Abstract
Viral vectors based on influenza virus, rabies virus (RV), and vaccinia virus (VV) were used to express large polypeptide segments derived from the Bacillus anthracis protective antigen (PA). For the infectious influenza virus vector and recombinant VV constructs, the receptor binding domain (RBD or domain 4) or the lethal and edema factor binding domain (LEF or domain 1′) were engineered into functional chimeric hemagglutinin (HA) glycoproteins. In the case of the RV vector, the viral glycoprotein (G) was used as a carrier for RBD in an inactivated form of the vector. These constructs were examined by using multiple homologous and heterologous prime/boost immunization regimens in order to optimize the induction of α-PA antibody responses. Several immunization combinations were shown to induce high titers of antibody recognizing the anthrax RBD and LEF domains, as well as the full-length PA protein in mice. The heterologous prime/boost immunization regimens that involved an initial intranasal administration of a live influenza virus vector, followed by an intramuscular boost with either the killed RV vector or the VV vector, were particularly effective, inducing antigen-specific antibodies at levels severalfold higher than homologous or alternative heterologous protocols. Furthermore, sera from several groups of the immunized mice demonstrated neutralization activity in an in vitro anthrax toxin neutralization assay. In some cases, such toxin-neutralizing activity was notably high, indicating that the mechanisms by which immunity is primed by live influenza virus vectors may have beneficial properties.
Influenza virus has a number of properties that make it worthy of consideration for use as a viral vector for pathogens that have proven problematic with regard to vaccine development. In addition to the fact that influenza vaccines have an extensive history of safety in the human population and have well-established protocols for large-scale production of both live and inactivated forms, influenza vaccines have been shown to elicit strong mucosal and systemic responses as early as 2 to 6 days postvaccination that encompass both the humoral and the cellular branches of the immune system (4, 7). The majority of neutralizing antibodies generated by influenza vaccines recognize the hemagglutinin (HA) glycoprotein on the viral surface, which has also been reported to have adjuvant-like effects when coadministered with viruslike particles (7, 19).
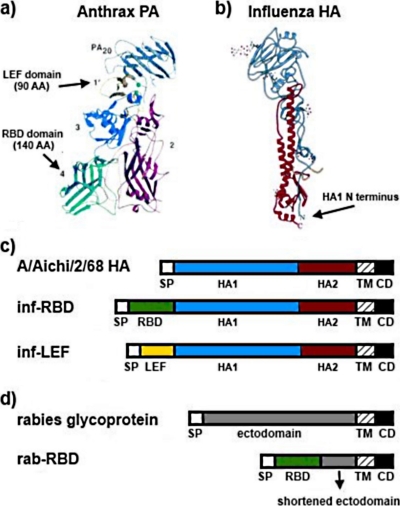
We recently reported that the large segments of foreign antigens can be incorporated as inserts into the HA protein without deleterious effects on HA functions. Specifically, we evaluated chimeric HA proteins containing domains from the protective antigen (PA) of Bacillus anthracis, the causative agent of anthrax (17). The PA protein is one of three protein components that constitute the anthrax toxin, the others being the lethal factor (LF) and the edema factor (EF). PA consists of 735 amino acids that fold into four structurally distinct domains (Fig. 1 a) (25). Neutralizing antibodies have been shown to specifically target domains 1 and 4 of the PA (8, 33). Domain 1 consists of amino acid residues 1 to 258, the first 167 of which are removed following cleavage by the protease furin after the binding of PA to the host cell receptor (25). The remaining residues constitute domain 1′, which is responsible for binding the LF and EF components and is therefore referred to as the LF and EF binding domain, or LEF (36). Domain 4 consists of 140 amino acids and is designated as the receptor binding domain (RBD), since it contains the determinants for binding to the host cell receptors, tumor endothelial marker 8 (TEM8) and capillary morphogenesis protein 2 (CMG2) (6, 22, 25, 27). Previous work demonstrated that chimeric HA proteins expressing the RBD or LEF domains were able to express on cell surfaces in native oligomeric form and maintain HA functions required for host cell entry. In addition, the recombinant influenza viruses containing the chimeric HA/PA proteins were able to replicate to titers similar to those of wild-type viruses and the inserts remained genetically stable over multiple rounds of virus replication. Furthermore, mice immunized with a single intranasal (i.n.) inoculum of the recombinant chimeric viruses were shown to generate high antibody titers specific for the inserted PA fragments.
FIG. 1.
Bacillus anthracis PA and vector constructs. (a) PA structure showing the location and size of the LEF and RBD domains (25). The LEF domain is indicated in yellow, and the RBD is indicated in green. (b) Structural depiction of the influenza virus HA indicating the insertion site of the PA domains. The HA1 subunit is in blue, and the HA2 is in red. (c) Schematic diagram depicting the wild-type HA from A/Aichi/2/68, as well as the organization of the constructs, with respect to location of the PA domains in the primary amino acid sequence. The colors of these domains are coordinated with the structure figures in panels a and b. (d) Schematic diagram depicting the wild-type RV glycoprotein and the organization of the RBD domain in the truncated RV G protein. For a more detailed description refer to the study by Smith et al. (30). inf, influenza virus; SP, signal peptide; TM, transmembrane domain; CD, cytoplasmic domain; rab, RV.
Similar studies were carried out utilizing a rabies virus (RV) vector, in which the RV glycoprotein was engineered to express the RBD domain (domain 4) from PA (30). These studies showed that G/PA chimeric proteins were able to incorporate into virus particles and that mice immunized with live or inactivated forms of the RV vector mounted antibody responses recognizing the inserted RBD domain. After a single inoculation with the RV vector, the measured humoral responses were similar to those observed in mice immunized with 150 times that amount of recombinant PA alone. The RV G/PA vector was also shown to stimulate a Th2 type response when given at doses of 50 ng or more (30).
Despite the induction of high levels of antibodies specific for PA by both the influenza virus and the RV vectors, we were unable to detect in vitro anthrax toxin neutralization activity in the sera of immunized mice following single administrations of antigen or homologous boost regimens. Therefore, the purpose of the present study was to examine the antibody responses induced by both the influenza virus and RV vectors, as well as a recombinant vaccinia virus (VV) vectors expressing HA/PA chimeric proteins, using alternative prime/boost strategies. Our results show that each vector was capable of inducing specific antibody responses and that a second inoculation with the homologous constructs yielded moderate antibody boosting effects. However, we observed a striking increase in PA-specific antibody titers following heterologous prime/boost approaches when using the influenza virus vector as the primary immunogen. Furthermore, using an in vitro toxin neutralization assay, we found that the immunization protocols involving influenza virus priming and heterologous vector boosting induced particularly high neutralizing antibody titers against the inserted domains. These results suggest that immunization regimens involving a primary immunization with live influenza virus vectors may induce initial immune response pathways that are advantageous for the production of antibodies directed against certain pathogens. Such broadly applicable approaches, and the mechanisms by which they operate, may warrant consideration for the design of novel vaccination strategies.
MATERIALS AND METHODS
Construction of plasmids and viral vectors.
The plasmids used for constructing the viral vectors utilized in the present study, as well as the generation and growth of these viral vectors, has been described previously (20, 30). Briefly, for the chimeric LEF/HA and RBD/HA constructs, the HA gene from the H3 subtype influenza virus A strain A/Aichi/2/68 was used as the backbone, and the B. anthracis domain 1′ (LEF) and domain 4 (RBD) regions of the PA gene were constructed by single-chain oligonucleotide extension with codons optimized for mammalian usage (13). The chimeric genes were initially cloned into pRB21 to generate recombinant VVs for protein expression and functional studies (3), and these VV vectors were subsequently used for immunization studies as well. Recombinant infectious influenza viruses were generated by using the 17 plasmid system initially described by Neumann et al. (24). For the RV construct, anthrax PA D4 was amplified from pGEM PA63 and cloned into pBS-STS to yield pD4-ΔED (28). The RV ectodomain fragment was ligated into pD4-ΔED, resulting in pD4-E51. The recombinant RV expressing pD4-E51 was digested with BsiWI and NheI, and the D4-51 fragment was ligated to pSPBN, resulting in pSPBN-D4-E51. Recombinant RVs were recovered by using standard methods (9).
Immunizations.
Female BALB/c mice (6 to 8 weeks old) were purchased from Jackson Laboratories. The immunization dosages for each vector were based on optimization for each construct in the mouse system (20, 30). The mice were infected with 105 PFU of the recombinant influenza viruses i.n., 3 × 106 PFU of the recombinant vaccinia viruses intraperitoneally, or 10 μg of inactivated RV virus SPBN-D4-E51 intramuscularly (i.m.) (5 μg in each hind leg). For boosting experiments, the second vector was given 42 days after the priming immunization. For the mixed infections, the total PFU and routes of infection were the same. Influenza viruses for the i.m. immunizations were inactivated by treatment with β-propiolactone (18). The mice were bled via cheek bleed at the times indicated, and the sera were collected after spinning at 13,000 rpm for 10 min in a tabletop centrifuge. The sera were stored at −80 C until use.
ELISA.
Enzyme-linked immunosorbent assays (ELISAs) were performed as described previously (20). Briefly, Nunc MaxiSorp plates (catalog no. 442404) were coated with 2.5 μg per well of recombinant PA, RBD, or LEF (obtained from BEI Resources) or standard amounts of mouse IgG diluted in BSS buffer and kept at 4°C overnight. The following day, serum was added at different concentrations, and the plates were washed three times with phosphate-buffered saline (PBS)-0.2% Tween 20 before horseradish peroxidase-conjugated goat α-mouse IgG was added (Sigma catalog no. A4416). SigmaFast OPD tablets (catalog no. P9187) were used to develop the plates. The reactions were stopped with 0.1 N H2SO4, and the plates were read at 490 nm. Standard curves were constructed from the IgG standards, and antibody concentrations specific for the coating protein were calculated from these.
Toxin neutralization assay.
Toxin neutralization assays were performed as previously described (16). Sera from the different groups of mice were pooled, serially diluted, and preincubated with 250 ng of rPA/ml and 50 ng of LF/ml (final concentrations). After 30 min, these were added to 96-well plates containing J774A.1 macrophage cells for 3 h. Then, 25 μl of a 5-mg/ml concentration of MTT dissolved in PBS was added to the wells for 2 h at 37°C, at which time DMF/sodium dodecyl sulfate (SDS) was added to each well to lyse the cells. The plates were incubated overnight and then read at 570 nm the next day. The concentration of serum that protected 50% of the cells was determined by comparison to wells that did not receive toxin.
RESULTS AND DISCUSSION
Design of chimeric proteins and generation of viral vectors.
The constructs involved in the generation and expression of the chimeric PA proteins analyzed in the present study are outlined in Fig. 1. Figure 1a shows the structure of the PA protein and highlights the individual domains. Based on structural considerations, coding regions for 90 residues corresponding to the LEF domain and 140 residues corresponding to the RBD domain were cloned for insertion into chimeric proteins. These were inserted near the N terminus of the HA protein (Fig. 1b), since it has been shown that this region of the protein is able to accommodate large polypeptide insertions in both H3 and H7 subtype HAs (14, 20). The constructs were designed to express the inserted domains at the N terminus of the HA ectodomain following cleavage of the signal peptide (Fig. 1c). This site was selected because it is believed to best support the folding of the inserted polypeptide domains, as well as the HA backbone, into native structures based on structural observations.
Initially, the HA/RBD and HA/LEF proteins were expressed by using recombinant VVs to verify cell surface expression, folding, and functional properties of the chimeric proteins. These VV recombinants were also used for some of the immunization regimens described below. The same chimeric HA/RBD and HA/LEF proteins were also used to generate infectious recombinant influenza viruses, which were shown to remain genetically stable and replicate to high titers in cell culture or embryonated eggs (20). For the RV vector used in the present study, the RBD domain was inserted into the RV glycoprotein as an N-terminal replacement for most of the ectodomain (Fig. 1d). As mentioned previously, these chimeric proteins have been shown to incorporate efficiently into infectious virions (30).
Immune responses using homologous or heterologous prime/boost regimens.
For the experiments involving influenza virus vectors, mice were inoculated i.n., and for the experiments involving inactivated RV, the mice were inoculated i.m. Groups of six mice were prebled and then inoculated with the influenza virus vector containing the chimeric HA/RBD protein (inf-RBD), the influenza virus vector with the chimeric HA/LEF protein (inf-LEF), a mixture of the two recombinant influenza virus vectors (inf-MIX), the RV containing the RBD domain (rab-RBD), or VVs expressing either HA/LEF (vv-LEF) or a mixture of HA/LEF and HA/RBD (vv-MIX). Mice were bled at days 28 and 42 and then boosted on day 42 with either the homologous vector or a heterologous vector. After the boost on day 42, blood was taken weekly up to day 77 (35 days postboost).
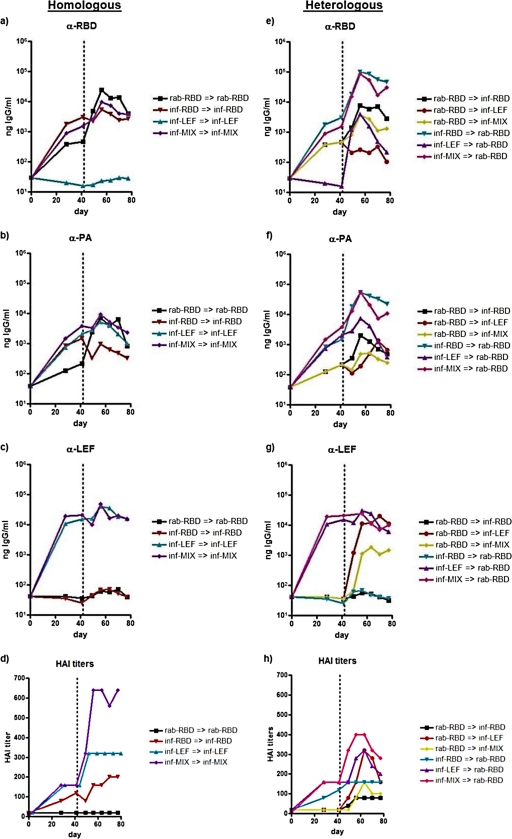
Sera from immunized mice were analyzed by ELISA to evaluate IgG reactivity to purified His-tagged LEF domain recombinant protein, His-tagged RBD domain recombinant protein, or complete recombinant PA protein. The data for these are shown in Fig. 2 and 3. Specifically, Fig. 2 shows the data for the influenza virus and RV prime/boost experiments. The data for reactivity to each antigen are displayed on separate graphs for homologous (Fig. 2a to c) or heterologous (Fig. 2e to g) boost experiments to allow data points to be more easily distinguished. The data in Fig. 2a show that the antibody titers against the RBD domain following the homologous prime/boost regimens were specific, since there is no titer observed for the mice inoculated with the LEF constructs. The immunizations with inf-RBD alone or a mixture of inf-RBD and inf-LEF gave similar results and provided for the higher initial antibody responses than the rab-RBD vector, as measured on days 28 and 42 after inoculation. However, the boost effect was greatest for mice primed with inf-RBD or inf-MIX and boosted by i.m. inoculation with the RV vectors, which resulted in titers of ∼104 ng of IgG/ml in sera following the boost. The reason for the rather moderate boost effect observed with the homologous influenza virus vector regimen is not known but may result from immunity to the influenza virus generated during the priming phase leading to the inhibition of replication with this live virus vector during the boosting phase.
FIG. 2.
Antibody responses following immunization with viral vectors. ELISA titers determined using purified recombinant PA, His-tagged RBD, or LEF proteins as the antigen. (a to c) α-RBD (a), α-PA (b), or α-LEF (c) antibody titers in mice before and after boosting on day 42 with homologous vectors. (e to g) α-RBD (e), α-PA (f), or α-LEF (g) antibody titers in mice before and after boosting on day 42 with heterologous vectors. The HAI titers against H3N1 subtype virus before and after homologous (d) or heterologous (h) boosting are also shown.
As shown in Fig. 2b, all vectors were capable of inducing antibodies against purified recombinant PA protein. The results following homologous prime/boost regimens again show that the influenza virus vectors provided for higher initial responses, but the homologous RV protocol imparted a larger boosting effect. The α-PA data also highlight that the inf-LEF, as well as the inf-RBD, can induce significant antibody responses to intact PA. The ELISA data showing the reactivity of sera to purified His-tagged LEF protein (Fig. 2c) indicate that the antibody response induced specifically to this domain are quite robust, even following a single inoculation. All influenza virus constructs also induced sizable antibody responses to the HA component of the chimeric protein, and these data are presented as hemagglutination inhibition (HAI) titers in Fig. 2d and h.
The IgG antibody responses induced following heterologous prime/boost regimens are shown in Fig. 2e, f, and g. The striking feature of these results involves the magnitude of the antibody responses induced by priming with the influenza virus vectors followed by boosting with the RV vectors, which reached titers on the order of 105 ng/ml. This was ∼1 log higher than those observed for the reciprocal RV/influenza virus regimen and ∼4-fold higher than that determined for homologous prime/boost experiments with the RV constructs alone. This suggests that the influenza virus vector is advantageous compared to the other vectors tested with respect to the mechanism of immune system priming. This could be due to several things, such as its properties as a live replicating vector, the route of inoculation in the respiratory tract, or the types of antigen-presenting cells in these tissues. Single inoculations with the influenza viruses-LEF viruses once again generated strong α-LEF responses but, as expected, were not boosted by the RV containing the RBD domain.
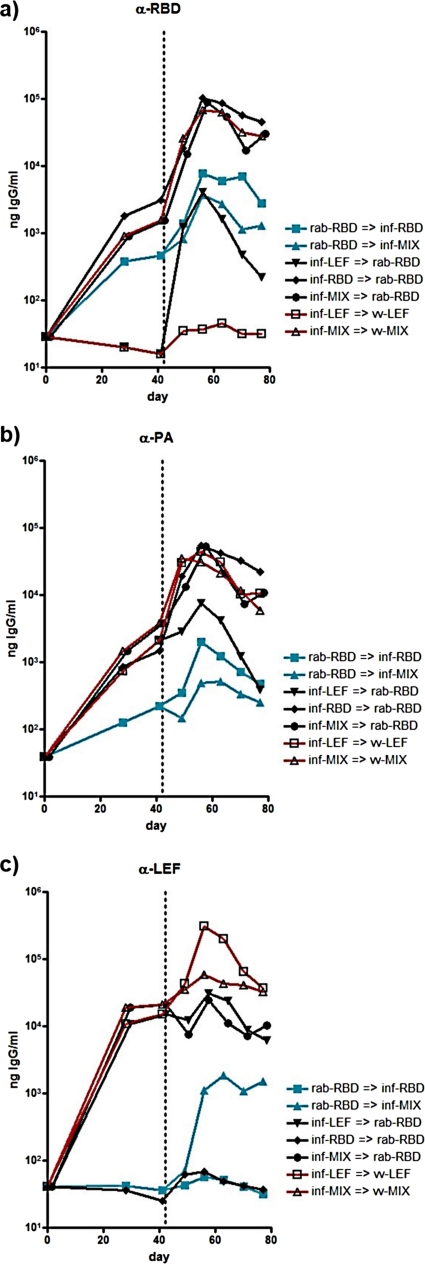
Although boosting with homologous viruses resulted in modest increases in antibody titers, the more striking results observed in influenza virus-primed/RV-boosted mice suggests that a heterologous boost is needed in order to avoid preexisting immunity to the original vector. This hypothesis is further supported by the ELISA data shown in Fig. 3, which were obtained after boosting with the recombinant VVs described above, which express chimeric HA/RBD or HA/LEF proteins equivalent to those in the influenza virus vectors. These data indicate that the VV vectors were able to boost the α-PA and α-RBD antibody titers to levels similar to those seen with the influenza virus-primed/RV-boosted groups. The enhanced boost effect was also observed with the mice that were primed with inf-LEF and then boosted with vv-LEF, for which the serum titers were almost a log higher than those primed and boosted with inf-LEF alone (Fig. 3b). These results suggest that a heterologous boost is necessary in order to achieve these high antibody levels.
FIG. 3.
Antibody responses after heterologous boosting. The α-RBD (a), α-PA (b), or α-LEF (c) antibody titers in mice before and after priming and boosting with the indicated vectors are presented.
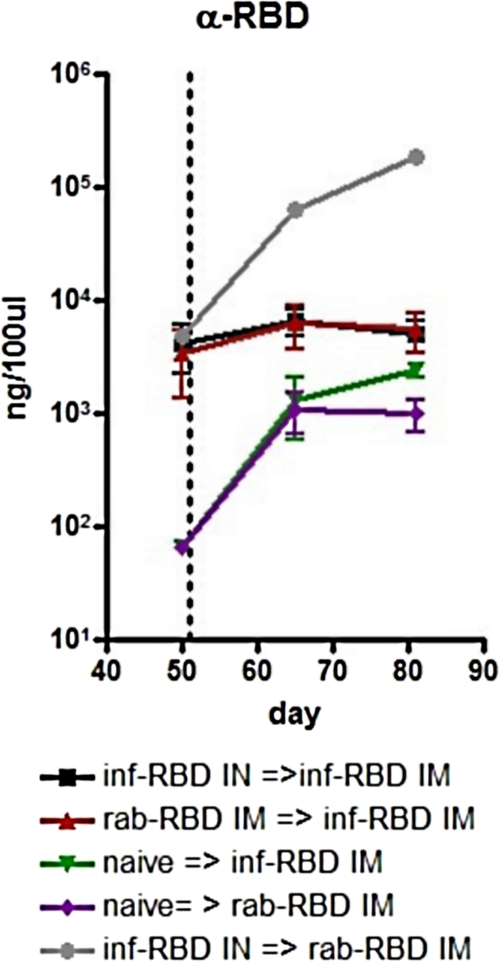
Boost effects using alternative routes of inoculation.
To examine whether the route of inoculation is responsible for the boost effects observed in Fig. 2e to g and Fig. 3, groups of mice were primed with inf-RBD IN or rab-RBD IM and then boosted i.m. with one of these two vectors on day 51. The results from these regimens are shown in Fig. 4. Naive mice immunized with either rab-RBD i.m. or β-propiolactone-inactivated inf-RBD i.m. showed similar antibody titers against RBD, demonstrating that the influenza virus vectors are immunogenic when given by this route. However, antibody levels were only slightly increased in mice that were primed with rab-RBD i.m. or inf-RBD i.n. and then boosted with inf-RBD i.m. In this experiment, high levels of α-RBD antibodies were again observed with the influenza virus i.n./RV i.m. regime, confirming the data from the experiments detailed in Fig. 2. These data suggest that it is unlikely that the route of inoculation alone is responsible for the increased titers observed in the inf-RBD-primed/rab-RBD-boosted mice. Perhaps, in inactivated form, the RV vector displays the antigen more effectively or persists for a longer period of time.
FIG. 4.
Antibody responses after i.m. boosting. α-RBD antibody titers in mice before and after intramuscular boosts with the indicated vector on day 42 are presented.
In vitro toxin neutralization.
The ability of serum obtained in the experiments detailed in Fig. 2 and 3 to neutralize anthrax toxin in vitro was assessed by using an MTT cell viability assay with J774 macrophage cells (26). In this assay, a neutralization titer greater than 100 is considered positive, and anything less than that is reported as <100. The results of this assay using pooled sera from different groups of mice taken at day 28 postprime and days 56 or 77 (days 14 and 35 postboost) were analyzed and are shown in Table 1. No neutralization was observed for mice that were primed with rab-RBD regardless of the time point or immunization protocol. Similarly, no neutralization was seen in mice that were primed with the inf-LEF vector, even though the mice that were boosted with vv-LEF displayed very high α-LEF titers (Fig. 3). This suggests that α-LEF antibodies alone may not be neutralizing in a BALB/c mouse background. In contrast, neutralizing activity was detectable with mice that were primed with a mix of inf-LEF and inf-RBD (inf-MIX) and boosted with either rab-RBD or a mix of vv-LEF and vv-RBD (vv-MIX). The only group that demonstrated any neutralization activity prior to being boosted was the inf-RBD-primed group. This is not surprising since it correlates with the slightly higher antibody titers observed in these mice by ELISA at this time point (Fig. 2, 3, and 4). Neutralizing activity remained detectable at day 14 following a homologous boost with inf-RBD but had waned by day 35. The most striking results can be seen in the mice that were primed with inf-RBD and then boosted with rab-RBD. These mice had a neutralizing titer of 1,038 on day 14 postboost, and this increased to 7,039 by day 35. The observation that the neutralization titers increased for this group, whereas the total specific antibody detectable by ELISA decreased (Fig. 2), is noteworthy. Potential explanations for this may involve B-cell affinity maturation or somatic hypermutation in germinal centers during this time. As noted above, it is also possible that persistence of antigen with the RV vector could play a role as well.
TABLE 1.
Anthrax toxin neutralization titersa
| Priming virus (day 0)b | Titer (day 28) | Boosting virus (day 42) | Titer |
|
|---|---|---|---|---|
| Day 56 | Day 77 | |||
| rab-RBD | <100 | rab-RBD | <100 | <100 |
| inf-RBD | <100 | <100 | ||
| inf-LEF | <100 | <100 | ||
| inf-MIX | <100 | <100 | ||
| inf-RBD | 166 | rab-RBD | 1,038 | 7,039 |
| inf-RBD | 163 | <100 | ||
| inf-LEF | <100 | rab-RBD | <100 | <100 |
| inf-LEF | <100 | <100 | ||
| vv-LEF | <100 | <100 | ||
| inf-MIX | <100 | rab-RBD | 165 | 241 |
| inf-MIX | <100 | <100 | ||
| vv-MIX | 165 | <100 | ||
| Wild-type influenza virus | <100 | |||
| Naive serum | <100 | |||
The mice were primed with the indicated virus on day 0 and then boosted with the indicated virus on day 42. The anthrax toxin neutralization titers at days 28, 56, and 77 are shown. The titers are expressed as the reciprocal of the dilution that protected 50% of the cells in an MTT assay (see Materials and Methods). A neutralizing titer less than 100 is considered negative and is reported as <100.
“Day” refers to days after initial inoculation.
Although the α-LEF antibodies were not shown to be neutralizing in these experiments, the correlates of toxin neutralization from challenge by live BA appear to vary with the animal model and genetic background. Indeed, α-LEF antibodies have been shown to be protective in C57BL/6 mice immunized with a purified form of this domain, and two monoclonal antibodies with toxin-neutralizing activity were shown to recognize distinct epitopes within this domain (2). The lack of neutralizing ability with α-LEF sera observed here could be attributed to the use of BALB/c mice, since the responses to all domains have been demonstrated to be variable depending on the genetic background of immunized mice (1). Using a killed, but metabolically active (KBMA) form of BA, Skoble et al. demonstrated the protection of mice against live spore challenges even though the α-PA antibodies in the sera were measured at levels of ∼103 ng/ml (29). This concentration is considerably lower than the antibody titers generated in our study, although other factors were also likely to be involved in the protective effects of the KBMA vaccine. Other studies suggest that the mouse model utilized here is not ideal for animal protection studies, particularly with regard to the role of α-PA responses (15, 34).
Despite these issues, there is clearly a need to continue exploring alternative vaccine strategies for protection against anthrax. Presently, there is only one U.S. Food and Drug Administration-approved vaccine against anthrax available in the United States, the anthrax vaccine absorbed (AVA). For several reasons, including the requirement of five or six immunizations over the first 18 months and yearly boosts thereafter (32), AVA is less than ideal, and a number of strategies have been explored over the past several years to express or deliver PA, or components of it, in efforts to improve the costs, logistics, and efficacy of anthrax vaccines (5, 10, 12, 21, 35). However, to date, none of these strategies have demonstrated sufficient efficacy to replace the AVA. For these reasons, we will continue the examination of our constructs, and immunization protocols in alternative animal models, for both the induction of toxin neutralization activity and protection from a BA spore challenge, are being planned.
Importantly, we demonstrate here that simultaneous immunization with two homologous vectors, one containing the LEF domain and the other the RBD domain, results in antibodies against both domains and that both responses can be boosted by heterologous vectors (Fig. 3). This could prove beneficial when immunizing more heterogeneous populations, including humans who have multiple major histocompatibility complex alleles. As with any vector-based immunization approach, preexisting immunity to the vector must be considered. For RV, we previously showed in mice and rhesus macaques that preexisting immunity against RV completely blocks a second infection with RV (11, 23, 31). However, such preexisting anti-RV immune responses do not affect the immune responses against boosting with killed virus carrying a foreign antigen in their virions (data not shown). In addition, the seroprevalence for RV is low in humans, as it is for VV among people under 40 years of age in the United States. With regard to influenza virus HA-based vectors, the expanding structural knowledge of the 16 HA subtypes should make it possible to construct influenza virus vectors with subtypes to which humans have limited preexisting immunity. Indeed, preexisting immunity to influenza virus vectors may not pose the problems that are envisaged, since drift strains appear capable of reinfecting individuals on a regular basis despite minimal changes to antigenic sites of HA. In relation to this, we have carried out a related set experiments involving responses to influenza virus HA vectors in mice that have been previously infected with viruses containing alternative surface antigens, and we have shown that whereas preexisting immunity does in fact dampen responses to homologous infection, it is possible to modulate immune responses to the insert when alternative HA and NA proteins are used (data not shown).
It is interesting that none of the sera from mice primed with rab-RBD demonstrated neutralization capacity, regardless of the immunization protocol. This suggests that the mechanism by which i.n. infection by live influenza viruses prime the immune system in this mouse model provides a desirable effect. Several factors could be responsible for this, including the properties of a live vector versus an inactivated vector, or possibly the species or environment of antigen-presenting cells encountered in the respiratory tract. These issues merit further examination, since they may be relevant for the design of immunogens unrelated to those examined in the present study. Furthermore, the utility of using chimeric influenza virus and RV vectors such as those described here is not limited to a single pathogen but can be broadly applicable.
Acknowledgments
We thank Johnny Peterson and Laurie Sower for generous assistance in carrying out the toxin neutralization assays, and we thank Summer Galloway, Ganesh Talekar, and Tim Barnett for critical comments on the manuscript.
This study was supported by NIH Public Health Service grant from NIAID AI/EB53359 and contract HHSN266200700006C to D.A.S. and grant R41AI063822 to M.J.S. and by the Emory Center for AIDS Research (P30AI050409).
M.J.S. declares competing financial interests due to a patent application for the RV technology and consulting agreements with commercial entities.
Footnotes
Published ahead of print on 26 May 2010.
REFERENCES
- 1.Abboud, N., and A. Casadevall. 2008. Immunogenicity of Bacillus anthracis protective antigen domains and efficacy of elicited antibody responses depend on host genetic background. Clin. Vaccine Immunol. 15:1115-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abboud, N., M. De Jesus, A. Nakouzi, R. J. Cordero, M. Pujato, A. Fiser, J. Rivera, and A. Casadevall. 2009. Identification of linear epitopes in Bacillus anthracis protective antigen bound by neutralizing antibodies. J. Biol. Chem. 284:25077-25086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blasco, R., and B. Moss. 1995. Selection of recombinant vaccinia viruses on the basis of plaque formation. Gene 158:157-162. [DOI] [PubMed] [Google Scholar]
- 4.Blazevic, V., C. M. Trubey, and G. M. Shearer. 2000. Comparison of in vitro immunostimulatory potential of live and inactivated influenza viruses. Hum. Immunol. 61:845-849. [DOI] [PubMed] [Google Scholar]
- 5.Boyaka, P. N., A. Tafaro, R. Fischer, S. H. Leppla, K. Fujihashi, and J. R. McGhee. 2003. Effective mucosal immunity to anthrax: neutralizing antibodies and Th cell responses following nasal immunization with protective antigen. J. Immunol. 170:5636-5643. [DOI] [PubMed] [Google Scholar]
- 6.Bradley, K. A., J. Mogridge, M. Mourez, R. J. Collier, and J. A. Young. 2001. Identification of the cellular receptor for anthrax toxin. Nature 414:225-229. [DOI] [PubMed] [Google Scholar]
- 7.Cox, R. J., K. A. Brokstad, and P. Ogra. 2004. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand. J. Immunol. 59:1-15. [DOI] [PubMed] [Google Scholar]
- 8.Flick-Smith, H. C., N. J. Walker, P. Gibson, H. Bullifent, S. Hayward, J. Miller, R. W. Titball, and E. D. Williamson. 2002. A recombinant carboxy-terminal domain of the protective antigen of Bacillus anthracis protects mice against anthrax infection. Infect. Immun. 70:1653-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foley, H. D., J. P. McGettigan, C. A. Siler, B. Dietzschold, and M. J. Schnell. 2000. A recombinant rabies virus expressing vesicular stomatitis virus glycoprotein fails to protect against rabies virus infection. Proc. Natl. Acad. Sci. U. S. A. 97:14680-14685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedlander, A. M., and S. F. Little. 2009. Advances in the development of next-generation anthrax vaccines. Vaccine 27(Suppl. 4):D28-D32. [DOI] [PubMed] [Google Scholar]
- 11.Gomme, E. A., E. J. Faul, P. Flomenberg, J. P. McGettigan, and M. J. Schnell. 2010. Characterization of a single-cycle rabies virus-based vaccine vector. J. Virol. 84:2820-2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorse, G. J., W. Keitel, H. Keyserling, D. N. Taylor, M. Lock, K. Alves, J. Kenner, L. Deans, and M. Gurwith. 2006. Immunogenicity and tolerance of ascending doses of a recombinant protective antigen (rPA102) anthrax vaccine: a randomized, double-blinded, controlled, multicenter trial. Vaccine 24:5950-5959. [DOI] [PubMed] [Google Scholar]
- 13.Haas, J., E. C. Park, and B. Seed. 1996. Codon usage limitation in the expression of HIV-1 envelope glycoprotein. Curr. Biol. 6:315-324. [DOI] [PubMed] [Google Scholar]
- 14.Hatziioannou, T., E. Delahaye, F. Martin, S. J. Russell, and F. L. Cosset. 1999. Retroviral display of functional binding domains fused to the amino terminus of influenza hemagglutinin. Hum. Gene Ther. 10:1533-1544. [DOI] [PubMed] [Google Scholar]
- 15.Heninger, S., M. Drysdale, J. Lovchik, J. Hutt, M. F. Lipscomb, T. M. Koehler, and C. R. Lyons. 2006. Toxin-deficient mutants of Bacillus anthracis are lethal in a murine model for pulmonary anthrax. Infect. Immun. 74:6067-6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hering, D., W. Thompson, J. Hewetson, S. Little, S. Norris, and J. Pace-Templeton. 2004. Validation of the anthrax lethal toxin neutralization assay. Biologicals 32:17-27. [DOI] [PubMed] [Google Scholar]
- 17.Jernigan, D. B., P. L. Raghunathan, B. P. Bell, R. Brechner, E. A. Bresnitz, J. C. Butler, M. Cetron, M. Cohen, T. Doyle, M. Fischer, C. Greene, K. S. Griffith, J. Guarner, J. L. Hadler, J. A. Hayslett, R. Meyer, L. R. Petersen, M. Phillips, R. Pinner, T. Popovic, C. P. Quinn, J. Reefhuis, D. Reissman, N. Rosenstein, A. Schuchat, W. J. Shieh, L. Siegal, D. L. Swerdlow, F. C. Tenover, M. Traeger, J. W. Ward, I. Weisfuse, S. Wiersma, K. Yeskey, S. Zaki, D. A. Ashford, B. A. Perkins, S. Ostroff, J. Hughes, D. Fleming, J. P. Koplan, and J. L. Gerberding. 2002. Investigation of bioterrorism-related anthrax, United States, 2001: epidemiologic findings. Emerg. Infect. Dis. 8:1019-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang, S. D., D. Pye, and J. C. Cox. 1986. Inactivation of poliovirus with beta-propiolactone. J. Biol. Stand. 14:103-109. [DOI] [PubMed] [Google Scholar]
- 19.Kang, S. M., L. Guo, Q. Yao, I. Skountzou, and R. W. Compans. 2004. Intranasal immunization with inactivated influenza virus enhances immune responses to coadministered simian-human immunodeficiency virus-like particle antigens. J. Virol. 78:9624-9632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li, Z. N., S. N. Mueller, L. Ye, Z. Bu, C. Yang, R. Ahmed, and D. A. Steinhauer. 2005. Chimeric influenza virus hemagglutinin proteins containing large domains of the Bacillus anthracis protective antigen: protein characterization, incorporation into infectious influenza viruses, and antigenicity. J. Virol. 79:10003-10012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Little, S. F., B. E. Ivins, P. F. Fellows, M. L. Pitt, S. L. Norris, and G. P. Andrews. 2004. Defining a serological correlate of protection in rabbits for a recombinant anthrax vaccine. Vaccine 22:422-430. [DOI] [PubMed] [Google Scholar]
- 22.Liu, S., and S. H. Leppla. 2003. Cell surface tumor endothelium marker 8 cytoplasmic tail-independent anthrax toxin binding, proteolytic processing, oligomer formation, and internalization. J. Biol. Chem. 278:5227-5234. [DOI] [PubMed] [Google Scholar]
- 23.McKenna, P. M., P. P. Aye, B. Dietzschold, D. C. Montefiori, L. N. Martin, P. A. Marx, R. J. Pomerantz, A. Lackner, and M. J. Schnell. 2004. Immunogenicity study of glycoprotein-deficient rabies virus expressing simian/human immunodeficiency virus SHIV89.6P envelope in a rhesus macaque. J. Virol. 78:13455-13459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neumann, G., T. Watanabe, H. Ito, S. Watanabe, H. Goto, P. Gao, M. Hughes, D. R. Perez, R. Donis, E. Hoffmann, G. Hobom, and Y. Kawaoka. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. U. S. A. 96:9345-9350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petosa, C., R. J. Collier, K. R. Klimpel, S. H. Leppla, and R. C. Liddington. 1997. Crystal structure of the anthrax toxin protective antigen. Nature 385:833-838. [DOI] [PubMed] [Google Scholar]
- 26.Pitt, M. L., S. F. Little, B. E. Ivins, P. Fellows, J. Barth, J. Hewetson, P. Gibbs, M. Dertzbaugh, and A. M. Friedlander. 2001. In vitro correlate of immunity in a rabbit model of inhalational anthrax. Vaccine 19:4768-4773. [DOI] [PubMed] [Google Scholar]
- 27.Scobie, H. M., G. J. Rainey, K. A. Bradley, and J. A. Young. 2003. Human capillary morphogenesis protein 2 functions as an anthrax toxin receptor. Proc. Natl. Acad. Sci. U. S. A. 100:5170-5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sellman, B. R., M. Mourez, and R. J. Collier. 2001. Dominant-negative mutants of a toxin subunit: an approach to therapy of anthrax. Science 292:695-697. [DOI] [PubMed] [Google Scholar]
- 29.Skoble, J., J. W. Beaber, Y. Gao, J. A. Lovchik, L. E. Sower, W. Liu, W. Luckett, J. W. Peterson, R. Calendar, D. A. Portnoy, C. R. Lyons, and T. W. Dubensky, Jr. 2009. Killed but metabolically active Bacillus anthracis vaccines induce broad and protective immunity against anthrax. Infect. Immun. 77:1649-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith, M. E., M. Koser, S. Xiao, C. Siler, J. P. McGettigan, C. Calkins, R. J. Pomerantz, B. Dietzschold, and M. J. Schnell. 2006. Rabies virus glycoprotein as a carrier for anthrax protective antigen. Virology 353:344-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tan, G. S., P. M. McKenna, M. L. Koser, R. McLinden, J. H. Kim, J. P. McGettigan, and M. J. Schnell. 2005. Strong cellular and humoral anti-HIV Env immune responses induced by a heterologous rhabdoviral prime-boost approach. Virology 331:82-93. [DOI] [PubMed] [Google Scholar]
- 32.Turnbull, P. C. 1991. Anthrax vaccines: past, present, and future. Vaccine 9:533-539. [DOI] [PubMed] [Google Scholar]
- 33.Welkos, S., S. Little, A. Friedlander, D. Fritz, and P. Fellows. 2001. The role of antibodies to Bacillus anthracis and anthrax toxin components in inhibiting the early stages of infection by anthrax spores. Microbiology 147:1677-1685. [DOI] [PubMed] [Google Scholar]
- 34.Welkos, S. L., and A. M. Friedlander. 1988. Pathogenesis and genetic control of resistance to the Sterne strain of Bacillus anthracis. Microb. Pathog. 4:53-69. [DOI] [PubMed] [Google Scholar]
- 35.Yin, Y., J. Zhang, D. Dong, S. Liu, Q. Guo, X. Song, G. Li, L. Fu, J. Xu, and W. Chen. 2008. Chimeric hepatitis B virus core particles carrying an epitope of anthrax protective antigen induce protective immunity against Bacillus anthracis. Vaccine 26:5814-5821. [DOI] [PubMed] [Google Scholar]
- 36.Zhao, J., J. C. Milne, and R. J. Collier. 1995. Effect of anthrax toxin's lethal factor on ion channels formed by the protective antigen. J. Biol. Chem. 270:18626-18630. [DOI] [PubMed] [Google Scholar]