Abstract
This study examines the longitudinal relationship between personal and sexual partner incarceration and subsequent HIV risk behaviors among drug-involved men and their primary female sexual partners. A random sample of 356 men in methadone treatment in New York City were interviewed at baseline, 6 and 12 months; these men also reported information on their primary female sexual partners. Female partner recent incarceration was associated with subsequent increase in multiple partnerships for the male participants (AOR: 3.31; 95% C.I.: 1.26–8.72, P < .05). Female partner incarceration was also associated with reduced likelihood of subsequent unprotected sex between primary partners (AOR: .13; 95% C.I.: .05–.40, P < .01); this finding is somewhat unique and warrants further investigation. Findings support the notion of mutual influence in the case of female partner incarceration, which is associated with both female partner and male partner risk behaviors. HIV prevention implications are discussed, including the need for couple-based HIV prevention interventions targeting couples affected by incarceration.
Keywords: Incarceration, HIV risk, Couples, Methadone, HIV prevention
Introduction
The criminal justice system has become an epicenter of the United States HIV/AIDS epidemic over the past decade. Increased prevalence of HIV has been demonstrated in studies of currently and formerly incarcerated men and women [1–3]; the reported overall prevalence of HIV in jail and prison inmates is approximately 2%[2] and HIV rates as high as 12–17% are reported among men and women on probation and parole [4, 5]. Incarceration is also linked to post-release sexual risk behaviors in the community such as unprotected sex [6, 7], multiple and/or concurrent sexual partnerships [8, 9], and trading sex for money or drugs [3]. In an event-level study of men being released from prison, two-thirds engaged in vaginal sex within a week of release, and less than one-fourth used a condom;[10] additional research has noted similar post-release risk behaviors among formerly incarcerated men [7, 11]. The growing awareness of the burden of HIV risk among offenders has led to identification of the criminal justice system as an important arena for HIV prevention [12, 13].
Each year, approximately 600,000 men and women are discharged from state and federal prisons; in addition there are an annual 7 million releases from local jails to the community [14]. More than half of released prisoners are estimated to return to their sexual partners in the community [15]. Incarcerated populations also bear high levels of social and economic disadvantage and drug use, which are strong determinants of HIV risk and infection [16–19]. Given the high prevalence of HIV infection among inmate populations and high levels of sexual risk-taking documented to occur after release from incarceration, intimate partners of former prisoners represent a large group at substantial risk of HIV acquisition.
Recent research has begun to describe effects of incarceration on intimate partner HIV risk. In a qualitative study of female offenders in the community, a male partner's incarceration was viewed as an opportunity to engage in sexual relationships with additional partners [20]. There is also epidemiologic evidence, albeit limited, that sexual partnership with a former inmate is associated with recent multiple new partnerships and transactional sex [8, 21]. Further, HIV infection appears to be common among the partners of persons with an incarceration history [22]. While this research suggests the potential influence of incarceration on sexual partner HIV/STI risk, most related studies have been limited by cross-sectional analyses and cannot therefore establish the temporal ordering of incarceration exposure to sexual risk behavior outcomes.
Theoretical Perspective
Although early approaches to the epidemiology and prevention of HIV tended to be individual-focused, recognizing sexual HIV risk-taking as a confluence of individual, interpersonal and structural factors associated with each sexual partner is essential to effective HIV prevention [23]. Social ecological principles, which emphasize the transactions between individuals, have been utilized to study dyadic processes as determinants of couple behavior, particularly in intimate partnerships [24, 25]. Within sexual partnerships, each person's sexual behavior is unlikely to be independent of his/her partner's behaviors and characteristics. The social ecological model of interdependence describes the relationship between factors associated with each partner and his/her own outcomes (actor effects) as well as the potential influence on his/her sexual partner's outcomes (partner effects) [26]. Lewis et al. [27] describe this concept as “mutual influence”—that each individual's outcomes may be affected by factors associated with themselves as well as factors associated with their sexual partner.
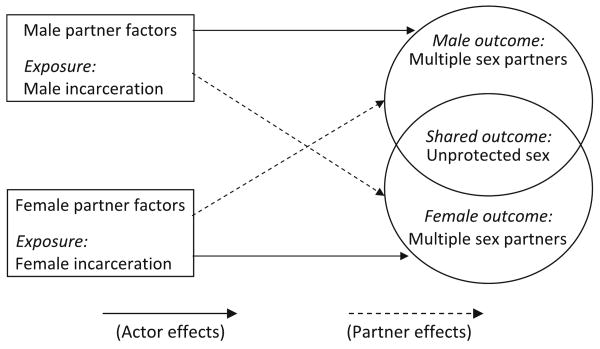
The purpose of this paper is to examine the longitudinal relationship between personal and sexual partner incarceration and subsequent HIV risk among drug-involved men and their primary female sexual partners. The research incorporates a social ecology perspective to conceptualize the actor and partner effects of incarceration on HIV risk while utilizing longitudinal data to model temporal relationships (Fig. 1). This paper will address the research question: Is male and/or female partner incarceration associated with: (1) Male multiple sex partnerships; (2) Female multiple sex partnerships; and (3) Unprotected sex between primary partners, controlling for male and female demographics, social disadvantage, and drug use? Findings from this study will improve our understanding of the context of HIV risk for couples affected by incarceration—a large and understudied population that is vulnerable to HIV infection.
Fig. 1.
Interdependence model of male and female incarceration on sexual risk behavior outcomes. Solid lines represent actor effects; dashed lines represent partner effects
Methods
Participants
The data presented in this paper come from a longitudinal study examining substance abuse and HIV risk among male methadone maintenance clients, who also reported information on their primary female sexual partners. Eligibility criteria for the study were: (1) being male aged 18 or over; (2) being enrolled in methadone treatment for at least 3 months; and (3) during the past year, having a sexual relationship with a woman described as a girlfriend, spouse, regular sexual partner, or the mother of his children. Using a random number generator in SPSS, we randomly selected 1,272 men from enumerated client lists of seven methadone clinics in New York City. A total of 774 men (61%) agreed to participate in a 15-min screening interview. After screening, 356 men (46%) met eligibility criteria and completed a baseline structured interview. Over 80% (289) participated in a 6-months follow-up interview, and 280 completed a 12-months follow-up interview. The institutional review boards for the participating methadone programs and Columbia University approved the study protocol. Detailed recruitment procedures have been described previously [28].
Measurement
At each assessment point, male respondents identified if they had a primary female sexual partner during the previous 6 months. Male participants were asked detailed questions about their female partner, including partner sociodemographic characteristics, substance use, sexual risk behavior, and HIV status.
Outcomes: Sexual HIV risk
Sexual risk behavior was measured by an instrument developed through use with more than 1,000 subjects in drug treatment [29, 30]. For the purpose of this paper, three primary HIV risk outcomes were defined: (1) Unprotected sex between primary partners was defined as one or more acts of unprotected vaginal or anal sex between the male participant and his primary female partner in the past 6 months. (2) Male multiple sex partnerships was defined as whether the male participant reported having more than one sexual partner in the past 6 months. (3) Female multiple sex partnerships was reported by the male participant on whether his primary female partner was known to have had more than one sexual partner in the past 6 months.
Exposure: Male participant and female partner incarceration
Male participants reported lifetime and past 6 months incarceration histories for themselves and their primary female partners. Personal recent incarceration was defined as the male participant having been incarcerated in jail or prison in the past 6 months, and partner's recent incarceration described whether the female partner was incarcerated in the past 6 months. For those incarcerated in the past 6 months, length of incarceration in days was reported.
Potential confounding covariates
At each time point, male participants reported sociodemographic information for themselves and their primary female partner, including: (1)Male: age, race/ethnicity, years of education, past 6-months unemployment, past 6-months homelessness, and average monthly income; (2) Female: age, race/ethnicity, years of education, being on welfare in the past 6 months, and past 6-months unemployment. Drug abuse histories for the male participant and female partner were measured using the Drug Use and Risk Behavior Questionnaire [30]. Recent drugs used was defined for each partner as the number of types of illicit drugs used over the past 6 months, including heroin, powder cocaine, crack, prescription drugs used without a prescription, any injection drug, and other drugs (range: 0–6).
Statistical Analysis
Utilizing baseline data, descriptive statistics were generated for male participants and female partners separately. Sociodemographic, drug use, and HIV risk variables were assessed for male participants and female partners and stratified by whether their primary partner had a lifetime incarceration history. Differences between those with and without a formerly incarcerated partner were tested using difference in means t-tests for continuous variables and chi-square tests of independence for dichotomous variables.
Approximately 80% of the sample was retained throughout the three waves of the study. To reduce the potential bias of missing data and differential attrition due to loss to follow-up in the longitudinal data, multiple imputation was employed using the MICE function in Stata 10 [31]. This process entailed creating a number of copies of the complete data (in this case, five copies were made), each of which had missing values imputed from prediction models based on the existing (observed) data. Subsequent estimates of variables of interest were averaged across the created datasets to give a single estimate, which takes into account the variation between values imputed in each dataset. It should be noted that all longitudinal analyses were conducted with both non-imputed and imputed data, and no significant differences were noted between the two models (no point estimates crossed the α = .05 level in either direction).
We used logistic regression with generalized estimating equations (GEE) to estimate unadjusted and adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between incarceration indicators and each sexual HIV risk outcome. GEE accounts for the potential correlation between repeated measures by noting that the data are clustered by the individual participant over time. There is evidence that in small to moderate sample sizes, using GEE on data which has been multiply imputed results in a model more accurate than competing models [32, 33].
To establish temporality, we estimated regression models to predict sexual HIV risk outcomes by lagged values of male participant and female partner incarceration, adjusting for lagged values of control variables. The adjusted models included the following male participant and female partner variables: Male participant: age, race/ethnicity, years of education, past 6-months homelessness, average monthly income, recent drugs used and HIV status; Female partner: age, race/ethnicity, years of education, being on welfare in the past 6 months, recent drugs used and HIV status. Additionally, each adjusted model controlled for lagged measurement of the outcome of interest. Lastly, because we expected drug use to have strong associations with sexual risk behaviors, we also controlled for recent drugs used by each partner concurrent to the outcome timeframe.
Results
Background Characteristics by Primary Partner Incarceration History
Table 1 presents demographic and HIV risk characteristics for the male participants and their female partners stratified by whether their primary partner had a lifetime history of incarceration. The male participants and their primary female partners identified predominantly as either Black or Latino and displayed high levels of unemployment. Men whose primary female partner had an incarceration history were more likely to have been recently homeless (29.6% vs. 13.5%, P < .001), and women whose primary male partner had an incarceration history displayed higher levels of welfare enrollment (45.1% vs. 27.5%, P < .01). For both the male participants and female partners in this study, having a primary partner with an incarceration history indicated an increased likelihood of having their own injection drug use history and incarceration history. Additionally, HIV prevalence was higher among those whose primary partner had a history of incarceration than those whose primary partner had never been incarcerated (men: 23.5% vs. 11.6%, P < .01; women: 9.5% vs. 3.3%, P < .05). Lastly, higher levels of recent multiple sex partnerships were noted among men (42% vs. 23%, P < .001) and women (7.6% vs. 2.2%, P < .001) who had a previously incarcerated primary partner.
Table 1.
Baseline characteristics of male participants and reported characteristics of female partners stratified by primary partner lifetime history of incarceration
| Male participant (N = 356) | Female partner (N = 356) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Primary female partner: no incarceration history (n = 275) |
Primary female partner: history of incarceration (n = 81) |
t-value (df = 354) |
Primary male partner: no incarceration history (n = 92) |
Primary male partner: history of incarceration (n = 264) |
t-value (df = 354) |
|||||
| Continuous variables | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Age (years) | 43.2 | 8.36 | 45.1 | 9.01 | −1.80 | 38.9 | 9.44 | 39.7 | 8.62 | −.72 |
| Years of education | 11.74 | 2.21 | 11.25 | 2.61 | 1.70 | 12.63 | 2.93 | 12.18 | 1.45 | 1.45 |
| Monthly income (dollars) | 1,007 | 963 | 883 | 768 | 1.07 | Na | – | – | – | – |
| Drugs used in past 6-months | 1.51 | 1.40 | 1.74 | 1.49 | −1.29 | .60 | 1.00 | .72 | 1.00 | −1.00 |
| Dichotomous variables | n | % | n | % | χ2(df = 1) | n | % | n | % | χ2 (df = 1) |
| Race/ethnicity: Black | 97 | 35.3 | 36 | 44.4 | 2.25 | 26 | 28.3 | 96 | 36.4 | 2.00 |
| Race/ethnicity: Latino | 133 | 48.4 | 28 | 34.6 | 4.81* | 44 | 47.8 | 114 | 43.2 | .60 |
| Unemployed past 6-months | 121 | 44.0 | 48 | 59.2 | 5.84* | 36 | 39.1 | 134 | 50.8 | 3.70* |
| Homeless past 6-months | 37 | 13.5 | 24 | 29.6 | 11.53*** | Na | – | – | – | – |
| On welfare past 6-months | Na | – | – | – | – | 25 | 27.5 | 119 | 45.1 | 8.70** |
| History of injection drug use | 183 | 66.6 | 66 | 81.5 | 6.64** | 12 | 13.0 | 82 | 31.0 | 11.40*** |
| Lifetime incarceration history | 191 | 69.5 | 73 | 90.1 | 13.95*** | 8 | 8.7 | 73 | 27.7 | 13.95*** |
| HIV positive | 32 | 11.6 | 19 | 23.5 | 7.12** | 3 | 3.3 | 25 | 9.5 | 3.70* |
| Unprotected sex past 6-months | 188 | 23.0 | 50 | 61.7 | 7.46** | 61 | 66.3 | 177 | 67.1 | .10 |
| Multiple partners past 6-months | 63 | 23.0 | 34 | 42.0 | 68.85*** | 2 | 2.2 | 20 | 7.6 | 20.60*** |
NA Not applicable: this variable was not measured
P < .05,
P < .01,
P < .001
Prevalence of Incarceration and Sexual HIV Risk Outcomes (Fig. 2)
Fig. 2.
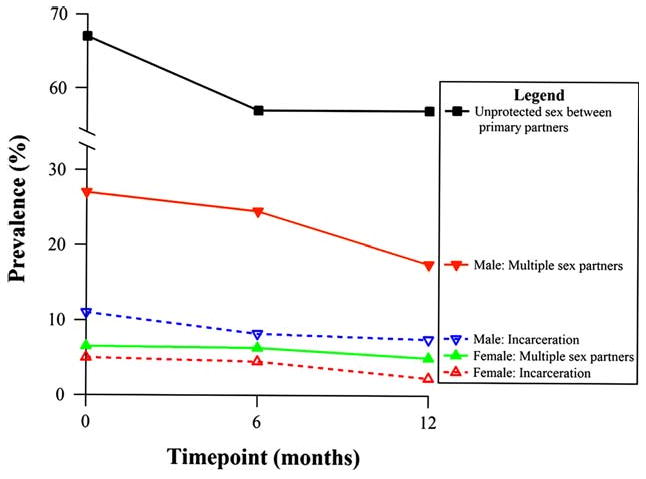
Recent incarceration (dashed lines) and sexual risk behaviors (solid lines) over time for male participants and reported characteristics for primary female partners
Across the three waves of the study, past 6-months incarceration ranged from 7.5 to 11% among men and 2.3 to 5.1% among female partners; mean length of incarceration was 14.1 days (SD: 29.1, Range: 0–97 days) among men and 5.5 days (SD: 16.7; Range: 0–90 days) among female partners. Unprotected sex between primary partners ranged from 57 to 67%. Multiple sex partnerships ranged from 17.6 to 27% for men and 5 to 6.2% for female partners.
Longitudinal Association Between Incarceration and Unprotected Sex
Table 2 displays GEE logistic regression results for the longitudinal associations between male participant and female partner recent incarceration and sexual risk behaviors. Male recent incarceration was not significantly associated with subsequent unprotected sex between primary partners. However, in both the unadjusted and adjusted models, female partner recent incarceration was significantly associated with lower odds of subsequent unprotected sex between within the primary partnership (Adjusted odds ratio [AOR]: .13; 95% CI: .05–.40, P < .01).
Table 2.
Generalized estimating equations (GEE) logistic regression results: Odds ratios and 95% confidence intervals (CIs) for the longitudinal associations between male participant and female partner past six-months incarceration and sexual risk behaviors
| Unprotected sex between primary partners: past 6-months | Male participant: multiple sex partnerships: past 6-months | Female partner: multiple sex partnerships: past 6-months | ||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | Unadjusted | Adjusteda | |
| Male partner: incarcerated past 6-months | 1.14 (.53–2.44) | 1.20 (.55–2.62) | 1.87 (.91–3.83) | 1.57 (.61–4.03) | .81 (.11–5.72) | .52 (.05–5.75) |
| Female partner: incarcerated past 6-months | .40* (.19–.87) | .13** (.05–.40) | 3.28** (1.45–7.42) | 3.31* (1.26–8.72) | 3.40* (1.10 –10.52) | 1.95 (.41–9.30) |
P < .05,
P < .01
Models adjusted for the following lagged variables: Male partner: age, race/ethnicity, years of education, past 6-months homelessness, average monthly income, recent drugs used, and HIV status; Female partner: age, race/ethnicity, years of education, being on welfare in the past 6 months, recent drugs used, and HIV status. Each adjusted model is also controlled for lagged measurement of the model outcome and each partner's recent drugs used concurrent to the outcome timeframe
Longitudinal Association Between Incarceration and Multiple Sex Partnerships
Male Participants
Among men, recent personal incarceration was not significantly associated with subsequent multiple sex partnerships (AOR: 1.57; 95% CI: .61–4.03, P > .05). However, men whose female partner was recently incarcerated reported much higher levels of subsequent multiple partnerships than men whose primary partner had not been recently incarcerated (AOR: 3.31; 95% CI: 1.26–8.72, P < .05).
Female Partners of Male Participants
Among female partners, recent personal incarceration was strongly associated with subsequent multiple sex partnerships in the unadjusted model (OR: 3.40; 95% CI: 1.10–10.52, P < .05). This longitudinal association was attenuated and no longer significant in the adjusted analysis (AOR: 1.95; 95% CI: .41–9.30, P < .05). Among female partners, recent incarceration of their male partner was not significantly associated with subsequent multiple sex partnerships in the unadjusted or adjusted models.
Discussion
For the men in this study and their primary female partners, having a sexual partner with a lifetime incarceration history is a marker for several risk factors, including one's own incarceration history, HIV infection, injection drug use history, unemployment, and homelessness. This confluence of risk factors for both individuals and couples in the study highlights the intersecting and potentially cumulative HIV/STI risks faced by couples affected by incarceration [18]. For this reason, couples in which one or both partners has a history of incarceration are a group particularly vulnerable to HIV acquisition and/or transmission and are therefore an important yet understudied population.
To our knowledge, this is the first longitudinal study to examine the actor and partner effects of incarceration on sexual HIV risk among drug-involved men and their female sexual partners. The findings support the social ecology principle of mutual influence, particularly in the case of female incarceration. In this longitudinal study, men whose female partner had been recently incarcerated reported much higher levels of multiple partnerships in the following 6 months, which could be interpreted as a partner effect. This longitudinal association remained significant despite controlling for numerous male and female partner characteristics as well as prior likelihood of multiple partnerships among male participants and each partner's drug use during the period of both exposure and outcome. Incarceration has been described as a disruptive life event that destabilizes intimate relationships, which helps to explain previously found associations between one's own incarceration and multiple sex partnerships [34, 35]. This study adds to extant research by suggesting that the disruption caused by a woman's incarceration could similarly affect her male partner and influence his likelihood to seek out additional sex partners as a result. This finding demonstrates that analytic models which incorporate factors associated with each sexual partner are a useful tool in clarifying risk relationships between and among couples.
Although female partner incarceration was associated with subsequent female multiple partnerships in the unadjusted model, the estimate in the fully-adjusted model was substantially weakened and no longer significant. The attenuated estimate was due primarily to the inclusion of lagged female multiple partnerships, which was strongly associated with both female incarceration and subsequent female multiple partnerships. The female partners in this study who became incarcerated appear likely to have engaged in multiple partnerships before their incarceration and to resume this behavior upon release.
Among the male participants in this study, recent personal incarceration was not longitudinally associated with multiple partnerships, which is somewhat consistent with previous research on drug using populations [34]. Although this study builds on prior research by employing a longitudinal design, we would caution against interpreting these results as conclusive evidence that male incarceration does not contribute to subsequent multiple partnerships. Considering nearly three-fourths of the men in this study had a lifetime history of incarceration, the incidence of incarceration at any one time point may not signify a uniquely stressful and disruptive event for these men or their female partners. Among men with less intense criminal justice histories, it is plausible that incarceration may be experienced as a more negative and disruptive occurrence and therefore more likely to influence sexual risk taking. Additionally, prior research has linked concurrent (but not multiple) sex partnerships to incarceration among drug-involved men [34], which underscores the importance of evaluating a variety of risk indicators in longitudinal studies in order to more fully understand the relationship between incarceration and sexual risk.
It is also important to note that the exposure of recent incarceration measured in this study was generally brief, as no individual experienced a recent incarceration longer than approximately 3 months, and the majority of recent incarcerations were less than 1 week in duration. The findings should therefore be framed with an understanding of the exposure as short-term incarceration in jail, which is far more prevalent in the US criminal justice system than longer-term prison incarcerations [36], and in previous research short-term incarceration was a stronger predictor of sexual risk-taking than long-term incarceration [21]. While the findings demonstrate fairly strong associations between recent female partner incarceration and subsequent sexual risk behaviors, we would expect the incarceration/sexual risk behavior relationship may look considerably different for both men and women in the case of longer-term incarceration.
The finding that female partner incarceration was associated with reduced likelihood of subsequent unprotected sex between primary partners was somewhat surprising, given prior evidence of association between incarceration and unprotected sex [6, 7, 9, 37]. However, most past research has focused on male incarceration; this study's finding could be illustrating a difference in gender dynamics with respect to effects of incarceration on condom use. Female incarceration is somewhat rare, and incarcerated women are more likely to be involved in drug use than their male counterparts [38]. Given the unadjusted association between female partner incarceration and multiple partnerships and the strong association between female partner incarceration and male multiple partnerships, one or both partners may experience heightened perceived HIV/STI risk after the female partner's incarceration, which may affect decision-making around condom use. Although this explanation infers that couples affected by incarceration may make attempts to mitigate their risk for HIV/STI's, this view is countered by the findings on both male and female multiple partnerships, which is considered an important determinant of HIV/STI transmission [39, 40]. Nonetheless, this unique finding should be explored further in research on the relationship between a woman's incarceration and subsequent condom use behaviors with primary and casual partners.
Several potential limitations of this research should be discussed. The study relies upon self-reported data, with no biological or case record confirmation of variables such as HIV status, drug use, and incarceration. A particularly weighty limitation is that all female partner data was collected via third-party reporting by the male participants. This could lead to under-reporting of female partner information due to misinformation, poor recall, or social desirability. Future research which collects data directly from both partners would significantly improve the validity of study findings. Second, the design of this study tests the effect of episodic incarceration on subsequent HIV risk behavior, and as such does not allow for an examination of the potentially cumulative HIV risk effects of repeated incarceration. Although sexual activity during incarceration is an important aspect of HIV risk [41], this study did not measure potential sexual activity while incarcerated. Additionally, although the inclusion of relationship length in preliminary analyses did not substantially alter this study's findings, couple-level variables describing the duration and quality of relationship should be assessed and considered in future dyadic research. Lastly, while multiple imputation is preferable to other techniques that operate under more strict assumptions, this method does assume that data are missing at random.
These limitations duly noted, the dyadic and longitudinal analyses in this paper are unique among research on incarceration and sexual HIV risk. This study underscores the need for further research on the dyadic and sexual network effects of incarceration on sexual risk-taking. The findings also support the need for continued application of theoretical perspectives such as social ecology, which can be incorporated to conceptualize how factors associated with each partner may have effects on both partners' sexual behaviors. An equally compelling rationale for couple-based research is the vast number of incarcerated men and women released from prisons and jails each year, more than half of whom return to primary sexual partnerships [42]. Given the high prevalence of HIV among prisoners and the association between incarceration and HIV risk behaviors, understanding how incarceration impacts HIV risk for sexual partners of incarcerated populations is an important public health issue [43].
The findings in this study call attention to the potential importance of couple-based HIV prevention for couples affected by incarceration. Research has consistently found that most couples in established relationships do not use condoms regularly, even if they are involved in drug use or engage in additional sexual HIV risks [44, 45]. HIV prevention interventions with couples affected by incarceration could raise both partners' awareness of risk factors associated with personal and partner incarceration and thus develop a more realistic appraisal of contracting HIV. Based on this study's finding and previous research [9, 21], HIV prevention efforts could include information on the association between incarceration and multiple sex partnerships and planning strategies for safer sex and HIV testing with these partners.
Individual HIV prevention efforts targeting only incarcerated persons would not be sufficient to address the potential outside risks that non-incarcerated partners engage in either during or after their partner's incarceration. HIV prevention interventions for couples are less common than individual approaches in general, and to our knowledge there are no current couple-based HIV prevention trials specifically targeting incarcerated populations. Engaging couples affected by incarceration is challenging and requires creative recruitment and implementation strategies. Moreover, couple-based HIV prevention among partnerships affected by incarceration should focus on community reentry of the incarcerated partner as a time of high exposure to risk behaviors [10]. Additionally, relationship maintenance practices during incarceration such as increased access to communication and visitation between the incarcerated and non-incarcerated partner may have protective effects against external partnerships and risk-taking.
In conclusion, the findings from this study add to a body of research highlighting health effects associated with incarceration and stress the importance of viewing criminal justice practices as not only an issue of public safety but also of public health. The United States bears the highest incarceration rates in the world and continues to demonstrate gross health disparities for those involved in the criminal justice system. A growing body of evidence suggests that incarceration has an influence on HIV risks, and that these extend beyond incarcerated populations to their primary and secondary sexual networks. HIV prevention interventions targeting couples affected by incarceration is an important piece in a continuum of HIV prevention which could ultimately affect a large and vulnerable population.
Acknowledgments
Dr. Epperson's research is supported by a postdoctoral fellowship from the National Institute of Mental Health awarded to the Center for Behavioral Health Services and Criminal Justice Research (T32MH070313, Principal Investigator Nancy Wolff). The parent study was supported by a grant from the National Institute on Drug Abuse (R01DA012335, Principal Investigator Nabila El-Bassel).
Contributor Information
Matthew W. Epperson, Center for Behavioral Health Services & Criminal Justice Research, Rutgers, The State University of New Jersey, 176 Ryders Lane, New Brunswick, NJ 08901, USA, mwepperson@gmail.com; Social Intervention Group, Columbia University School of Social Work, New York, NY, USA
Maria R. Khan, School of Public Health, University of Maryland, College Park, MD, USA
Nabila El-Bassel, Social Intervention Group, Columbia University School of Social Work, New York, NY, USA.
Elwin Wu, Social Intervention Group, Columbia University School of Social Work, New York, NY, USA.
Louisa Gilbert, Social Intervention Group, Columbia University School of Social Work, New York, NY, USA.
References
- 1.Kim A, Page-Shafer K, Ruiz J, et al. Vulnerability to HIV among women formerly incarcerated and women with incarcerated sexual partners. AIDS Behav. 2002;6(4):331–8. [Google Scholar]
- 2.Maruschak LM. HIV in Prisons and Jails, 2002. Bur Justice Stat Spec Rep. 2004:1–11. NCJ 205333. [Google Scholar]
- 3.Epperson M, El-Bassel N, Gilbert L, Orellana E, Chang M. Increased HIV risk associated with criminal justice involvement among men on methadone. AIDS Behav. 2008;12(1):51–7. doi: 10.1007/s10461-007-9298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belenko S, Langley S, Crimmins S, Chaple M. HIV risk behaviors, knowledge, and prevention education among offenders under community supervision: a hidden risk group. AIDS Educ Prev. 2004;16(4):367–85. doi: 10.1521/aeap.16.4.367.40394. [DOI] [PubMed] [Google Scholar]
- 5.Martin S, O'Connell D, Inciardi J, Surratt H, Beard R. HIV/AIDS among probationers: an assessment of risk and results from a brief intervention. J Psychoactive Drugs. 2003;35(4):435–43. doi: 10.1080/02791072.2003.10400490. [DOI] [PubMed] [Google Scholar]
- 6.Werb D, Kerr T, Small W, Li K, Montaner J, Wood E. HIV risks associated with incarceration among injection drug users: implications for prison-based public health strategies. J Public Health. 2008;30(2):126–32. doi: 10.1093/pubmed/fdn021. [DOI] [PubMed] [Google Scholar]
- 7.MacGowan R, Margolis A, Gaiter J, et al. Predictors of risky sex of young men after release from prison. Int J STD AIDS. 2003;14:519–23. doi: 10.1258/095646203767869110. [DOI] [PubMed] [Google Scholar]
- 8.Khan MR, Wohl DA, Weir SS, et al. Incarceration and risky sexual partnerships in a southern US city. J Urban Health. 2008;85(1):100–13. doi: 10.1007/s11524-007-9237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Margolis A, MacGowan R, Grinstead O, Sosman J, Kashif I, Flanigan T. Unprotected sex with multiple partners: implications for HIV prevention among young men with a history of incarceration. Sex Transm Dis. 2006;33(3):175–80. doi: 10.1097/01.olq.0000187232.49111.48. [DOI] [PubMed] [Google Scholar]
- 10.Morrow KM, Eldridge G, Nealey-Moore J, Grinstead O. HIV, STD, and hepatitis risk in the week following release from prison: an event-level analysis. J Correct Health Care. 2007;13(1):27–38. [Google Scholar]
- 11.Stephenson BL, Wohl DA, Golin CE, Tien HC, Stewart P, Kaplan AH. Effect of release from prison and re-incarceration on the viral loads of HIV-infected individuals. Public Health Rep. 2005;120(1):84–8. doi: 10.1177/003335490512000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vlahov D, Putnam S. From corrections to communities as an HIV priority. J Urban Health. 2006;83(3):339–48. doi: 10.1007/s11524-006-9041-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freudenberg N, Daniels J, Crum M, Peridns T, Richie BE. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2005;95(10):1725–36. doi: 10.2105/AJPH.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freudenberg N. Coming home from jail: a review of health and social problems facing US jail populations and of opportunities for reentry interventions. Washington, DC: Urban Institute; 2006. [Google Scholar]
- 15.Grinstead O, Zack B, Faigeles B, Grossman N, Blea L. Reducing postrelease HIV risk among male prison inmates: a peer-led intervention. Crim Justice Behav. 1999;26:453–65. [Google Scholar]
- 16.Kral A, Bluthenthal M, Booth R, Watter J. HIV seroprevalence among street-recruited injection drug and crack cocaine users in 16 US municipalities. Am J Public Health. 1998;88(1):108–13. doi: 10.2105/ajph.88.1.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Rep. 2002;117(Supplement 1):S135–45. [PMC free article] [PubMed] [Google Scholar]
- 18.Conklin T, Lincoln T, Tuthill R. Self-reported health and prior health behaviors of newly admitted correctional inmates. Am J Public Health. 2000;90(12):1939–41. doi: 10.2105/ajph.90.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wingood GM, DiClemente RJ. The influence of psychosocial factors, alcohol, drug use on African-American women's high-risk sexual behavior. Am J Prev Med. 1998;15(1):54–9. doi: 10.1016/s0749-3797(98)00027-0. [DOI] [PubMed] [Google Scholar]
- 20.Epperson M, Platais I, Valera P, Barbieri R, Gilbert L, El-Bassel N. Fear, trust, and negotiating safety: HIV risk contexts for Black women defendants. Affilia. 2009;24(3):257–71. doi: 10.1177/0886109909337377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan MR, Miller WC, Schoenbach VJ, et al. Timing and duration of incarceration and high-risk sexual partnerships among African Americans in North Carolina. Ann Epidemiol. 2008;18(5):403–10. doi: 10.1016/j.annepidem.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adimora AA, Schoenbach VJ, Martinson FE, et al. Heterosexually transmitted HIV infection among African Americans in North Carolina. J Acquir Immune Defic Syndr. 2006;41(5):616–23. doi: 10.1097/01.qai.0000191382.62070.a5. [DOI] [PubMed] [Google Scholar]
- 23.Latkin CA, Knowlton AR. Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care. 2005;17:102–13. doi: 10.1080/09540120500121185. [DOI] [PubMed] [Google Scholar]
- 24.Lewis ND. Is the social—ecological framework useful in understanding infectious diseases? The case of HIV/AIDS. Ecohealth. 2005;2(4):343–8. [Google Scholar]
- 25.Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol. 1992;47(1):6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 26.Kenny DA. Models of non-independence in dyadic research. J Soc Pers Relat. 1996;13(2):279–94. [Google Scholar]
- 27.Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. Understanding health behavior change among couples: an interdependence and communal coping approach. Soc Sci Med. 2006;62(6):1369–80. doi: 10.1016/j.socscimed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 28.El-Bassel N, Gilbert L, Golder S, et al. Deconstructing the relationship between intimate partner violence and sexual IPV risk among drug-involved men and their female partners. AIDS Behav. 2004;8(4):429–39. doi: 10.1007/s10461-004-7327-0. [DOI] [PubMed] [Google Scholar]
- 29.El-Bassel N, Gilbert L, Schilling RF, Ivanoff A, Borne D, Safyer SF. Correlates of crack abuse among drug-using incarcerated women: psychological trauma, social support, and coping. Am J Drug Alcohol Abuse. 1996;22:41–56. doi: 10.3109/00952999609001644. [DOI] [PubMed] [Google Scholar]
- 30.El-Bassel N, Ivanoff A, Schilling RF, Gilbert L, Borne D, Chen D. Preventing HIV/AIDS in drug-abusing incarcerated women through skills-building and social support enhancement: preliminary outcomes. Soc Work Res. 1995;19:131–41. [PubMed] [Google Scholar]
- 31.Royston P. Multiple imputation of missing values. Stata J. 2004;4(3):227–41. [Google Scholar]
- 32.Paik MC. The generalized estimating equation approach when data are not missing completely at random. J Am Stat Assoc. 1997;92:440. [Google Scholar]
- 33.Beunckens C, Sotto C, Molenberghs G. A simulation study comparing weighted estimating equations with multiple imputation based estimating equations for longitudinal binary data. Comput Stat Data Anal. 2008;52(3):1533–48. [Google Scholar]
- 34.Khan M, Doherty I, Schoenbach V, Taylor E, Epperson M, Adimora A. Incarceration and high-risk sexual partnerships among men in the United States. J Urban Health. 2009;86(4):584–601. doi: 10.1007/s11524-009-9348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Browning S, Miller S, Lisa M. Criminal incarceration dividing the ties that bind: black men and their families. J Afr Am Men. 2001;6(1):87–102. [Google Scholar]
- 36.Pew Center on the States. One in 31: the long reach of American corrections. Washington, DC: The Pew Charitable Trusts; 2009. [Google Scholar]
- 37.Seal DW. HIV-related issues and concerns for imprisoned persons throughout the world. Curr Opin Psychiatry. 2005;18(5):530–5. doi: 10.1097/01.yco.0000179492.08064.de. [DOI] [PubMed] [Google Scholar]
- 38.Greenfeld LA, Snell T. Women offenders: US Department of Justice, Office of Justice Programs. 2000 [Google Scholar]
- 39.Morris M, Kretzschmar M. Concurrent partnerships and the spread of HIV. AIDS. 1997;11(5):641–8. doi: 10.1097/00002030-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Rosenberg MD, Gurvey JE, Adler N, Dunlop MB, Ellen JM. Concurrent sex partners and risk for sexually transmitted diseases among adolescents. Sex Transm Dis. 1999;26(4):208–12. doi: 10.1097/00007435-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Arriola KR. Debunking the myth of the safe haven: toward a better understanding of intraprison HIV transmission. Criminol Public Policy. 2006;5(1):137–47. [Google Scholar]
- 42.Grinstead OA, Faigeles B, Comfort M, et al. HIV, STD, and hepatitis risk to primary female partners of men being released from prison. J Women Health. 2005;41(2):63–80. doi: 10.1300/J013v41n02_05. [DOI] [PubMed] [Google Scholar]
- 43.Hammett TM, Roberts C, Kennedy S. Health-related issues in prisoner reentry. Crime Delinq. 2001;47(3):390–411. [Google Scholar]
- 44.Bryan AD, Fisher JD, Fisher WA, Murray DM. Understanding condom use among heroin addicts in methadone maintenance using the information-motivation-behavioral skills model. Subst Use Misuse. 2000;35(4):451–71. doi: 10.3109/10826080009147468. [DOI] [PubMed] [Google Scholar]
- 45.Misovich S, Fisher J, Fisher W. Close relationships and elevated HIV risk behavior: evidence and possible underlying psychological processes. Rev Gen Psychol. 1997;1(1):72–107. [Google Scholar]