Abstract
BACKGROUND
It is unknown whether survival after in-hospital cardiopulmonary resuscitation (CPR) is improving and which patient and hospital characteristics predict survival.
METHODS
We examined fee-for-service Medicare data from 1992 to 2005 to identify beneficiaries ≥ 65 years old who received CPR in US hospitals. We examined temporal trends in the incidence of and survival after CPR, as well as patient and hospital-level predictors of survival to discharge.
RESULTS
We identified 433,985 cases of in-hospital CPR and 18.3% survived to discharge (95% CI 18.2-18.5%). Survival was static during this period. The incidence of CPR was 2.73 events per 1000 admissions and was higher among non-white patients. The proportion of dying patients receiving in-hospital CPR prior to death increased over time and was higher for non-white patients. Patients who were male, older, had more co-morbid illness, or were admitted from a skilled nursing facility had lower survival. Adjusted odds of survival for black patients were 23.6% lower than similar white patients (95% CI 21.2%-25.9%). The association between race and survival was partially explained by hospital effects: black patients were more likely to receive CPR in hospitals with lower post-CPR survival. Among patients surviving in-hospital CPR, the proportion of patients discharged home decreased over time.
CONCLUSIONS
Survival following in-hospital CPR did not improve from 1992-2005 and the proportion of patients receiving in-hospital CPR prior to death increased while the proportion of survivors discharged home after CPR decreased. Black race was associated with higher rates of CPR, but lower survival after CPR.
Keywords: Adult; Aged; Aged, 80 and over; Cardiopulmonary Resuscitation/methods/ statistics & numerical data; Cohort studies; Electric Countershock; Female; Heart Arrest/mortality/therapy; Hospitalization/ statistics & numerical data; Humans; Incidence; Male; Medicare; Outcome Assessment (Health Care); Resuscitation Orders; Retrospective Studies; Terminal Care/ utilization; United States/epidemiology
INTRODUCTION
After the development of cardiopulmonary resuscitation (CPR), this procedure evolved from a specific intervention applied in limited clinical situations to the default response to cardiac arrest in and out of the hospital, an evolution accompanied by a dramatic decline in survival rates.1-3 Subsequently, innovations allowing rapid out-of-hospital CPR translated to improved outcomes in the out-of-hospital setting.4, 5 However, it is unclear whether advances in CPR or post-arrest care have improved outcomes following in-hospital arrest.
Reports of survival to discharge following in-hospital CPR vary from 7% to 26%. 6-8 The largest study to date included 14,720 CPR events from the National Registry of CPR (NRCPR) and found 17% of patients surviving to discharge.9 Associations between age and survival after CPR remain unclear, with prior studies finding conflicting results.6, 10, 11 Black race may be associated with lower survival after in- and out-of-hospital CPR, and may be associated with delayed defibrillation.12-14
We investigated the epidemiology of in-hospital CPR in older US adults from 1992 to 2005, including trends in incidence, survival to hospital discharge, proportion of in-hospital deaths preceded by CPR, discharge destination among survivors, and patient and hospital characteristics associated with survival.
METHODS
Data Sources and Study Population
We analyzed 100% of Medicare Medical Provider Analysis and Review (MedPAR) hospital claims from 1992 through 2005 to identify beneficiaries 65 years or older who received in-hospital CPR, defined as presence of either of two procedure codes in the International Classification of Diseases, Ninth Revision (ICD-9): 99.60 (Cardiopulmonary resuscitation, not otherwise specified) or 99.63 (Closed chest cardiac massage). We restricted analyses to individuals receiving Medicare through the Old Age & Survivors Insurance program excluding those receiving Social Security Disability Income. We excluded individuals co-enrolled in a health maintenance organization (HMO) who may have had incomplete CPR claims data and thus would have introduced bias; exclusion of HMO co-enrollees is common when using MedPAR to assess health care services.15, 16 For individuals with more than one CPR event, we analyzed only the first occurrence.
Our primary outcome was survival to hospital discharge. Potential predictors included age, gender, race, chronic comorbid illness, zip-code median income, admission from a skilled nursing facility, and hospital size, rurality, and teaching status. We also examined the influence of individual hospital on survival. Because race designation other than black and white within Medicare data may be inaccurate, we categorized race as white, black, or other.17 We used the Deyo-Charlson score to assess chronic illness burden, categorized as 0, 1, 2, or ≥3 and included in regression models as a grouped-linear variable; this score does not measure type or severity of acute illness.18 We used regional median household income from 1999 US Census data by patient zip code to assess socioeconomic status. We examined hospital identity using Medicare provider number, and used Centers for Medicare & Medicaid Services (CMS) data to determine hospital characteristics such as bed number and teaching status. We examined rurality of hospital using zip code and the Rural-Urban Commuting Area Codes approximation, version 2.0, dichotomized as metropolitan and non-metropolitan.19 The 22 discharge destination codes within MedPAR were reduced to “home”, “another hospital”, “skilled nursing facility”, or “hospice”, and were used to estimate functional status at discharge. The Institutional Review Boards of the University of Washington and CMS approved this study.
The authors designed and executed this study. Dr. Ehlenbach had access to all data, takes responsibility for all data and analyses, wrote the manuscript with input from co-authors, and controlled the decision to publish.
Statistical Analysis
We evaluated between-group differences and trends in survival and incidence using the χ2 test, and adjusted trends using the likelihood ratio test. We excluded 55,665 individuals (12.8%) with missing values for one or more variables of interest from bivariate and multivariable analyses; 40,885 were only missing income data. Bivariate analyses of the association of survival with patient and hospital characteristics were performed with logistic regression using empirical standard error estimates to account for correlation between multiple observations within hospitals. Variables with a statistically significant association (p< 0.05) were included in multivariable models. We created one multivariable model including all significant patient and hospital characteristics using logistic regression with empirical standard error estimates. In order to investigate the role that individual hospitals played in racial differences in survival, we created a second multivariable model including patient factors and individual hospital identifiers. We used Stata, version 10.0 (StataCorp, College Station, TX), and SAS, version 9.1 (SAS Institute, Cary, NC), for statistical analyses.
RESULTS
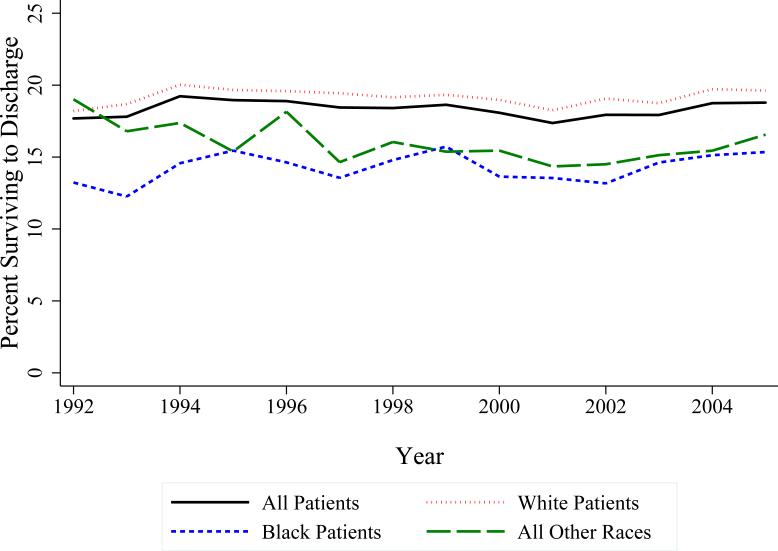
We identified 433,985 beneficiaries receiving in-hospital CPR; 18.3% survived to discharge (95% CI 18.2-18.5%). Survival was lower for patients who were men, older, non-white, admitted from a skilled nursing facility, had a Deyo-Charlson ≥3, or received care in metropolitan or teaching hospitals (Table 1). Patients diagnosed with a myocardial infarction or congestive heart failure during the hospitalization at which CPR occurred had slightly higher survival. There was no significant trend in survival over time crudely (p=0.569, Figure 1), or after adjusting for diagnoses (p=0.856).
Table 1.
Percent of Patients Who Underwent In-Hospital CPR Surviving to Hospital Discharge by Patient and Hospital Characteristics
| n (%) | % Surviving* | |
|---|---|---|
| Total | 433,985 | 18.3 |
| Patient Characteristics | ||
| Sex | ||
| Men | 219,377 (50.5) | 17.5 [17.3, 17.6] |
| Women | 214,608 (49.5) | 19.2 [19.1, 19.4] |
| Age | ||
| 65-69 | 63,299 (14.6) | 22.2 [21.9, 22.6] |
| 70-74 | 84,353 (19.4) | 20.9 [20.6, 21.1] |
| 75-79 | 98,263(22.6) | 19.1 [18.9, 19.3] |
| 80-84 | 91,471 (21.1) | 17.0 [16.8, 17.3] |
| 85-89 | 62,530 (14.4) | 15.1 [14.8, 15.4] |
| ≥90 | 34,069 (7.9) | 12.2 [11.9, 12.6] |
| Race | ||
| White | 352,173 (81.2) | 19.2 [19.1, 19.3] |
| Black | 59,682 (13.8) | 14.3 [14.0, 14.6] |
| All Other Races | 22,130 (5.1) | 15.9 [15.4, 16.4] |
| Deyo-Charlson score | ||
| 0 | 77,349 (17.8) | 18.7 [18.5, 19.0] |
| 1 | 145,627 (33.6) | 19.1 [18.9, 19.3] |
| 2 | 116,401 (26.8) | 18.9 [18.7, 19.2] |
| ≥3 | 94,608 (21.8) | 16.1 [15.8, 16.3] |
| SNF Residence† | ||
| Yes | 10,924 (2.5) | 11.5 [10.9, 12.1] |
| No | 423,061 (97.5) | 18.5 [18.4, 18.6] |
| Zipcode Median Income | ||
| < $15,000 | 10,626 (2.5) | 13.3 [12.7, 14.0] |
| $15,000-29,999 | 87,164 (20.1) | 17.9 [17.7, 18.2] |
| $30,000-44,999 | 178,536 (41.1) | 19.1 [19.0, 19.3] |
| $45,000-59999 | 70,429 (16.2) | 18.4 [18.1, 18.7] |
| $60,000-74,999 | 22,083(5.1) | 18.3 [17.8, 18.8] |
| $75,000+ | 15,458 (3.6) | 17.6 [17.0, 18.2] |
| No income data | 49,489 (11.5) | 17.4 [17.1, 17.7] |
| Diagnoses | ||
| Myocardial Infarction | ||
| Yes | 92,968 (21.4) | 20.4 [20.1, 20.7] |
| No | 340,999 (78.6) | 17.9 [17.7, 17.9] |
| Congestive Heart Failure | ||
| Yes | 168,515 (38.3) | 20.3 [20.1, 20.6] |
| No | 265,470 (61.2) | 17.1 [16.9, 17.2] |
| Stroke | ||
| Yes | 38,121 (8.8) | 18.2 [17.8, 18.5] |
| No | 395,864 (91.2) | 18.3 [18.2, 18.4] |
| Diabetes Mellitus | ||
| Yes | 78,840 (18.2) | 17.3 [17.0, 17.6] |
| No | 355,145 (81.8) | 18.6 [18.4, 18.7] |
| COPD | ||
| Yes | 116,997 (27.0) | 18.9 [18.6, 19.1] |
| No | 316,988 (73.0) | 18.2 [18.0, 18.3] |
| Hospital Characteristics ‡ | ||
| Rurality | ||
| Metropolitan | 345,808 (79.7) | 18.0 [17.9, 18.1] |
| Non-Metro | 73,397 (16.9) | 21.1 [20.9, 21.5] |
| Unknown | 14,780 (3.4) | 12.6 [12.0, 13.1] |
| Teaching Status | ||
| Teaching Hosp. | 144,385 (33.3) | 17.4 [17.2, 17.6] |
| Non-Teaching | 288,774 (66.7) | 18.8 [18.6, 18.9] |
| Unknown | 826 (0.2) | 26.3 [23.3, 29.3] |
| Hospital Size | ||
| <250 beds | 165,514 (38.1) | 19.6 [19.4, 19.8] |
| 250-449 beds | 142,462 (32.8) | 17.7 [17.5, 17.9] |
| 450 + beds | 125,183 (28.9) | 17.3 [17.1, 17.5] |
| Unknown | 826 (0.2) | 26.3 [23.3, 29.3] |
χ2 p<0.001 for all between-category differences, except for stroke whose p=0.32.
Residence at a skilled nursing facility prior to hospital admission
Diagnoses coded during the hospitalization at which CPR was performed.
Figure 1. Survival to Hospital Discharge Following In-Hospital CPR by Year and Race.
Survival is poorer for non-white individuals. There is no significant trend in overall survival 1992-2005 (Likelihood ratio p=0.569).
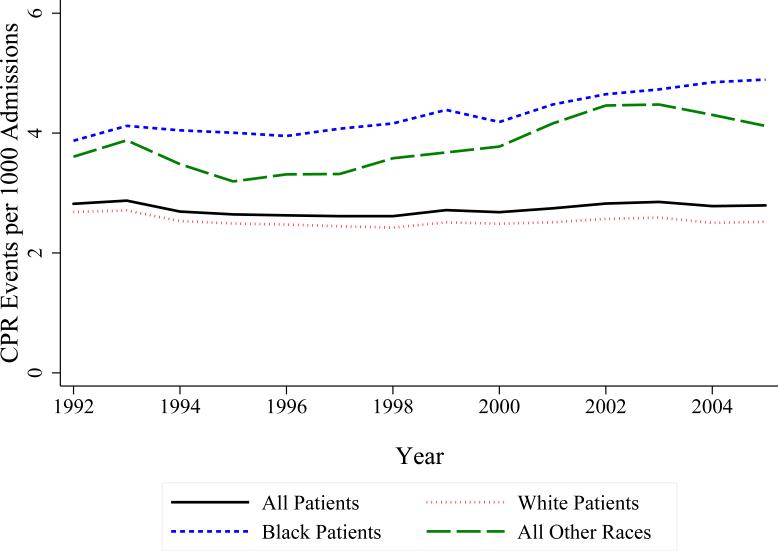
There were 158,730,366 hospital admissions among eligible beneficiaries, for a cumulative incidence of in-hospital CPR of 2.73 events per 1000 admissions. This incidence did not change substantially from 1992 to 2005 (Figure 2). Small variations resulted in a clinically insignificant but statistically significant positive linear trend for the study period (p<0.001). The incidence of CPR differed by race: 2.53/1000 admissions in white patients, 4.35/1000 admissions in black patients, and 3.85/1000 admissions for other races.
Figure 2. Trends in CPR Utilization, by Race.
A. Incidence of in-hospital CPR. The incidence of in-hospital CPR is higher for non-white individuals. There is a clinically insignificant but statistically significant positive linear trend in incidence when considering all patients 1992-2005 (p <0.001). B. Deaths following in-hospital CPR as a percentage of all hospital deaths. The percentage of dying patients receiving CPR prior to death is increasing, and is higher for non-white individuals. The linear trend, considering all patients, is highly statistically significant (p<0.001).
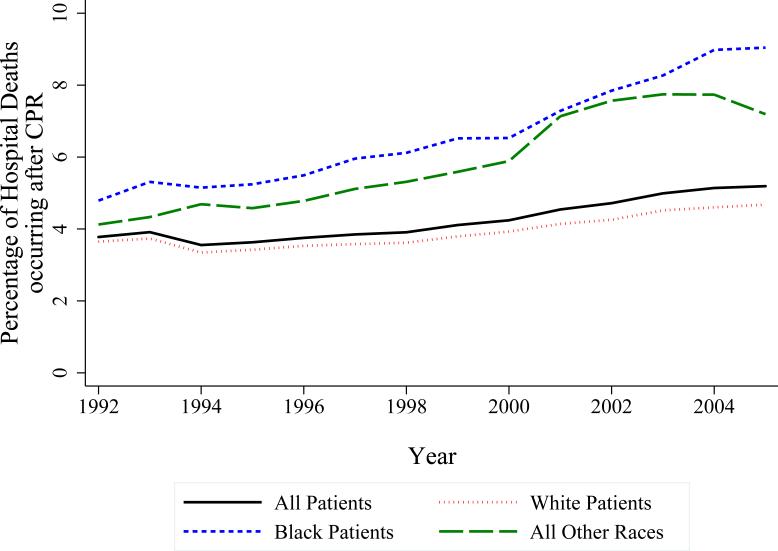
Among hospital deaths, 4.21% were preceded by in-hospital CPR, and this differed by race (3.90% for white patients, 6.57% for black patients, and 5.83% for individuals of other races). Furthermore, the proportion of hospital deaths associated with in-hospital CPR increased more than 37% during the study period, from 3.78% in 1992 to 5.19% in 2005, and increased for each racial category (p<0.001, Figure 2). Similar patterns emerged when evaluating deaths following in-hospital CPR as a proportion of in- and out-of-hospital deaths (data not shown).
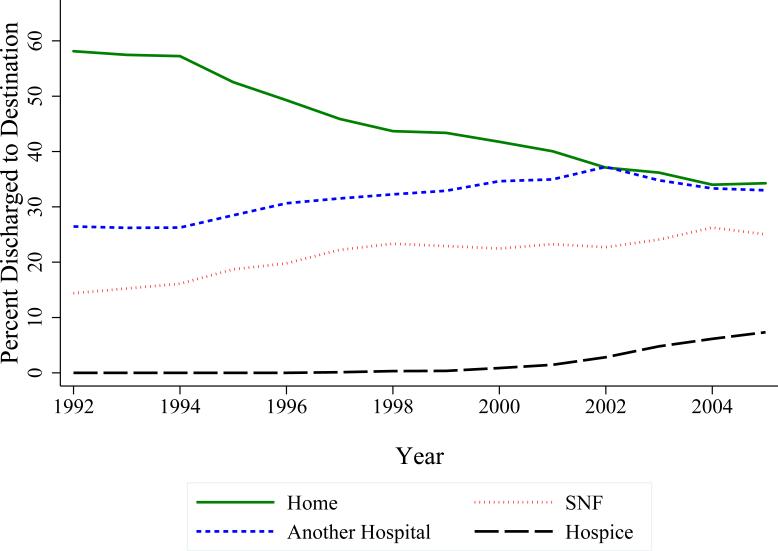
The proportion of survivors discharged home decreased during the study (Figure 3), while the proportion of patients discharged to hospice increased after 1997 when this designation was added to the database. These trends were all statistically significant (p<0.001).
Figure 3. Trends in Discharge Destination of Survivors of In-Hospital CPR.
Patients discharged home with or without home health or home IV services were included in the “Home” group. Patients discharged to a skilled nursing facility under Medicare or Medicaid were included in the “Skilled Nursing Facility” group. Patients discharged to another acute care hospital, intermediate care facility, long-term care hospital, swing bed within the same hospital, or a rehabilitation hospital were included in the “Another Hospital” group. The “Hospice” group included those discharged to hospice at home or a medical facility, and was used for years 1997 and beyond. All trends were highly statistically significant (p<0.001).
All patient and hospital characteristics except income were significantly associated with survival in bivariate analyses (p<0.001) and included in multivariable models. Differences between unadjusted analyses and the first multivariable model including patient and hospital characteristics (Table 2) were minimal, except the direction of the association between teaching status and survival reversed and was no longer significant. Non-white race was associated with significantly lower odds of survival compared to white patients. In the second multivariable model including indicator variables for individual hospitals, the association between black race and lower odds of survival remained strong but was slightly attenuated (Table 2), and the variability in survivorship among hospitals was statistically significant (p<0.001). The multivariable models were rerun including individuals missing income data with no substantial differences in results (data not shown).
Table 2.
Multivariable Analyses for Factors Associated with Survival to Discharge
| Analysis for Patient and Hospital Factors* | |||
| Predictor | Adjusted Odds Ratio | 95% CI | p-value |
| Age | 0.971 | 0.970 to 0.972 | < 0.001 |
| Male sex | 0.837 | 0.823 to 0.852 | < 0.001 |
| Race | |||
| White | Referent | -- | -- |
| Black | 0.701 | 0.674 to 0.729 | < 0.001 |
| All Other Races | 0.852 | 0.815 to 0.891 | < 0.001 |
| Deyo-Charlson score† | 0.927 | 0.919 to 0.935 | < 0.001 |
| Admission from SNF‡ | 0.603 | 0.539 to 0.674 | < 0.001 |
| Rural Hospital | 1.133 | 1.085 to 1.184 | 0.001 |
| No. of Hospital Beds§ | 0.975 | 0.965 to 0.985 | <0.001 |
| Cared for at Teaching Hospital | 1.002 | 0.974 to 1.073 | 0.379 |
| Analysis After Adjustment for Hospital where CPR was performedΔ | |||
| Predictor | Adjusted Odds Ratio | 95% CI | p-value |
| Age | 0.972 | 0.971 to 0.973 | < 0.001 |
| Male sex | 0.829 | 0.815 to 0.843 | < 0.001 |
| Race | |||
| White | Referent | -- | -- |
| Black | 0.764 | 0.741 to 0.788 | < 0.001 |
| All Other Races | 0.917 | 0.877 to 0.959 | < 0.001 |
| Deyo-Charlson score† | 0.930 | 0.922 to 0.938 | < 0.001 |
| Admission from SNF‡ | 0.690 | 0.646 to 0.738 | < 0.001 |
Multivariable logistic regression with empirical standard error estimates, accounting for clustering within hospital
OR is that seen when increasing from one category of Deyo-Charlson (0, 1, 2, or ≥3) score to the next
Skilled nursing facility
OR for every 100 additional hospital beds.
Logistic regression modeling survival to discharge and including an indicator variable for each of the 6,033 hospitals at which patients received CPR
DISCUSSION
We found that 18.3% of patients in this cohort of Medicare beneficiaries receiving in-hospital CPR survived to hospital discharge. With our analysis limited to older adults, it is surprising that survival was slightly higher than that seen in the NRCPR study of nearly 15,000 cardiac arrests in patients of all ages (17%).9 The over-representation of large, urban, academic hospitals in NRCPR may result in over-representation of patients with higher acuity of illness.
There are numerous possible explanations for our finding no increase in survival following in-hospital CPR from 1992 to 2005. One possibility is that attempts at enhancing CPR delivery have not improved outcomes after inpatient cardiopulmonary arrest. Systems changes in the out-of-hospital setting contributing to improved survival including widespread bystander CPR, emergency response crew-witnessed cardiac arrest, telephone dispatcher-assisted CPR, and automated external defibrillator use, do not have analogues in the in-hospital setting.20, 21 Another possibility is that cardiac arrest patients’ acuity of illness, underlying cause of cardiac arrest, or initial arrest rhythm have changed over time. Although all patients requiring CPR have severe acute illness by virtue of needing CPR, there may be differences in the type or severity of the acute illness leading to CPR that may influence outcomes. Perhaps declining cardiovascular mortality and morbidity, coupled with the increasing incidence of critical illnesses such as severe sepsis, has led to a decrease in the proportion of patients whose initial cardiac arrest rhythm is either ventricular fibrillation or ventricular tachycardia, both of which are associated with higher survival.9, 22-24 Therefore a static survival rate could occur if CPR delivery has actually improved but been offset by an increasing proportion of patients with non-survivable primary illnesses receiving CPR.
Overall cumulative incidence of CPR was 2.73 per 1000 hospital admissions and fell within the range of 1 to 5 per 1000 reported previously.25-28 An important finding of this study is that although the incidence of CPR did not change substantially during the study period, the proportion in-patient deaths preceded by CPR increased. Since we observed the same trend when the denominator was all beneficiary deaths, the movement towards more death in the home or hospice cannot explain this increase. While do-not-resuscitate (DNR) orders became more common throughout the 1980s, our findings suggest either a reversal in that trend or that DNR orders are not effectively limiting CPR in individuals unlikely to benefit from resuscitation.29 Perhaps this increase represents a trend towards poorer candidates for CPR being more likely to receive resuscitation, and if so, provides another potential explanation for the observed static survival following CPR. The significant increase in the proportion of survivors having discharge destinations other than home may indicate a trend towards poorer neurologic and functional outcomes among CPR survivors. However, this trend may be confounded by a shortening of inpatient hospitalizations during the study.30
The associations of greater age, male sex, and a higher chronic illness burden with poorer survival are not surprising. Our finding that residence in a skilled nursing facility prior to admission was associated with poorer survival provides further evidence that chronic illness impacts outcomes following CPR. Our finding that CPR in a smaller or non-metropolitan hospital was associated with greater survival is unexpected, although residual confounding by severity of acute illness is likely, given our inability to assess this factor.
We found a strong association between race and survival, with black and other non-white patients having significantly higher likelihood of receiving CPR and lower odds of survival. This association did not change when adjusted for patient factors but was slightly attenuated by adjusting for individual hospital, suggesting that the difference in survival between white and non-white patients may be partially explained by the fact that non-white patients were more likely to receive care in hospitals where patients had lower odds of survival following CPR, regardless of their race. Prior studies have found reduced survival in black individuals following both in- and out-of-hospital arrest, and recent work has reported that black race is associated with delayed defibrillation in the hospital.12-14 Initial cardiac arrest rhythm may differ by race, suggesting that differences in the biology of cardiac arrest, perhaps due to genetic and environmental factors, could partially explain racial differences in survival.13 It is also possible that the quality of care before, during, and after cardiac arrest is lower for black patients.31 Finally, recent findings suggest that systems factors may affect survival following CPR. For example, variations in survival by time of day appeared lower in hospitals with more extensive monitoring, suggesting that system-level variations in quality of care may help explain hospital differences in survival and between-hospital differences in systems facilitating rapid resuscitation may partially explain racial differences in survival.32, 33
We found the incidence of in-hospital CPR is higher and increasing faster for black patients than for other patients, a result mirroring the higher incidence of out-of-hospital cardiac arrest seen in black patients.13 This racial difference in incidence may result from higher chronic illness burden, as reflected by higher Deyo-Charlson scores, in black patients. The higher incidence and severity of diseases such as cardiovascular disease among black patients may also play a role in this difference.34 Thus, the increasing incidence of in-hospital CPR could partially result from increasing severity of acute and chronic illness among hospitalized black patients.
We also found that a higher proportion of black patients dying in the hospital received CPR compared to members of other racial groups, which coincides with evidence that black patients are more likely to receive higher intensity of care, including ICU care, at the end of life.35 This may result from black patients less frequently choosing DNR status, a mechanism that could also partially explain the difference in incidence of in-hospital CPR by race.36-38 If more commonly choosing to be resuscitated results in more CPR being performed among patients with lower likelihood of survival, this could account for much of the racial difference in survival.
There are several important limitations of this study. First, our definition of CPR is dependent on ICD-9 codes. This definition has not been validated within Medicare data, and the specificity and sensitivity may vary between hospitals. However, our estimates of CPR survival and incidence are similar to prior studies, supporting the accuracy of this definition. Furthermore, it is unlikely that the sensitivity and specificity have changed over time, making it likely that these trends in survival and incidence are accurate. Finally, short of conducting a detailed prospective observational study, validating our definition of in-hospital CPR within Medicare data is virtually impossible because there is no “gold standard” with which to compare it. A second limitation is the absence of some potential predictors of survival following CPR within MedPAR. These include severity and type of underlying acute illness, initial rhythm during arrest, location within the hospital, and time to defibrillation. Such features may be particularly important in understanding differences in survival by race and hospital. Finally, survival to discharge may not be the most clinically relevant outcome following CPR. The ability to evaluate longer term outcomes, including the degree of neurological impairment after CPR, would be valuable.
In summary, we found that survival to discharge following in-hospital CPR has not changed among Medicare beneficiaries 65 and older between 1992 and 2005. The incidence of in-hospital CPR has also not substantially changed during this time period. Of significant concern is our finding that the proportion of patients receiving CPR prior to death has increased during a time of more education and awareness about the limits of CPR in patients with advanced chronic illness and life-threatening acute disease.39 Our findings that survivors of in-hospital CPR are less frequently being discharged to home is also concerning, but may be confounded by trends toward shorter hospital stays. Factors associated with lower odds of survival included older age, male sex, chronic disease burden, and non-white race. Some, but not all, of the racial difference in survival appears to be attributable to the hospitals where patients receive care, with black patients more often receiving care at hospitals where patients of all races have lower odds of survival after CPR. We have also found that black patients are more likely to receive in-hospital CPR prior to death. A greater preference for CPR, despite prognosis, may provide another explanation for differences in survival by race. This study provides information useful to older patients and their clinicians when considering preferences for CPR since the proportion of elderly patients choosing CPR is directly related to the probability of survival presented to these patients.40 Our findings also provide stimulus for further research to better understand the association between race and survival, not only with the goal of eliminating racial disparities in the quality of medical care, but also to help understand factors associated with the occurrence of and survival following CPR for patients of all races.
ACKOWLEDGEMENTS
This work was supported by the ASP-CHEST Foundation of the American College of Chest Physicians-Geriatric Development Research Award funded by Atlantic Philanthropies, CHEST Foundation, the John A. Hartford Foundation, and the Association of Specialty Professors. It was also supported by a National Institutes of Health/National Center for Research Resources Roadmap K12 (8K12RR023265) and COBRE Awards (5P20RR015557) (Dr. Stapleton). Dr. Ehlenbach was supported by a National Institutes of Health training grant (T32 HL 007287). Dr. Barnato was supported by a National Institutes of Health career award (K08AG021921). The funding organizations played no role in the design and conduct of the study; in collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. The manuscript was reviewed by CMS Division of Privacy Compliance Data Development with the sole purpose of ensuring the protection of beneficiary privacy.
Footnotes
DISCLOSURE
None of the authors have relationships of any kind with commercial entities that have an interest in the subject of this study.
References
- 1.Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. Jama. 1960;173:1064–7. doi: 10.1001/jama.1960.03020280004002. [DOI] [PubMed] [Google Scholar]
- 2.Linko E, Koskinen PJ, Siitonen L, Ruosteenoja R. Resuscitation in cardiac arrest. An analysis of 100 successive medical cases. Acta medica Scandinavica. 1967;182:611–20. [PubMed] [Google Scholar]
- 3.Nachlas MM, Miller DI. Closed-Chest Cardiac Resuscitation in Patients with Acute Myocardial Infarction. American heart journal. 1965;69:448–59. doi: 10.1016/0002-8703(65)90414-x. [DOI] [PubMed] [Google Scholar]
- 4.Eisenberg MS, Bergner L, Hallstrom A. Out-of-hospital cardiac arrest: improved survival with paramedic services. Lancet. 1980;1:812–5. doi: 10.1016/s0140-6736(80)91305-7. [DOI] [PubMed] [Google Scholar]
- 5.Cobb LA, Fahrenbruch CE, Walsh TR, et al. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation. JAMA. 1999;281:1182–8. doi: 10.1001/jama.281.13.1182. [DOI] [PubMed] [Google Scholar]
- 6.Tresch D, Heudebert G, Kutty K, Ohlert J, VanBeek K, Masi A. Cardiopulmonary resuscitation in elderly patients hospitalized in the 1990s: a favorable outcome. J Am Geriatr Soc. 1994;42:137–41. doi: 10.1111/j.1532-5415.1994.tb04940.x. [DOI] [PubMed] [Google Scholar]
- 7.Warner SC, Sharma TK. Outcome of cardiopulmonary resuscitation and predictors of resuscitation status in an urban community teaching hospital. Resuscitation. 1994;27:13–21. doi: 10.1016/0300-9572(94)90016-7. [DOI] [PubMed] [Google Scholar]
- 8.Ebell MH, Becker LA, Barry HC, Hagen M. Survival after in-hospital cardiopulmonary resuscitation. A meta-analysis. J Gen Intern Med. 1998;13:805–16. doi: 10.1046/j.1525-1497.1998.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 10.Taffet GE, Teasdale TA, Luchi RJ. In-hospital cardiopulmonary resuscitation. Jama. 1988;260:2069–72. [PubMed] [Google Scholar]
- 11.Saklayen M, Liss H, Markert R. In-hospital cardiopulmonary resuscitation. Survival in 1 hospital and literature review. Medicine (Baltimore) 1995;74:163–75. doi: 10.1097/00005792-199507000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Ebell MH, Smith M, Kruse JA, Drader-Wilcox J, Novak J. Effect of race on survival following in-hospital cardiopulmonary resuscitation. J Fam Pract. 1995;40:571–7. [PubMed] [Google Scholar]
- 13.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–43. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 14.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 15.Begg CB, Riedel ER, Bach PB, et al. Variations in morbidity after radical prostatectomy. N Engl J Med. 2002;346:1138–44. doi: 10.1056/NEJMsa011788. [DOI] [PubMed] [Google Scholar]
- 16.Schermerhorn ML, O'Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008;358:464–74. doi: 10.1056/NEJMoa0707348. [DOI] [PubMed] [Google Scholar]
- 17.Arday SL, Arday DR, Monroe S, Zhang J. HCFA's racial and ethnic data: current accuracy and recent improvements. Health Care Financ Rev. 2000;21:107–16. [PMC free article] [PubMed] [Google Scholar]
- 18.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 19.Morrill R, Cromartie J, Hart G. Metropolitan, Urban, and Rural Commuting Areas: Toward a Better Depiction of the United States Settlement System. Urban geography. 1999:20. [Google Scholar]
- 20.Becker L, Gold LS, Eisenberg M, White L, Hearne T, Rea T. Ventricular fibrillation in King County, Washington: a 30-year perspective. Resuscitation. 2008;79:22–7. doi: 10.1016/j.resuscitation.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 21.Hollenberg J, Herlitz J, Lindqvist J, et al. Improved survival after out-of-hospital cardiac arrest is associated with an increase in proportion of emergency crew--witnessed cases and bystander cardiopulmonary resuscitation. Circulation. 2008;118:389–96. doi: 10.1161/CIRCULATIONAHA.107.734137. [DOI] [PubMed] [Google Scholar]
- 22.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. Jama. 2006;295:50–7. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 24.Wellenius GA, Mittleman MA. Disparities in myocardial infarction case fatality rates among the elderly: the 20-year Medicare experience. American heart journal. 2008;156:483–90. doi: 10.1016/j.ahj.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skogvoll E, Isern E, Sangolt GK, Gisvold SE. In-hospital cardiopulmonary resuscitation. 5 years’ incidence and survival according to the Utstein template. Acta Anaesthesiol Scand. 1999;43:177–84. doi: 10.1034/j.1399-6576.1999.430210.x. [DOI] [PubMed] [Google Scholar]
- 26.Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation. 2002;54:115–23. doi: 10.1016/s0300-9572(02)00098-9. [DOI] [PubMed] [Google Scholar]
- 27.Sandroni C, Ferro G, Santangelo S, et al. In-hospital cardiac arrest: survival depends mainly on the effectiveness of the emergency response. Resuscitation. 2004;62:291–7. doi: 10.1016/j.resuscitation.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 28.Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33:237–45. doi: 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 29.Wenger NS, Pearson ML, Desmond KA, Kahn KL. Changes over time in the use of do not resuscitate orders and the outcomes of patients receiving them. Med Care. 1997;35:311–9. doi: 10.1097/00005650-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Kaplan SJ. Growth and payment adequacy of medicare postacute care rehabilitation. Arch Phys Med Rehabil. 2007;88:1494–9. doi: 10.1016/j.apmr.2007.08.112. [DOI] [PubMed] [Google Scholar]
- 31.Virnig BA, Lurie N, Huang Z, Musgrave D, McBean AM, Dowd B. Racial variation in quality of care among Medicare+Choice enrollees. Health Aff (Millwood) 2002;21:224–30. doi: 10.1377/hlthaff.21.6.224. [DOI] [PubMed] [Google Scholar]
- 32.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. Jama. 2008;299:785–92. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 33.Jones-Crawford JL, Parish DC, Smith BE, Dane FC. Resuscitation in the hospital: circadian variation of cardiopulmonary arrest. Am J Med. 2007;120:158–64. doi: 10.1016/j.amjmed.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 34.Watkins LO. Epidemiology and burden of cardiovascular disease. Clin Cardiol. 2004;27:III2–6. doi: 10.1002/clc.4960271503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barnato AE, Chang CC, Saynina O, Garber AM. Influence of race on inpatient treatment intensity at the end of life. J Gen Intern Med. 2007;22:338–45. doi: 10.1007/s11606-006-0088-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wenger NS, Pearson ML, Desmond KA, et al. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995;155:2056–62. [PubMed] [Google Scholar]
- 37.Levy CR, Fish R, Kramer A. Do-not-resuscitate and do-not-hospitalize directives of persons admitted to skilled nursing facilities under the Medicare benefit. J Am Geriatr Soc. 2005;53:2060–8. doi: 10.1111/j.1532-5415.2005.00523.x. [DOI] [PubMed] [Google Scholar]
- 38.Shepardson LB, Gordon HS, Ibrahim SA, Harper DL, Rosenthal GE. Racial variation in the use of do-not-resuscitate orders. J Gen Intern Med. 1999;14:15–20. doi: 10.1046/j.1525-1497.1999.00275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jackson EA, Yarzebski JL, Goldberg RJ, et al. Do-not-resuscitate orders in patients hospitalized with acute myocardial infarction: the Worcester Heart Attack Study. Arch Intern Med. 2004;164:776–83. doi: 10.1001/archinte.164.7.776. [DOI] [PubMed] [Google Scholar]
- 40.Murphy DJ, Burrows D, Santilli S, et al. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330:545–9. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]