Abstract
Objectives
The Canadian C-Spine Rule for imaging of the cervical spine was developed for use by physicians. We believe that nurses in the emergency department could use this rule to clinically clear the cervical spine. We prospectively evaluated the accuracy, reliability and acceptability of the Canadian C-Spine Rule when used by nurses.
Methods
We conducted this three-year prospective cohort study in six Canadian emergency departments. The study involved adult trauma patients who were alert and whose condition was stable. We provided two hours of training to 191 triage nurses. The nurses then assessed patients using the Canadian C-Spine Rule, including determination of neck tenderness and range of motion, reapplied immobilization and completed a data form.
Results
Of the 3633 study patients, 42 (1.2%) had clinically important injuries of the cervical spine. The kappa value for interobserver assessments of 498 patients with the Canadian C-Spine Rule was 0.78. We calculated sensitivity of 100.0% (95% confidence interval [CI] 91.0%–100.0%) and specificity of 43.4% (95% CI 42.0%–45.0%) for the Canadian C-Spine Rule as interpreted by the investigators. The nurses classified patients with a sensitivity of 90.2% (95% CI 76.0%–95.0%) and a specificity of 43.9% (95% CI 42.0%–46.0%). Early in the study, nurses failed to identify four cases of injury, despite the presence of clear high-risk factors. None of these patients suffered sequelae, and after retraining there were no further missed cases. We estimated that for 40.7% of patients, the cervical spine could be cleared clinically by nurses. Nurses reported discomfort in applying the Canadian C-Spine Rule in only 4.8% of cases.
Conclusion
Use of the Canadian C-Spine Rule by nurses was accurate, reliable and clinically acceptable. Widespread implementation by nurses throughout Canada and elsewhere would diminish patient discomfort and improve patient flow in overcrowded emergency departments.
Each year, Canadian emergency departments treat 1.3 million patients who have suffered blunt trauma from falls or motor vehicle collisions and who are at risk for injury of the cervical spine.1 Most of these cases involve adults who are alert and in stable condition, and less than 1% involve fracture of the cervical spine.2 Most trauma patients who have been transported in ambulances are protected by a backboard, collar and neck supports. Nurses are responsible for initial triage in the emergency department and usually send such patients to high-acuity resuscitation rooms, where they may remain fully immobilized for hours until assessment by a physician and radiography are complete. This prolonged immobilization is often unnecessary and adds considerably to patient discomfort. The delay also adds to the burden of overcrowded Canadian emergency departments in an era when they are under unprecedented pressures.3–5 These patients occupy valuable space in resuscitation rooms, and repeated efforts to obtain satisfactory radiographs or computed tomography scans of the cervical spine use valuable time on the part of physicians, nurses and technicians.
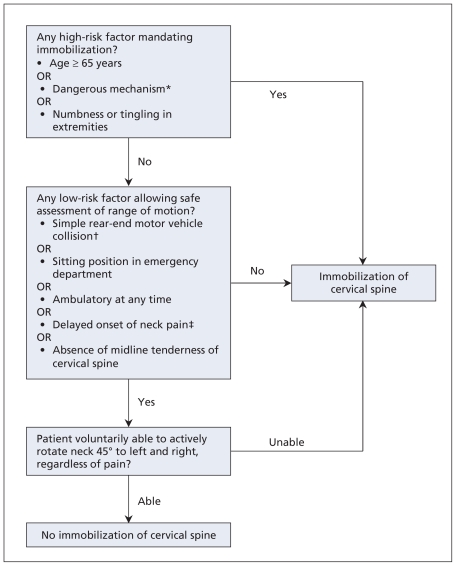
A clinical decision rule is defined as a decision-making tool incorporating three or more variables from the patient’s history, a physical examination or simple tests. Such rules are derived from original research and help clinicians with diagnostic or therapeutic decisions at the bedside. We previously developed a clinical decision rule for evaluation of the cervical spine.6,7 The Canadian C-Spine Rule comprises simple clinical variables (Figure 1) and was designed to allow clinicians to “clear” immobilization of the cervical spine (i.e., remove neck collar and other devices) without radiography and to decrease immobilization times.8 We also validated the accuracy of the rule when used by physicians.9 We recently completed an implementation trial at 12 Canadian hospitals to evaluate the impact on patient care and outcomes of the Canadian C-Spine Rule when used by physicians.10
Figure 1.
The Canadian C-Spine Rule to rule out cervical spine injury, adapted for use by nurses. The rule is intended for patients who have experienced trauma, who are alert (score on Glasgow Coma Scale = 15) and whose condition is stable. *The following mechanisms of injury were defined as dangerous: fall from elevation of more than 3 ft (91 cm) or five stairs, axial load to the head (e.g., diving injury), motor vehicle collision at high speed (> 100 km/h), motor vehicle collision involving a rollover or ejection, injury involving a motorized recreational vehicle, bicycle-related injury (rider struck or collision). †Simple rear-end motor vehicle collisions exclude incidents in which the patient was pushed into oncoming traffic or was hit by a bus, large truck or vehicle travelling at high speed, as well as rollovers; all such incidents would be considered high risk. ‡Neck pain with delayed onset is any pain that did not occur immediately following the precipitating incident. Adapted, with permission, from Stiell IG, Wells GA, Vandemheen K, et al. The Canadian Cervical Spine Radiography Rule for alert and stable trauma patients. JAMA 2001;286:1841–8.8 Copyright © 2001 American Medical Association. All rights reserved.
Nurses in the emergency department usually do not evaluate the cervical spine of trauma patients, and they routinely send all immobilized patients to the emergency department’s resuscitation room. We believe that nurses could safely evaluate alert patients who have arrived by ambulance and whose condition is stable and could “clear” immobilization of the cervical spine of low-risk patients upon arrival at the triage station.11 Patients could then be much more rapidly, comfortably and efficiently managed in other areas of the emergency department. An expanded decision-making role for nurses has the potential to improve the efficiency of trauma care in all Canadian hospitals. Very little research has been done to determine the ability of nurses to clear immobilization of the cervical spine.12–15 Our objective in this study was to prospectively evaluate the accuracy, reliability and acceptability of the Canadian C-Spine Rule when used by nurses to assess patients’ need for immobilization.
Methods
Study design and setting
We conducted this prospective cohort study in the emergency departments of two large teaching hospitals and four smaller community hospitals with a combined annual volume of about 210 000 visits to the emergency department. The teaching hospitals were located in Ottawa, Ontario (population 900 000), and each of the two emergency departments had an annual census of 60 000 patients and was staffed by full-time certified emergency physicians and emergency medicine residents. The community hospitals were located in small towns (population 6000 to 8000) near Ottawa, and each of the emergency departments had an annual census of 15 000 to 25 000 patients and was staffed by full-time and part-time emergency physicians.
Patient population
We enrolled consecutive alert adults who were in stable condition and who presented with potential cervical spine injury after acute blunt trauma, including patients with posterior neck pain and those presenting by ambulance with immobilization of the cervical spine. The patients had to be alert and cooperative, with a Glasgow Coma Scale16 score of 15; their condition had to be stable, with normal vital signs as defined by the Revised Trauma Score;17 and the injury had to have occurred within the previous 48 hours. We excluded patients under the age of 16 years; those with penetrating trauma, acute paralysis or known vertebral disease (i.e., ankylosing spondylitis, rheumatoid arthritis, spinal stenosis or previous cervical spine surgery); and those who were returning for reassessment of a previously treated injury or who had been referred from another hospital. The research ethics board of each hospital approved the study without the need for informed patient consent at the time of the visit to the emergency department.
Study nurses and training
Typically 30%–50% of the more experienced nurses in the study emergency departments undergo additional training to perform the triage role. For these nurses, we developed unique training tools for the Canadian C-Spine Rule, including a computer-based one-hour auto-tutorial CD and a one-hour practical session. The self-teaching CD included Power-Point slides on evidence for and application of the rule, video demonstrations of techniques, questions and answers, and case studies. During each practical session, a nurse educator met with small groups of nurses to review the rule, demonstrate techniques, answer questions and provide three patient scenarios for hands-on training to each nurse. The nurse educator used a performance checklist to evaluate each nurse during the patient scenarios and to ensure the nurse’s competence in applying the rule. In addition, each nurse had to complete and pass a written test to be certified in cervical spine assessment. We conducted a “train-the-trainer” teaching day to prepare local champion-trainers for each site. Several pages from the training CD, as well as the checklist, test and certificate, are presented in Appendix 1, available at www.cmaj.ca/cgi/content/full/cmaj.091430/DC1.
The triage nurses assessed all eligible trauma patients who were alert and in stable condition and who arrived by ambulance, recording their findings on a data form. Although the nurses temporarily loosened patients’ cervical collars to assess tenderness and range of motion, if applicable, they did not remove immobilization or otherwise attempt to clear immobilization of the cervical spine in this validation study. Where possible, on a convenience basis, a nurse or physician colleague was asked to independently assess the same patient to allow determination of interobserver agreement. These secondary assessments were performed on a voluntary and non-systematic basis. We also conducted brief retraining sessions over the course of the study and circulated regular newsletters to participating nurses.
Outcome measures and data collection
We screened all potentially eligible patients and kept a log of those for whom a data form was not completed (i.e., patients not enrolled). We obtained data for patients’ characteristics and outcomes, including imaging of the cervical spine, admission, surgery and adverse outcomes, from the emergency department chart and electronic hospital records. The primary outcome was clinically important cervical spine injury, defined as any fracture, dislocation or ligamentous instability requiring internal fixation or treatment with a halo, brace or rigid collar.18 All injuries were considered clinically important unless imaging demonstrated the following clinically unimportant injuries: isolated avulsion fracture of osteophyte, isolated fracture of transverse process not involving a facet joint, isolated fracture of spinous process not involving lamina or simple compression fracture involving less than 25% of vertebral body height. Radiographs were interpreted by independent staff radiologists who were given routine clinical information on the requisition but were blinded to the contents of the data collection sheet. A surveillance strategy was implemented to identify missed fractures or serious adverse outcomes. We monitored each emergency department’s patient visit logs for 30 days to identify return visits by patients who did not undergo imaging during their initial visit. This monitoring encompassed the regional neurosurgical centre, which was one of the study hospitals and which was the spine injury referral hospital for all of the other study hospitals.
Statistical analysis
We examined demographic and clinical characteristics using simple descriptive statistics. We assessed interobserver agreement with the kappa statistic. We determined nurses’ accuracy in overall interpretation of the rule (immobilization required v. no immobilization required) by comparing the nurse’s response on the data collection form for each patient with the “gold standard” interpretation of the rule made by the investigators, based on a review of all clinical notes. The accuracy of the rule was evaluated with measures of sensitivity, specificity and potential impact on clinical clearance rates with 95% confidence intervals (CIs). Finally, we compiled the responses to a five-point Likert scale question about nurses’ comfort with use of the rule, in a simple descriptive format.
Results
From April 2005 to Jan. 31, 2008, a total of 4739 eligible patients presented to the six participating emergency departments, and a total of 191 participating triage nurses enrolled and assessed 3633 (76.7%) of these patients. The participating nurses had the following characteristics: 152 women (79.6%), 56 (29.3%) with a baccalaureate degree, mean of 19 years in nursing, mean of 11 years in the emergency department and mean of 28 hours worked per week.
The 3633 patients who were evaluated ranged in age from 16 to 100 years, 2696 (74.2%) arrived by ambulance, and 42 (1.2%) had clinically important injuries of the cervical spine (Table 1). Enrolment ranged from 222 at one of the community hospitals to 1237 at one of the teaching hospitals, and individual nurses assessed between 1 and 166 patients. Although the two teaching hospitals had more patients than the community hospitals, they also had four to five times more nurses participating in the study. The prevalence of cervical spine injury was 1.1% and 1.5% at the two teaching hospitals and ranged from 0.4% to 1.5% at the four community hospitals. The 1106 eligible patients who were not enrolled presented at times when the study nurses were not available. These non-enrolled patients had similar characteristics to those who were enrolled: mean age 41 years, 774 (70.0%) arrived by ambulance, and 8 (0.7%) had clinically important injuries.
Table 1.
Characteristics of 3633 patients with trauma who were assessed for potential injury to the cervical spine
| Characteristic | No. (%) of patients* |
|---|---|
| Age, yr | |
| Mean (SD) | 41 (18) |
| Range | 16–100 |
| Sex, female | 1946 (53.6) |
| Hospital | |
| Ottawa Hospital — Civic Campus | 1281 (35.3) |
| Ottawa Hospital — General Campus | 1237 (34.0) |
| Perth Memorial Hospital | 346 (9.5) |
| Smith Falls Memorial Hospital | 246 (6.8) |
| Winchester District Memorial Hospital | 222 (6.1) |
| Hawkesbury District and General Hospital | 301 (8.3) |
| Mechanism of injury | |
| Motor vehicle collision | 2288 (63.0) |
| Pedestrian struck | 98 (2.7) |
| Bicycle collision | 133 (3.7) |
| Fall | 679 (18.7) |
| Assault | 58 (1.6) |
| Axial load (e.g., diving, fall, sports) | 60 (1.7) |
| Hit head on an object | 170 (4.7) |
| Other | 60 (1.7) |
| Time from injury to arrival, h, median (IQR) | 1.2 (0.9–1.6) |
| Arrived by ambulance | 2696 (74.2) |
| Radiography of cervical spine performed | 1714 (47.2) |
| Type of injury of cervical spine | |
| Clinically important† | 42 (1.2) |
| Fracture | 41 (97.6) |
| Dislocation | 1 (2.4) |
| Ligamentous instability | 1 (2.4) |
| Clinically unimportant | 6 (0.2) |
| Neurologic deficit developed | 10 (0.3) |
| Stabilizing treatments | 38 (1.0) |
| Internal fixation | 8 (0.2) |
| Halo | 6 (0.2) |
| Brace | 5 (0.1) |
| Rigid collar | 19 (0.5) |
| Time from arrival to disposition, h, median (IQR) | 4.5 (2.7–7.1) |
| Admission to hospital | 292 (8.0) |
Note: IQR = interquartile range, SD = standard deviation.
Unless otherwise indicated.
Percentages for individual types of clinically important injury to the cervical spine are based on the number of patients with such an injury (n = 42).
The most common positive finding among the criteria of the Canadian C-Spine Rule was adequate ability to rotate the neck (1531 patients [42.1%]) (Table 2). Overall, only 1909 (52.5%) of the patients were deemed to require ongoing immobilization.
Table 2.
Findings relevant to the Canadian C-Spine Rule for the 3633 study patients
| Finding | No. (%) of patients |
|---|---|
| From history | |
| Dangerous mechanism | 1125 (31.0) |
| Paresthesias in extremities | 327 (9.0) |
| Simple rear-end motor vehicle collision | 542 (14.9) |
| Ambulatory at any time | 1320 (36.3) |
| Immediate onset of neck pain | 1486 (40.9) |
| From physical examination | |
| Sitting position in emergency department | 558 (15.4) |
| Midline tenderness of the cervical spine | 1294 (35.6) |
| Able to rotate neck | 1531 (42.1) |
| Immobilization required | 1909 (52.5) |
We assessed interobserver agreement for a convenience sample of 498 patients who were examined by a triage nurse and then by a physician (334 [67.1%] of cases) or a second triage nurse (164 [32.9%]). Interobserver assessments for overall interpretation of the Canadian C-Spine Rule for need for immobilization showed simple agreement of 90.5% and kappa of 0.78 (95% CI 0.72–0.84) (Table 3). In addition, agreement for the nine individual components of the rule was also very good, the kappa values ranging from 0.56 to 0.96.
Table 3.
Interobserver agreement for the clinical criteria in the Canadian C-Spine Rule (n = 498)
| Criterion | Kappa value (95% CI) |
|---|---|
| Any high-risk factor | 0.80 (0.75–0.86) |
| Age ≥ 65 yr | 0.96 (0.92–1.00) |
| Dangerous mechanism | 0.80 (0.74–0.86) |
| Paresthesias | 0.70 (0.59–0.81) |
| Any low-risk factor | 0.64 (0.44–0.85) |
| Rear-end motor vehicle collision | 0.74 (0.65–0.84) |
| Upright position | 0.75 (0.66–0.85) |
| Ambulatory | 0.65 (0.54–0.75) |
| Delayed onset of neck pain | 0.60 (0.49–0.71) |
| Midline tenderness | 0.56 (0.45–0.66) |
| Able to rotate neck | 0.72 (0.53–0.92) |
| Decision to immobilize | |
| Overall | 0.78 (0.72–0.84) |
| Nurse–nurse comparisons | 0.80 (0.71–0.90) |
| Nurse–physician comparisons | 0.75 (0.67–0.84) |
Note: CI = confidence interval.
With regard to accuracy of assessment, nurses did not evaluate range of motion, as required by the algorithm, for 181 (5.0%) of the patients, and the investigators later classified these cases as “indeterminate” for the rule. Excluding these indeterminate cases, we calculated sensitivity of 100% (95% CI 91.0%–100.0%) and specificity of 43.4% (95% CI 42.0%–45.0%) for the Canadian C-Spine Rule as interpreted by the investigators (Table 4). The nurses’ classification of patients according to the Canadian C-Spine Rule had a sensitivity of 90.2% (95% CI 76.0%–95.0%) and a specificity of 43.9% (95% CI 42.0%–46.0%) (Table 5). The overall accuracy of the nurses’ interpretation relative to that of the investigators was 92.5%. In the first few months of the study, nurses at the teaching hospitals failed to identify four of the clinically important injury cases (Box 1), despite the presence of factors identified in the Canadian C-Spine Rule as representing high risk (age 65 years, presence of paresthesias or dangerous mechanism). None of these patients experienced an adverse outcome, and we intensified our continuing education efforts with lunch-and-learn sessions and regular newsletters. Of all 3633 patients in the study, including the indeterminate cases, the result of the Canadian C-Spine Rule was negative for 1480 (40.7%), meaning that immobilization of the cervical spine could have been cleared for these patients if the rule was being applied and was interpreted accurately. The proportion of patients classified as not requiring immobilization varied, by hospital, from 54 (17.9%) of 301 to 110 (44.7%) of 246, with community hospitals having both the lowest and the highest rates.
Table 4.
Performance of the Canadian C-Spine Rule for 42 “clinically important” injury cases among 3633 patients, as judged by the Investigators
| Result with rule | Cervical spine injury | No cervical spine injury |
|---|---|---|
| Positive | 41 | 1931 |
| Negative | 0 | 1480 |
| Indeterminate* | 1 | 180 |
| Sensitivity, % (95% CI) | 100.0 (91.0–100.0) | |
| Specificity, % (95% CI) | 43.4 (42.0–45.0) | |
| Negative predictive value, % | 100 | |
Note: CI = confidence interval.
Data for rule were incomplete.
Table 5.
Performance of nurses’ interpretation of the Canadian C-Spine Rule for 42 “clinically important” injury cases among 3633 patients
| Nurses’ result with rule | Cervical spine injury | No cervical spine injury |
|---|---|---|
| Positive | 37 | 1958 |
| Negative | 4 | 1535 |
| Indeterminate* | 1 | 98 |
| Sensitivity, % (95% CI) | 90.2 (76.0–95.0) | |
| Specificity, % (95% CI) | 43.9 (42.0–46.0) | |
| Negative predictive value, % | 99.7 | |
Note: CI = confidence interval.
Data for rule were incomplete.
Box 1. Clinically important cases of injury to the cervical spine not identified by nurses
Case 1
Ambulatory 25-year-old patient who had been in a motor vehicle collision
High-risk criterion overlooked by nurse: paresthesia
Fracture of superior facet of seventh cervical vertebra involving lateral mass
Rigid collar was applied, and patient was released
Case 2
Ambulatory 65-year-old patient who fell down stairs onto head and who walked into the emergency department
High-risk criteria overlooked by nurse: age 65 years, dangerous mechanism
Teardrop fracture of seventh cervical vertebra with minimal wedging
Hard collar was applied, and patient was admitted overnight
Case 3
Ambulatory 33-year-old patient who fell down stairs onto head
High-risk criterion overlooked by nurse: dangerous mechanism
Traumatic subluxation of third and fourth cervical vertebrae
Internal fixation was applied
Case 4
Ambulatory 17-year-old patient who was ejected from car in a motor vehicle collision
High-risk criterion overlooked by nurse: dangerous mechanism
Traumatic subluxation of fifth and sixth cervical vertebrae
Patient was admitted two days later, and a halo was applied
Using a five-point Likert scale, nurses reported their level of comfort in applying the Canadian C-Spine Rule for 3199 of the cases: the nurses were very comfortable in applying the rule in 1681 cases (52.5%), comfortable in 1196 cases (37.4%), neutral in 168 cases (5.3%), uncomfortable in 122 cases (3.8%) and very uncomfortable in 32 cases (1.0%). The responses were similar among all six hospitals.
Discussion
This large-scale, multicentre study has demonstrated the reliability, accuracy, acceptability and potential impact of having triage nurses in the emergency department apply the Canadian C-Spine Rule to clinically clear the cervical spine for alert trauma patients in stable condition. The interobserver agreement between nurses and other nurses or physicians in terms of evaluating the overall rule, as well as the components of the rule, was excellent. Although nurses failed to identify four cases of injury early in the study, enhanced training and reminders led to very good accuracy of rule interpretation for the rest of the study. Our findings suggest that about 40% of trauma patients whose condition is stable could have immobilization of the cervical spine removed by triage nurses. Finally, the nurses indicated a generally high degree of comfort in applying the Canadian C-Spine Rule for individual patients. The large numbers of patients and nurses in this study, as well as the mixture of large and small hospital sites, contribute to the generalizability of these findings. Implementation programs that are now under way should lead to widespread clearance of cervical spine immobilization by emergency department nurses.
Because of the potential for spinal injury, North American emergency care workers go to great lengths to protect the cervical spine of trauma patients. Consequently, regardless of whether neck symptoms are present, most trauma patients transported to hospital in an ambulance are protected by such measures as a backboard, collar and sandbags.19,20 Such patients commonly occupy scarce resuscitation bays in the emergency department, with full immobilization, for several hours until radiography or computed tomography of the cervical spine can be performed and the images interpreted. In many cases, prolonged immobilization is unnecessary and adds considerably to patient discomfort. In addition, the delay compounds the burden on crowded Canadian emergency departments in an era when they are under unprecedented pressures.3,5,21 These patients occupy space in the resuscitation room, which is often viewed as the most valuable space within the emergency department. As well, repeated attempts are often needed to obtain satisfactory radiographs of the cervical spine, which consumes valuable time on the part of physicians, nurses and radiology technicians and distracts them from other urgent responsibilities.4,22 At the time of writing, we were aware of no US or Canadian hospital where triage nurses in the emergency department had the authority to clinically clear the cervical spine.
Although the concept of having nurses clear the cervical spine was first proposed in 1992,11 there has been little research in this area. More commonly, investigators have studied evaluation by nurses of ankle and knee injuries.23–26 Recent review articles have strongly supported the concept of nurses in the emergency department clinically clearing the cervical spine,27–29 but we have been able to identify only four original research papers assessing the potential for nurses to evaluate the cervical spine. Hsieh and colleagues12 described a small US cohort study that evaluated a nonvalidated clearance protocol, similar to the criteria of the National Emergency X-Radiography Utilization Study (also knowns as NEXUS). The authors evaluated interobserver agreement for 211 patients and concluded that there was good agreement between nurses and physicians for these assessments. Miller and associates,13 in a study performed in the United Kingdom, evaluated 112 emergency nurses and their interpretation of the Canadian C-Spine Rule in 460 patients. That study also demonstrated good interobserver agreement between nurses and physicians and found that the majority of nurses were comfortable in using the rule.13 Kelly and coworkers,14 in Australia, also reported good interobserver agreement between nurses and physicians in interpreting the Canadian C-Spine Rule in 88 patients. In another UK study, Pitt and colleagues15 had emergency nurses attempt to clear the cervical spine of trauma patients using the NEXUS criteria. In that small study of 112 patients, the nurses actually cleared the cervical spine in 59 cases. To our knowledge, there have been no reports from North America of nurses attempting to clear the cervical spine.
We expect that use of the Canadian C-Spine Rule by nurses will ultimately lead to improved efficiency for Canadian emergency hospitals and increased comfort for individual patients. Injury is an extremely common presentation for all Canadian emergency departments. This validation study represents an important step in extending the responsibility of effective triage of trauma patients to nurses across Canada and elsewhere. Canadian nurses currently do not evaluate patients for potential injury of the cervical spine, a task performed exclusively by physicians. We believe that use of the Canadian C-Spine Rule has the potential to improve the efficiency of patient flow in busy Canadian emergency departments and to increase the autonomy of the nursing profession in managing low-risk trauma patients. We expect the results of this study to be applicable to triage nurses in emergency departments throughout Canada. We are currently conducting an implementation study in which triage nurses are clearing the cervical spine and removing neck collars and other immobilization devices. We expect that this approach will eventually be adopted as standard nursing practice in all Canadian emergency departments.
Limitations
The study had several potential limitations. First, it was a validation study, in which we evaluated the accuracy of nurses’ interpretation of the Canadian C-Spine Rule but did not have the nurses actually remove immobilization devices. Second, the interobserver cohort was assembled on a purely convenience basis, which might have introduced some selection bias or inflated the kappa values. Nevertheless, the sample of 498 cases is far larger than we achieved in previous derivation and validation studies with physicians.8,9 Third, the nurses failed to identify four cases of important injury early in the study, which meant that the overall sensitivity among nurses was 90.2%. However, in the comparable physician validation study, physicians missed and sent home 9 of 169 patients with clinically important injury without any patient harm.9 We believe that interpretation of this rule by nurses is both reliable and safe but that appropriate emphasis on high-risk factors is important in teaching and refresher sessions. It is also important to remember that these patients are at very low risk, are usually capable of ambulation and will be assessed by a physician before discharge. Finally, we were obliged to classify the result of the rule as indeterminate for 5.0% of the patients, because rotation of the neck was not assessed, even though these patients were found to be at low risk. We view this as a conservative approach by nurses in specific cases where they were uncomfortable assessing rotation. Notably, physicians did not evaluate range of motion in 2.6% of cases in the physician validation study.9
Conclusions
We found that use of the Canadian C-Spine Rule by emergency nurses was accurate, reliable and clinically acceptable. Widespread implementation by triage nurses would prevent prolonged and uncomfortable immobilization for many trauma patients in emergency departments throughout Canada and elsewhere. This would diminish patient discomfort and improve patient flow in overcrowded emergency departments.
Supplementary Material
Acknowledgements
The authors are grateful for the support of the following nursing directors and their organizations: Lucille Auffrey RN MN, Canadian Nurses Association; Doris Grinspun RN MSN, Registered Nurses’ Association of Ontario; Emergency Nurses Association of Ontario; National Emergency Nurses Affiliation; and Nursing Secretariat, Ontario Ministry of Health and Long-Term Care.
The authors thank the following individuals for their much-appreciated efforts on the study: for training and data collection, Michael Hendley, Mary Ann Scollan, Nancy Rattle, Martha Moore, Judy Tessier and Krista O’Donohue; for medical supervision, Dr. Chuck Su, Dr. Michael Horsey and Dr. Alan Drummond; for data management, MyLinh Tran, and Sheryl Domingo; and for manuscript preparation, Angela Marcantonio. Finally, the authors thank the 191 emergency nurses whose voluntary participation in the study made it a success.
Data from this study were presented at the annual meetings of the Society for Academic Emergency Medicine, Washington, DC, in May 2008, and the Canadian Association of Emergency Physicians, Ottawa, Ont., in June 2008.
Footnotes
Funding: This study was funded by a peer-reviewed grant from the Canadian Health Services Research Foundation and the Canadian Institutes of Health Research (FRN-73075).
Previously published at www.cmaj.ca
Competing interests: George A. Wells is a biostatistical consultant for CMAJ and was not involved in the editorial decision-making process for this article. None declared for all other authors.
Contributors: Ian G. Stiell, Catherine M. Clement, Annette O’Connor, Barbara Davies and George A. Wells developed and contributed substantially to study concept and design. Ian G. Stiell, Catherine M. Clement, Christine Leclair, Pamela Sheehan, Tamara Clavet, Christine Beland and Taryn MacKenzie acquired the data. Ian G. Stiell, Catherine M. Clement, Annette O’Connor, Barbara Davies and George A. Wells collated the data and assisted with data analysis. All authors drafted the manuscript and/or contributed to its revision. All authors gave final approval of the version to be published.
This article has been peer reviewed.
REFERENCES
- 1.Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Rep. 2008;(7):1–38. [PubMed] [Google Scholar]
- 2.Stiell IG, Wells GA, Vandemheen K, et al. Variation in emergency department use of cervical spine radiography for alert, stable trauma patients. CMAJ. 1997;156:1537–44. [PMC free article] [PubMed] [Google Scholar]
- 3.Chan BT, Schull MJ, Schultz SE. Emergency department services in Ontario 1993–2000. Toronto (ON): Institute for Clinical Evaluative Sciences; 2001. [Google Scholar]
- 4.Schull MJ, Slaughter PM, Redelmeier DA. Urban emergency department overcrowding: defining the problem and eliminating misconceptions. CJEM. 2002;4:76–83. doi: 10.1017/s1481803500006163. [DOI] [PubMed] [Google Scholar]
- 5.Lindsay P, Bronskill S, Schull MJ, et al. Clinical utilization and outcomes. In: Brown AD, editor. Hospital report 2001: emergency department care. Toronto (ON): Ontario Hospital Association and Government of Ontario; 2001. [Google Scholar]
- 6.Stiell IG, Wells GA, McKnight RD, et al. The Canadian C-Spine Rule Study for alert and stable trauma patients: background and rationale. CJEM. 2002;4:84–90. [PubMed] [Google Scholar]
- 7.Stiell IG, Wells GA, McKnight RD, et al. Canadian C-Spine Rule study for alert and stable trauma patients: II. Study objectives and methodology. CJEM. 2002;4:185–93. [PubMed] [Google Scholar]
- 8.Stiell IG, Wells GA, Vandemheen K, et al. The Canadian Cervical Spine Radiography Rule for alert and stable trauma patients. JAMA. 2001;286:1841–8. doi: 10.1001/jama.286.15.1841. [DOI] [PubMed] [Google Scholar]
- 9.Stiell IG, Clement C, McKnight RD, et al. Comparative validation of the Canadian C-Spine Rule and the NEXUS low-risk criteria in alert and stable trauma patients. N Engl J Med. 2003;349:2510–8. doi: 10.1056/NEJMoa031375. [DOI] [PubMed] [Google Scholar]
- 10.Stiell IG, Clement CM, Grimshaw J, et al. Implementation of the Canadian CSpine Rule: prospective 12 centre cluster randomised trial. BMJ. 2009;339:b4146. doi: 10.1136/bmj.b4146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Selivanov V, Martinez R. Clinical clearance of the cervical spine. J Emerg Nurs. 1992;18:79–80. [PubMed] [Google Scholar]
- 12.Hsieh M, Gutman M, Haliscak D. Clinical clearance of cervical spine injuries by emergency nurses. Acad Emerg Med. 2000;7:342–7. doi: 10.1111/j.1553-2712.2000.tb02234.x. [DOI] [PubMed] [Google Scholar]
- 13.Miller P, Coffey F, Reid AM, et al. Can emergency nurses use the Canadian cervical spine rule to reduce unnecessary patient immobilisation? Accid Emerg Nurs. 2006;14:133–40. doi: 10.1016/j.aaen.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Kelly AM, Bradshaw L, Kerr D. Can nurses apply the Canadian c-spine rule? A pilot study. CJEM. 2004;6:161–4. doi: 10.1017/s1481803500006850. [DOI] [PubMed] [Google Scholar]
- 15.Pitt E, Pedley DK, Nelson A, et al. Removal of C-spine protection by A&E triage nurses: a prospective trial of a clinical decision making instrument. Emerg Med J. 2006;23:214–5. doi: 10.1136/emj.2005.023697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2:81–4. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 17.Advanced trauma life support instructor manual. Chicago (IL): American College of Surgeons; 1997. [Google Scholar]
- 18.Stiell IG, Lesiuk H, Vandemheen K, et al. Obtaining consensus for a definition of “clinically important cervical spine injury” in the CCC Study. Acad Emerg Med. 1999;6:435. [Google Scholar]
- 19.Bachulis BL, Long WB, Hynes GD, et al. Clinical indications for cervical spine radiographs in the traumatized patient. Am J Surg. 1987;153:473–7. doi: 10.1016/0002-9610(87)90796-3. [DOI] [PubMed] [Google Scholar]
- 20.McNamara RM, Heine E, Esposito B. Cervical spine injury and radiography in alert, high-risk patients. J Emerg Med. 1990;8:177–82. doi: 10.1016/0736-4679(90)90229-o. [DOI] [PubMed] [Google Scholar]
- 21.Schull MJ, Szalai JP, Schwartz B, et al. Emergency department overcrowding following systematic hospital restructuring: trends at twenty hospitals over ten years. Acad Emerg Med. 2001;8:1037–43. doi: 10.1111/j.1553-2712.2001.tb01112.x. [DOI] [PubMed] [Google Scholar]
- 22.Vandemark RM. Radiology of the cervical spine in trauma patients: practice pitfalls and recommendations for improving efficiency and communication. AJR Am J Roentgenol. 1990;155:465–72. doi: 10.2214/ajr.155.3.2117342. [DOI] [PubMed] [Google Scholar]
- 23.Szucs PA, Richman PB, Mandell M. Triage nurse application of the Ottawa knee rule. Acad Emerg Med. 2001;8:112–6. doi: 10.1111/j.1553-2712.2001.tb01274.x. [DOI] [PubMed] [Google Scholar]
- 24.Kec RM, Richman PB, Szucs PA, et al. Can emergency department triage nurses appropriately utilize the Ottawa Knee Rules to order radiographs? — An implementation trial. Acad Emerg Med. 2003;10:146–50. doi: 10.1197/aemj.10.2.146. [DOI] [PubMed] [Google Scholar]
- 25.Fiesseler F, Szucs P, Kec R, et al. Can nurses appropriately interpret the Ottawa Ankle Rule? Am J Emerg Med. 2004;22:145–8. doi: 10.1016/j.ajem.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 26.Derksen R-J, Bakker FC, Geervliet PC, et al. Diagnostic accuracy and reproducibility in the interpretation of Ottawa ankle and foot rules by specialized emergency nurses. Am J Emerg Med. 2005;23:725–9. doi: 10.1016/j.ajem.2005.02.054. [DOI] [PubMed] [Google Scholar]
- 27.Charters A. Can nurses, working in the emergency department, independently clear cervical spine? A review of the literature. Accid Emerg Nurs. 2004;12:19–23. doi: 10.1016/j.aaen.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 28.Danis DM. Trauma today and tomorrow: recent clinical literature. J Emerg Nurs. 2005;31:447–55. doi: 10.1016/j.jen.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Zimmerman PG. Cutting-edge discussions on management, policy, and program issues in emergency care. J Emerg Nurs. 2006;32:525–9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.