Abstract
Rates of teenage pregnancy and parenthood in the United States remain high. Although many consequences of teenage parenthood have been well studied, little prospective research has examined its effect on mental health. This study aims to better understand the impact of teenage parenthood on mental health and to determine whether sex modifies this relation. Using data from the National Longitudinal Survey of Youth, 1997 (1997–2006), and a matched cohort design, the authors compared changes in the mental health of parenting teenagers and nonparenting teenagers over 6 years of follow-up with mixed-effects regression. The results indicate that mental health improved for all teenagers over 6 years of follow-up. Furthermore, overall, teenage parenthood was not associated with changes in mental health; however, sex modified this relation. Although the mental health of teenage fathers improved at a faster rate compared with nonparenting teenage males, teenage mothers improved at a slower rate compared with nonparenting teenage females. Psychological health has important implications for both the teenage parent and the child. Future studies should aim to better understand the mechanisms through which teenage parenthood impacts mental health among both males and females, and interventions should be developed to ensure mental health among young parents.
Keywords: adolescent, mental health, parents
Despite significant declines, the rates of teenage pregnancy and parenthood continue to be high in the United States (1–3). In 2006, the rates of livebirths were 41.9 per 1,000 for women and 17.7 per 1,000 for men aged 15–19, yielding more than 430,000 livebirths (3). Teenage parents often have more limited educational attainment, marital instability, and restricted economic opportunities compared with their peers who delay childbearing (4–7).
Although research has consistently documented increased risk for teenage pregnancy and parenthood among teens with worse mental health (8–10), less is known about the impact of teenage parenthood on mental health trajectories. Studies comparing younger mothers with older mothers (11, 12) may neglect to address whether worse psychological functioning is an artifact of adolescence, not young motherhood. Only a few studies have examined the changes in mental health among young parents and their childless peers, with inconsistent results. In a cross-sectional study, Mirowsky and Ross (13) found that early age at first birth was associated with greater depression among males and females. Conversely, using data from the National Longitudinal Study of Adolescent Health, Booth et al. (14) found no differences in changes in depressive symptomology for parents compared with nonparents among adolescent males and females. Similarly, Mollborn and Morningstar (15) found that teenage parenthood was not associated with changes in distress levels among females when comparing teenage parents with their childless peers and older mothers.
Understanding the relation between parenthood and mental health is particularly important given that parental mental health is integral to effective parenting (16–20). Particularly among mothers, mental health is associated with poorer adaptive skills, delayed language, and social and emotional development for the child (21–24). Limited research among fathers suggests that their psychological health may be equally important and that psychological distress may inhibit involvement (25–28).
The current literature highlights the need to more fully understand the impact of teenage parenthood on mental health, particularly among young males (6, 7, 29). This study aims to add to limited research to better understand the effect of teenage parenthood on mental health trajectories and to determine whether there are sex differentials in this relation using a contemporary and diverse sample of teenagers in the United States.
MATERIALS AND METHODS
Participants and procedures
Data for this study came from the National Longitudinal Survey of Youth, 1997 (NLSY97). This longitudinal, nationally representative (plus an oversample of racial minorities) survey included 8,984 US youths aged 12–16 years on December 31, 1996. The youth and his/her parent each completed an interview lasting approximately 1 hour. Youths were interviewed annually. Further details on the NLSY97 procedures can be found at the website, http://www.nlsinfo.org/nlsy97/97guide/chap2.htm.
Although 11 rounds of data are currently available (1997–2007), mental health measures were assessed only in rounds 4, 6, 8, and 10 (2000, 2002, 2004, and 2006). Therefore, in order to be eligible for this analysis, NLSY97 participants had to be a teenager in 2000, to have been interviewed in 2000 or 2002, and to have been childless at the time of this interview. In addition, because the outcome of interest was the trajectory in mental health status from pre- to postbirth, we needed to establish the timing of the assessments in relation to the birth. We defined the interview at which mental health status was assessed immediately prior to the birth as year 0 and subsequent interviews after the birth of a child as years 2–6, corresponding to the number of years since year 0. Finally, sociodemographic covariates were assessed at round 1 (collected in 1997–1998), which we refer to as “baseline.”
Because year 0 was defined as the interview prior to the birth of the child, this definition was relevant only for the parenting teenagers. Therefore, we matched nonparenting teenagers to parenting teenagers (1:2 or 1:1) on the year of the latter group's prebirth interview in order to define year 0 and subsequent follow-up years for nonparenting teenagers and to ensure equivalence in the year interviewed. To aid in controlling for confounding, we also matched on age at year 0 (within 6 months) and race/ethnicity, stratified by sex. Nonparenting teenagers were assigned the same year 0 interview year (2000 or 2002) as their matched parenting teenagers.
As previously stated, 8,984 adolescents were interviewed at baseline. This analysis was restricted to those who were less than 20 years of age in 2000 in order to ensure that participants had the opportunity to become teenage parents after the first available mental health measure (n = 7,388). Participants reporting mixed race were excluded because they could not be reclassified (n = 69). Participants who were already parents by the 2000 interview (n = 499) were also excluded.
Participants were also excluded if they did not complete interviews at year 0 (n = 57 parenting teenagers) or did not have valid mental health measures at year 0 (n = 4 parenting teenagers and 4 nonparenting teenagers). Participants who did not have any follow-up interview with a valid mental health score (n = 1 parenting teenager and 42 nonparenting teenagers) were excluded. After exclusion of these nonparenting teenagers, 1 parenting teenager had no matches; as a result, this individual was removed from the sample. Additionally, the 2 nonparenting teenagers matched to the excluded parenting teenager were removed from the sample.
These exclusions resulted in a final sample of 178 teenage fathers matched to 330 nonparenting teenage males and 314 teenage mothers matched to 604 nonparenting teenage females for an overall sample of 492 teenage parents and 934 nonparenting teenagers.
Measures
Primary outcome measure.
Mental health status was assessed by using a scale adapted from the frequently used, well-validated, and reliable mental health inventory subscale (MHI-5) of the Short Form 36 (SF-36) instrument, which is designed to assess depression and anxiety (30–34). Its sensitivity and specificity for detecting clinical depression have been shown to be high, and it has been shown to perform well in criterion-based tests of validity, with low-scoring subjects needing psychiatric care more frequently (34). Example questions included how much time in the last month “have you been a very nervous person” and “felt calm and peaceful?” Responses were measured on a 4-point scale, ranging from all of the time (0 points) to none of the time (3 points), and summed. Scores ranged from 0 to 15, with higher scores indicating more positive mental health (α = 0.76).
Primary exposure measure.
Age at first birth was calculated as the difference between the participant's date of birth and his/her first biologic child's date of birth. Teenage parenthood was characterized by being less than 20 years of age at the birth of the first child.
Covariates.
Individual, family, and contextual variables were included as covariates in the multivariate analysis to account for potential early predictors of teenage parenthood and mental health (35, 36).
Individual.
Participants self-reported on sex and race/ethnicity, which was categorized as white/other, black non-Hispanic, and Hispanic. Additionally, they reported their date of birth from which age at baseline was calculated.
Family.
Percent of poverty level was determined by dividing the total household income by the federal poverty level (which accounts for household size) for the previous year and multiplying by 100%. A value of 100% indicates that the household income is equal to the poverty level, a value of less than 100% indicates a household income less than the poverty level, and a value of greater than 100% indicates a household income greater than the poverty level. Maternal and paternal education were reported by the parents of the participants and dichotomized into less than 12 or 12 years or more. Parents also indicated whether or not the participant lived in 1 home with both biologic parents at age 2. The number of children in the home represented the total number of people less than 18 years of age who shared a home with the participant at baseline. To measure maternal and paternal monitoring, participants responded to 4 items (e.g., how much does he/she know about your close friends) on a 5-point scale. Scores could range from 0 to 16, with higher scores indicating more monitoring (α = 0.68 and 0.81, respectively) (37). Parental monitoring was determined by the highest score for either maternal or paternal monitoring. Finally, maternal and paternal relationship quality was assessed by asking participants about their relationship with their residential mother and father by use of 8 questions each (e.g., I think highly of him/her, how often does she criticize you or your ideas) with responses measured on a 5-point scale. Scores could range from 0 to 32, with higher scores indicating a more positive relationship (37). Parental relationship quality was determined by the highest score for either maternal or paternal relationship quality (α = 0.73 and 0.82, respectively).
Contextual.
To assess academic achievement, the original surveyors administered the math subtest of the Peabody Individual Achievement Test (PIAT) to participants. Scores were then normalized, and percentiles ranging from 0 to 100 were calculated (37). Residential location was measured according to whether the participant's place of residence was urban, rural, or unknown based on census definitions. The unknown category (n = 50) was assigned to participants whose zipcode includes both urban and rural areas or whose residence cannot be identified. We dichotomized into urban and not urban (37).
Additionally, in order to account for differences of when baseline interviews were conducted, we assessed the difference in months between the baseline interview and the year 0 interview.
Statistical analysis
Bivariate associations between individual, family, and contextual characteristics and teenage parenthood stratified by sex were assessed by using chi-square tests and t tests. The mean mental health scores at each timepoint were calculated, and bivariate associations with teenage parenthood stratified by sex were assessed by use of t tests. In order to examine the effect of teenage parenthood on mental health scores over time, a series of mixed-effects models was developed. These models allow for incomplete data across timepoints, thus reducing bias introduced by excluding individuals with incomplete data (38). We developed 3-level random intercepts-only models with an unstructured covariance structure to account for dependence resulting from interviews (level 1) being nested within individuals (level 2) and individuals being nested within matched sets (level 3). In multivariate models, all baseline covariates were included and treated as time unvarying.
First, a model was developed with an interaction between teenage parenthood and year of follow-up to determine whether changes in mental health scores differed for teenage parents compared with nonparenting teenagers, after controlling for baseline sociodemographic characteristics. Second, a 3-way interaction among sex, teenage parenthood, and year of follow-up was added to examine whether there were sex differences in the effect of teenage parenthood on mental health trajectories. Next, we tested for quadratic and cubic time effects to characterize the functional form of the mental health trajectories. Finally, a sex-stratified analysis was conducted to further describe these relations. For all models, the year of follow-up effect was treated as years of follow-up since year 0 and can be interpreted as the effect of a 1-year increase on mental health.
A number of covariates had a substantial amount of missing data. Specifically, 26.9% (n = 384) were missing for percent of poverty level, 23.6% (n = 337) for paternal education, 6.7% (n = 95) for maternal education, 12.2% (n = 174) for biologic parents in the home, 10.4% (n = 148) for parental monitoring, and 9.5% (n = 136) for parental relationship quality and PIAT score. Rather than excluding variables or individuals with incomplete data, which assumes that data are missing completely at random, we performed multiple imputation using a Markov Chain Monte Carlo procedure to determine values for missing data and to estimate unbiased parameters and standard errors (39–41) using available sociodemographic characteristics (i.e., nonmissing data on other variables for a given participant and nonmissing data on a given variable for other participants). This assumed that they are missing at random and that values could be predicted by observed data (39, 40, 42). The resulting multiple complete data sets were then analyzed by use of the mixed-effects regression procedures described above. Parameter estimates from each imputed data set were averaged, and standard errors were calculated. For each model, adjusted degrees of freedom were estimated by using 1 of the 5 imputed data sets. The models were not sensitive to choice of degrees of freedom.
Sampling weights were not used because the purpose was to examine the relation between teenage parenthood and mental health trajectories, not to describe nationally representative rates (43).
RESULTS
In this sample, nearly 40% of the respondents were non-Hispanic black and 60% were less than 18 years of age. Approximately 70% of the fathers and mothers of these adolescents had completed high school. Sixty percent of adolescents did not live in a home with both biologic parents at age 2 (Table 1). Teenage parenthood—overall (data not shown) and among males and females—was associated with individual, family, and contextual demographic characteristics (Table 1). Additionally, mental health scores at year 0 differed significantly by sex, age, parental relationship quality, and PIAT score (all P < 0.05) (data not shown). On average, among those who eventually became teenage parents, year 0 mental health scores were measured 349 days prior to the birth of their first child.
Table 1.
Individual, Family, and Contextual Characteristics, Overall and by Teenage Parenthood Stratified by Sex, National Longitudinal Survey of Youth, 1997
| Measure | Overall (N = 1,426)a | Teen Mother (n = 314)a | Nonparenting Teen Female (n = 604)a | P Value | Teen Father (n = 178)a | Nonparenting Teen Male (n = 330)a | P Value | ||||||||||
| No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | |||
| Raceb | 0.978 | 0.950 | |||||||||||||||
| Nonblack/non-Hispanic | 487 | 34.1 | 116 | 36.9 | 219 | 36.3 | 52 | 29.2 | 100 | 30.3 | |||||||
| Non-Hispanic black | 553 | 38.8 | 108 | 34.4 | 211 | 34.9 | 82 | 46.1 | 152 | 46.1 | |||||||
| Hispanic | 386 | 27.1 | 90 | 28.7 | 174 | 28.8 | 44 | 24.7 | 78 | 23.6 | |||||||
| Age at year 0b | 0.705 | 0.905 | |||||||||||||||
| 18 years or older | 578 | 40.5 | 129 | 41.1 | 256 | 42.4 | 67 | 37.6 | 126 | 38.2 | |||||||
| Less than 18 years | 848 | 59.5 | 185 | 59.9 | 348 | 57.6 | 111 | 62.4 | 204 | 61.8 | |||||||
| Percent of poverty level | 237.2 (238.2) | 165.9 (137.1) | 278.9 (272.4) | <0.001 | 165.8 (137.6) | 265.1 (263.5) | <0.001 | ||||||||||
| Paternal education | <0.001 | <0.001 | |||||||||||||||
| High school or more | 792 | 72.7 | 136 | 60.4 | 395 | 80.1 | 70 | 57.4 | 191 | 76.7 | |||||||
| Less than high school | 297 | 27.3 | 89 | 39.6 | 98 | 19.9 | 52 | 42.6 | 58 | 23.3 | |||||||
| Maternal education | <0.001 | ||||||||||||||||
| High school or more | 936 | 70.3 | 168 | 57.9 | 443 | 76.8 | 97 | 61.0 | 228 | 74.7 | |||||||
| Less than high school | 395 | 29.7 | 122 | 42.1 | 134 | 23.2 | 62 | 39.0 | 77 | 25.3 | 0.002 | ||||||
| Both biologic parents in home (age 2) | <0.001 | 0.001 | |||||||||||||||
| Yes | 499 | 39.9 | 84 | 31.2 | 248 | 47.1 | 42 | 26.6 | 125 | 37.9 | |||||||
| No | 753 | 60.1 | 185 | 68.8 | 279 | 52.9 | 116 | 73.4 | 205 | 62.1 | |||||||
| No. of children in home | 0.013 | 0.180 | |||||||||||||||
| 2 or fewer | 768 | 53.9 | 154 | 49.0 | 348 | 57.6 | 86 | 48.3 | 180 | 54.6 | |||||||
| More than 2 | 658 | 46.1 | 160 | 51.0 | 256 | 42.4 | 92 | 51.7 | 150 | 45.4 | |||||||
| Parental monitoring (residential) | 10.4 (3.2) | 10.3 (3.3) | 10.6 (3.1) | 0.261 | 9.8 (3.1) | 10.4 (3.3) | 0.058 | ||||||||||
| Parental relationship quality (residential) | 25.9 (4.6) | 25.2 (4.7) | 26.2 (4.5) | 0.003 | 25.8 (3.9) | 25.9 (4.8) | 0.727 | ||||||||||
| PIAT score, percentile | 34.9 (26.1) | 28.5 (22.5) | 39.2 (27.1) | <0.001 | 28.6 (23.5) | 36.6 (27.0) | 0.001 | ||||||||||
| Residential location | 0.009 | 0.205 | |||||||||||||||
| Urban | 1,119 | 78.5 | 233 | 74.2 | 493 | 81.6 | 132 | 74.2 | 261 | 79.1 | |||||||
| Not urban | 307 | 21.5 | 81 | 25.8 | 111 | 18.4 | 46 | 25.8 | 69 | 20.9 | |||||||
| Difference in months, baseline to year 0 | 51.1 (11.3) | 50.8 (11.3) | 51.0 (11.3) | 0.769 | 51.7 (11.4) | 51.4 (11.4) | 0.743 | ||||||||||
Abbreviations: PIAT, Peabody Individual Achievement Test; SD, standard deviation.
Numbers vary according to the number of missing values for each variable.
Those who were not teenage parents were matched to teenage parents on the basis of age at baseline and race and stratified by sex.
Teenage parenthood and mental health
The average mental health score ranged from 10.00 (standard deviation (SD) = 2.56) at year 0 to 10.44 (SD = 2.52) at year 6 (Table 2). In unadjusted analysis, overall, parenting teenagers had lower mental health scores than nonparenting teenagers at each timepoint (all P < 0.01) (data not shown). However, among females, teenage mothers and nonparenting teenagers had similar mental health scores at year 0 (9.40 vs. 9.67; P = 0.128) but differed at year 2 (9.54 vs. 10.03; P = 0.005), year 4 (9.61 vs. 10.32; P < 0.001), and year 6 (9.86 vs. 10.44; P = 0.007) (Table 2). Conversely, among males, teenage fathers had lower mental health scores than nonparenting teenagers at year 0 (10.31 vs. 10.99; P = 0.004) and year 2 (9.89 vs. 10.71; P < 0.001), but they did not differ at year 4 (10.62 vs. 10.88; P = 0.309) or year 6 (10.80 vs. 10.86; P = 0.837) (Table 2).
Table 2.
Mean Mental Health Score (SD) at Years 0, 2, 4, and 6, Overall and by Teenage Parenthood Stratified by Sex, National Longitudinal Survey of Youth, 1997
| Overall (N = 1,426a) | Teen Mother (n = 314a) | Nonparenting Teen Female (n = 604a) | P Value | Teen Father (n = 178a) | Nonparenting Teen Male (n = 330a) | P Value | |
| Year 0 (n = 1,426) | 10.00 (2.56) | 9.40 (2.58) | 9.67 (2.45) | 0.128 | 10.31 (2.59) | 10.99 (2.43) | 0.004 |
| Year 2 (n = 1,367) | 10.06 (2.52) | 9.54 (2.62) | 10.03 (2.40) | 0.005 | 9.89 (2.87) | 10.71 (2.31) | <0.001 |
| Year 4 (n = 1,300) | 10.32 (2.54) | 9.61 (2.74) | 10.32 (2.35) | <0.001 | 10.62 (2.86) | 10.88 (2.34) | 0.309 |
| Year 6 (n = 911) | 10.44 (2.52) | 9.86 (2.58) | 10.44 (2.40) | 0.007 | 10.80 (2.61) | 10.86 (2.54) | 0.837 |
Abbreviation: SD, standard deviation.
Numbers vary according to the number of missing mental health measures at each timepoint.
In multivariate analysis, on average, mental health scores improved over time, with a one-tenth point increase in mental health score each year of follow-up (estimate = 0.097, standard error (SE) = 0.013; P < 0.001) (data not shown). Overall, changes in mental health scores over time did not differ for parenting teenagers compared with nonparenting teenagers (for teenage parenthood × year interaction, estimate = −0.007, SE = 0.027; P = 0.806) (Table 3). However, after adding interactions for sex, males and females differed in the effect that teenage parenthood had on mental health over time (for teenage parenthood × male × year interaction, estimate = 0.190, SE = 0.055; P < 0.001) (Table 3). Additionally, the form of the mental health trajectories differed by sex (for male × year × year interaction, estimate = 0.035, SE = 0.014; P = 0.016) (Table 3). Specifically, among males, mental health changes were quadratic in nature (P = 0.007); however, the changes among females were not (P = 0.838) (Table 4).
Table 3.
Changes in Mental Health Score at Baseline and at 2-, 4-, and 6-Year Follow-up, National Longitudinal Survey of Youth, 1997a
| Measureb | Teenage Parenthood Model | Sex Interaction Model | Final Model With Quadratic Time Effect | ||||||
| Parameter Estimate | SE | P Value | Parameter Estimate | SE | P Value | Parameter Estimate | SE | P Value | |
| Interceptc | 9.883 | 0.156 | <0.001 | 9.742 | 0.162 | <0.001 | 9.736 | 0.164 | <0.001 |
| Year (0 = year 0, 2 = 2-year follow-up, etc.) | 0.099 | 0.016 | <0.001 | 0.152 | 0.019 | <0.001 | 0.163 | 0.052 | 0.002 |
| Teenage parenthood | −0.414 | 0.130 | 0.001 | −0.226 | 0.161 | 0.163 | −0.225 | 0.161 | 0.163 |
| Male | 0.822 | 0.108 | <0.001 | 1.227 | 0.157 | <0.001 | 1.345 | 0.165 | <0.001 |
| Teenage parenthood × year | −0.007 | 0.027 | 0.806 | −0.073 | 0.033 | 0.025 | −0.073 | 0.033 | 0.025 |
| Male × year | −0.150 | 0.033 | <0.001 | −0.347 | 0.088 | <0.001 | |||
| Teenage parenthood × male | −0.535 | 0.264 | 0.043 | −0.536 | 0.264 | 0.042 | |||
| Teenage parenthood × male × year | 0.190 | 0.055 | <0.001 | 0.191 | 0.055 | <0.001 | |||
| Year × year | −0.002 | 0.008 | 0.816 | ||||||
| Male × year × year | 0.035 | 0.014 | 0.016 | ||||||
| Percent of poverty level | −0.0001 | 0.0003 | 0.691 | −0.0001 | 0.0003 | 0.690 | −0.0001 | 0.0003 | 0.690 |
| Paternal education | 0.029 | 0.116 | 0.846 | 0.031 | 0.148 | 0.833 | 0.031 | 0.148 | 0.835 |
| Maternal education | −0.099 | 0.136 | 0.467 | −0.102 | 0.136 | 0.455 | −0.101 | 0.136 | 0.458 |
| Both biologic parents in home (age 2) | −0.037 | 0.117 | 0.748 | −0.039 | 0.117 | 0.741 | −0.040 | 0.117 | 0.734 |
| No. of children in home | −0.042 | 0.108 | 0.697 | −0.043 | 0.108 | 0.693 | −0.044 | 0.108 | 0.687 |
| Parental monitoring (residential) | 0.020 | 0.019 | 0.295 | 0.020 | 0.019 | 0.297 | 0.020 | 0.019 | 0.298 |
| Parental relationship quality (residential) | 0.034 | 0.014 | 0.016 | 0.034 | 0.014 | 0.016 | 0.034 | 0.014 | 0.016 |
| PIAT score, percentile | 0.004 | 0.002 | 0.063 | 0.004 | 0.002 | 0.069 | 0.004 | 0.002 | 0.067 |
| Residential location | −0.026 | 0.125 | 0.834 | −0.027 | 0.125 | 0.826 | −0.027 | 0.125 | 0.830 |
| Difference in months, baseline to year 0 | 0.007 | 0.005 | 0.140 | 0.007 | 0.005 | 0.141 | 0.008 | 0.005 | 0.107 |
Abbreviations: PIAT, Peabody Individual Achievement Test; SE, standard error.
Values represent unstandardized coefficients.
Percent of poverty level, parental monitoring, parental relationship quality, PIAT score, and difference in months between 1997 baseline interview and year 0 were centered on the grand means.
Intercept is the year 0 mental health score for individuals who do not become teenage parents when all continuous variables are at their grand mean and all categorical variables are equal to 0.
Table 4.
Changes in Mental Health Score, Stratified by Sex, National Longitudinal Survey of Youth, 1997a
| Measureb | Females | Males | ||||
| Parameter Estimate | SE | P Value | Parameter Estimate | SE | P Value | |
| Intercept | 9.668 | 0.189 | <0.001 | 11.196 | 0.269 | <0.001 |
| Year (0 = year 0, 2 = 2-year follow-up, etc.) | 0.162 | 0.051 | 0.002 | −0.182 | 0.072 | 0.012 |
| Year × year | −0.002 | 0.008 | 0.838 | 0.032 | 0.012 | 0.007 |
| Teenage parenthood | −0.189 | 0.163 | 0.248 | −0.809 | 0.217 | <0.001 |
| Teenage parenthood × year | −0.073 | 0.032 | 0.024 | 0.119 | 0.046 | 0.009 |
Abbreviations: PIAT, Peabody Individual Achievement Test; SE, standard error.
Values represent unstandardized coefficients.
Adjusted for percent of poverty level, paternal education, maternal education, both biologic parents in home, number of children in home, parental monitoring, parental relationship quality, PIAT score, residential location, and difference in months between 1997 baseline interview and year 0 interview.
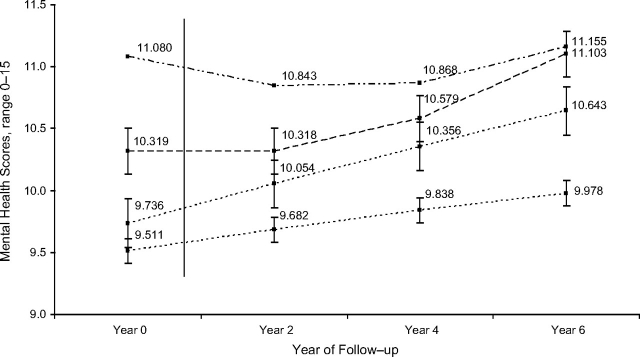
Notably, after adjustment for baseline covariates and the functional form of the trajectories, the modifying effect of sex on the relation between teenage parenthood and mental health trajectories remained (estimate = 0.191, SE = 0.055; P < 0.001) (Table 3). At year 0, males who became teenage fathers had significantly worse mental health scores than males who did not become teenage fathers (adjusted difference = −0.76; P = 0.008) (Figure 1). Over time, the mental health scores of teenage fathers improved, while scores of nonparenting teenage males remained relatively stable (estimate = 0.119, SE = 0.046; P = 0.009) (Table 4). As a result, teenage fathers and nonparenting teenage males had similar scores at 6-year follow-up (adjusted difference = −0.06; P = 0.890) (Figure 1). Conversely, at year 0, females who became teenage mothers had similar mental health scores as females who did not become teenage mothers (adjusted difference = −0.25; P = 0.457) (Figure 1). However, over time, the mental health scores of teenage mothers improved at a slower rate than those of nonparenting teenage females (estimate = −0.073, SE = 0.032; P = 0.024) (Table 4), resulting in larger differences in mental health scores at the 6-year follow-up, with teenage mothers having worse mental health scores (adjusted difference = −0.66; P = 0.016) (Figure 1).
Figure 1.
Adjusted mental health scores at years 0, 2, 4, and 6, stratified by sex and teenage parenthood, National Longitudinal Survey of Youth, 1997. Mental health scores were adjusted for percent of poverty level, paternal education, maternal education, both biologic parents in home, number of children in home, parental monitoring, parental relationship quality, PIAT score, residential location, and difference in months between 1997 baseline interview and year 0 interview. Values for mental health scores represent the average score when all continuous variables are at their grand mean and all categorical variables are equal to 0. Solid vertical line represents the mean time post-year 0 interview when the teenage births occurred (349.49 days post-year 0 interview). PIAT, Peabody Individual Achievement Test. Dashed lines: top, nonparenting teenage males; second, teenage fathers; third, nonparenting teenage females; bottom, teenage mothers.
DISCUSSION
The results of this study indicate that all teenagers had improved mental health over 6 years of follow-up and that, overall, teenage parenthood was not associated with changes in mental health. However, sex modified this relation. Specifically, while the mental health scores of teenage fathers were worse than those of nonparenting teenage males prior to the birth, scores of teenage fathers improved after the birth of a child and scores of nonparenting teenage males remained relatively stable. This resulted in similar scores at the 6-year follow-up. On the other hand, prior to the birth, the mental health scores of teenage mothers and nonparenting teenage females did not differ. Yet, the mental health scores of teenage mothers improved at a slower rate than those of nonparenting teenage females, resulting in larger differences in mental health scores at 6-year follow-up, with teenage mothers having worse mental health scores.
The overall improvement of mental health over time is consistently supported by data that suggest that the mental health of adolescents improves as they transition into adulthood (44, 45). Prior research on the relation between early parenting and mental health trajectories has shown inconsistent results, with no indication of sex differentials (13–15). Our results support the assertion that teenage parenthood does, in fact, impact changes in mental health status over time, but only when stratified by sex. The observed sex differences in mental health trajectories for parenting teenagers compared with nonparenting teenagers may be explained in a number of ways. It is possible that males simply respond to stressful events differently from females (46, 47) and, as a result, teenage parenthood may not have as detrimental an impact on their mental health trajectory. Another possibility might be explained by the different role that young parents play in their children's lives. Specifically, young fathers more often play secondary parenting roles or are more often absent in the lives of their children (5, 29). As a result, for fathers, becoming a teenage parent may have a stabilizing effect. This stabilizing effect may not occur for teenage mothers, as they are more intimately involved with the daily stresses of parenting. A distinct, but related possibility is that, while poor mental health at baseline may in fact affect whether teenage males become fathers, they are then not impacted as severely by their subsequent role of father, and the greater improvement compared with their nonparenting teenage peers is just a “catching up” as they transition to young adulthood. In fact, a secondary analysis, while potentially underpowered, lends tentative support to this premise. When stratified by baseline mental health score (above vs. below the median), the effect of teenage parenting on mental health trajectories disappeared for males but not for females (data not shown).
Strengths and limitations
This study is an important contribution to the literature, as it adds to the limited research on an important public health problem by using a longitudinal study in a large and diverse population of youth, allowing us to assess characteristics from early adolescence and to follow youth into early adulthood. However, our analysis is not without limitations. This study was a secondary data analysis and, as a result, was limited to the available measures. This could lead to misclassification of the outcome variable or covariates, leading to imperfect control for early sociodemographic characteristics. On the other hand, the mental health measure is frequently used and has been shown to be valid and reliable for capturing depression and anxiety. Additionally, data were collected by self-report, which can also lead to misclassification. However, audio-enhanced, computer-assisted self-interviewing was used to minimize bias. The youngest parenting teenagers were excluded from this analysis, because they became parents before the 2000 interview. This may have introduced selection bias; however, a secondary analysis comparing nonparenting teenagers with younger parenting teenagers (≤17 years of age at first birth) indicated that the parameter estimate was only slightly smaller than in the full analysis, suggesting only a slight overestimation of effect. Finally, as previously stated, there were substantial missing data for some covariates. Although multiple imputation was used to reduce the potential bias of a complete-case analysis, the missing-at-random assumption could not be tested and, thus, bias could exist. However, even if the data were not strictly missing at random, this assumption is often reasonable (42).
Significance and implications
Psychological well-being among parents is important for effective parenting and for ensuring healthy child development, particularly for young parents who are already faced with numerous other disadvantages (35, 36). These data have implications for intervention approaches, suggesting that strategies should differentially address young men and women. First, our results suggest that improving mental health among young men may reduce the risk of teenage fatherhood and that interventions should target young men within the first postpartum year in order to promote father involvement and reduce maternal distress (26, 28). Additionally, this study highlights the need for psychological support among young mothers throughout this period as they become accustomed to their new role. Finally, future studies should aim to understand the distinct mechanisms through which teenage parenthood impacts mental health for males and females.
Acknowledgments
Author affiliations: Yale School of Public Health, New Haven, Connecticut (Katie Brooks Biello, Heather L. Sipsma, Trace Kershaw); and Center for Interdisciplinary Research on AIDS, Yale University, New Haven, Connecticut (Katie Brooks Biello, Heather L. Sipsma, Trace Kershaw).
This work was supported by the National Institute of Mental Health at the National Institutes of Health (grant T32MH020031).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Conflict of interest: none declared.
Glossary
Abbreviations
- NLSY97
National Longitudinal Survey of Youth, 1997
- PIAT
Peabody Individual Achievement Test
- SD
standard deviation
- SE
standard error
References
- 1.Darroch JE, Frost JJ, Singh S, et al. Teenage Sexual and Reproductive Behavior in Developed Countries: Can More Progress Be Made? New York, NY: The Alan Guttmacher Institute; 2001. [Google Scholar]
- 2.The Guttmacher Institute. Facts on American Teens’ Sexual and Reproductive Health. New York, NY: The Guttmacher Institute; 2006. [Google Scholar]
- 3.Martin J, Hamilton B, Sutton P, et al. Births: final data for 2006. Natl Vital Stat Rep. 2009;57(7):1–102. [PubMed] [Google Scholar]
- 4.Card JJ, Wise LL. Teenage mothers and teenage fathers: the impact of early childbearing on the parents’ personal and professional lives. Fam Plann Perspect. 1978;10(4):199–205. [PubMed] [Google Scholar]
- 5.Coley RL, Chase-Lansdale PL. Adolescent pregnancy and parenthood. Recent evidence and future directions. Am Psychol. 1998;53(2):152–166. doi: 10.1037//0003-066x.53.2.152. [DOI] [PubMed] [Google Scholar]
- 6.Paranjothy S, Broughton H, Adappa R, et al. Teenage pregnancy: who suffers? Arch Dis Child. 2009;94(3):239–245. doi: 10.1136/adc.2007.115915. [DOI] [PubMed] [Google Scholar]
- 7.Taylor JL. Midlife impacts of adolescent parenthood. J Fam Issues. 2009;30(4):484–510. doi: 10.1177/0192513X08329601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DiClemente RJ, Wingood GM, Crosby RA, et al. A prospective study of psychological distress and sexual risk behavior among black adolescent females. Pediatrics. 2001;108(5):E85. doi: 10.1542/peds.108.5.e85. (doi:10.1542/peds.108.5.e85) [DOI] [PubMed] [Google Scholar]
- 9.Lehrer JA, Shrier LA, Gortmaker S, et al. Depressive symptoms as a longitudinal predictor of sexual risk behaviors among US middle and high school students. Pediatrics. 2006;118(1):189–200. doi: 10.1542/peds.2005-1320. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Berglund PA, Foster CL, et al. Social consequences of psychiatric disorders. II. Teenage parenthood. Am J Psychiatry. 1997;154(10):1405–1411. doi: 10.1176/ajp.154.10.1405. [DOI] [PubMed] [Google Scholar]
- 11.Luke S, Salihu HM, Alio AP, et al. Risk factors for major antenatal depression among low-income African American women. J Womens Health (Larchmt) 2009;18(11):1841–1846. doi: 10.1089/jwh.2008.1261. [DOI] [PubMed] [Google Scholar]
- 12.Rich-Edwards JW, Kleinman K, Abrams A, et al. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60(3):221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mirowsky J, Ross CE. Depression, parenthood, and age at first birth. Soc Sci Med. 2002;54(8):1281–1298. doi: 10.1016/s0277-9536(01)00096-x. [DOI] [PubMed] [Google Scholar]
- 14.Booth A, Rustenbach E, Mchale S. Early family transitions and depressive symptom changes from adolescence to early adulthood. J Marriage Fam. 2008;70(1):3–14. [Google Scholar]
- 15.Mollborn S, Morningstar E. Investigating the relationship between teenage childbearing and psychological distress using longitudinal evidence. J Health Soc Behav. 2009;50(3):310–326. doi: 10.1177/002214650905000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bosquet M, Egeland B. Associations among maternal depressive symptomatology, state of mind and parent and child behaviors: implications for attachment-based interventions. Attach Hum Dev. 2001;3(2):173–199. doi: 10.1080/14616730010058007. [DOI] [PubMed] [Google Scholar]
- 17.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106(3):458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- 18.Hammen C. The social context of risk and resilience in children of depressed mothers. In: Hammen C, editor. Depression Runs in Families: The Social Context of Risk and Resilience in Children of Depressed Mothers. New York, NY: Springer-Verlag; 1991. [Google Scholar]
- 19.Kochanska G, Kuczynski L, Radke-Yarrow M, et al. Resolutions of control episodes between well and affectively ill mothers and their young children. J Abnorm Child Psychol. 1987;15(3):441–456. doi: 10.1007/BF00916460. [DOI] [PubMed] [Google Scholar]
- 20.Lyons-Ruth K, Wolfe R, Lyubchik A. Depression and the parenting of young children: making the case for early preventive mental health services. Harv Rev Psychiatry. 2000;8(3):148–153. [PubMed] [Google Scholar]
- 21.Beeber LS, Perreira KM, Schwartz T. Supporting the mental health of mothers raising children in poverty: how do we target them for intervention studies? Ann N Y Acad Sci. 2008;1136:86–100. doi: 10.1196/annals.1425.008. (doi:10.1196/annals.1425.008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conger RD, Wallace LE, Sun Y, et al. Economic pressure in African American families: a replication and extension of the family stress model. Dev Psychol. 2002;38(2):179–193. [PubMed] [Google Scholar]
- 23.McLoyd VC, Jayaratne TE, Ceballo R, et al. Unemployment and work interruption among African American single mothers: effects on parenting and adolescent socioemotional functioning. Child Dev. 1994;65(2 spec no.):562–589. [PubMed] [Google Scholar]
- 24.Riley AW, Coiro MJ, Broitman M, et al. Mental health of children of low-income depressed mothers: influences of parenting, family environment, and raters. Psychiatr Serv. 2009;60(3):329–336. doi: 10.1176/appi.ps.60.3.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gee CB, Rhodes JE. Postpartum transitions in adolescent mothers’ romantic and maternal relationships. Merrill Palmer Q. 1999;45(3):512–532. [Google Scholar]
- 26.Gee CB, Rhodes JE. Adolescent mothers’ relationship with their children's biological fathers: social support, social strain, and relationship continuity. J Fam Psychol. 2003;17(3):370–383. doi: 10.1037/0893-3200.17.3.370. [DOI] [PubMed] [Google Scholar]
- 27.Spector AZ. Fatherhood and depression: a review of risks, effects, and clinical application. Issues Ment Health Nurs. 2006;27(8):867–883. doi: 10.1080/01612840600840844. [DOI] [PubMed] [Google Scholar]
- 28.Bronte-Tinkew J, Moore KA, Matthews G, et al. Symptoms of major depression in a sample of fathers of infants: sociodemographic correlates and links to father involvement. J Fam Issues. 2007;28(1):61–99. [Google Scholar]
- 29.Bunting L, McAuley C. Research review: teenage pregnancy and parenthood: the role of fathers. Child Fam Soc Work. 2004;9(3):295–303. [Google Scholar]
- 30.Kelly MJ, Dunstan FD, Lloyd K, et al. Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: a comparison of five different methods. BMC Psychiatry. 2008;8:10. doi: 10.1186/1471-244X-8-10. (doi:10.1186/1471-244X-8-10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ware J. SF-36 health survey update. ( http://www.sf-36.org/tools/sf36.shtml). (doi:10.1186/1477-7525-3-74) [Google Scholar]
- 32.Ware J, Snow K, Kosinski M, et al. SF-36 Health Survey: Manual Interpretation and Guide. Lincoln, RI: QualityMetric, Inc; 1993. [Google Scholar]
- 33.McHorney CA, Ware JE, Jr., Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36). II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Berwick DM, Murphy JM, Goldman PA, et al. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Meade CS, Kershaw TS, Ickovics JR. The intergenerational cycle of teenage motherhood: an ecological approach. Health Psychol. 2008;27(4):419–429. doi: 10.1037/0278-6133.27.4.419. [DOI] [PubMed] [Google Scholar]
- 36.Sipsma H, Biello KB, Cole-Lewis H, et al. Like father, like son: the intergenerational cycle of adolescent fatherhood. Am J Public Health. 2010;100(3):517–524. doi: 10.2105/AJPH.2009.177600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Child Trends, Inc. Washington, DC: US Department of Labor; NLSY97 codebook supplement main file round 1: appendix 9. Family process and adolescent outcome measures. Bureau of Labor Statistics; 1999. ( http://www.nlsinfo.org/ordering/display_db.php3#NLSY97) [Google Scholar]
- 38.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 39.Little RJA, Rubin DB. Statistical Analysis With Missing Data. 2nd ed. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- 40.Schafer JL. Analysis of Incomplete Multivariate Data. London, United Kingdom: Chapman & Hall; 1997. [Google Scholar]
- 41.Base SAS® 9.1.3 Procedures Guide. Cary, NC: SAS Institute, Inc; 2006. SAS Institute Inc. [Google Scholar]
- 42.Davey A, Shanahan MJ, Schafer JL. Correcting for selective nonresponse in the National Longitudinal Survey of Youth using multiple imputation. J Hum Res. 2001;36(3):500–519. [Google Scholar]
- 43.Winship C, Radbill L. Sampling weights and regression-analysis. Sociol Methods Res. 1994;23(2):230–257. [Google Scholar]
- 44.Meadows SO, Brown JS, Elder GH. Depressive symptoms, stress, and support: gendered trajectories from adolescence to young adulthood. J Youth Adolesc. 2006;35(1):93–103. [Google Scholar]
- 45.Wickrama KA, Wickrama T, Lott R. Heterogeneity in youth depressive symptom trajectories: social stratification and implications for young adult physical health. J Adolesc Health. 2009;45(4):335–343. doi: 10.1016/j.jadohealth.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 46.Rudolph KD. Gender differences in emotional responses to interpersonal stress during adolescence. J Adolesc Health. 2002;30(4 suppl):3–13. doi: 10.1016/s1054-139x(01)00383-4. [DOI] [PubMed] [Google Scholar]
- 47.Chaplin TM, Hong K, Bergquist K, et al. Gender differences in response to emotional stress: an assessment across subjective, behavioral, and physiological domains and relations to alcohol craving. Alcohol Clin Exp Res. 2008;32(7):1242–1250. doi: 10.1111/j.1530-0277.2008.00679.x. [DOI] [PMC free article] [PubMed] [Google Scholar]