Abstract
Aims
In this study we investigated the effects of the physical work environment on two physiological measures of the stress response.
Methods and Results
Circadian variations in vagally mediated HRV and the morning rise in cortisol were evaluated in sixty participants working in a government building either in a traditional (individual offices and old cubicles; n=40) or a modern workspace (individualized cubicles with improved views and lighting; n=20). Results revealed significant linear (B = −1.03; CI: −1.05 to −1.01, p < .05) and quadratic (B = 1.001; CI: 1.0004 to 1.002, p < .05) trends by office type interactions for indices of vagally mediated HRV. Individuals in the old office space had flatter slopes and thus less circadian variation including less HRV at night, and a larger rise in cortisol upon awakening compared to those in the new office space.
Conclusions
These results indicate that physical features of the work environment may affect two aspects of the physiological stress response: circadian variations in HRV and the morning rise in cortisol. These findings have important social, economic, and public health implications for work environment risk factors on health.
Keywords: work stress, heart rate variability, cortisol
INTRODUCTION
Recent research has suggested that stress at work is a major public health risk associated with cardiovascular morbidity 1, 2, 3. In addition, stress at work is associated with substantial economic consequences, including increased absenteeism, increased worker turnover, decreased worker job satisfaction and associated decreases in worker productivity 4,5. Importantly, the physical characteristics of the work environment including noise, lighting, and ventilation have been linked to job satisfaction in office workers 6 and are therefore implicated in the effects of work-related stress on health. To date few studies have directly investigated the effects of the physical work environment on physiological health outcomes.
In this study, we measured two aspects of the physiological stress response: vagally mediated heart rate variability (HRV) and salivary cortisol, measures of the autonomic nervous system and the hormonal stress response, respectively. These measures were applied to workers in two different office settings.
Decreased vagally mediated HRV is an independent risk factor for morbidity and mortality 7. In healthy individuals there is a prominent circadian variation in HRV such that there are significant increases during the nighttime. We have shown that this increase in HRV during the night is blunted by acute stress as well as in conditions such as chronic alcoholism 8,9 . In addition, diurnal variations in activation of the hormonal stress response, as indexed by cortisol levels, have been associated with increased cardiovascular disease risk 10. Finally, a recent report from the Whitehall Study has shown that work stress is associated with decreased vagally mediated HRV and a larger rise in morning cortisol 2. In the present study we therefore examined the effects of the physical work environment on diurnal variations in HRV and the morning rise in cortisol in workers in old or new office space. We hypothesized that improvement in physical work environment factors previously shown to be associated with job satisfaction, such as natural lighting and views, noise/privacy and ventilation, would be associated with increased diurnal HRV variations and decreased morning rise in cortisol.
METHODS
Subjects
The study protocol was presented to the entire staff working in a single government facility in the Rocky Mountain region of the United States. Of the 200 workers in the facility, 60 (30%) agreed to participate. Subjects were enrolled serially after receiving medical clearance, and were studied over a period of 17 months. Our sample consisted of 60 subjects, of whom 40 were initially working in a traditional workspace and 20 were working in a modern workspace. Forty-seven participants agreed to participate in a second measurement day. Six of these 47 participants changed office type in between the first and the second measurement day (5 from old to new; 1 from new to old). Table 1 shows the descriptive statistics of the total sample, split on type of office space in which participants were first measured. All participants were apparently healthy by medical examination and none were on medications that could potentially interfere with heart rate variability and cortisol levels. Pregnant women were excluded from the study.
Table 1.
Descriptive statistics
| Old Office Space (N = 40) |
New Office Space (N = 20) |
|
|---|---|---|
| Person level | ||
| Gender | 70.0% female | 65.0% female |
| Ethnicity | ||
| Caucasian | 85.0% | 65.0% |
| African-American | 2.5% | 10.0% |
| Hispanic / Latino | 7.5% | 20.0% |
| Asian / Pacific Islander | 5.0% | 0% |
| Marital Status | ||
| Single | 22.5% | 30.0% |
| Married | 60.0% | 45.0% |
| Divorced | 17.5% | 25.0% |
| Age | 46.56 (10.51) | 40.91 (11.14) |
| Months working in workspace | 25.50 (23.66) | 8.35 (6.44) |
| Physical fitness | 3.68 (1.90) | 3.60 (2.35) |
| Daily stress | 2.04 (1.07) | 1.72 (0.99) |
| Episode level | ||
| MSD | 22.65 (18.46) | 22.98 (15.71) |
| nHF | 24.34 (12.38) | 23.07 (13.37) |
| Cortisol | 476.56 (192.67) | 416.29 (114.68) |
| Cigarette consumption | 0.00 (0.05) | 0.10 (0.31) |
| Alcohol consumption | 0.02 (0.14) | 0.00 (0.07) |
| Coffee consumption | 0.25 (0.43) | 0.26 (0.44) |
| Motility | 0.07 (0.13) | 0.05 (0.08) |
Characteristics of the work performed
All workers were white-collar workers involved in real estate management for the government. This is generally sedentary work, requiring typical office-based activities, including substantial computer use, interpersonal interactions (face-to-face meetings of varied sizes and by telephone), moderate amounts of movement within the office environment, and less frequently, travel to other locations.
Physical characteristics of the office spaces
The study was performed in a federally owned building in the United States, which was undergoing serial renovations. This allowed us to measure participants in one geographical location with common external environmental conditions in older traditional office spaces and new renovated office spaces. Some conditions are the same in both new and old spaces, including the heating, ventilating and air conditioning system, ceiling height, and the distance from the window wall to the center of the building (the core). The salient differences between the two spaces are described in Table 2.
Table 2.
Physical characteristics of the old and new office spaces
| Old Office Space (N = 40) |
New Office Space (N = 20) |
|
|---|---|---|
| Workstation layout | Located along the window wall | Located near the core |
| Accessibility of views | Ceiling-height solid partitions | No ceiling-height solid partitions |
| Furniture partitions >64 inches | Furniture partitions <64 inches | |
| No Transparent windows | Transparent windows | |
| Open aisle along the window wall | ||
| Light levels on the work surface | 325 lux | 375 lux |
| Skylights | Not Present | Present |
| Sound | ||
| - Sound masking | Not Present | Present |
| - Low-frequency background noise at 20db |
62 db | 58 db |
| - Quality | Neutral (good) | Marginally acceptable (low frequency/rumble) |
| Measurements of CO2 | ||
| - Temperature at three different height levels: |
No differences | No differences |
| - Volatile organic compounds (VOC), carbon monoxide (CO) and particulates |
No differences | No differences |
| Relative humidity | 17.4% | 20% |
Assessment of subjective responses to physical characteristics of the office spaces
As part of the routine assessments of the workers, an anonymous survey was completed by workers in the old and the new office spaces. From this larger survey 11 questions related to the physical characteristics of the office space, which had previously been shown to be associated with job satisfaction 6 were examined. These questions included satisfaction with numerous factors associated with noise/privacy, ventilation, and lighting and views (see Table 3). The response scales ranged from −3 (very dissatisfied) to +3 (very satisfied).
Table 3.
Differences in employee satisfaction between the office spaces
| Old (n = 46) |
New (n = 22) |
|||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t | p | |
| Temperature | 0.20 | 1.869 | 0.64 | 1.620 | 0.948 | .347 |
| Noise level | 0.09 | 1.736 | 0.32 | 2.079 | 0.482 | .632 |
| Sound privacy | −1.02 | 1.626 | −1.14 | 1.699 | 0.268 | .789 |
| Air quality | 0.09 | 1.872 | 1.55 | 0.858 | 4.405 | .000 |
| Amount of light in own workspace | 1.28 | 1.440 | 2.05 | 1.133 | 2.180 | .033 |
| Distribution of light in own workspace | 1.13 | 1.455 | 1.67 | 1.461 | 1.398 | .171 |
| Amount of daylight in own workspace? | −0.04 | 2.078 | 1.14 | 1.670 | 2.321 | .023 |
| Visual comfort of the lighting | 1.13 | 1.628 | 1.50 | 1.596 | 0.881 | .381 |
| Access to a window view | −0.17 | 2.224 | 1.45 | 1.565 | 3.480 | .001 |
| Overall building | 1.26 | 1.639 | 1.45 | 1.224 | 0.492 | .624 |
| Overall workspace | 0.89 | 1.581 | 1.36 | 1.217 | 1.236 | .221 |
| Questions |
|---|
| How satisfied are you with the temperature in your workspace? |
| How satisfied are you with the noise level in your office? |
| How satisfied are you with your sound privacy? |
| How satisfied are you with the air quality in your workspace? |
| How satisfied are you with the amount of light in your workspace? |
| How satisfied are you with the distribution of light in your workspace? |
| How satisfied are you with the amount of daylight in your workspace? |
| How satisfied are you with the visual comfort of the lighting |
| How satisfied are you with your access to a window view? |
| How satisfied are you with the building overall? |
| All things considered. how satisfied are you with your workspace? |
Procedures
All workers in the building were contacted concerning participation in the study. This study was approved by the National Institute on Aging (MedStar) IRB. Volunteers were solicited and gave written informed consent. After receiving consent a medical exam was scheduled. Those volunteers who were medically cleared for participation were scheduled for a 24-hour ambulatory heart rate recording and diurnal cortisol assessment. Within two weeks, an experimenter fitted the ambulatory ECG device in the morning before the employees started their regular work activities and instructed them on the use of this device as well as on the use of a handheld computer that contained the hourly diary questions. Participants carried both electronic devices for 24 hours. In addition, before the scheduled ECG recording day, participants were instructed on the cortisol assessment and provided with five labelled Salivette tubes. The following morning both electronic devices and the cortisol tubes were collected by the experimenters. For those 47 participants who were measured on a second day, this same basic procedure was followed.
State measurements
Diary format
A Palm™ m100 handheld device (Palm Inc., Santa Clara, CA, USA) was used for the hourly diary. Customized software (Pendragon Forms, version 3.1.; Pendragon Software Corporation, Libertyville, Illinois) was used to implement questions and to transfer responses from the handheld to MS-Access data format. For the hourly diary, an hourly tone (plus or minus 15 min) was set from 8.00 AM to 10.00 PM on which participants were instructed to fill in the computerized questions. When the subjects answered the first question of each entry of the log, the present time was stored to enable comparison between their responses and the cardiac measurements.
Daily Stress and other (bio)behavioral variables
During the last 15 minutes of each hourly measurement period, until 10 PM, the subjects reported on the handheld computer to what extent they had felt stressed (not at all, some, a bit, much, very much). The participants also reported consumed units of tobacco, coffee and alcohol (0, 1–2, 2–4, more than 4) in the preceding hour. In addition, participants rated their habitual physical activity using the University of Houston Non-exercise Questionnaire, a seven-point behaviorally anchored rating scale that has been shown to provide valid measures of habitual physical activity 11.
Cardiac activity
Ambulatory cardiac measures were acquired continuously by the VU-AMS device (version 4.6. TD-FPP, Vrije Universiteit, Amsterdam, the Netherlands). This device has been used extensively and details of its characteristics have been published elsewhere 12. Spectral analysis based upon an autoregressive technique using standard methods was employed 13. The autoregressive algorithm was applied to these data to obtain the high-frequency (0.15 – 0.40 Hz) (HF) component. The HF component is thought to reflect parasympathetic activity. The mean of the absolute successive difference between normal to normal beats (MSD) and normalized high frequency (0.15 to 0.40 Hz; nHF) for consecutive hourly periods were used as indices of vagal activity. The MSD is less affected by breathing and is therefore a suitable outcome measure in ambulatory studies 14. Measures of HRV have been shown to be reliable and reproducible 15.
Cortisol Measurements
Participants were provided with labeled Salivette tubes for collection of saliva to be used for the assessment of cortisol levels. They were instructed to collect saliva upon wakening, 30 minutes after awakening, after arrival at work, mid-day, and in the evening before bedtime. Cortisol samples were analyzed with radio immunoassay (Cortisol RIA kit TKC05). Results are given in ug/dl. The variation coefficient of the assay (CV%) was less than 8.5%.
Statistical Analysis
Individual growth curve models were applied to estimate the effects of the office space, the biobehavioral variables and daily stress, aggregated per measurement day, on circadian variation in natural logarithm transformation of the Mean of Successive Differences (lnMSD), normalized high frequency power (nHF) and cortisol 16, 17. The data collected in the present study had a three-level hierarchical structure, with several daily measurements of biobehavioral variables, MSD, nHF, and cortisol nested within subjects, and subjects clustered within the office spaces.
The distribution of MSD was significantly skewed. This skewness was reduced by logarithmically transforming this variable. In the text, raw data (antilog) values are reported. All analyses were performed using the linear mixed model (MIXED) procedure in SPSS 14.0, with maximum likelihood (ML) estimation. We have previously reported 12 the use of these statistical methods (multi-level regression models), where subjects are treated as random effects, as a valid approach to studying subjects in real-life situations, such as described here.
RESULTS
Descriptive statistics as a function of office type are presented in table 1. The number of months working in the office space was the only variable that significantly differed between the office spaces (t(58) = 4.55, p < .05). We therefore controlled for time in office space in the statistical model.
Heart rate variability
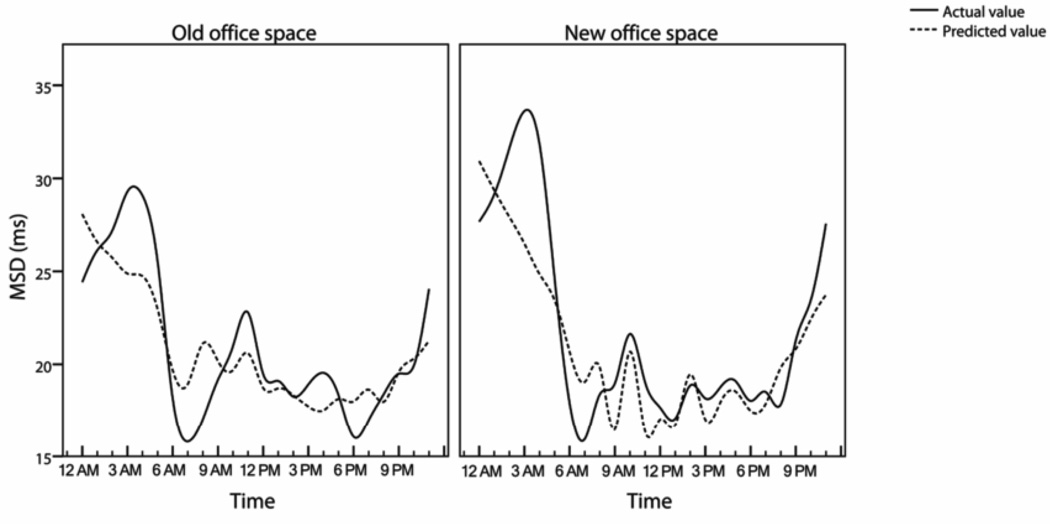
Inspection of the graphs (see figure 1) suggested that the dependent HRV measures could best be described by a quadratic trend, with HRV highest during mid-night and lowest during the working hours as expected. The intraclass correlations showed that 61.56% of the variation in lnMSD and 47.40% of the variation in nHF was due to clustering of the measurements within participants and office spaces, providing strong evidence for a three level hierarchical data structure.
Figure 1.
Estimated circadian heart rate variability curves (MSD) by office space
Effects on lnMSD
Results of the baseline growth curve model are presented in Table 4, which confirms that circadian lnMSD is best described by a quadratic trend (model 1). Office space and its interactions with the time variables were added as a predictors to the model (model 2) resulting in a better fit based on the deviance test (χ2 = 51.71, df = 5, p < .01). There was no main effect of office space on lnMSD. However, there was a significant difference between the office spaces in the circadian lnMSD curve which was indicated by a significant interaction between office space and a linear time trend (B = −1.03 (antilog value); CI: −1.05 to −1.01, p < .05) and a significant interaction between office space and a quadratic time trend (B = 1.001 (antilog value); CI: 1.0004 to 1.002, p < .05). When controlling for the effects of biobehavioral variables, the interaction effects between the office spaces and the times variables remained significant (model 3). This model fitted the data best (comparing model 3 with model 2: χ2 = 470.90, df = 9, p < .001). These interactions support statistically what is visible in figure 1, namely that in the new office space, in comparison with the old office space, HRV is higher during the night and lower during the working hours. Thus the HRV slope is less flat in the new space compared to the old space as shown by the difference between the highest lnMSD value and the lowest value being larger in the new space, compared to the old office space.
Table 4.
Results of fitting a multilevel model for change on the lnMSD data
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Dependent variable Predictor | lnMSD | lnMSD | lnMSD |
| Fixed effects | |||
| Intercept | 3.286 (.065)* | 3.212 (.079)* | 4.275 (.291)* |
| Time, linear slope | −.075 (.004)* | −.065 (.006)* | −.038 (.006)* |
| Time, quadratic slope | .003 (.0001)* | .002 (.0002)* | .001 (.0002)* |
| Office space | .199 (.130) | .112 (.131) | |
| Time, linear x Office space | −.029 (.009)* | −.020 (.010)* | |
| Time, quadratic x Office space | .001 (.0003)* | .0007 (.0003)* | |
| Cigarette consumption | −.099 (.020)* | ||
| Alcohol consumption | −.262 (.075)* | ||
| Coffee consumption | .016 (.016) | ||
| Motility | −1.381 (.086)* | ||
| Gender | .386 (.126)* | ||
| Age | −.027 (.006)* | ||
| Daily stress | −.050 (.035) | ||
| Months working at office space | .002 (.001) | ||
| Physical fitness | −.029 (.013)* | ||
| Variance components | |||
| Repeated Measures | .142 (.004)* | .134 (.004)* | .118 (.004)* |
| Intercept variance | .277 (.047)* | .253 (.045)* | .212 (.043)* |
| Intercept-Slope covariance | .0003 (.0008) | .001 (.0008)* | |
| Slope variance | .0001 (.0000)* | .0001 (.0000)* | |
| Deviance | 2236.89 | 2185.18 | 1714.28 |
lnMSD = natural logarithm transformation of the Mean of Successive Differences (MSD).
Values are estimates (± SE).
p < .05.
Model 1: baseline growth level model with random intercept. In models 2 and 3 the intercept and the slope of time were allowed to vary between office spaces and subjects.
The mixed model, or random effects model method of statistical analysis applied here and in table 5 and 6, was selected in order to address issues that arise when performing studies in real life situations, that is, issues related to missing data, unequal cells with respect to time or location, order of recruitment, order of repeated measures, seasonal effects, potential co-morbidities or medication use. Office space and subjects were included as higher level (random) effects and day of measurement and hours since waking, as repeated effects. All independent variables were centered on their grand mean. The units reported in the tables represent the change from the intercept (increase or decrease) associated with the effect of each variable. A sequence of three models was tested for each dependent variable: a baseline growth curve model containing only time variables (HRV: linear and quadratic time trends; cortisol: cubic time trend) served as a baseline model to assess the contribution of adding other predictor variables to the model. The main effects of interest. office space and its interaction with time variables were added in a second model. Modelling variation of slopes across persons was applied to evaluate whether these variables had a random effect. Finally, biobehavioral variables, aggregated per measurement day were added to the model, to examine whether these could account for potential significant effects of the office space.
Effects on nHF
Normalized high frequency power was also best described by a quadratic trend (see also table 5; model 1). When office space and its interactions with the time variables were added as a predictors to the model (model 2), the model fit improved (χ2 = 102.69, df = 5, p < .001). The circadian nHF curves were significantly different for the office spaces, indicated by a significant interaction between office space and a linear time trend (B = −.67; CI: −1.08 to −0.26, p < .01) and a significant interaction between office space and a quadratic time trend (B = 0.028; CI: 0.012 to 0.044, p < .01). This pattern remained significant after controlling for the biobehavioral variables, which resulted in a better fitting model (χ2 = 92.93, df = 9, p < .001). Thus, the nHF analyses yield very similar results as the lnMSD analyses.
Table 5.
Results of fitting a multilevel model for change on the nHF data
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Dependent variable Predictor | nHF | nHF | nHF |
| Fixed effects | |||
| Intercept | 34.043 (1.578)* | 33.312 (1.727)* | 41.775 (4.679)* |
| Time, linear slope | −2.191 (.097)* | −1.967 (.124)* | −1.739 (.126)* |
| Time, quadratic slope | .082 (.004)* | .072 (.005)* | .063 (.005)* |
| Office space | 2.372 (2.831) | 2.639 (2.675) | |
| Time, linear x Office space | −.670 (.210)* | −.658 (.207)* | |
| Time, quadratic x Office space | .028 (.008)* | .027 (.008)* | |
| Cigarette consumption | −1.664 (.383)* | ||
| Alcohol consumption | −2.040 (1.396) | ||
| Coffee consumption | −.068 (.219) | ||
| Motility | −13.219 (1.841)* | ||
| Gender | −5.329 (2.023)* | ||
| Age | −.132 (.089) | ||
| Daily stress | .914 (.654) | ||
| Months working at workspace | .012 (.023) | ||
| Physical fitness | −.312 (.258) | ||
| Variance components | |||
| Repeated Measures | 67.607 (2.073)* | 62.408 (1.947)* | 59.967 (1.87.)* |
| Intercept variance | 80.831 (13.919)* | 119.701 (21.321)* | 100.955 (18.724)* |
| Intercept-Slope covariance | −2.248 (.594)* | −2.075 (.551)* | |
| Slope variance | .097 (.023)* | .099 (.023)* | |
| Deviance | 15774.73 | 15672.04 | 15578.11 |
nHF = normalized high frequency power.
Values are estimates (± SE).
p < .05.
Model 1: baseline growth level model with random intercept. In models 2 and 3 the intercept and the slope of time were allowed to vary between office spaces and subjects.
Taken together, the HRV analyses showed that HRV was higher during the night-time and lower during the working hours in the new office space compared to the old space.
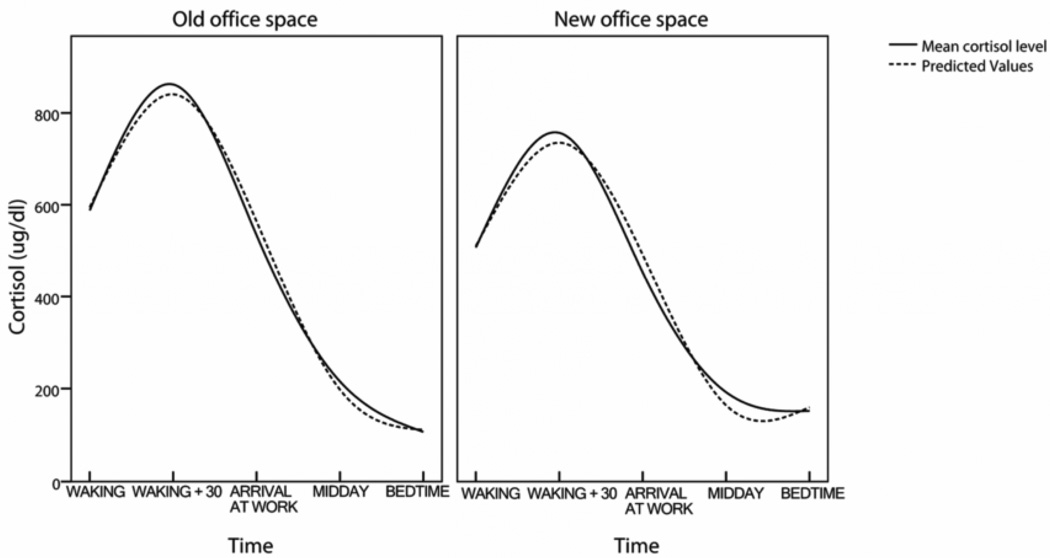
Cortisol
Results of the multilevel analysis of the cortisol data are presented in table 6. Inspection of the graphs (see figure 2) suggested that the circadian cortisol curves could best be described by a cubic time trend, with cortisol highest 30 minutes after waking. This was confirmed in a baseline growth curve model (model 1). In the second model office space and its interaction with the cubic time trend were entered into the model resulting in an overall better fitting model (χ2 = 22.43, df = 2, p < .001). A significant main effect of office space was found (B = −114.82; CI: −224.79 to −4.85), with overall higher levels of cortisol in the old office space. The interaction of office space with the cubic time trend was also significant (B = 2.39; CI: 0.12 to 4.66). Pre-planned t-tests showed statistically higher cortisol levels at 30 minutes after awakening in participants working in the old office space (M = 871.07 ug/dl, SD = 362.50) versus participants working in the new office space (M = 756.64 ug/dl, SD = 286.47, t(80) = 1.41, p = .04, one-tailed). Controlling for biobehavioral variables in the third model resulted in a better fitting model (χ2 = 202.27, df = 9, p < .001), yet only caffeine intake had a – marginally - significant negative effect on overall cortisol levels (p = .062, two-tailed). The main effect of office space was slightly reduced and became a statistical trend (p = .080, two-tailed), but the interaction between office space and the cubic time trend remained significant. These results suggest that the morning rise in cortisol is greater in the old office space compared to the new office space.
Table 6.
Results of fitting a multilevel model for change on the cortisol data
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Dependent variable Predictor | Cortisol | Cortisol | Cortisol |
| Fixed effects | |||
| Intercept | 565.54 (32.06)* | 603.56 (42.02)* | 652.47 (122.84)* |
| Time, linear slope | 632.55 (68.51)* | 632.44 (66.40)* | 613.67 (67.14)* |
| Time, quadratic slope | −457.14 (43.33)* | −456.53 (41.87)* | −444.35 (42.25)* |
| Time, cubic slope | 67.92 (7.12)* | 67.01 (6.88)* | 65.06 (6.95)* |
| Office space | −114.82 (55.16)* | −102.43 (57.66)(p = .080) | |
| Time, Cubic x Office Space | 2.39 (1.14)* | 2.49 (1.16)* | |
| Cigarette consumption | 4.28 (15.48) | ||
| Alcohol consumption | 74.50 (48.25) | ||
| Coffee consumption | −15.90 (8.30)(p = .062) | ||
| Motility | −193.62 (235.98) | ||
| Gender | −5.01 (44.76) | ||
| Age | −.92 (2.10) | ||
| Daily stress | −13.29 (27.94) | ||
| Months working at office space | 1.48 (1.20) | ||
| Physical fitness | −5.21 (10.08) | ||
| Variance components | |||
| Repeated Measures | 59262.31 (4560.46)* | 55264.71 (4429.52)* | 54116.84 (4455.87)* |
| Intercept variance | 16363.20 (4973.52)* | 39218.10 (11694.72)* | 38657.58 (12095.75)* |
| Intercept-Slope covariance | −6440.03 (3138.72)* | −6779.82 (3181.23)* | |
| Slope variance | 1068.81 (983.48)* | 1190.68 (980.26) | |
| Deviance a | 5620.02 | 5597.60 | 5395.68 |
Values are estimates (± SE).
p < .05. Model 1: baseline growth level model with random intercept. In models 2 and 3 the intercept and the slope of time were allowed to vary between office spaces and subjects.
Figure 2.
Estimated diurnal cortisol curves by office space
DISCUSSION
The results of the present study provide important new evidence for the effects of the physical work environment on work-related stress. This study for the first time links the physical work environment to altered physiological aspects of the stress response. We found that old office space, characterized by poorer lighting and air quality compared to the new office space, was associated with less vagally mediated HRV at night and a higher morning cortisol rise. The pattern of relatively lower nighttime and higher daytime vagally mediated HRV observed in subjects in the old office space was opposite to the expected typical healthy pattern, in which HRV should be higher at night and lower during working hours. Together these findings indicate greater activation of both the autonomic and hormonal stress response in subjects in old office space, and a shift towards a more vagally mediated, lower stress hormone responsive state in subjects in the new office space.
Numerous studies have now reported that work stress is associated with increased risk of coronary heart disease (CHD) 18,19. In a prospective study based on the Whitehall II study Chandola et al (2008) 2 found that work stress was associated with lower vagally mediated HRV and a greater morning rise in cortisol unrelated to other health behaviors. Thus, these authors suggested that work stress had direct effects on autonomic (ANS) and endocrine responses that were not mediated through health behaviors.
In the current study we found that the physical characteristics of the work place had effects on these same ANS and endocrine responses, and that these effects were also not mediated by health-related behaviors such as smoking, physical fitness, alcohol or caffeine consumption. Specifically, we found that persons working in the older office space, which was characterized by poorer subjective air quality and lighting features such as less daylight and less access to window views, had a decreased diurnal variation in HRV, including less HRV at night, as well as a larger morning rise in cortisol. These are the same physiological responses identified by Chandola et al 2 as intermediate mechanisms for the relationship between work stress and CHD. Importantly our findings were independent of any difference reported by subjects in the two office spaces in perceived stress. In fact, the HRV effects were greatest during the night when no self-reports were possible. Thus, our study suggests that the physical work environment may affect at least some of the underlying physiological factors associated with the negative health effects of increased work stress without the subjects being consciously aware of a stressful experience.
We have previously shown that stress and worry during the day can have effects on both daytime and nighttime cardiac activity 12, 20. These nighttime effects included increased HR and decreased HRV. Moreover, we hypothesized that these nighttime effects were occurring outside of conscious awareness and that these may represent a major source of stress-related cardiac activity that goes unreported. In the current study we were able to identify that physical workspace, as a whole, may account for at least some of these unreported stress effects of the work environment. In addition the effects on HRV in the present study were of the same magnitude as we previously found to be associated with reported stress and worry (approximately 1 ms) even though in this study there were no significant differences in reported stress between the two office types.
Although in this study we did not address the individual features of the two workspaces that might account for these effects, there were distinct differences between them, which together could account for these differences. These include lighting/views, acoustics, and perceived air quality. These features have been reported to be associated with worker satisfaction in other studies 6. In order to evaluate the contribution of such specific features of the work environment to worker satisfaction, Veitch et al 6 (2007) developed and applied a set of standardized measurement tools for the assessment of workers’ perceptions of their work environment. Three primary factors were identified, which were associated with workers’ perceptions of satisfaction with their workplace. These factors were privacy/acoustics, ventilation/temperature, and lighting/views.
In the present study, workers in the new office space reported greater satisfaction in the air quality, amount of daylight and access to window views compared to those in the older office space. Light levels and views of nature have both been associated with better health outcomes and lower depressive symptomatology in hospital settings 21, and could contribute to a shift in stress response systems 22. The difference of 50 lux on the work surfaces measured in the two office spaces is within the perceivable range and could contribute to differential physiological responses in the two spaces. Although airflow and ventilation were not measurably different in the two spaces, workers in this study reported more satisfaction with air quality in the new compared to the old office space. An additional feature that distinguishes the two workspaces is the considerable amount of low-frequency noise in the old compared to the new space. Low-frequency mechanical noise has been linked to increased occupant discomfort 23, and noise levels in general have been associated with activation of the stress response and worse health outcomes in a variety of settings 24. Together these features corresponded to physical differences between the two office spaces, although the two spaces were both within established limits for safety and comfort. Thus, although both spaces were within acceptable limits, it is possible that subtle differences in architectural features of workspaces could have a significant effect on health outcomes.
In order to rule out whether the difference in numbers of months workers had spent in the two types of office space could have contributed to the observed effects, we controlled for time in office space and found that this variable was not a significant contributor in the models. Furthermore, we allowed participants habituation time (at least 8 weeks) in the new space to minimize any potential acute effects of the move.
More work is needed to identify the specific physical characteristics of the work place, which can impact health and consequent related aspects of work behavior such as absenteeism, worker turnover, worker job satisfaction, and worker productivity. However the clear association we report here between overall workplace physical environment and physiological measures of the stress response, which are known to be intermediate mechanisms in stress-related illnesses, points to the importance of the physical work environment on health. The current study suggests some features of the physical work environment that should be considered for future study, and provides sensitive objective outcome measures that could be used in subsequent research to address this relatively overlooked factor contributing to workplace stress, with important social, economic, and public health impact on workers.
ACKNOWLEDGEMENTS
This study was funded by the United States General Services Administration, the Intramural Research Program of the National Institute of Mental Health and National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi-amorn C, Sato H, Yusaf S. INTERHEART investigators. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 2.Chandola T, Britton A, Brunner E, Hemingway H, Malik M, Kumari M, Badrick E, Kivimaki M, Marmot M. Work stress and coronary heart disease: what are the mechanisms? Eur Heart J. 2008;29(5):640–648. doi: 10.1093/eurheartj/ehm584. [DOI] [PubMed] [Google Scholar]
- 3.Kornitzer M, deSmet P, Sans S, Dramaix M, Boulenguez C, DeBacker G, Ferrario M, Houtman I, Isacsson SO, Ostergren PO, Peres I, Pelfrene E, Romon M, Rosengren A, Cesana G, Wilhelmsen L. Job stress and major coronary events: results from the Job Stress, Absenteeism and Coronary Heart Disease in Europe study. Eur J Cardiovasc Prev Rehabil. 2006 Oct;13(5):695–704. doi: 10.1097/01.hjr.0000221865.19415.e9. [DOI] [PubMed] [Google Scholar]
- 4.Duijts SFA, Kant I, Swaen GMH, van den Brandt PA, Zeegers MPA. A meta-analysis of observational studies identifies predictors of sickness absence. J Clin Epidemiol. 2007;60(11):1105–1115. doi: 10.1016/j.jclinepi.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Harter JK, Schmidt FL, Hayes TL. Business-unit level relationship between employee satisfaction, employee engagement, and business outcomes: A meta-analysis. J Appl Psych. 2002;87:268–279. doi: 10.1037/0021-9010.87.2.268. [DOI] [PubMed] [Google Scholar]
- 6.Veitch JA, Charles KE, Farley KMJ, Newsham GR. A model of satisfaction with open-plan office conditions: COPE field findings. J Environ Psych. 2007;27:177–189. [Google Scholar]
- 7.Tsuji H, Larson MG, Venditti FJ, Jr, Manders ES, Evans JC, Feldman CL, Levy D. Impact of reduced heart rate variability on risk for cardiac events. The Framingham heart study. Circulation. 1996;94(11):2850–2855. doi: 10.1161/01.cir.94.11.2850. [DOI] [PubMed] [Google Scholar]
- 8.Hall M, Vasko R, Buysse D, Ombao H, Chen Q, Cashmere JD, Kupfer D, Thayer JF. Acute stress affects heart rate variability during sleep. Psychosomatic Medicine. 2004;66(1):56–62. doi: 10.1097/01.psy.0000106884.58744.09. [DOI] [PubMed] [Google Scholar]
- 9.Irwin M, Valladares E, Motivala S, Thayer JF, Ehlers C. Association between nocturnal vagal tone and sleep depth, sleep quality and fatigue in alcohol dependence. Psychosomatic Medicine. 2006;68(1):159–166. doi: 10.1097/01.psy.0000195743.60952.00. [DOI] [PubMed] [Google Scholar]
- 10.Kunz-Ebrecht SR, Kirschbaum C, Steptoe A. Work stress, socioeconomic status and neuroendocrine activation over the working day. Soc Sci Med. 2004;58(8):1523–1530. doi: 10.1016/S0277-9536(03)00347-2. [DOI] [PubMed] [Google Scholar]
- 11.Jackson AS, Blair SN, Mahar MT, Weir LT, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22(6):863–870. doi: 10.1249/00005768-199012000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Pieper S, Brosschot JF, van der Leeden R, Thayer JF. Cardiac effects of momentary assessed worry episodes and stressful events. Psychosomatic Medicine. 2007;69(9):901–909. doi: 10.1097/PSY.0b013e31815a9230. [DOI] [PubMed] [Google Scholar]
- 13.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17(3):354–381. [PubMed] [Google Scholar]
- 14.Penttila J, Helminen A, Jartti T, Kuusela T, Huikuri HV, Tulppo MP, Coffeng R, Scheinin H. Time domain, geometrical and frequency domain analysis of cardiac vagal outflow: effects of various respiratory patterns. Clin Physiol. 2001;21:365–376. doi: 10.1046/j.1365-2281.2001.00337.x. [DOI] [PubMed] [Google Scholar]
- 15.Li Z, Snieder H, Su S, Ding X, Thayer JF, Trieber FA, Wang X. A longitudinal study in youth of heart rate variability at rest and in response to stress. International Journal of Psychophysiology. 2009;73:212–217. doi: 10.1016/j.ijpsycho.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hruschka DJ, Kohrt BA, Worthman CM. Estimating between- and within-individual variation in cortisol levels using multilevel modeling. Psychoneuroendocrinology. 2005;30(7):698–714. doi: 10.1016/j.psyneuen.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press; 2003. [Google Scholar]
- 18.Aboa-Eboule C, Brisson C, Maunsell E, Masse B, Bourbonnais R, Vezina M, Milot A, Theroux P, Dagenais GR. Job strain and risk of acute recurrent coronary heart disease events. Journal of the American Medical Association. 2007;298(14):1652–1660. doi: 10.1001/jama.298.14.1652. [DOI] [PubMed] [Google Scholar]
- 19.Belkic KL, Landsbergis PA, Schnall PL, Baker D. Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health. 2004;30(2):85–128. doi: 10.5271/sjweh.769. [DOI] [PubMed] [Google Scholar]
- 20.Brosschot JF, van Dijk E, Thayer JF. Daily worry is related to low heart rate variability during waking and the subsequent nocturnal sleep period. Journal of Psychophysiology. 2007;(1):39–47. doi: 10.1016/j.ijpsycho.2006.07.016. International. [DOI] [PubMed] [Google Scholar]
- 21.Ulrich R. View through a window may influence recovery from surgery. Science. 1984;224(4647):420–421. doi: 10.1126/science.6143402. [DOI] [PubMed] [Google Scholar]
- 22.Leather P, Pyrgas M, Beale D, Lawrence C. Windows in the workplace: Sunlight, view and occupational stress. Environment and Behavior. 1998;30(6):739–762. [Google Scholar]
- 23.Benton S, Leventhall HG. The role of "background stressors" in the formation of annoyance and stress responses. Jnl Low Freq Noise Vibn. 1994;13:95–102. [Google Scholar]
- 24.Hagerman I, Rasmanis G, Blomkvist V, Ulrich R, Eriksen CA, Theorell T. Influence of intensive coronary care acoustics on the quality of care and physiological state of patients. Int J Cardiology. 2005;98(2):267–270. doi: 10.1016/j.ijcard.2003.11.006. [DOI] [PubMed] [Google Scholar]