Abstract
Forty-four of 48 Burkholderia cepacia complex strains cultured from Danish cystic fibrosis patients were Burkholderia multivorans, a distribution of species that has not been reported before. Although cases of cross infections were demonstrated, no major epidemic clone was found. The species distribution may represent the sporadic acquisition of bacteria from the environment.
Burkholderia cepacia and related bacteria have emerged as significant pathogens in cystic fibrosis (CF) patients due to the risk of cepacia syndrome (a fatal necrotizing pneumonia with bacteremia), the organism's innate multiresistance to antibiotics, and the transmissibility of bacterial strains between patients by social contact (10, 15). The genus Burkholderia encompasses more than 50 validly published species that can be divided into four groups (21). Strains colonizing the respiratory tract of CF patients are predominantly members of the B. cepacia complex (BCC), with 17 formally named species (23). Chronic infections typically involve a single strain, although strain displacements have been demonstrated (24).
Most or all species of the BCC can colonize the lower airways of CF patients, although some of them are infrequently demonstrated. Studies from North America, Europe, and Australasia have shown that Burkholderia cenocepacia is the dominant species being recovered from 46 to 90% of colonized patients (4, 6, 13, 17, 19, 20). Different situations have been described in Lisbon, where contamination of saline solutions used in inhalant therapy by CF patients has resulted in a predominance of B. cepacia (5), and in France, where a small excess of B. multivorans (52%) over B. cenocepacia (45%) has been reported (3).
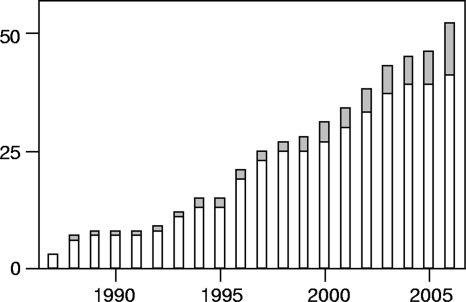
Danish CF patients are treated in two centers, and respiratory cultures are routinely performed at the monthly visit to the outpatient clinic. Four hundred thirty-one patients were alive by 1 January 2007, and 24 (5.6%) were chronically infected with BCC species. A chronic infection was defined as the isolation of BCC bacteria from more than half of sputum cultures for more than 6 months (modified “Leeds criteria” for chronic Pseudomonas aeruginosa infection [14]), and/or the development of ≥2 precipitins measured by crossed immunoelectrophoresis (18). A total of 52 Danish CF patients are known to have been intermittently (n = 11) or chronically (n = 41) infected with BCC bacteria (Fig. 1). Intermittently colonized patients may be underrepresented in data from before the routine use of colistin-containing selective agar plates (9), and some of the recent BCC acquisitions may be reclassified as chronic infections with time. In retrospect, the first Danish patient was chronically infected with BCC in the late 1970s (18), but few cases were identified until 1990. The increased rate of BCC colonization after 1990 may be secondary to the widespread use of inhaled colistin for P. aeruginosa infection, which was introduced in the 1980s (11). Since 1993, the rate has stabilized at around three new cases per year (43 BCC acquisitions during 14 years) (Fig. 1). In the same time period, 174 Danish patients have been diagnosed with CF (on average, 12.4 ± 4.4 [mean ± standard deviation] new patients per year; range, 6 to 22).
FIG. 1.
Cumulative numbers of Danish CF patients experiencing a first-time isolation of BCC bacteria, separated by status (open bars, chronic infections; gray bars, intermittent colonizations).
BCC isolates from 9 intermittently colonized and 39 chronically infected patients were available for characterization. One isolate per patient, cultured between 1994 and 2006, was included in the study. Allocation to species within the BCC was performed by partial atpD and recA sequencing (1); occasional isolates with no PCR product from either amplification were subjected to partial sequencing of fur (16). Two independent sequence-based identifications were thus obtained for all BCC isolates. Only three species were identified in Danish patients, and B. multivorans accounted for more than 90% of the isolates (Table 1). Pulsed-field gel electrophoresis (PFGE) genotypes were assessed after digestion with Xba and SpeI and interpreted as described previously (22). Thirty-eight BCC genotypes were disclosed by both enzymes, and five of the genotypes were identified in more than one patient (two to four patients). Some of these small clusters were epidemiologically related and probably reflect cases of cross infections. Two pairs of siblings each carried the same strain, and one additional patient harbored the same genotype as the two siblings treated in that CF center. Between 1994 and 2003, chronic infections with BCC of a single genotype were established in 4 patients treated in one center. A fourth cluster was composed of patients treated at both of the two Danish CF centers; a possible epidemiological relationship between these three patients was unknown. No patient-to-patient transmission could have occurred in the fifth cluster, where the same genotype was intermittently detected in two patients in 1994 and 1999, respectively, and established a chronic infection in a third patient in 2005. All BCC genotypes identified in more than one patient were B. multivorans.
TABLE 1.
Specific identification of 48 BCC strains isolated from Danish CF patients
| Species | No. of strains from patients in whom colonization was: |
Total (%) | |
|---|---|---|---|
| Intermittent | Chronic | ||
| B. multivorans | 8 | 36 | 44 (92) |
| B. cenocepacia | 1 | 2 | 3 (6) |
| B. anthina | 0 | 1 | 1 (2) |
The marked preponderance of B. multivorans in Danish CF patients was unexpected. Although frequently identified in samples from this group of patients, the species is considered second to B. cenocepacia as the major Burkholderia pathogen in CF patients. The unusual species distribution could not be attributed to cross infections. Genotyping of strains clearly indicated that most isolates were unique and that suspected cases of person-to-person transmission beyond siblings were restricted to a few cases. A pathogenic role of P. aeruginosa was suspected at the Copenhagen CF center by 1974, and segregation policies with respect to this bacterium were effective by 1981 (12). It is possible that the early attention to Gram-negative nonfermenters, with a focus on hygienic precautions and segregation, may be responsible for the limited spread of BCC bacteria among Danish CF patients.
The transmission of microorganisms between patients can be documented and to some degree controlled, while sporadic acquisition of BCC from the environment is less amenable to control. The demonstration of identical genotypes in intermittently colonized patients separated by a time span of 5 years is conspicuous; the acquisition of the same genotype by these patients may have involved a common but unidentified source. Instances of isolation and typing of BCC from the proximate environment of CF patients are sparse, but indistinguishable environmental and clinical strains have been reported (2). The prevalence of chronic BCC infections in Denmark (5.6%) is higher than in neighboring countries (7). Exposure to BCC may vary with climate, place of residence, and occupation. Little scientific evidence is available to suggest restrictions in the patient's contacts with soil, crops, or nature, and consensus guidelines have not been issued.
Given the limited number of cross infections among Danish CF patients, the species distribution must reflect the sporadic acquisition of BCC bacteria from the environment. The marked contrast to reports from other CF centers could result from exposure to different pools of environmental bacteria determined by local physical conditions. However, the predominance of B. cenocepacia in many clinics may also be explained by the introduction of epidemic clones of this species, which has spread widely within and between clinics. Since the introduction of segregation policies in the United Kingdom, a shift toward B. multivorans has been observed (8). A similar change in the relative frequencies of infecting species has been reported for strains being referred to the North American B. cepacia Repository at the University of Michigan, Ann Arbor (19).
Acknowledgments
This work was supported by a grant from the Danish Cystic Fibrosis Foundation to N.N.-L.
Footnotes
Published ahead of print on 2 June 2010.
REFERENCES
- 1.Baldwin, A., E. Mahenthiralingam, K. M. Thickett, D. Honeybourne, M. C. Maiden, J. R. Govan, D. P. Speert, J. J. Lipuma, P. Vandamme, and C. G. Dowson. 2005. Multilocus sequence typing scheme that provides both species and strain differentiation for the Burkholderia cepacia complex. J. Clin. Microbiol. 43:4665-4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baldwin, A., E. Mahenthiralingam, P. Drevinek, P. Vandamme, J. R. Govan, D. J. Waine, J. J. LiPuma, L. Chiarini, C. Dalmastri, D. A. Henry, D. P. Speert, D. Honeybourne, M. C. Maiden, and C. G. Dowson. 2007. Environmental Burkholderia cepacia complex isolates in human infections. Emerg. Infect. Dis. 13:458-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brisse, S., C. Cordevant, P. Vandamme, P. Bidet, C. Loukil, G. Chabanon, M. Lange, and E. Bingen. 2004. Species distribution and ribotype diversity of Burkholderia cepacia complex isolates from French patients with cystic fibrosis. J. Clin. Microbiol. 42:4824-4827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campana, S., G. Taccetti, N. Ravenni, F. Favari, L. Cariani, A. Sciacca, D. Savoia, A. Collura, E. Fiscarelli, G. De Intinis, M. Busetti, A. Cipolloni, A. d'Aprile, E. Provenzano, I. Collebrusco, P. Frontini, G. Stassi, M. Trancassini, D. Tovagliari, A. Lavitola, C. J. Doherty, T. Coenye, J. R. Govan, and P. Vandamme. 2005. Transmission of Burkholderia cepacia complex: evidence for new epidemic clones infecting cystic fibrosis patients in Italy. J. Clin. Microbiol. 43:5136-5142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunha, M. V., A. Pinto-de-Oliveira, L. Meirinhos-Soares, M. J. Salgado, J. Melo-Cristino, S. Correia, C. Barreto, and I. Sá-Correia. 2007. Exceptionally high representation of Burkholderia cepacia among B. cepacia complex isolates recovered from the major Portuguese cystic fibrosis center. J. Clin. Microbiol. 45:1628-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drevinek, P., O. Cinek, J. Melter, L. Langsadl, Y. Navesnakova, and V. Vavrova. 2003. Genomovar distribution of the Burkholderia cepacia complex differs significantly between Czech and Slovak patients with cystic fibrosis. J. Med. Microbiol. 52:603-604. [DOI] [PubMed] [Google Scholar]
- 7.European Cystic Fibrosis Society. 2009. European cystic fibrosis registry report 2006 data. http://www.ecfs.eu/files/webfm/webfiles/File/ecfs_registry/ECFRreportA2006.pdf.
- 8.France, M. W., M. E. Dodd, J. R. Govan, C. J. Doherty, A. K. Webb, and A. M. Jones. 2008. The changing epidemiology of Burkholderia species infection at an adult cystic fibrosis centre. J. Cyst. Fibros. 7:368-372. [DOI] [PubMed] [Google Scholar]
- 9.Henry, D. A., M. E. Campbell, J. J. LiPuma, and D. P. Speert. 1997. Identification of Burkholderia cepacia isolates from patients with cystic fibrosis and use of a simple new selective medium. J. Clin. Microbiol. 35:614-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isles, A., I. Maclusky, M. Corey, R. Gold, C. Prober, P. Fleming, and H. Levison. 1984. Pseudomonas cepacia infection in cystic fibrosis: an emerging problem. J. Pediatr. 104:206-210. [DOI] [PubMed] [Google Scholar]
- 11.Jensen, T., S. S. Pedersen, S. Garne, C. Heilmann, N. Høiby, and C. Koch. 1987. Colistin inhalation therapy in cystic fibrosis patients with chronic Pseudomonas aeruginosa lung infection. J. Antimicrob. Chemother. 19:831-838. [DOI] [PubMed] [Google Scholar]
- 12.Jørgensen, I. M., H. K. Johansen, B. Frederiksen, T. Pressler, A. Hansen, P. Vandamme, N. Høiby, and C. Koch. 2003. Epidemic spread of Pandoraea apista, a new pathogen causing severe lung disease in cystic fibrosis patients. Pediatr. Pulmonol. 36:439-446. [DOI] [PubMed] [Google Scholar]
- 13.Kidd, T. J., J. M. Douglas, H. A. Bergh, C. Coulter, and S. C. Bell. 2008. Burkholderia cepacia complex epidemiology in persons with cystic fibrosis from Australia and New Zealand. Res. Microbiol. 159:194-199. [DOI] [PubMed] [Google Scholar]
- 14.Lee, T. W., K. G. Brownlee, S. P. Conway, M. Denton, and J. M. Littlewood. 2003. Evaluation of a new definition for chronic Pseudomonas aeruginosa infection in cystic fibrosis patients. J. Cyst. Fibros. 2:29-34. [DOI] [PubMed] [Google Scholar]
- 15.LiPuma, J. J., S. E. Dasen, D. W. Nielson, R. C. Stern, and T. L. Stull. 1990. Person-to-person transmission of Pseudomonas cepacia between patients with cystic fibrosis. Lancet 336:1094-1096. [DOI] [PubMed] [Google Scholar]
- 16.Lynch, K. H., and J. J. Dennis. 2008. Development of a species-specific fur gene-based method for identification of the Burkholderia cepacia complex. J. Clin. Microbiol. 46:447-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDowell, A., E. Mahenthiralingam, K. E. Dunbar, J. E. Moore, M. Crowe, and J. S. Elborn. 2004. Epidemiology of Burkholderia cepacia complex species recovered from cystic fibrosis patients: issues related to patient segregation. J. Med. Microbiol. 53:663-668. [DOI] [PubMed] [Google Scholar]
- 18.Nir, M., H. K. Johansen, and N. Høiby. 1992. Low incidence of pulmonary Pseudomonas cepacia infection in Danish cystic fibrosis patients. Acta Paediatr. 81:1042-1043. [DOI] [PubMed] [Google Scholar]
- 19.Reik, R., T. Spilker, and J. J. Lipuma. 2005. Distribution of Burkholderia cepacia complex species among isolates recovered from persons with or without cystic fibrosis. J. Clin. Microbiol. 43:2926-2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Speert, D. P., D. Henry, P. Vandamme, M. Corey, and E. Mahenthiralingam. 2002. Epidemiology of Burkholderia cepacia complex in patients with cystic fibrosis, Canada. Emerg. Infect. Dis. 8:181-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tayeb, L. A., M. Lefevre, V. Passet, L. Diancourt, S. Brisse, and P. A. Grimont. 2008. Comparative phylogenies of Burkholderia, Ralstonia, Comamonas, Brevundimonas and related organisms derived from rpoB, gyrB and rrs gene sequences. Res. Microbiol. 159:169-177. [DOI] [PubMed] [Google Scholar]
- 22.Tenover, F. C., R. D. Arbeit, R. V. Goering, P. A. Mickelsen, B. E. Murray, D. H. Persing, and B. Swaminathan. 1995. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vanlaere, E., A. Baldwin, D. Gevers, D. Henry, E. De Brandt, J. J. LiPuma, E. Mahenthiralingam, D. P. Speert, C. Dowson, and P. Vandamme. 2009. Taxon K, a complex within the Burkholderia cepacia complex, comprises at least two novel species, Burkholderia contaminans sp. nov. and Burkholderia lata sp. nov. Int. J. Syst. Evol. Microbiol. 59:102-111. [DOI] [PubMed] [Google Scholar]
- 24.Yang, J. H., T. Spilker, and J. J. LiPuma. 2006. Simultaneous coinfection by multiple strains during Burkholderia cepacia complex infection in cystic fibrosis. Diagn. Microbiol. Infect. Dis. 54:95-98. [DOI] [PubMed] [Google Scholar]