfer a set of effector proteins with potent antiphagocytic and/or anti-inflammatory effects (2, 67) directly to the cytosol of the eukaryotic cell. Mutants lacking pgm or pCD1 are safer to manipulate, allowing experimental studies to be carried out in BSL-2 laboratories. However, the disease progression elicited by these strains does not recapitulate that observed with fully virulent strains (44), and in comparison to the wild-type strain, these strains are highly attenuated by any natural route of infection. Specifically, the Δpgm strain KIM5 is attenuated when given subcutaneously (s.c.) (52). Similarly, another Δpgm derivative of the virulent strain KIM, strain D27 (KIM D27), was unable to grow to high numbers in the lungs of intranasally infected mice, suggesting that bacterial growth was contained by the host's innate immune system. Moreover, these mice did not develop significant pneumonia, as they would if infected with wild-type Y. pestis strains (33). However, strain KIM D27 was still able to spread and grow in spleens and livers. This suggested that the iron uptake system of the pgm locus was needed to counteract iron restriction in the lungs. Interestingly, the results of earlier studies suggested that parenteral administration of iron sulfate to mice could bypass the need for yersiniabactin, rendering a parenterally administered Y. pestis Δpgm mutant fully virulent (10). However, a recent study showed that the use of the same approach to induce pneumonic plague after intranasal (i.n.) administration of pgm strain KIM D27 was not successful (33). This study also highlighted the toxicity of ferrous chloride, limiting administration doses to 0.5 mg per mouse. The latter result was consistent with the early toxicity data for inorganic iron at 30 to 60 mg/kg of body weight (26).
The toxicity problem of inorganic iron and the need for iron treatments for various medical conditions led to the development of less-toxic colloids consisting of various carbohydrates with ferric (oxy)hydroxide (16). In agreement with the results of earlier studies with inorganic iron, intraperitoneal (i.p.) administration of colloidal iron to mice subsequently infected subcutaneously with a Y. pestis pgm strain resulted in death, with histological lesions in the livers and spleens resembling those resulting from infection with a virulent strain (68). A variety of more-recent models of bacterial infections were developed by taking advantage of the extremely low toxicity of the colloid iron dextran, administrations of which in the milligram range were shown to be nontoxic (29, 62, 75). Based on the success of these models, we undertook experiments to determine whether the administration of high doses of iron dextran would permit Y. pestis to grow in the lungs of i.n. infected mice and cause local inflammation. Here we describe the development of a BSL-2 pneumonic plague model in mice based on the administration of iron dextran. In contrast to the negative results obtained with iron chloride, the use of iron dextran has allowed us to bypass toxicity problems and to take advantage of its favorable pharmacokinetic properties, such as slower clearance and a longer half-life for iron than those with other colloidal or inorganic iron preparations (16).
Our model was tested by confirming the expected protective property of F1 in pneumonic plague. We also used the model to evaluate the potential protective property of the Psa fimbriae (pH 6 antigen). Both F1 and Psa are surface structures that share the structural properties of homopolymeric fimbriae, each formed by a protein subunit that requires its own chaperone and usher proteins for export. Structural studies have classified F1 and Psa within a family of fimbrial polyadhesins assembled by FGL chaperones (for their long F1 and G1 β-strands) (76). The F1 capsular antigen is an efficient immunogen that is protective by itself in a murine model of pneumonic plague with F1+ strains (4). The protective property of the F1 immunogen can be attributed in great part to its polymeric structure and in vivo surface exposure. Similarly, mixtures of fimbriae and surface-exposed adhesins of other pathogens have been used successfully as commercial vaccine components for both humans and animals (17, 43, 54). Surface-expressed antigens such as F1 induce opsonizing and/or antivirulence antibodies, and such antibodies by themselves are protective (28). A role for opsonization by antibodies directed toward Y. pestis surface antigens is suggested by studies that showed that neutrophil depletion (15) or inhibition of cytokines that boost the antimicrobial activity of macrophages (18, 50) interfered with antibody-mediated protection. Properties of Psa similar to those of F1, such as its polymeric structure and bacterial surface location, make it an attractive vaccine candidate. Therefore, we evaluated Psa for its in vivo expression, immunogenicity, and protective properties by using the pneumonic plague model that we developed.
MATERIALS AND METHODS
Reagents and antibodies.
All bacteriological medium components and Freund's adjuvants were from Difco (BD Diagnostics, NJ). Iron dextran (ferric hydroxide dextran complex) was from Sigma-Aldrich (St. Louis, MO). Aluminum hydroxide (Alhydrogel) was obtained from Accurate Chemical (Westbury, NY). The specific rabbit antisera against the Y. pestis Psa and F1 proteins have been described previously (37).
Bacterial strains and plasmid constructs.
The Escherichia coli and Y. pestis strains and the plasmids used in this study are listed in Table 1. E. coli was routinely grown at 37°C in Luria-Bertani (LB) medium, supplemented with ampicillin (200 μg/ml) when appropriate. Y. pestis strains were grown overnight in brain heart infusion broth (BHI), at 26°C, diluted 1:10 in fresh BHI containing 2.5 mM CaCl2, buffered to pH 6.0 with 0.1 M MES (morpholineethanesulfonic acid), and cultured overnight at 37°C. Bacterial counts were determined on TB (13 g tryptose broth, 2.5 g NaCl, and 3.0 g Bacto beef extract paste in 1 liter) agar plates. Y. pestis KIM5 mutants DSY24 and DSY39 were constructed by allelic exchange, as described previously for the same mutations prepared in Y. pestis KIM6 (37). Maintenance of the KIM5 plasmids in the mutants was checked by agarose gel electrophoresis.
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Genotype or characteristic | Source or reference |
|---|---|---|
| Strains | ||
| E. coli | ||
| BL21(DE3) | F−ompT hsdSB(rB− mB−) dcm gal (DE3) | Novagen (Madison, WI) |
| Y. pestis | ||
| KIM5 | pCD1+ (LCR+) pgm (Pgm−) | 23 |
| KIM6 | KIM5 pCD1− (LCR−) | 23 |
| DSY24 | KIM5 Δcaf::blaM | This study |
| DSY39 | KIM5 Δcaf::blaM Δpsa::aphA | This study |
| Plasmids | ||
| pCS267 | pBR322-psaABC | 37 |
| pCS274 | pET16-caf1M-caf1A-caf1 | 37 |
| pDMS167 | pBR322fas (987P+) | 59 |
Isolation of fimbriae.
Recombinant Psa, F1, or 987P fimbriae were expressed on the bacterial surface of E. coli BL21(DE3) transformed with plasmid pCS267, pCS274, or pDMS167, respectively (Table 1). The surface-expressed proteins were isolated by heat extraction (20, 37) using the following modifications. For the Psa preparation, bacteria were inoculated in LB medium supplemented with ampicillin and were grown overnight at 37°C. Fresh LB medium was subsequently inoculated with 1% of this culture, which was then grown at 37°C for 5 to 7 h (to an optical density at 600 nm [OD600] of ∼0.8). The bacteria were harvested by centrifugation at 4,000 × g for 15 min. Next, the cell pellets were suspended in 0.5 mM Tris-HCl (pH 7.4)-75 mM NaCl and were treated at 58°C for 30 min. After centrifugation, ammonium sulfate was added to the supernatant or to the spent medium to 0.5% saturation, and the two fractions were incubated overnight on ice. The precipitated proteins were separated by centrifugation and shown to contain mainly contaminants. The supernatants from the bacterial surface and the spent medium were then subjected to a second precipitation step by addition of a saturated ammonium sulfate solution to reach 30% saturation. Proteins that precipitated overnight at 4°C were collected by centrifugation at 10,000 × g for 30 min and were dialyzed extensively against distilled water. F1 and 987P preparations were made essentially as described above, with the following minor modifications. F1 expression was induced by addition of 0.25 mM isopropyl-β-d-thiogalactopyranoside (IPTG) to the bacterial culture (OD600, ∼0.5) and incubation for 2 h at 37°C. The 987P fimbriae were prepared directly from overnight cultures. The heat treatments to isolate F1 and 987P were done at 60°C and 62°C, respectively. The final precipitation step for 987P preparation used a 50% saturated ammonium sulfate solution. The protein concentrations of the fimbrial preparations were determined to be 2.0 to 2.5 mg/liter of bacterial culture for Psa, 2.8 to 4.0 mg/liter for F1, and 3.0 to 3.5 mg/liter for 987P (39). The purity of the proteins (>95%) was confirmed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and Coomassie blue staining. The fimbrial preparations were further purified by affinity chromatography with immobilized polymyxin B to remove excess endotoxin. For this purpose, the proteins (4 mg per 2 ml endotoxin-free distilled water) were passaged several times through columns of 2 ml Detoxi-Gel (Pierce), as recommended by the manufacturer. The endotoxin levels of the purified proteins (<0.53 endotoxin units [EU]/dose of 40 μg antigen, corresponding to LcrV and F1 doses administered in a human clinical trial) were significantly below the FDA acceptable levels (350 EU/dose for a 70-kg human), as determined by the Limulus amoebocyte lysate assay (Lonza Walkersville Inc., MD) using E. coli 0111:B4 lipopolysaccharide (LPS) as a standard (6, 74).
Infection of mice.
Six- to 8-week-old female C57BL/6 mice were purchased from the Jackson Laboratory (Bar Harbor, ME). All experiments were performed by following the guidelines of the University of Pennsylvania Institutional Animal Care and Use Committee (IACUC), and animals were provided food and fresh water ad libitum during the experiment. Bacteria were grown at 37°C and were washed in sterile phosphate-buffered saline (PBS). Numbers of CFU inoculated were determined by plating serial dilutions onto TB agar plates (21). Mice were anesthetized with ketamine and xylazine (100 and 10 mg/kg of body weight) i.p. and were inoculated by the i.n. route with 20 μl of Y. pestis in PBS. In order to set the conditions for iron supplementation in mice, groups of five to eight mice received 1 to 10 mg iron (formulated as iron dextran) i.p. 2 to 3 h before i.n. inoculation of 1 × 105 CFU of Y. pestis strain KIM5 or KIM6. In some experiments, 0.75 to 2.0 mg iron dextran was delivered i.n. 3 h after the bacterial inoculation. Where indicated, the i.p. iron dextran was administered once a day during the course of the experiment. Mice were monitored for survival twice daily for 10 days. For experiments to determine the 50% lethal dose (LD50), groups of 10 mice were infected intranasally with serial 10-fold dilutions of Y. pestis strain KIM5, ranging from 10 CFU to 1 × 105 CFU. Animals that were moribund, as determined by IACUC guidelines, were euthanized; otherwise, animals were euthanized at the end of the experiment. Lungs and spleens were surgically removed and homogenized in 5.0 ml of sterile PBS by using a Stomacher Lab Blender (Seward Medical Limited), and the CFU per organ for each strain was calculated by plating serial dilutions onto TB agar.
Histopathology and immunohistochemistry.
Mice infected i.n. with 1 × 105 to 4 × 105 CFU of Y. pestis strain KIM5 were euthanized at various time points postinfection (p.i.). All tissues were fixed in 10% buffered formalin, sectioned, dehydrated, and paraffin embedded. Glass slide-mounted serial sections were stained with hematoxylin and eosin (H&E). Following a complete necropsy of each mouse, all tissues were collected and were carefully examined grossly and microscopically. All lung lobes were blindly evaluated, and histopathological scorings were done on individual mice. For this purpose, lesion numbers were counted, and each lesion was graded as 1 (minimal), 2 (mild), 3 (moderate), or 4 (severe) by evaluating its size and the presence of edema, inflammatory cells (such as macrophages and neutrophils), and necrotic cells. A cumulative pathology score was calculated for each mouse by adding the grades of all of its pulmonary lesions. For indirect immunohistochemistry, tissue sections were treated with polyclonal rabbit anti-F1 or anti-Psa antisera that had been adsorbed with strain DSY39 (Y. pestis psa caf) and E. coli BL21(DE3) (Table 1). All reactions were performed at room temperature. Tissue sections were treated with H2O2 for 10 min to inactivate endogenous peroxidases and were incubated with the primary antibody for 30 min, followed by a biotinylated anti-rabbit antibody for 15 min, horseradish peroxidase (HRP)-conjugated streptavidin for 15 min, and 3,3′-diaminobenzidine as a chromogen for 3 min. Counterstaining was done using Mayer's hematoxylin; the slides were then dehydrated, and coverslips were applied. The negative controls were prepared using N-Universal Negative Control (cocktail mixture of nonspecific rabbit IgG, IgM, IgG2a, IgG2b, and IgG3; DakoCytomation, Carpinteria, CA) instead of the primary antibodies.
Animal immunizations and bacterial challenge studies.
For vaccination, the purified proteins were mixed with an equal volume of the adjuvant Alhydrogel or Freund's complete adjuvant (FCA) to yield a final protein concentration of 400 μg/ml. Protein-adjuvant mixtures containing 40 μg of antigen were administered s.c. to mice (6 to 10 mice/group), followed by one s.c. boost immunization of the same dose in Alhydrogel, or two s.c. boost immunizations of the same dose in Freund's incomplete adjuvant (FIA), at 14- to 21-day intervals post-primary vaccination. The corresponding control groups were vaccinated with Alhydrogel and 987P, Alhydrogel alone, or FCA with FIA as the boost. The vaccinated mice were challenged with Y. pestis KIM5 2 weeks after the last immunization.
ELISA.
Sera collected from individual mice at the end of the vaccination trials were assayed for anti-F1 or anti-Psa IgG antibodies by a standard enzyme-linked immunosorbent assay (ELISA) on individual animals, with 0.5 μg/100 μl of either recombinant F1 or recombinant Psa applied to each well of a 96-well microtiter plate. The endpoint titers were determined by the highest serum dilutions with A450 values that were at least twice the A450 values for blank wells (not coated with antigen).
Statistical analysis.
Groups of mice were compared by using the unpaired Student t test, and survival curves were analyzed by the Mantel-Cox log rank test (statistical significance at a P value of <0.05), using Prism, version 5 (GraphPad Software, Inc., La Jolla, CA). LD50s and median survival times (MST) were determined by standard methods (73).
RESULTS
Inorganic iron does not suppress the attenuated phenotype of Y. pestis pgm strain KIM5 in murine lungs.
C57BL/6 mice challenged i.n. with 105 CFU of Y. pestis KIM5 showed a lethality of only 60% with an MST of 9 days (Fig. 1 A). These mice showed no noticeable macroscopic signs of pneumonia, consistent with the low numbers of bacteria in their lungs (∼104 CFU) (Fig. 1B), which did not increase over time (data not shown). No significant histological changes were observed in the lungs of dead or euthanized moribund mice at days 6 to 9 (Fig. 2 A and B) or in those of a mouse euthanized at an earlier time point, day 3 (not shown). In contrast, the spleens of these mice had moderate hyperplasia and sporadic single-lymphocyte death (not shown) with significantly higher numbers of strain KIM5 than numbers in lungs (Fig. 1B), revealing bacteremic spread. These results indicated that pgm strain KIM5 administered into the respiratory tract kills mice following bacteremia without the typical pneumonic lesions and the concomitant uncontrolled bacterial growth characteristic of pneumonic plague induced by fully virulent strains (32). Y. pestis pgm mutants lack the yersiniabactin-dependent iron transport system, which was shown to be essential for plague infection from s.c. or i.p. injections (52). Since earlier studies had shown that the need for yersiniabactin can be bypassed by iron treatment in murine models of bubonic plague (10), we undertook experiments to determine whether i.n. infection of iron-treated mice with a Y. pestis pgm mutant can recapitulate the bacterial multiplication and lung lesions typical of pneumonic plague. Iron sulfate administered i.p. (0.4 mg for the first day and 0.2 mg per following day) to C57BL/6 mice before an i.n. challenge with 105 CFU of strain KIM5 did not result in bacterial growth accompanied by pulmonary lesions (data not shown). Lee-Lewis and Anderson recently described comparable results in a study with BALB/c mice challenged i.n. with pgm strain KIM D27, where despite persistent low-level colonization of the lungs, the typical pulmonary inflammation and disease pathology of pneumonic plague were absent (33).
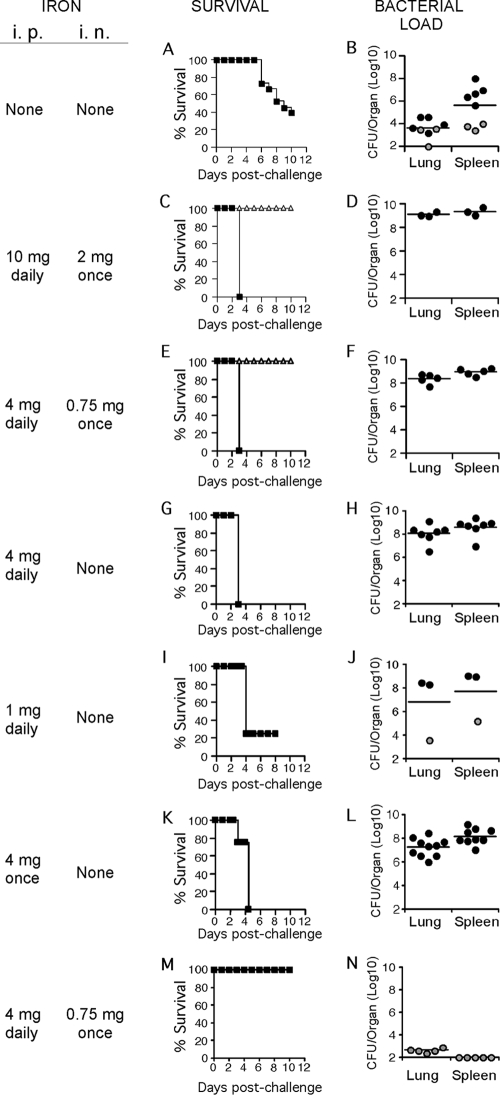
FIG. 1.
Survival and bacterial loads in organs of iron-treated mice infected i.n. with Y. pestis. Groups of mice underwent different regimens of iron supplementation by receiving iron dextran i.n. and/or i.p. as indicated. Mice were challenged i.n. with 1 × 105 CFU Y. pestis strain KIM5 (A to L) or KIM6 (M and N). Survival was assessed by monitoring the mice twice daily for 10 days (A, C, E, G, I, K, and M). Bacterial loads in the lungs and spleen (B, D, F, H, J, L, and N) were quantified by CFU counts from tissue homogenates (euthanized mice with terminal symptoms) (filled circles) or at the end of the experiment (shaded circles). Open triangles in panels C and E represent the survival curves of mice receiving iron dextran but no bacteria. The solid lines represent corresponding geometric means. Data were from three independent experiments, each of them with 5 mice (A and B); from one experiment with 5 mice per group (C and D, E and F, I and J, M and N); from two independent experiments, each of them with 5 mice (G and H); or from one experiment with 10 mice (K and L). The survival curve in panel A was significantly different from those in panels C, E, G, or K (P < 0.001 by the log rank test). Bacterial loads in the lungs were significantly different from those in the spleen in panel B (P < 0.005). Bacterial loads in both the lungs and the spleen were significantly different for panel B versus panel L (P < 0.001).
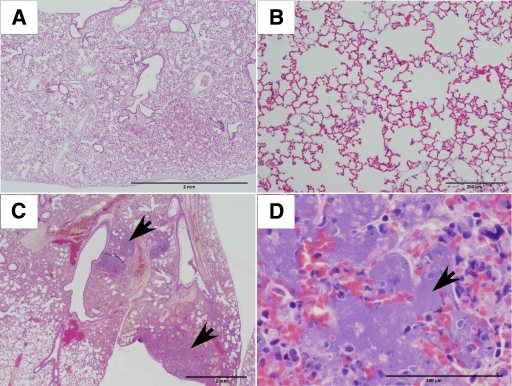
FIG. 2.
Lung histopathology of mice infected i.n. with Y. pestis strain KIM5. Mice received either no iron dextran (A and B) or 10 mg iron dextran i.p. 2 to 3 h before infection and daily thereafter, with an additional dose of 2 mg i.n. 3 h p.i. (C and D). Mice were challenged with 105 CFU of strain KIM5. (A and B) Representative lungs of mice that died or were euthanized moribund at day 6 to 9 (see Fig. 1A) or that were euthanized after 10 symptomless days p.i. (C and D) Representative lungs of mice that succumbed to the infection 2.5 days p.i. were fixed with 0.4% formaldehyde, and sections were stained with H&E. Arrows indicate masses of bacteria. Bars, 2 mm (A and C), 200 μm (B), and 300 μm (D).
Iron dextran suppresses the attenuated phenotype of Y. pestis pgm strain KIM5 in murine lungs.
Iron is rapidly eliminated or rendered unavailable in hosts injected with inorganic iron, and the profound toxicity of inorganic ferric iron unmixed with carbohydrates precludes its administration at high doses (16). Thus, we decided to test iron dextran, which is significantly less toxic and is available for a longer period in the circulation (16, 34). When the i.n. challenge with strain KIM5 (1 × 105 CFU) was accompanied by daily administration of 10 mg iron dextran i.p. together with one i.n. delivery of 2 mg iron dextran 2 to 3 h postinfection, general disease symptoms such as weight loss and lethargy typically appeared in 2 days, followed by a 100% lethal outcome at 72 h (Fig. 1C), with high bacterial counts in both lungs and spleens (Fig. 1D). At the time of death or just before death, in contrast to the lungs of infected but untreated mice (Fig. 2A and B), the lungs of iron dextran-treated mice showed large focal aggregates of bacteria with a multifocal neutrophilic and histiocytic infiltrate effacing the alveolar network (Fig. 2C and D). A set of further experiments was undertaken to determine whether lower doses of iron dextran were still able to induce pneumonia in mice infected i.n. with strain KIM5. Comparable lethal effects (Fig. 1C, E, and G) and essentially corresponding high bacterial counts were obtained with daily administration of 10 mg or 4 mg iron dextran by the i.p. route, with or without additional i.n. administrations of iron dextran 2 to 3 h before infection (Fig. 1D, F, and H). In mice receiving 4 mg iron dextran daily, lungs were affected by multifocal inflammatory foci that were characterized by complete effacement of the parenchyma via numerous neutrophils and necrosuppurative lesions with karyorrhexis (Fig. 3 A and B). Spleens were affected by red pulp necrosis with lymphocyte loss and mesothelial hypertrophy (not shown). When the amount of iron dextran was decreased to a daily i.p. application of 1 mg, bacterial counts in the lungs and spleens of affected mice (Fig. 1J) were almost as high as those observed when larger iron doses were administered. However, the fatality rates decreased, dropping to 75% (Fig. 1I). In contrast, a single injection of 4 mg iron dextran i.p. given on the same day as the bacterial challenge caused 100% death after 4.5 days (Fig. 1K). Moreover, the bacterial counts in the lungs and spleens were well over 1,000 times higher than those found in the organs of mice that received no iron, reaching 107 to 108 CFU per organ (Fig. 1L). Histology of the lungs delineated clear inflammatory foci composed mainly of neutrophils and proteinaceous fluid (Fig. 3C and D), contrasting with the total absence of such lesions in mice administered only iron dextran (Fig. 3E and F). To quantitatively evaluate how the different iron dextran treatments affected the pulmonary histopathology of the infected mice, pathological scores reflecting the numbers and extents of focal inflammatory lesions were recorded as described in Materials and Methods. Infected mice given 4 mg iron dextran daily showed scores significantly different from those of mice given the same treatment only once (P, <0.019), and infected mice treated only once with iron dextran showed significantly higher scores than infected but untreated mice (P, <0.034) (Fig. 3G). This result indicated that the severity of pneumonia was modulated by the iron dextran dosage; a single or a daily dose of 4 mg led to light or severe pneumonia, respectively. As an additional negative control, iron dextran-treated mice (4 mg i.p. daily and 0.75 mg once i.n.) were challenged i.n. with strain KIM6, which lacks the virulence plasmid pCD1. All the mice survived (Fig. 1M), and the CFU counts were negligible 10 days after infection (Fig. 1N), confirming that iron dextran by itself had no significant deleterious effect on mice and that the iron dextran-promoted virulence detected was specific for pgm strain KIM5.
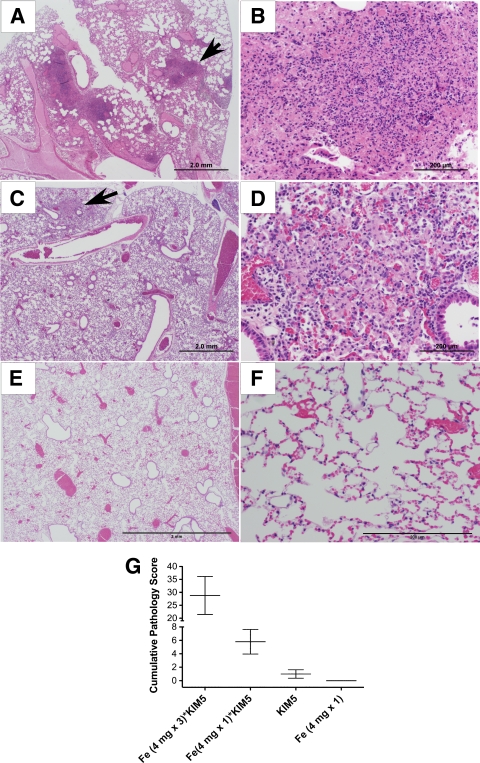
FIG. 3.
Lung histopathology of iron dextran-treated mice infected i.n. with Y. pestis strain KIM5. Mice received 4 mg iron dextran i.p. either daily (A and B) or once (C, D, E, and F) and either were infected i.n. with 105 CFU of strain KIM5 (A to D) or received PBS i.n. (negative control) (E and F). Lungs of mice that either succumbed to the infection 2.5 to 4 days p.i. (A to D) or were euthanized 9 days p.i. (E and F) were fixed with 0.4% formaldehyde, and sections were stained with H&E. Arrows in the left panels indicate the areas shown on the right panels for the same row. Bars, 2 mm (A, C and E) or 200 μm (B, D, and F). None of the iron dextran-treated uninfected mice showed any lesions (E and F). (G) Lung pathology scores showed significant differences between the infected mice that were treated daily and those treated once with iron dextran (P < 0.019), and the infected mice treated only once with iron dextran showed significantly higher scores than the infected but untreated mice (see Fig. 2A and B) (P < 0.034).
Taken together, our data showed that the pathology of pneumonic plague could be recapitulated with strain KIM5 by pretreating the mice with iron dextran. Most importantly, the lesions observed compared well with those described previously for pneumonic plague induced by wild-type strains (3, 25, 32). Since a higher dose of iron dextran increased the severity of the infectious process, it was not surprising that it also decreased the LD50. With the least aggressive iron dextran treatment that still induced distinctively pneumonic plague, namely, 4 mg i.p. once, the LD50 of KIM5 was determined to be 760 CFU. In contrast, the LD50 of KIM5 was determined to be 31 CFU with the daily administrations of 4 mg iron dextran i.p., which induced more-extensive pneumonic lesions. These values compared well with literature data showing an LD50 of 330 CFU for strain KIM given i.n. to BALB/c mice (19, 69), or 40 to 1200 CFU for strain CO92 administered i.n. to C57BL/6 mice (9, 30, 32).
In vivo expression and antigenicity of F1 and Psa.
Having shown that strain KIM5 can induce primary pneumonia in iron dextran-treated C57BL/6 mice, we determined whether this infection model would be useful for protection studies with experimental vaccines. The currently best studied experimental vaccine against pneumonic plague consists of the F1 and LcrV antigens, each of which by itself has protective properties against virulent wild-type strains of Y. pestis, such as strains KIM and CO92 (60). Thus, to further validate the pneumonic plague model with iron dextran-treated mice and strain KIM5, it was essential to demonstrate F1 antigen expression in this model. The immunogenicity and protective properties of F1 can be attributed to its efficient in vivo expression as a homopolymeric surface protein. Since, like F1, the Psa fimbria of Y. pestis is also exported as a homopolymer by a chaperone-usher apparatus, Psa fimbrial protein was investigated in parallel with the F1 antigen. Strain KIM5 was shown by immunohistochemistry to express both the F1 and Psa antigens in the spleens of infected mice, irrespective of iron dextran administration (Fig. 4 A, B, D, E, and G [negative control]). The two antigens were also detected in the lungs and bronchial lymph nodes, though only for iron dextran-treated mice (Fig. 4C, F, H, and I); bacterial numbers were probably too low for visualization in the lungs of untreated mice (not shown). Bacterial expression of F1 and Psa in the lungs was independent of the iron dextran dosage studied (4 mg once or daily). Having demonstrated in vivo expression of F1 and Psa, we next aimed to investigate the immunogenicity of these two antigens. For this purpose, C57BL/6 mice (n = 5) were immunized with two doses of 40 μg recombinant antigen in Alhydrogel. Since our recombinant E. coli expressing Psa from plasmid pCS267 (37) released large amounts of the Psa antigen into the medium, we isolated and tested both released and bacteria-associated antigens. Although the latter Psa antigen gave slightly better titers (one 2-fold dilution), each antigen (F1 and the two Psa protein preparations) induced a strong humoral immune response (geometric mean IgG titer, >105, as determined by ELISA 2 weeks after the last immunization). Taken together, the data showed that F1 and Psa are expressed in vivo, particularly in affected lungs of iron dextran-treated mice, and that the Psa protein is as immunogenic as the F1 antigen. In addition the results were consistent with human data, which strongly suggested that the Psa protein induces strong immune responses, since the invading Y. pestis elicited anti-Psa antibodies in plague patients (35).
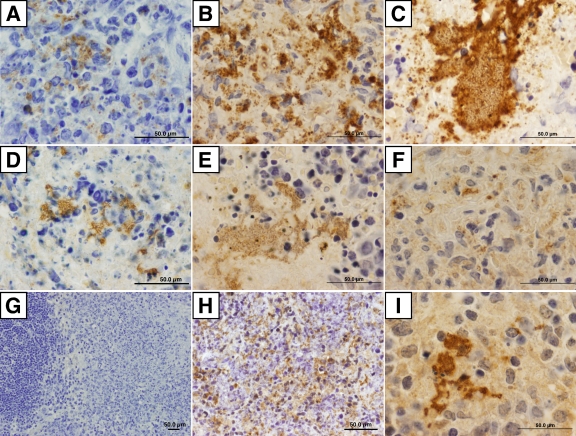
FIG. 4.
Y. pestis expression of the F1 antigen or Psa in infected mice. Immunohistochemistry of organs from mice challenged i.n. with 105 Y. pestis KIM5 bacteria was performed. Murine tissues were stained with hematoxylin (blue). Bacteria expressing the F1 antigen (in brown) were detected with specific antisera in the spleens of mice that received no iron (A) or 4 mg iron once (B), as well as in the lungs of the latter mice (C). Bacterial numbers in the lungs of the former mice were too low for detection (see Fig. 1B). Similarly, bacteria expressing Psa were detected in the spleens of mice that received no iron (D) or 4 mg iron once (E), as well as in the lungs (F) and bronchial lymph nodes (H) of the latter mice, but not in the lungs of the former mice (not shown). Bacteria expressing Psa were also detected in the lungs of mice treated daily with 4 mg iron dextran (I). No bacteria were visualized in tissues stained with nonspecific antibodies (G). Organs were from day 2.5 (I), 4 (B, C, E, F, and H), or 5 (A, D, and G) p.i. Bars, 50 μm.
Iron dextran-treated KIM5-infected mice: a pneumonic plague model for antigen protection assays.
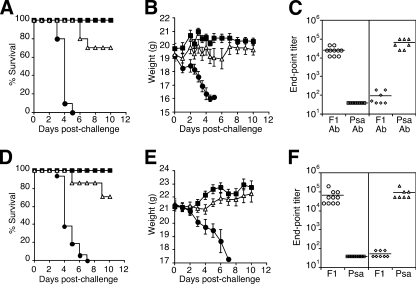
Having shown that an iron dextran-treated mouse model could be used to mimic pneumonic plague with strain KIM5, we determined whether the known protective antigen F1 demonstrates protection with this model. Psa was also investigated with this model, since it was expressed in vivo, was a strong immunogen, and appeared to have protective properties in a preliminary study. The latter study had tested the protective properties of Psa with mice that were not treated with iron. Three groups of 10 C57BL/6 mice had been immunized s.c. with the F1 antigen, Psa, or the E. coli 987P fimbriae as a negative control (40 μg of purified antigen injected on days 0 and 21). On day 35 postimmunization, non-iron-treated mice were challenged i.n. with 6.6 × 106 CFU of strain KIM5. As expected, immunization with F1 provided 100% protection. Interestingly, all the Psa-immunized mice were also protected, while 60% of control mice immunized with the unrelated fimbrial protein 987P died (P, 0.0042 for comparison of the F1 or Psa against the 987P data). Consistent with these observations, Psa- and F1-immunized mice did not show any significant decrease in weight, whereas all the mice immunized with 987P fimbriae lost weight (P, <0.001 for comparison of the F1 or Psa against the 987P data), and those that survived began to recover at day 7 postinfection (data not shown). Although the data for the control mice indicated that the challenge dose was barely above 1 LD50, the result for the Psa antigen warranted its further inclusion in protection experiments with iron dextran-treated mice. For this purpose, an experiment was carried out with C57BL/6 mice (n = 10) immunized with two doses of 40 μg of recombinant F1 antigen or Psa isolated from bacterial surfaces, mixed with the adjuvant Alhydrogel. Two challenge doses were studied by infecting iron dextran-treated mice (one dose of 4.0 mg i.p.) i.n. with 210 or 21 LD50s of Y. pestis KIM5. As expected, all the control mice that were immunized with the adjuvant alone died 3 to 5 days after immunization (MST, 4 days) with 210 LD50s (Fig. 5A). In contrast, 100% of the F1 antigen-immunized mice and 70% of the Psa-immunized mice survived the bacterial challenge with 210 LD50s (P, < 0.0001 for comparison of the F1 or Psa against the adjuvant-alone data; P, >0.05 for comparison of the F1 against the Psa data), and all the deaths in the Psa-immunized group occurred between days 6 and 7. No significant weight variations were observed for the F1- or the Psa-immunized mice that survived (Fig. 5B). All the control mice gradually lost weight after the second day postinfection, whereas the Psa-immunized mice that became sick began to lose weight only after day 3 to 4 postinfection. In these experiments, the F1 antigen, as well as Psa, induced high immunogen-specific antibody titers in mice, with endpoint titers of 10,000 to 100,000 (Fig. 5C). Comparable results were obtained for mice infected with 21 LD50s, with 100% of F1-immunized mice and 80% of Psa-immunized mice surviving the challenge (P, < 0.002) (data not shown).
FIG. 5.
Challenge of F1 antigen- or Psa-immunized mice. Groups of 7 to 10 mice were immunized s.c. with Alhydrogel (A, B, and C) or Freund's adjuvant (D, E, and F) either alone (filled circles) or together with the F1 antigen (filled squares) or Psa (open triangles). Mice received either one boost immunization at a 3-week interval (A, B, and C) or two boost immunizations at 3- and 2-week intervals (D, E, and F). Two weeks following the last boost immunization, mice were administered 4 mg iron dextran i.p. 2 to 3 h before challenge with 210 LD50s (A, B, and C) or 17 LD50s (D, E, and F) of Y. pestis KIM5 by i.n. instillation. The second group of mice received additional administrations of 4 mg iron dextran i.p. at days 2 and 3. Survival (A and D) and weight (B and E) were monitored for 10 days. F1-specific and Psa-specific antibodies were measured by ELISAs in sera from F1-immunized mice (C and F, left panels), and from Psa-immunized mice (C and F, right panels).
To test the iron dextran-treated mouse model more stringently, additional experiments were undertaken with F1 antigen- or Psa-immunized mice by administering the iron dextran regimen (4 mg daily) shown to induce severe and extensive pneumonia in KIM5-infected mice. Moreover, since Psa did not protect as well as the F1 antigen in the earlier experiment, and in order to evaluate the potential protective properties of Psa with a more powerful adjuvant, the new experiments were undertaken with Freund's adjuvant. Ten C57BL/6 mice were immunized with 40 μg antigen in FCA, with two boosts of the same dose in FIA, at 2- to 3-week intervals. In a first experiment, the immunized and iron dextran-treated mice were challenged i.n. with 17 LD50s of Y. pestis KIM5. All the control mice immunized with the adjuvant alone died 3 to 7 days p.i. (MST. 4 days) (Fig. 5D). In contrast, 100% of the F1 antigen-immunized mice and 70% of the Psa-immunized mice survived this bacterial challenge (P, < 0.0001 for comparison of the F1 or Psa data against the adjuvant-alone data; P, >0.05 for comparison of the F1 against the Psa data). In the Psa-vaccinated group, all the deaths occurred between days 5 and 9. No significant weight variations were observed for the F1 antigen-immunized mice (Fig. 5E). All the control mice gradually lost weight after the second day p. i., whereas the Psa-immunized mice started to gain weight by day 5 after an initial weight loss on days 3 and 4 p.i. In these experiments, the F1 antigen as well as Psa induced high immunogen-specific antibody titers in mice, with endpoint titers of 10,000 to 100,000 (Fig. 5F). In contrast to the significant but partial protection of the Psa-immunized mice in this experiment, Psa was not protective when the bacterial challenge dose was increased to 170 LD50s. Although all the F1 antigen-immunized mice survived, all the Psa-immunized mice died, as did the control (adjuvant-alone) mice. However, the survival data were significantly different for the latter two groups (P, 0.028), with survival times of 4 to 9 (MST, 5 days) and 3 to 6 (MST, 3 days) days p.i. for the Psa-immunized mice and the control mice, respectively. In summary, these results indicated that the F1 antigen is similarly protective against pneumonic plague whether a wild-type strain is used to challenge mice, as described in the literature (4, 58, 60), or whether iron dextran-treated mice are challenged with strain KIM5. Moreover, the data suggested that Psa has some protective properties for mice affected by pneumonic plague, although they are less impressive than those of the F1 antigen, since significant protective effects against severe pneumonia were detected only when the i.n. bacterial challenge was not in excess of 17 LD50s.
DISCUSSION
Various experimental animals have been used to model human pneumonic plague. Most studies in the literature have focused on the murine model, particularly the more recent investigations, which have began to unravel the contributions of cellular immune components to the benefit of vaccine development (60, 61). Although early live vaccines and several promising new mutants have been shown to deliver protective properties, they still have poor or unknown safety records (1, 38, 41, 46, 47, 63, 65). By definition, an ideal vaccine should be not only 100% protective but also 100% safe. Thus, a killed vaccine or a multisubunit vaccine that affords full protection is the most desirable vaccine. Because killed vaccines have proven insufficient in providing protection against pneumonic plague (41, 60), most research to date has focused on the experimental F1 and LcrV subunit vaccine, which protects mice against bubonic and pneumonic plague (58). Although protection proved insufficient in an analogous primate model (1, 55, 60), this vaccine appears to be safe and immunogenic in humans (74). However, the ability of F1-deficient strains of Y. pestis to cause pneumonic plague in mice and primates, and the consequent reliance on just one immunogen for protection, highlights the need to identify additional protective subunits (1, 40, 45, 60). A variety of protein subunits, such as the YpkA (5), YopD (5), YscC (24), YscF (40, 64), and YadC (45) proteins of Y. pestis, have been shown to possess some protective properties. Unfortunately, the experimental protocols used to detect protection are so varied that a comparative evaluation of the different immunogens is not possible. A major hurdle for the identification and characterization of new protective immunogens is the need to undertake challenge experiments with wild-type strains of Y. pestis and thus to use BSL-3 conditions. Here we tested the possibility of using strain KIM5 in a new BSL-2 model of pneumonic plague. Strain KIM5 lacks the pgm locus, which encodes, among others, an essential virulence factor for nonintravenous plague infections, namely, the yersiniabactin-dependent iron transport system (52). Disease progression induced by Y. pestis pgm strains, such as strain KIM5, does not recapitulate that observed with fully virulent strains (19, 33, 44). As recently reported by others, we were unable to infect mice successfully by administering KIM5 by the i.n. route; the bacteria multiplied poorly in the lungs, which showed no significant histopathology. Early studies indicated that iron injections given to mice could suppress pgm attenuation in Y. pestis (10). However, a detailed recent study based on the administration of iron chloride to mice demonstrated the absence of pneumonic lesions after i.n. challenge with strain KIM D27 (33). Although we observed similar results with iron sulfate, we were able to recapitulate pneumonic plague following i.n. infection with strain KIM5 in iron dextran-treated mice. Survival curves and strain KIM5 multiplication in the lungs were similar to those described elsewhere for wild-type strains (3, 32). Moreover, the F1 antigen was clearly detectable in the lungs and spleens of KIM5-infected mice.
Interestingly, Fetherston et al. have recently shown that the i.n. LD50 of Y. pestis irp2 (irp2 being a yersiniabactin biosynthetic gene) was ∼670 times higher than that of the wild-type strain, whereas the i.n. LD50 of Y. pestis pgm was ∼12,000 times higher than that of the wild-type strain (19). This >15-fold-increased lethality highlighted the presence of at least one other virulence factor in the pgm locus; the yersiniabactin locus occupies only a portion of it. An obvious candidate virulence factor could be the ripA gene (57), although Bliska and Perry reported that a ΔripABC mutant was fully virulent in mice (cited in reference 19). Even though several other genes of the pgm locus have been proposed to be involved in this increased virulence of pneumonic plague, the effect of such genes on LD50s was significantly less impressive than the effect of irp2 (19). Thus, the yersiniabactin locus has to be considered the major player in the virulence attributed to the pgm locus, in support of our use of iron dextran to bypass pgm attenuation. Moreover, in contrast to the i.n. LD50 of strain KIM5 (>3.9 × 106 CFU), the LD50s of strain KIM5 with the iron dextran-treated mouse model of pneumonic plague (30 to 760 CFU) and the parental wild-type strain KIM with untreated mice (330 CFU) were essentially in the same range (19, 69), strongly suggesting that the predicted additional pgm virulence factor did not significantly influence the parameters for pneumonic plague tested here. Nevertheless, a potential caveat for iron-treated mouse models is that iron can influence the host's innate immune responses, for example, by allowing virulent bacteria to multiply better in iron-rich phagocytes (22, 42, 70). Also, administration of iron renders mice more susceptible to human pathogens, a method that has been used to develop a variety of infectious-disease models (62, 71, 75). Thus, the KIM5-iron dextran model of pneumonic plague might be considered too stringent if it were used to study the protective properties of potential vaccines or the effects of attenuation with mutants of potential virulence factors. For this reason, the model was further tested in protection assays with the F1 immunogen, a Y. pestis immunogen known to protect against i.n. infections with wild-type strains. F1-immunized mice were fully protected in our model, consistent with the protective property of this antigen for murine pneumonic plague (4) and further supporting the use of the iron dextran-treated mouse model of primary pneumonic plague with strain KIM5. This simple, safe, and cost-reducing BSL-2 model of infection should be valuable for exploratory investigations aimed at identifying the few bacterial antigens or virulence factors that should be further characterized in infection models with fully virulent wild-type strains that require BSL-3 facilities.
Y. pestis Psa fimbriae were previously found by us and others to bind to respiratory tract epithelial cells and interact with macrophages (31, 37). Although the results of previous studies indirectly suggested that the Psa fimbriae are expressed in vivo (7, 13, 14, 35, 36), definitive evidence was lacking. In this study we have conclusively demonstrated by immunohistochemistry that the Psa antigen is produced in tissues of Y. pestis-infected mice. Psa harbors a major desirable property of a protective immunogen for vaccine design in that it is conserved in all currently sequenced Y. pestis strains. We showed here that, consistent with human data (35), Psa is immunogenic in mice and has significant protective properties in the iron dextran-treated mouse model of pneumonic plague, although they are less dramatic than those of F1. Our results contrasted with a reference to unpublished data (cited in reference 66) and a recent study that did not detect Psa-mediated protection (7). However, a different antigen preparation technique, a lower antigen dose, the absence of an adjuvant, and challenge with a different bacterial strain by another route (s.c.) in the latter study could each explain this discrepancy. Although the results of the current study will have to be confirmed by wild-type strain infection challenges, they provide a sound basis for further evaluation of Psa as a vaccine component.
This study and other studies have now identified several Y. pestis proteins (61) that might serve to complement the current experimental acellular Y. pestis vaccine based on the F1 and LcrV immunogens. A multicomponent vaccine against pneumonic plague could be modeled on the successful acellular Bordetella pertussis cocktail vaccines, all of which include several proteins, and those with three or more components are considered to be more effective than one- or two-component vaccines that contain only pertussis toxin (PT) or both PT and filamentous hemagglutinin (FHA) (27, 56). Thus, it is expected that a cocktail of Y. pestis immunogens will not only elicit an immune response capable of blocking bacterium-host interactions but will also broaden the range of protected individuals. Moreover, a vaccine consisting of multiple Y. pestis immunogens will have the advantage of extending protection against natural mutants and genetically engineered mutants intentionally designed to remain pathogenic.
Acknowledgments
We thank Leonard Bello for reading the manuscript and Melissa Lasaro for technical help. We are also grateful to Jacqueline Ferracone for indirect immunohistochemistry expertise, and we are in debt to Perry L. Habecker for his support.
This work was supported by NIH grant 1R21 AI076695, a University of Pennsylvania Research Foundation grant, and Research Initiative Funds from the University of Pennsylvania Veterinary Center for Infectious Disease.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 24 May 2010.
REFERENCES
- 1.Adamovicz, J. J., and G. P. Andrews. 2005. Plague vaccines: retrospective analysis and future developments, p. 121-153. In L. E. Lindler, F. J. Lebeda, and G. W. Korch (ed.), Biological weapons defense: infectious diseases and counterbioterrorism. Humana Press, Inc., Totowa, NJ.
- 2.Aepfelbacher, M., C. Trasak, and K. Ruckdeschel. 2007. Effector functions of pathogenic Yersinia species. Thromb. Haemost. 98:521-529. [PubMed] [Google Scholar]
- 3.Agar, S. L., J. Sha, S. M. Foltz, T. E. Erova, K. G. Walberg, T. E. Parham, W. B. Baze, G. Suarez, J. W. Peterson, and A. K. Chopra. 2008. Characterization of a mouse model of plague after aerosolization of Yersinia pestis CO92. Microbiology 154:1939-1948. [DOI] [PubMed] [Google Scholar]
- 4.Andrews, G. P., D. G. Heath, G. W. Anderson, Jr., S. L. Welkos, and A. M. Friedlander. 1996. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and from an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect. Immun. 64:2180-2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andrews, G. P., S. T. Strachan, G. E. Benner, A. K. Sample, G. W. Anderson, Jr., J. J. Adamovicz, S. L. Welkos, J. K. Pullen, and A. M. Friedlander. 1999. Protective efficacy of recombinant Yersinia outer proteins against bubonic plague caused by encapsulated and nonencapsulated Yersinia pestis. Infect. Immun. 67:1533-1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angov, E., B. M. Aufiero, A. M. Turgeon, M. Van Handenhove, C. F. Ockenhouse, K. E. Kester, D. S. Walsh, J. S. McBride, M. C. Dubois, J. Cohen, J. D. Haynes, K. H. Eckels, D. G. Heppner, W. R. Ballou, C. L. Diggs, and J. A. Lyon. 2003. Development and pre-clinical analysis of a Plasmodium falciparum Merozoite Surface Protein-142 malaria vaccine. Mol. Biochem. Parasitol. 128:195-204. [DOI] [PubMed] [Google Scholar]
- 7.Anisimov, A. P., I. V. Bakhteeva, E. A. Panfertsev, T. E. Svetoch, T. B. Kravchenko, M. E. Platonov, G. M. Titareva, T. I. Kombarova, S. A. Ivanov, A. V. Rakin, K. K. Amoako, and S. V. Dentovskaya. 2009. The subcutaneous inoculation of pH 6 antigen mutants of Yersinia pestis does not affect virulence and immune response in mice. J. Med. Microbiol. 58:26-36. [DOI] [PubMed] [Google Scholar]
- 8.Bearden, S. W., and R. D. Perry. 2008. Laboratory maintenance and characterization of Yersinia pestis. Curr. Protoc. Microbiol. 11:5B.1.1-5B.1.13. [DOI] [PubMed] [Google Scholar]
- 9.Bubeck, S. S., A. M. Cantwell, and P. H. Dube. 2007. Delayed inflammatory response to primary pneumonic plague occurs in both outbred and inbred mice. Infect. Immun. 75:697-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burrows, T. W., and S. Jackson. 1956. The virulence-enhancing effect of iron on nonpigmented mutants of virulent strains of Pasteurella pestis. Br. J. Exp. Pathol. 37:577-583. [PMC free article] [PubMed] [Google Scholar]
- 11.Butler, T. 2009. Plague into the 21st century. Clin. Infect. Dis. 49:736-742. [DOI] [PubMed] [Google Scholar]
- 12.Casman, E. A., and B. Fischhoff. 2008. Risk communication planning for the aftermath of a plague bioattack. Risk Anal. 28:1327-1342. [DOI] [PubMed] [Google Scholar]
- 13.Cathelyn, J. S., S. D. Crosby, W. W. Lathem, W. E. Goldman, and V. L. Miller. 2006. RovA, a global regulator of Yersinia pestis, specifically required for bubonic plague. Proc. Natl. Acad. Sci. U. S. A. 103:13514-13519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chauvaux, S., M. L. Rosso, L. Frangeul, C. Lacroix, L. Labarre, A. Schiavo, M. Marceau, M. A. Dillies, J. Foulon, J. Y. Coppee, C. Medigue, M. Simonet, and E. Carniel. 2007. Transcriptome analysis of Yersinia pestis in human plasma: an approach for discovering bacterial genes involved in septicaemic plague. Microbiology 153:3112-3124. [DOI] [PubMed] [Google Scholar]
- 15.Cowan, C., A. V. Philipovskiy, C. R. Wulff-Strobel, Z. Ye, and S. C. Straley. 2005. Anti-LcrV antibody inhibits delivery of Yops by Yersinia pestis KIM5 by directly promoting phagocytosis. Infect. Immun. 73:6127-6137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Danielson, B. G. 2004. Structure, chemistry, and pharmacokinetics of intravenous iron agents. J. Am. Soc. Nephrol. 15(Suppl. 2):S93-S98. [DOI] [PubMed] [Google Scholar]
- 17.Denoel, P., F. Godfroid, N. Guiso, H. Hallander, and J. Poolman. 2005. Comparison of acellular pertussis vaccines-induced immunity against infection due to Bordetella pertussis variant isolates in a mouse model. Vaccine 23:5333-5341. [DOI] [PubMed] [Google Scholar]
- 18.Elvin, S. J., and E. D. Williamson. 2004. Stat 4 but not Stat 6 mediated immune mechanisms are essential in protection against plague. Microb. Pathog. 37:177-184. [DOI] [PubMed] [Google Scholar]
- 19.Fetherston, J. D., O. Kirillina, A. G. Bobrov, J. T. Paulley, and R. D. Perry. 2010. The yersiniabactin transport system is critical for the pathogenesis of bubonic and pneumonic plague. Infect. Immun. 78:2045-2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galván, E. M., H. Chen, and D. M. Schifferli. 2007. The Psa fimbriae of Yersinia pestis interact with phosphatidylcholine on alveolar epithelial cells and pulmonary surfactant. Infect. Immun. 75:1272-1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galván, E. M., M. A. Lasaro, and D. M. Schifferli. 2008. Capsular antigen fraction 1 and Pla modulate the susceptibility of Yersinia pestis to pulmonary antimicrobial peptides such as cathelicidin. Infect. Immun. 76:1456-1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gauthier, Y. P., and P. Isoard. 1995. Effect of iron and phagocytosis on murine macrophage activation in vitro. Biol. Trace Elem. Res. 47:37-50. [DOI] [PubMed] [Google Scholar]
- 23.Goguen, J. D., J. Yother, and S. C. Straley. 1984. Genetic analysis of the low calcium response in Yersinia pestis mu d1(Ap lac) insertion mutants. J. Bacteriol. 160:842-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodin, J. L., R. W. Raab, R. L. McKown, G. L. Coffman, B. S. Powell, J. T. Enama, J. A. Ligon, and G. P. Andrews. 2005. Yersinia pestis outer membrane type III secretion protein YscC: expression, purification, characterization, and induction of specific antiserum. Protein Expr. Purif. 40:152-163. [DOI] [PubMed] [Google Scholar]
- 25.Guarner, J., W. J. Shieh, P. W. Greer, J. M. Gabastou, M. Chu, E. Hayes, K. B. Nolte, and S. R. Zaki. 2002. Immunohistochemical detection of Yersinia pestis in formalin-fixed, paraffin-embedded tissue. Am. J. Clin. Pathol. 117:205-209. [DOI] [PubMed] [Google Scholar]
- 26.Heath, C. W., M. B. Strauss, and W. B. Castle. 1932. Quantitative aspects of iron deficiency in hypochromic anemia: the parenteral administration of iron. J. Clin. Invest. 11:1293-1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hellwig, S. M., M. E. Rodriguez, G. A. Berbers, J. G. van de Winkel, and F. R. Mooi. 2003. Crucial role of antibodies to pertactin in Bordetella pertussis immunity. J. Infect. Dis. 188:738-742. [DOI] [PubMed] [Google Scholar]
- 28.Hill, J., J. E. Eyles, S. J. Elvin, G. D. Healey, R. A. Lukaszewski, and R. W. Titball. 2006. Administration of antibody to the lung protects mice against pneumonic plague. Infect. Immun. 74:3068-3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holbein, B. E., K. W. Jericho, and G. C. Likes. 1979. Neisseria meningitidis infection in mice: influence of iron, variations in virulence among strains, and pathology. Infect. Immun. 24:545-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Honko, A. N., N. Sriranganathan, C. J. Lees, and S. B. Mizel. 2006. Flagellin is an effective adjuvant for immunization against lethal respiratory challenge with Yersinia pestis. Infect. Immun. 74:1113-1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang, X. Z., and L. E. Lindler. 2004. The pH 6 antigen is an antiphagocytic factor produced by Yersinia pestis independent of Yersinia outer proteins and capsule antigen. Infect. Immun. 72:7212-7219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lathem, W. W., S. D. Crosby, V. L. Miller, and W. E. Goldman. 2005. Progression of primary pneumonic plague: a mouse model of infection, pathology, and bacterial transcriptional activity. Proc. Natl. Acad. Sci. U. S. A. 102:17786-17791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee-Lewis, H., and D. M. Anderson. 2010. Absence of inflammation and pneumonia during infection with nonpigmented Yersinia pestis reveals a new role for the pgm locus in pathogenesis. Infect. Immun. 78:220-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Legssyer, R., P. Geisser, H. McArdle, R. R. Crichton, and R. J. Ward. 2003. Comparison of injectable iron complexes in their ability to iron load tissues and to induce oxidative stress. Biometals 16:425-433. [DOI] [PubMed] [Google Scholar]
- 35.Li, B., D. Zhou, Z. Wang, Z. Song, H. Wang, M. Li, X. Dong, M. Wu, Z. Guo, and R. Yang. 2008. Antibody profiling in plague patients by protein microarray. Microbes Infect. 10:45-51. [DOI] [PubMed] [Google Scholar]
- 36.Lindler, L. E., M. S. Klempner, and S. C. Straley. 1990. Yersinia pestis pH 6 antigen: genetic, biochemical, and virulence characterization of a protein involved in the pathogenesis of bubonic plague. Infect. Immun. 58:2569-2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu, F., H. Chen, E. M. Galván, M. A. Lasaro, and D. M. Schifferli. 2006. Effects of Psa and F1 on the adhesive and invasive interactions of Yersinia pestis with human respiratory tract epithelial cells. Infect. Immun. 74:5636-5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu, T., S. L. Agar, J. Sha, and A. K. Chopra. 2010. Deletion of Braun lipoprotein gene (lpp) attenuates Yersinia pestis KIM/D27 strain: role of Lpp in modulating host immune response, NF-κB activation and cell death. Microb. Pathog. 48:42-52. [DOI] [PubMed] [Google Scholar]
- 39.Markwell, M. A., S. M. Haas, L. L. Bieber, and N. E. Tolbert. 1978. A modification of the Lowry procedure to simplify protein determination in membrane and lipoprotein samples. Anal. Biochem. 87:206-210. [DOI] [PubMed] [Google Scholar]
- 40.Matson, J. S., K. A. Durick, D. S. Bradley, and M. L. Nilles. 2005. Immunization of mice with YscF provides protection from Yersinia pestis infections. BMC Microbiol. 5:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meyer, K. F., D. C. Cavanaugh, P. J. Bartelloni, and J. D. Marshall, Jr. 1974. Plague immunization. I. Past and present trends. J. Infect. Dis. 129(Suppl.):S13-S18. [DOI] [PubMed] [Google Scholar]
- 42.Moalem, S., E. D. Weinberg, and M. E. Percy. 2004. Hemochromatosis and the enigma of misplaced iron: implications for infectious disease and survival. Biometals 17:135-139. [DOI] [PubMed] [Google Scholar]
- 43.Moon, H. W., and T. O. Bunn. 1993. Vaccines for preventing enterotoxigenic Escherichia coli infections in farm animals. Vaccine 11:200-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morita, H., M. Yamamoto, and A. Wake. 1970. Histopathological changes of mice injected with plague live vaccine strain EV. Jpn. J. Med. Sci. Biol. 23:87-97. [DOI] [PubMed] [Google Scholar]
- 45.Murphy, B. S., C. R. Wulff, B. A. Garvy, and S. C. Straley. 2007. Yersinia pestis YadC: a novel vaccine candidate against plague. Adv. Exp. Med. Biol. 603:400-414. [DOI] [PubMed] [Google Scholar]
- 46.Okan, N. A., P. Mena, J. L. Benach, J. B. Bliska, and A. W. Karzai. 2010. The smpB-ssrA mutant of Yersinia pestis functions as a live attenuated vaccine to protect mice against pulmonary plague infection. Infect. Immun. 78:1284-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oyston, P. C., G. Mellado-Sanchez, M. F. Pasetti, J. P. Nataro, R. W. Titball, and H. S. Atkins. 2010. A Yersinia pestis guaBA mutant is attenuated in virulence and provides protection against plague in a mouse model of infection. Microb. Pathog. 48:191-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pan, N. J., M. J. Brady, J. M. Leong, and J. D. Goguen. 2009. Targeting type III secretion in Yersinia pestis. Antimicrob. Agents Chemother. 53:385-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Panchal, R. G., R. L. Ulrich, D. Lane, M. M. Butler, C. Houseweart, T. Opperman, J. D. Williams, N. P. Peet, D. T. Moir, T. Nguyen, R. Gussio, T. Bowlin, and S. Bavari. 2009. Novel broad-spectrum bis-(imidazolinylindole) derivatives with potent antibacterial activities against antibiotic-resistant strains. Antimicrob. Agents Chemother. 53:4283-4291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parent, M. A., L. B. Wilhelm, L. W. Kummer, F. M. Szaba, I. K. Mullarky, and S. T. Smiley. 2006. Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect. Immun. 74:3381-3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Perry, R. D., and S. W. Bearden. 2008. Isolation and confirmation of Yersinia pestis mutants exempt from select agent regulations. Curr. Protoc. Microbiol. 11:5B.2.1-5B.2.12. [DOI] [PubMed] [Google Scholar]
- 52.Perry, R. D., and J. D. Fetherston. 2004. Iron and heme uptake systems, p. 257-283. In E. Carniel and B. J. Hinnebusch (ed.), Yersinia: molecular and cellular biology. Horizon Bioscience/Caister Academic Press, Wymondham, Norfolk, United Kingdom.
- 53.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pichichero, M. E., and J. R. Casey. 2005. Acellular pertussis vaccines for adolescents. Pediatr. Infect. Dis. J. 24:S117-S126. [DOI] [PubMed] [Google Scholar]
- 55.Pitt, L. 2004. Nonhuman primates as a model for pneumonic plague, p. 222-248. In Public workshop on animal models and correlates of protection for plague vaccines, 13 to 14 October 2004, Gaithersburg, MD. FDA, Silver Spring, MD. http://www.fda.gov/downloads/BiologicsBloodVaccines/NewsEvents/WorkshopsMeetingsConferences/TranscriptsMinutes/UCM054438.pdf.
- 56.Poolman, J. T., and H. O. Hallander. 2007. Acellular pertussis vaccines and the role of pertactin and fimbriae. Expert Rev. Vaccines 6:47-56. [DOI] [PubMed] [Google Scholar]
- 57.Pujol, C., J. P. Grabenstein, R. D. Perry, and J. B. Bliska. 2005. Replication of Yersinia pestis in interferon gamma-activated macrophages requires ripA, a gene encoded in the pigmentation locus. Proc. Natl. Acad. Sci. U. S. A. 102:12909-12914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Quenee, L. E., and O. Schneewind. 2009. Plague vaccines and the molecular basis of immunity against Yersinia pestis. Hum. Vaccin. 5:817-823. [DOI] [PubMed] [Google Scholar]
- 59.Schifferli, D. M., and M. Alrutz. 1994. Permissive linker insertion sites in the outer membrane protein of 987P fimbriae of Escherichia coli. J. Bacteriol. 176:1099-1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smiley, S. T. 2008. Current challenges in the development of vaccines for pneumonic plague. Expert Rev. Vaccines 7:209-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Smiley, S. T. 2008. Immune defense against pneumonic plague. Immunol. Rev. 225:256-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Starks, A. M., T. R. Schoeb, M. L. Tamplin, S. Parveen, T. J. Doyle, P. E. Bomeisl, G. M. Escudero, and P. A. Gulig. 2000. Pathogenesis of infection by clinical and environmental strains of Vibrio vulnificus in iron-dextran-treated mice. Infect. Immun. 68:5785-5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sun, W., K. L. Roland, X. Kuang, C. G. Branger, and R. Curtiss III. 2010. Yersinia pestis with regulated delayed attenuation as a vaccine candidate to induce protective immunity against plague. Infect. Immun. 78:1304-1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Swietnicki, W., B. S. Powell, and J. Goodin. 2005. Yersinia pestis Yop secretion protein F: purification, characterization, and protective efficacy against bubonic plague. Protein Expr. Purif. 42:166-172. [DOI] [PubMed] [Google Scholar]
- 65.Tidhar, A., Y. Flashner, S. Cohen, Y. Levi, A. Zauberman, D. Gur, M. Aftalion, E. Elhanany, A. Zvi, A. Shafferman, and E. Mamroud. 2009. The NlpD lipoprotein is a novel Yersinia pestis virulence factor essential for the development of plague. PLoS One 4:e7023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Titball, R. W., and E. D. Williamson. 2001. Vaccination against bubonic and pneumonic plague. Vaccine 19:4175-4184. [DOI] [PubMed] [Google Scholar]
- 67.Viboud, G. I., and J. B. Bliska. 2005. Yersinia outer proteins: role in modulation of host cell signalling responses and pathogenesis. Annu. Rev. Microbiol. 59:69-89. [DOI] [PubMed] [Google Scholar]
- 68.Wake, A., H. Morita, and M. Yamamoto. 1972. The effect of an iron drug on host response to experimental plague infection. Jpn. J. Med. Sci. Biol. 25:75-84. [DOI] [PubMed] [Google Scholar]
- 69.Wang, S., S. Joshi, I. Mboudjeka, F. Liu, T. Ling, J. D. Goguen, and S. Lu. 2008. Relative immunogenicity and protection potential of candidate Yersinia pestis antigens against lethal mucosal plague challenge in Balb/C mice. Vaccine 26:1664-1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Weinberg, E. D. 2009. Iron availability and infection. Biochim. Biophys. Acta 1790:600-605. [DOI] [PubMed] [Google Scholar]
- 71.Weinberg, E. D. 2000. Microbial pathogens with impaired ability to acquire host iron. Biometals 13:85-89. [DOI] [PubMed] [Google Scholar]
- 72.Welch, T. J., W. F. Fricke, P. F. McDermott, D. G. White, M. L. Rosso, D. A. Rasko, M. K. Mammel, M. Eppinger, M. J. Rosovitz, D. Wagner, L. Rahalison, J. E. Leclerc, J. M. Hinshaw, L. E. Lindler, T. A. Cebula, E. Carniel, and J. Ravel. 2007. Multiple antimicrobial resistance in plague: an emerging public health risk. PLoS One 2:e309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Welkos, S., and A. O'Brien. 1994. Determination of median lethal and infectious doses in animal model systems. Methods Enzymol. 235:29-39. [DOI] [PubMed] [Google Scholar]
- 74.Williamson, E. D., H. C. Flick-Smith, C. Lebutt, C. A. Rowland, S. M. Jones, E. L. Waters, R. J. Gwyther, J. Miller, P. J. Packer, and M. Irving. 2005. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect. Immun. 73:3598-3608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yi, K., D. S. Stephens, and I. Stojiljkovic. 2003. Development and evaluation of an improved mouse model of meningococcal colonization. Infect. Immun. 71:1849-1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zavialov, A., G. Zav'yalova, T. Korpela, and V. Zav'yalov. 2007. FGL chaperone-assembled fimbrial polyadhesins: anti-immune armament of Gram-negative bacterial pathogens. FEMS Microbiol. Rev. 31:478-514. [DOI] [PubMed] [Google Scholar]