A 70-year-old man was admitted to hospital because of multiple injuries from a traffic collision. On day 16 after admission, he started to complain of pain, weakness and numbness in his right leg.
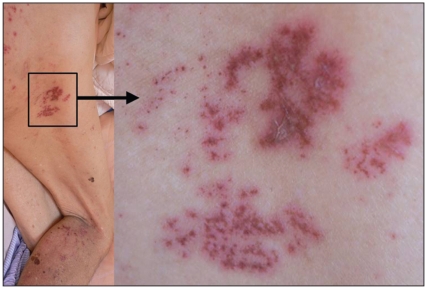
A contrast-enhanced computed tomographic scan of the lumbar spine showed a displaced sacral fracture with compression of the S1 ventral ramus (Appendix 1, available at www.cmaj.ca/cgi/content/full/cmaj.091534/DC1). The patient’s symptoms persisted despite treatment with diclofenac, chlor-zoxazone, fursultiamine and betamethasone. Severe tingling pain and allodynia (pain with light touch) developed seven days later. Thirty days after admission, several painful grouped erythematous plaques with vesicles were found on his right buttock and the posterior aspect of his right leg (Figure 1). The distribution was consistent with the S1 dermatome, and a diagnosis of herpes zoster was made. The patient was prescribed valacyclovir hydrochloride, 500 mg three times daily for five days. The cutaneous lesions healed about seven days after the treatment was started and the tingling pain resolved gradually. We discharged the patient 42 days after admission.
Figure 1.
Painful grouped erythematous plaques with vesicles, found along the S1 dermatome in a 70-year-old man, seven days after the start of sciatic symptoms.
Older age, altered cell-mediated immunity and diseases such as malignancy, chronic lung disease, renal failure and liver disease are common risk factors for herpes zoster.1 Thomas and colleagues2 reported a case–control study based in general practice in London, UK, of the determinants of zoster in adults without underlying immunosuppression. They concluded that recent trauma is associated with an adjusted 12-fold increased risk of herpes zoster at the site of injury, but not at other body sites. The increase in absolute risk was 3.9%. In our patient, the major cause of reactivation of herpes zoster would seem to be the recent trauma. Direct stimulation of the nerve may have triggered reactivation of the virus in the dorsal root ganglion. The pain associated with herpes zoster mimicked post-traumatic sciatic pain, which made the diagnosis difficult. Although sacral segments rarely show involvement of herpes zoster,3 clincians should consider this possibility when patients are suffering from intractable pain after recent trauma.
Supplementary Material
Footnotes
Previously published at www.cmaj.ca
Competing interests: None declared.
This article has been peer reviewed.
REFERENCES
- 1.McDonald JR, Zeringue AL, Caplan L, et al. Herpes zoster risk factors in a national cohort of veterans with rheumatoid arthritis. Clin Infect Dis. 2009;48:1364–71. doi: 10.1086/598331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomas SL, Wheeler JG, Hall AJ. Case–control study of the effect of mechanical trauma on the risk of herpes zoster. BMJ. 2004;328:439–40. doi: 10.1136/bmj.37991.511829.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scheld WM, Whitley RJ, Marra CM. Infections of the central nervous system. 3. Philadelphia (PA): Lippincott, Williams & Wilkins; 2004. p. 149. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.