Abstract
Chagas' disease is a global public health problem due to the recent exchange of population between Latin America and other regions, including Europe. The recent development of rapid diagnostic tests (RDTs) for Trypanosoma cruzi infection may improve patient access to diagnosis and care worldwide. We evaluated the diagnostic accuracy of the Chagas Stat-Pak RDT in a cohort of undocumented Latin-American migrants living in Geneva, Switzerland. Study participants were enrolled in a primary health care center. The Chagas Stat-Pak test was performed independently on blood and serum samples. A combination of two commercialized enzyme-linked immunosorbent assay (ELISA)-based serological tests was used for comparison (reference standard). A total of 999 adults (median age, 36 years) were included in the study; the majority were women (83%) and originally from Bolivia (47%) or Brazil (25%). A total of 125 participants (12.5%) were diagnosed with T. cruzi infection; with the exception of three individuals, all individuals diagnosed with T. cruzi were originally from Bolivia. The sensitivity and specificity of the Chagas Stat-Pak test on blood samples were 95.2% (95% confidence interval [95% CI], 89.2% to 97.9%) and 99.9% (95% CI, 99.3% to 100%), respectively. When the test was performed on serum samples, the sensitivity was 96% (95% CI, 91% to 98.3%), and the specificity was 99.8% (95% CI, 99.2% to 99.9%). The concordance of test results for blood and serum samples was 99.7%. Both negative and positive predictive values were above 98%. The Chagas Stat-Pak is an accurate diagnostic test for T. cruzi infection among Latin-American migrants living in Europe. The mild deficit in sensitivity should be interpreted in light of its ease of use and capacity to provide immediate results, which allow more people at risk to have access to diagnosis and care both in countries where Chagas' disease is endemic and in countries where this disease is not endemic.
Chagas' disease is caused by Trypanosoma cruzi, a protozoan parasite naturally transmitted by hematophagous triatomine insects. The parasite can also be transmitted by blood transfusion or organ transplantation, from mother to fetus, sporadically by ingestion of contaminated food or drinks, and rarely by laboratory accident. Vector-borne transmission is restricted to the Americas, where an estimated 8 million people are infected, with the majority undiagnosed and in the chronic stage of the disease (15). However, Chagas' disease should now be considered a global disease mainly due to important migration movements between Latin America and the United States, Canada, Japan, Australia, and many European countries (19). Physicians working outside Latin America should be aware not only of the chronic cardiac and digestive complications that occur in 20 to 30% of infected patients typically after 10 to 30 years but also of the risk of active local transmission of T. cruzi to newborns (vertical transmission) and to recipients of infected blood or organs.
In Europe, many countries are affected by the emergence of Chagas' disease, Spain being the most affected country with an estimated 36,000 to 122,000 infected people (6, 16). Switzerland has not been spared, with several reported cases of chronic disease with and without cardiopathy, congenital infections, and reactivation following organ transplant over the last few years (7, 9). Many Latin-American immigrants at risk for T. cruzi infection who recently settled down in Switzerland have neither residence permit nor health insurance (undocumented). The majority are women of childbearing age who are employed in the domestic industry (i.e., housecleaning and keeping children). A recent study conducted within this population in Geneva, Switzerland, showed that 130 out of 1,012 (12.8%) persons were infected by T. cruzi, with a very high prevalence found among Bolivians (26.2%) (8).
The diagnosis of T. cruzi infection among immigrants living in countries where T. cruzi infection is not endemic, such as Switzerland, is crucial. First, it allows individuals to receive antiparasitic treatment, which is likely to prevent or slow down the progression of chronic organ damage (22). Treating women of childbearing age may also decrease the risk of vertical transmission of T. cruzi during subsequent pregnancies. Second, systematic screening of pregnant women at risk allows for early detection of infection in newborns at the time of delivery or early after delivery, antiparasitic drugs being highly efficacious and well tolerated during the first 3 years of life (1, 9). Third, screening blood and organ donors at risk prevents the transmission of T. cruzi. Last, screening immunosuppressed individuals (e.g., organ transplant recipients) allows for early detection and treatment of disease reactivation.
The diagnosis of Chagas' disease during the chronic phase relies on serological tests, as both parasitological and molecular methods lack sensitivity. As no single assay is considered both sufficiently sensitive and specific, two or more tests based on different antigens or techniques are used in parallel to increase diagnostic accuracy. Recently, rapid diagnostic tests (RDTs), such as the Chagas Stat-Pak (Chembio Diagnostic Systems, Medford, NY), have been developed using recombinant proteins in an immunochromatographic assay. The main advantages of RDTs are (i) devices available for individual use, (ii) rapid processing, (iii) storage at room temperature, (iv) no requirement for laboratory reagents or equipment, (v) no need for specialized laboratory technical skills, and (vi) the possibility of storing the device with the patient's file (13). The Chagas Stat-Pak assay (on serum) was initially evaluated in multicentric studies conducted in South and Central America, yielding sensitivity and specificity estimates of 98.5 to 100% and 94.8 to 99.9%, respectively (12, 17). Two field evaluations of the Chagas Stat-Pak assay (on finger-pricked blood) in Bolivia showed sensitivity and specificity estimates of 93.4 to 94.7 and 97.3 to 99%, respectively (3, 18). The lower sensitivity estimates observed in the two latter studies could be caused by the use of blood instead of serum. A direct comparison of the Chagas Stat-Pak on blood and serum showed similar results but on a limited number of samples (n = 33) (12). Other factors, such as geographic location, age, and pregnancy, have been shown to influence the performance of the Stat-Pak (3, 20, 21). The Chagas Stat-Pak has never been evaluated in migrants living outside Latin America who carry no risk of chronic reinfections. Therefore, we aimed to evaluate and compare the diagnostic performance of the Chagas Stat-Pak on blood and serum samples from a cohort of Latin-American migrants originally from various countries where Chagas' disease is endemic and living in Geneva, Switzerland.
MATERIALS AND METHODS
Study location and participants.
The study was conducted in the city of Geneva (population, 188,000) located in the canton of Geneva (population, 450,000) in western Switzerland between June and November 2008. Enrollment in the study took place at the Unité Mobile de Soins Communautaires (UMSCO) and in the community (e.g., after church service). The UMSCO is a primary health care center run by the Geneva University Hospitals (HUG) that provides more than 14,000 consultations yearly, 65% of which are for Latin-American undocumented migrants. Latin-American communities were mobilized by the distribution of flyers, the hanging of information posters in key locations and by direct discussions with community leaders. A bilingual (Spanish and French) nurse was responsible for enrolling participants and performing the index test. All Latin-American migrants living in the canton of Geneva in Switzerland and 16 years old or more were eligible for the study. Eligible persons received written (patient information forms available in Spanish, Portuguese, and French) and oral information. After inclusion, a short questionnaire collecting demographic and medical data was completed by all participants. The study was approved by the ethical review board of the Geneva University Hospitals in January 2008 (study protocol 07-285).
Procedures.
Blood samples were collected from the study participants and stored in one tube containing EDTA and two tubes without anticoagulant at 4 to 8°C. At the end of the daily enrollment period (i.e., within 4 h), the research nurse performed the Chagas Stat-Pak test on the EDTA-treated blood sample following a standard operating procedure (SOP) based on the manufacturer's instructions. Within 48 h, the two dry tubes were carried in a cool box to the HUG parasitology lab, where the serum samples were collected, aliquoted, and stored at −20°C. The Chagas Stat-Pak test was performed on stored sera 3 or 4 times weekly by a senior laboratory technician who was blinded to the results of the Chagas Stat-Pak test performed on blood samples.
Chagas Stat-Pak assay.
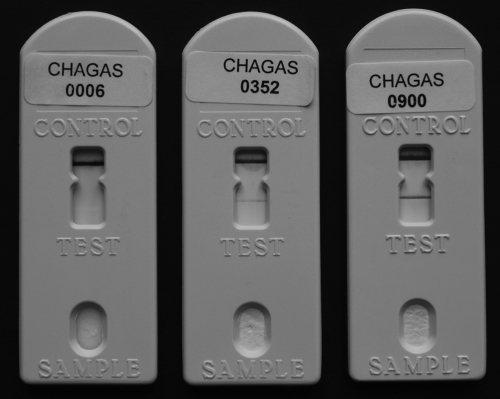
Ten microliters of room temperature EDTA-treated blood (at UMSCO) or 5 μl of serum (at HUG parasitology lab) were collected with a disposable Microsafe tube or a micropipette, respectively, and were added to the “sample” well. After the diluent was added, the sample was allowed to flow laterally across the membrane, and the result was read after exactly 15 min (Fig. 1). The test was considered positive if pink/purple lines were seen in the test and control areas. The test was considered negative if a pink/purple line was seen only in the control area. The test was invalid (and was repeated) if no line was seen in the control area.
FIG. 1.
Examples of negative and positive Chagas Stat-Pak results. From left to right, negative, weakly positive, and strongly positive Stat-Pak results are shown.
Reference standard.
A combination of two commercialized enzyme-linked immunosorbent assay (ELISA)-based serological tests was used for diagnostic classification and served for comparison (reference standard) for the Chagas Stat-Pak assay: the bioMérieux Elisa cruzi and the Biokit bioelisa Chagas, which detect antibodies against crude and recombinant T. cruzi antigens, respectively. Both tests were performed according to the manufacturers' instructions every 2 to 4 weeks by the head of the HUG parasitology lab, who was kept blinded to the results of the Chagas Stat-Pak test. Both tests were repeated in case of discrepant results (e.g., positive and negative results; doubtful and negative results). If the discrepancy remained, the serum sample was sent to the reference laboratory for definite classification (see below).
All individuals were contacted on their mobile phone to communicate the results of the ELISAs. Patients with positive test results were given an appointment to be clinically investigated for the presence of chronic cardiac or digestive tract complications. The indication for specific treatment with nifurtimox or benznidazole was discussed individually, following recently published guidelines (2).
Laboratory quality control.
Serum samples from all individuals with positive or discordant ELISA results and from 10% of the individuals with negative tests were sent every 2 months to the laboratory of the University of Goias (A. Luquetti), Brazil, for independent quality control. A combination of four serological tests was performed there: Chagatek ELISA (bioMérieux, Argentina), EIE-recombinant Chagas (Bio-Manguinhos, Brazil), Chagatest hemagglutination inhibition (HAI) (Wiener, Argentina), and an in-house immunofluorescence test using bioMérieux conjugate (bioMérieux, Brazil). The results were sent back to the investigators with an integrated conclusion (positive, negative, or nonconclusive).
Data management and statistical analysis.
The results of the Chagas Stat-Pak test on blood and serum samples and of bioMérieux Elisa cruzi and Biokit bioelisa Chagas were entered into separate Excel files and later merged by one of the investigators (F. Chappuis). The data were analyzed with SPSS 15.0 for Windows version (SPSS, Inc., Chicago, Ill.). T. cruzi infection was defined by positive bioMérieux Elisa cruzi and Biokit bioelisa Chagas tests (HUG), with positive result of the panel of serological tests at the reference laboratory in Brazil. The absence of T. cruzi infection was defined as (i) negative bioMérieux Elisa cruzi and Biokit bioelisa Chagas tests in the absence of a positive or nonconclusive test result in the reference laboratory or (ii) discrepant bioMérieux Elisa cruzi and Biokit bioelisa Chagas test results with negative test results in the reference laboratory. The sensitivity, specificity, positive and negative predictive values, and their 95% confidence intervals (95% CIs) were calculated for the Chagas Stat-Pak test on blood and serum samples from the groups of infected and noninfected individuals by using the Confidence Interval Analysis software for Windows. Reproducibility was assessed by comparing the result of the Chagas Stat-Pak test on blood at UMSCO with the Chagas Stat-Pak from stored serum at HUG using Cohen's kappa coefficient, which was interpreted according to the grading system of Landis and Koch (11).
RESULTS
Demographics.
Out of a total of 1,012 individuals enrolled at UMSCO between June and November 2009, 999 were included in the diagnostic validation analysis of the Chagas Stat-Pak assay. Thirteen participants were excluded from analysis because of previous treatment for Chagas' disease (n = 10) or uncertain disease status (n = 3). These three individuals had negative ELISA results at the HUG but nonconclusive test results at the reference laboratory in Brazil. The median age of the 999 participants was 36 years (interquartile range, 28 to 46) with a large predominance of females (82.5%). The study participants were originally from Bolivia (47.4%), Brazil (25.1%), Colombia (6.2%), Ecuador (4.8%), Peru (4.8%), Paraguay (2.8%), Nicaragua (2.4%), Honduras (2.4%), Chile (1.1%), or elsewhere in Latin America (3%). All but one participant were undocumented migrants who had been living outside Latin America for a median time of 4 years (range, 0 to 42 years).
Sensitivity and specificity.
The Chagas Stat-Pak assay was performed on blood samples from 874 participants (87.5%) at UMSCO, and the assay was performed on serum samples from all study participants at the HUG parasitology lab. The Chagas Stat-Pak assay could not be performed in the first 125 individuals at UMSCO because the supply of tests was unexpectedly delayed for 2 weeks. The median time between blood sampling and Stat-Pak testing with serum was 2 days (range, 0 to 16 days). Trypanosoma cruzi infection was serologically diagnosed in 125 (12.5%) of the 999 participants: 122 (97.6%) from Bolivia, 2 (1.6%) from Brazil, and 1 (0.8%) from Argentina. All positive results at HUG were confirmed at the reference laboratory of the University of Goias, Brazil. When the Chagas Stat-Pak assay was performed on blood samples, it correctly identified 99 out of 104 infected patients (sensitivity, 95.2%; 95% CI, 89.2% to 97.9%) and 769 out of 770 noninfected individuals (specificity, 99.9%; 95% CI, 99.3% to 100%). When it was performed on serum samples, 120 out of 125 infected patients (sensitivity, 96%; 95% CI, 91% to 98.3%) and 872 out of 874 noninfected individuals (specificity, 99.8%; 95% CI, 99.2% to 99.9%) were correctly classified. A summary of the Stat-Pak assay results and performance that includes positive and negative predictive value estimates is shown in Tables 1 and 2.
TABLE 1.
Results of the Chagas Stat-Pak assay on blood and serum samples from Latin-American migrants in Geneva, Switzerland
| Subject | Chagas Stat-Pak assay result on: |
|||
|---|---|---|---|---|
| Blood samples (n = 874) |
Serum samples (n = 999) |
|||
| Positive | Negative | Positive | Negative | |
| Infected patients | 99 | 5 | 120 | 5 |
| Noninfected individuals | 1 | 769 | 2 | 872 |
TABLE 2.
Summary of the performance of the Chagas Stat-Pak assay on blood and serum samples from Latin-American migrants in Geneva, Switzerlanda
| Sample | Sensitivity (%) (95% CI) | Specificity (%) (95% CI) | Positive PV (%) (95% CI) | Negative PV (%) (95% CI) |
|---|---|---|---|---|
| Blood | 95.2 (89.2-97.9) | 99.9 (99.3-100) | 99.0 (94.6-99.8) | 99.4 (98.5-99.7) |
| Serum | 96.0 (91.0-98.3) | 99.8 (99.2-99.9) | 98.4 (94.2-99.5) | 98.4 (94.2-99.5) |
95% CI, 95% confidence interval; PV, predictive value.
Reproducibility.
The comparative results of the Chagas Stat-Pak performed on blood samples (UMSCO) and serum samples (HUG) are shown in Table 3. Reproducibility was excellent (kappa, 0.98; 95% CI, 96.4% to 100%), and 99.7% of the test results were concordant.
TABLE 3.
Comparison of the Chagas Stat-Pak test results on blood samples versus serum samples from 874 Latin-American migrants in Geneva, Switzerlanda
| Test result on serum samples | No. of blood samples with the following test result: |
|
|---|---|---|
| Positive | Negative | |
| Positive | 100 | 3 |
| Negative | 0 | 771 |
Concordance of results was 99.7%.
DISCUSSION
The Chagas Stat-Pak assay, a rapid diagnostic test (RDT) detecting antibodies against recombinant antigens of T. cruzi, showed good sensitivity (95.2 to 96%) and excellent specificity (99.8 to 99.9%) when tested with blood or serum samples from a large cohort of Latin-American adult migrants living in Geneva, Switzerland. The positive and negative predictive values were both above 98% in the population studied, which had a 12.5% prevalence of T. cruzi infection. The concordance of Stat-Pak results for blood and serum samples was near perfect (99.7%), and the reproducibility of the test was high.
Most previous studies evaluating the diagnostic accuracy of the Chagas Stat-Pak assay in South and Central America also revealed high sensitivity and specificity estimates (3, 10, 12, 17, 18, 20). Considering (i) the very high proportion (97.6%) of Bolivians among T. cruzi-infected patients in our study and (ii) the probable influence of geography on the Chagas Stat-Pak test performance (20, 21), it is more appropriate to restrict the comparison of test sensitivity with studies conducted with Bolivian patients. Our findings are consistent with published sensitivity estimates of the Chagas Stat-Pak in Bolivian patients, ranging from 93.4% to 98.6% (3, 14, 18, 20). One study showed lower Stat-Pak sensitivity (87.5%) among pregnant Bolivian woman, but the precision of the estimate was limited by the small number (n = 24) of T. cruzi-infected patients tested (21). Whereas the Chagas Stat-Pak assay appears less sensitive than some of the more sophisticated serological tests (e.g., ELISA, Western blotting [WB]) (14), this relative deficit in sensitivity must be interpreted in light of its ease of use, low cost, and capacity to provide immediate results. These practical issues are crucial, as they allow more people at risk to have access to diagnosis both in countries where Chagas' disease is endemic and in countries where this disease is not endemic (e.g., utilization in primary health care centers). Nevertheless, the development of a RDT with improved sensitivity is a priority.
The very high specificity of the Chagas Stat-Pak assay found in this study is consistent with high specificity estimates (97.4 to 100%) found by others (3, 12, 17, 18, 20, 21). Very high positive predictive values are therefore found when the prevalence of T. cruzi infection is moderate or high in the population tested. In these settings (e.g., Bolivians from areas where Chagas' disease is highly endemic) and provided that the test procedure is carefully followed, a positive Chagas Stat-Pak test result is diagnostic of T. cruzi infection.
We found a very high reproducibility of the Chagas Stat-Pak assay. The performance of the test was not significantly altered (only three false-negative results) when the test was performed on blood samples by a trained nurse with no prior experience in laboratory work compared to the test performed on serum samples by an experienced laboratory technician. A mistake in reading the test result is unlikely, as the three false-negative RDT results were confirmed as negative by an independent reader after completion of the study. It is therefore possible that testing patients using blood samples instead of serum or plasma samples may result in a loss of sensitivity, as hypothesized by others (3, 18), but our data show that the resulting loss in sensitivity is small, if present at all.
Some limitations of our study must be emphasized. First, as already mentioned, the sensitivity estimate of the Chagas Stat-Pak assay is valid for Bolivian adults only, as children were not included in our study and as nearly all T. cruzi-infected patients were originally from Bolivia. Second, the diagnostic accuracy of the Chagas Stat-Pak test may be overestimated, as the reference standard was also composed of serological tests. Unfortunately, this limitation cannot be avoided, as the sensitivity of other diagnostic approaches (i.e., parasitological and molecular techniques) is low during the chronic phase of Chagas' disease. Third, false-positive results of the Chagas Stat-Pak and ELISAs used as reference standards may have been caused by cross-reactivity with past or present leishmaniasis. Such cross-reactivity is seen mainly with visceral leishmaniasis, a rare and geographically restricted disease in Bolivia (5). None of our patients had symptoms or signs of active leishmaniasis.
The study results have had a significant impact on the diagnostic management of Chagas' disease in our hospital (HUG). The Chagas Stat-Pak assay has been recently introduced as a point-of-care test (POCT) in the primary care center (UMSCO) that provides care to the vast majority of undocumented Latin-American migrants living in Geneva, Switzerland. The test is also used as a POCT in the maternity ward when pregnant Latin-American migrants with no prior Chagas testing are admitted for delivery. A positive result triggers investigations of the cord blood to diagnose congenital transmission (9). Several nurses and midwives have been trained to perform the Stat-Pak assay procedure and quality surveillance has been implemented. In other departments (e.g., general outpatient department [OPD]) or settings (e.g., prenatal consultation at the maternity ward), the Chagas Stat-Pak assay is performed on serum samples in the parasitology lab in parallel with a commercial ELISA. In the case of discordant results, serum samples are sent to the Swiss Tropical and Public Health Institute where two other serological tests are available (immunofluorescence [IF] and in-house ELISA).
In conclusion, the Chagas Stat-Pak RDT proved to be an accurate diagnostic test for T. cruzi infection in a cohort of adult Latin-American migrants living in Geneva, Switzerland, leading to improved access to diagnosis and care. The sensitivity of the test could be further improved, or another Chagas RDT with higher sensitivity could be used in parallel. A few other commercial serological RDTs have been evaluated, although less extensively than the Chagas Stat-Pak RDT, with promising results (4, 10, 21). A multicentric evaluation of several Chagas RDTs is planned by the WHO. Accurate RDTs for Chagas' disease have a huge potential to improve access to diagnosis and care for this neglected disease both in countries where Chagas' disease is endemic and in countries where this disease is not endemic.
Acknowledgments
This work was supported by the Foundation Simon I. Patino, the World Health Organization, the Geneva University Hospitals, and the Faculty of Medicine of the University of Geneva. The authors declare no conflict of interests.
bioMérieux Switzerland and Ruwag Switzerland donated the reference serological tests.
Footnotes
Published ahead of print on 16 June 2010.
REFERENCES
- 1.Altcheh, J., M. Biancardi, A. Lapena, G. Ballering, and H. Freilij. 2005. Congenital Chagas disease: experience in the Hospital de Ninos, Ricardo Gutierrez, Buenos Aires, Argentina. Rev. Soc. Bras. Med. Trop. 38(Suppl. 2):41-45. (In Spanish.) [PubMed] [Google Scholar]
- 2.Bern, C., S. P. Montgomery, B. L. Herwaldt, A. Rassi, Jr., J. A. Marin-Neto, R. O. Dantas, J. H. Maguire, H. Acquatella, C. Morillo, L. V. Kirchhoff, R. H. Gilman, P. A. Reyes, R. Salvatella, and A. C. Moore. 2007. Evaluation and treatment of Chagas disease in the United States: a systematic review. JAMA 298:2171-2181. [DOI] [PubMed] [Google Scholar]
- 3.Chippaux, J. P., J. A. Santalla, J. R. Postigo, M. Romero, N. A. Salas Clavijo, D. Schneider, and L. Brutus. 2009. Sensitivity and specificity of Chagas Stat-Pak(R) test in Bolivia. Trop. Med. Int. Health 14:732-735. [DOI] [PubMed] [Google Scholar]
- 4.Flores-Chavez, M., I. Cruz, M. Rodriguez, J. Nieto, E. Franco, T. Garate, and C. Canavate. 2010. Comparison of conventional and non-conventional serological tests for the diagnosis of imported Chagas disease in Spain. Enferm. Infecc. Microbiol. Clin. 28:284-293. (In Spanish.) [DOI] [PubMed] [Google Scholar]
- 5.Garcia, A. L., R. Parrado, E. Rojas, R. Delgado, J.-C. Dujardin, and R. Reithinger. 2009. Leishmaniasis in Bolivia: comprehensive review and current status. Am. J. Trop. Med. Hyg. 80:704-711. [PubMed] [Google Scholar]
- 6.Guerri-Guttenberg, R. A., D. R. Grana, G. Ambrosio, and J. Milei. 2008. Chagas cardiomyopathy: Europe is not spared! Eur. Heart J. 29:2587-2591. [DOI] [PubMed] [Google Scholar]
- 7.Jackson, Y., F. Chappuis, and L. Loutan. 2008. Chagas disease in Switzerland: managing an emerging infection and interrupting its transmission. Rev. Med. Suisse 4:1212-1217. (In French.) [PubMed] [Google Scholar]
- 8.Jackson, Y., L. Getaz, H. Wolff, M. Holst, A. Mauris, A. Tardin, J. Sztajzel, V. Besse, L. Loutan, J. M. Gaspoz, J. Jannin, P. Albajar Vinas, A. Luquetti, and F. Chappuis. 2010.Prevalence, clinical staging and risk for blood-borne transmission of Chagas disease among Latin American migrants in Geneva, Switzerland. PLoS Negl. Trop. Dis. 4:e592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson, Y., C. Myers, A. Diana, H. P. Marti, H. Wolff, F. Chappuis, L. Loutan, and A. Gervaix. 2009. Congenital transmission of Chagas disease in Latin American immigrants in Switzerland. Emerg. Infect. Dis. 15:601-603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ji, M. J., J. S. Noh, B. K. Cho, Y. S. Cho, S. J. Kim, and B. S. Yoon. 2009. Evaluation of SD BIOLINE Chagas Ab Rapid kit. Korean J. Lab. Med. 29:48-52. (In Korean.) [DOI] [PubMed] [Google Scholar]
- 11.Landis, J. R., and G. G. Koch. 1977. The measurement of observer agreement for categorical data. Biometrics 33:159-174. [PubMed] [Google Scholar]
- 12.Luquetti, A. O., C. Ponce, E. Ponce, J. Esfandiari, A. Schijman, S. Revollo, N. Anez, B. Zingales, R. Ramgel-Aldao, A. Gonzalez, M. J. Levin, E. S. Umezawa, and J. Franco da Silveira. 2003. Chagas' disease diagnosis: a multicentric evaluation of Chagas Stat-Pak, a rapid immunochromatographic assay with recombinant proteins of Trypanosoma cruzi. Diagn. Microbiol. Infect. Dis. 46:265-271. [DOI] [PubMed] [Google Scholar]
- 13.Médecins sans Frontières and Campaign for Access to Essential Medicines. 2008. International meeting: new diagnostic tests are urgently needed to treat patients with Chagas disease. Rev. Soc. Bras. Med. Trop. 41:315-319. [DOI] [PubMed] [Google Scholar]
- 14.Otani, M. M., E. Vinelli, L. V. Kirchhoff, A. del Pozo, A. Sands, G. Vercauteren, and E. C. Sabino. 2009. WHO comparative evaluation of serologic assays for Chagas disease. Transfusion 49:1076-1082. [DOI] [PubMed] [Google Scholar]
- 15.Pan American Health Organization. 2006. Quantitative estimation of Chagas disease in the Americas. OPS/HDM/CD/425-06. Pan American Health Organization, Washington, DC. (In Spanish.)
- 16.Pérez de Ayala, A., J.-A. Pérez-Molina, F. Norman, and R. Lopez-Vélez. 2009. Chagasic cardiomyopathy in immigrants from Latin America to Spain. Emerg. Infect. Dis. 15:607-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ponce, C., E. Ponce, E. Vinelli, A. Montoya, V. de Aguilar, A. Gonzalez, B. Zingales, R. Rangel-Aldao, M. J. Levin, J. Esfandiari, E. S. Umezawa, A. O. Luquetti, and J. F. da Silveira. 2005. Validation of a rapid and reliable test for diagnosis of Chagas' disease by detection of Trypanosoma cruzi-specific antibodies in blood of donors and patients in Central America. J. Clin. Microbiol. 43:5065-5068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roddy, P., J. Goiri, L. Flevaud, P. P. Palma, S. Morote, N. Lima, L. Villa, F. Torrico, and P. Albajar-Vinas. 2008. Field evaluation of a rapid immunochromatographic assay for detection of Trypanosoma cruzi infection by use of whole blood. J. Clin. Microbiol. 46:2022-2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmunis, G. A. 2007. Epidemiology of Chagas disease in non-endemic countries: the role of international migration. Mem. Inst. Oswaldo Cruz 102(Suppl. 1):75-85. [DOI] [PubMed] [Google Scholar]
- 20.Sosa-Estani, S., M. R. Gamboa-Leon, J. Del Cid-Lemus, F. Althabe, J. Alger, O. Almendares, M. L. Cafferata, J. P. Chippaux, E. Dumonteil, L. Gibbons, N. Padilla-Raygoza, D. Schneider, J. M. Belizan, and P. Buekens. 2008. Use of a rapid test on umbilical cord blood to screen for Trypanosoma cruzi infection in pregnant women in Argentina, Bolivia, Honduras, and Mexico. Am. J. Trop. Med. Hyg. 79:755-759. [PubMed] [Google Scholar]
- 21.Verani, J. R., A. Seitz, R. H. Gilman, C. LaFuente, G. Galdos-Cardenas, V. Kawai, E. de LaFuente, L. Ferrufino, N. M. Bowman, V. Pinedo-Cancino, M. Z. Levy, F. Steurer, C. W. Todd, L. V. Kirchhoff, L. Cabrera, M. Verastegui, and C. Bern. 2009. Geographic variation in the sensitivity of recombinant antigen-based rapid tests for chronic Trypanosoma cruzi infection. Am. J. Trop. Med. Hyg. 80:410-415. [PubMed] [Google Scholar]
- 22.Viotti, R., C. Vigliano, B. Lococo, G. Bertocchi, M. Petti, M. G. Alvarez, M. Postan, and A. Armenti. 2006. Long-term cardiac outcomes of treating chronic Chagas disease with benznidazole versus no treatment: a nonrandomized trial. Ann. Intern. Med. 144:724-734. [DOI] [PubMed] [Google Scholar]