Abstract
Objective
Disease activity in systemic lupus erythematosus (SLE) is typically monitored by measuring serum C3 and C4. However, these proteins have limited utility as lupus biomarkers, because they are substrates rather than products of complement activation. The aim of this study was to evaluate the utility of measuring the erythrocyte-bound complement activation products, erythrocyte-bound C3d (E-C3d) and E-C4d, compared with that of serum C3 and C4 for monitoring disease activity in patients with SLE.
Methods
The levels of E-C3d and E-C4d were measured by flow cytometry in 157 patients with SLE, 290 patients with other diseases, and 256 healthy individuals. The patients with SLE were followed up longitudinally. Disease activity was measured at each visit, using the validated Systemic Lupus Activity Measure (SLAM) and the Safety of Estrogens in Lupus Erythematosus: National Assessment (SELENA) version of the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI).
Results
At baseline, patients with SLE had higher median levels of E-C3d and E-C4d (P < 0.0001) in addition to higher within-patient and between-patient variability in both E-C3d and E-C4d when compared with the 2 non-SLE groups. In a longitudinal analysis of patients with SLE, E-C3d, E-C4d, serum C3, and anti–double-stranded DNA (anti-dsDNA) antibodies were each significantly associated with the SLAM and SELENA–SLEDAI. In a multivariable analysis, E-C4d remained significantly associated with these SLE activity measures after adjusting for serum C3, C4, and anti-dsDNA antibodies; however, E-C3d was associated with the SLAM but not with the SELENA–SLEDAI.
Conclusion
Determining the levels of the erythrocyte-bound complement activation products, especially E-C4d, is an informative measure of SLE disease activity as compared with assessing serum C4 levels and should be considered for monitoring disease activity in patients with SLE.
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease with polymorphic clinical manifestations that range from mild symptoms to life-threatening multiorgan dysfunction. The combination of heterogeneous clinical presentations at the time of diagnosis and unpredictable disease courses represents an immense medical and scientific challenge to biomarker development. Despite our advancing knowledge of the pathogenesis of SLE, few lupus biomarkers have been validated and widely accepted, and those in routine clinical use have been in place for decades (1,2). The dearth of lupus biomarkers is a major contributing factor to challenges in the clinical care of patients with lupus, in the accurate and thorough interpretation of clinical lupus research, in randomized controlled clinical trials, and in the development of new therapeutic agents for lupus. The US Food and Drug Administration has not approved a new drug for lupus in >50 years.
In lieu of more useful lupus biomarkers, numerous indices have been developed in an attempt to measure disease activity in patients with lupus; the most widely used indices are the Systemic Lupus Activity Measure (SLAM) (3), the Safety of Estrogens in Lupus Erythematosus: National Assessment (SELENA) version of the Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) (4), and the British Isles Lupus Assessment Group index (5). All of these indices have been validated and have excellent reliability, validity, and responsiveness to change. However, these indices are used almost exclusively by lupus research specialists; intense training is required to accurately complete these indices, and they may be too complex, cumbersome, and time-consuming to be used in routine clinical practice.
Numerous studies have documented abnormalities in complement activation and clearance of immune complexes by erythrocytes as central pathogenic mechanisms in SLE (6,7). Measurement of serum C3 and serum C4 has traditionally been the gold standard for monitoring disease activity in patients with SLE; however, several major weaknesses in this approach have been previously identified. First, there is a wide range of variation of serum C3 and serum C4 levels among healthy individuals, and this range overlaps with the range observed in patients with SLE. Second, these are measurements of precursors rather than products of complement activation. Systemic inflammation resulting in an acute-phase response can increase synthesis of C3 and C4 that balances the increased catabolism of these proteins. Third, hereditary deficiencies and partial deficiencies of C4-null alleles may result in persistently lower-than-normal serum C4 levels because of decreased synthesis rather than because of increased complement activation and/or active SLE. Although the value of using serum C3 and serum C4 levels as biomarkers for SLE remains controversial, these markers are widely used in clinical practice (8–17).
The recognition that complement and SLE are intimately associated, together with the questionable value of using serum C3 and serum C4 levels as biomarkers of lupus disease activity (8–17), led us to consider alternative measures of complement activation for monitoring patients with SLE (18–20).
Proteolytic fragments of complement component C4, particularly C4d, are present on the surface of normal erythrocytes (21,22). Our group previously demonstrated that patients with SLE had significantly higher levels of erythrocyte-bound C4d (E-C4d) and lower levels of erythrocyte-expressing complement receptor 1 than did patients with other diseases and healthy control subjects (19). In addition, we observed that lupus disease activity correlated with reticulocyte C4d in a cross-sectional analysis and correlated serial measurements of E-C4d and reticulocyte C4d with disease activity in individual patients with SLE (20).
In this longitudinal study, we assessed the utility of assays with E-C3d and E-C4d, as compared with the serum C3 and C4 assays in routine clinical use, as measures of lupus disease activity.
PATIENTS AND METHODS
Study participants
All study participants were 18 years of age or older, and all provided written informed consent. No one was excluded based on sex or ethnicity. The University of Pittsburgh Institutional Review Board approved this study.
SLE patients
Consecutive patients with SLE were recruited and followed up during routine visits to the University of Pittsburgh Lupus Patient Care and Translational Research Center, from August 2000 to January 2005. Only patients who met the 1982 (23) or 1997 (24) American College of Rheumatology revised criteria for the classification of definite SLE and who had attended at least 3 office visits were included in this study. As part of their routine care, all patients underwent a history-taking and physical examination by physicians (SM, AK, and KM) who were blinded to the results of the E-C3d and E-C4d assays. The majority of the patients were evaluated by a single physician (SM). SLE disease activity was measured at the time of each clinic visit, using the SLAM (3) and SELENA–SLEDAI (4). All physicians were trained in completion of these disease activity indices. All records were reviewed and verified by a single reviewer (AK).
Patients with other diseases
Two hundred ninety randomly selected patients with 1 of 16 other rheumatologic, inflammatory, or hematologic diseases were recruited from subspecialty clinics affiliated with the University of Pittsburgh. These diseases included systemic sclerosis (n = 69), inflammatory myopathy (n = 52), rheumatoid arthritis (n = 44), chronic hepatitis C virus infection (n = 45), primary Sjögren’s syndrome (n = 24), primary antiphospholipid syndrome (n = 9), urticarial vasculitis (n = 8), sickle cell disease (n = 8), primary Raynaud’s phenomenon (n = 6), systemic vasculitis (n = 5), stem cell transplant (n = 8), cutaneous lupus (n = 3), coagulopathy (n = 4), psoriatic arthritis (n = 2), sarcoidosis (n = 1), and osteoarthritis (n = 2).
Healthy control subjects
Healthy control subjects were recruited through advertisements posted on the University of Pittsburgh campus. To confirm their healthy status, these participants completed a brief questionnaire regarding obvious medical conditions.
Flow cytometry characterization
At the time of the study visit, a 5-cc sample of blood from each study participant was collected in EDTA as an anticoagulant (Becton Dickinson, Franklin Lakes, NJ). The samples were analyzed within 24 hours of collection. Whole blood was diluted in phosphate buffered saline (PBS) containing 1% bovine calf serum, and erythrocytes were pelleted, washed with PBS containing bovine calf serum, and aliquotted for antibody staining. Mouse monoclonal antibodies that recognize human C4d or human C3d (Quidel, San Diego, CA) or the isotype-matched control MOPC21 were added to erythrocytes at a concentration of 10 µg/ml. Fluorescein isothiocyanate–conjugated goat anti-mouse IgG F(ab′)2 (Jackson ImmunoResearch, West Grove, PA) was added at a concentration of 10 µg/ml. Cells were analyzed by flow cytometry using a FACSCalibur flow cytometer (Becton Dickinson Immunocytometry Systems, San Jose, CA). Erythrocytes were electronically gated based on forward and side scatter properties to include only single cells. Surface expression of C4d and C3d on gated cells was expressed as the specific mean fluorescence intensity (C4d- or C3d-specific mean fluorescence minus the isotype control mean fluorescence). Quality control of this assay has been demonstrated previously (19).
Statistical analysis
Descriptive statistics were computed as the mean ± SD or the median (with interquartile range [IQR]), depending on the distribution of the continuous data. Frequency distributions were determined for categorical variables. Independent-group t-tests or Wilcoxon’s rank sum tests for continuous variables and chi-square tests for categorical variables were used in the univariate analysis of the demographic characteristics between the SLE group and the comparative groups (control subjects and patients with other diseases).
The SELENA–SLEDAI and SLAM were used to determine the association of E-C4d and E-C3d levels with the disease course. A modified SELENA–SLEDAI was created by excluding the serum C3, C4, and anti–double-stranded DNA (anti-dsDNA) antibody parameters, which would have scored as 2 for hypocomplementemia and the presence of anti-dsDNA antibodies separately. Total scores for the modified SLEDAI and SLAM were used as continuous variables.
The primary statistical tools for relating the biomarkers to disease progression included multivariable linear modeling for the dependent measures. Although regression provides a valuable tool in relating the biomarker to clinical status, a single common regression for all study patients with SLE is inappropriate. Different patients have diverse baseline levels of E-C3d and E-C4d and SLE disease activity scores. Therefore, a patient-specific approach that incorporates these differences must be used. For this purpose, a linear mixed-effects model was used, with the patient defining a factor and the potential biomarker defining a covariate. In this way, each patient’s evolving clinical status was regressed on each of the biomarkers.
Overall, patient-to-patient differences are reflected in the patient effects (which define patient-specific regression intercepts in the regression of SLE disease activity on biomarkers), but a common biomarker slope was used for the different patients. Using symbols, if yit is the clinical measure on patient i and time t, and xit is the value of the biomarker on the same patient at the same time, the statistical model is as follows: yit = μi + β xit + eit, where β is the coefficient of the regression of the clinical measure on the biomarker, μi is the patient-specific true clinical status at xit = 0, and eit is a random error term. Patient–time combinations in which x or y is missing are ignored in the fitting. The observation time t does not appear explicitly in the model; its effect is implicit in the time variation of the biomarker and clinical status.
This linear mixed-effects model was fitted using SAS mixed procedure software (SAS, Cary, NC), treating patients as a random effect. Wald’s test of the coefficients was used to determine whether each independent variable adds predictive value to all other independent variables in the regression model. The partial R2 value shows the contribution of each independent variable to the predictive capability of the regression model.
RESULTS
The 157 patients with SLE had a median of 4 consecutive visits per patient (range 3–13) and a total of 1,005 patient-visits. The majority of the patients with other diseases (n = 290) and healthy control subjects (n = 256) had a single visit (range 1–18) and 660 patient-visits (range 1–13) and 395 person-visits, respectively. At the time of entry into the study, the mean ± SD age of the patients with SLE was 41.1 ± 12.6 years (range 18–75 years); 79.2% of these patients were white, and 95.5% were female. The mean ± SD age of the patients with other diseases at the time of entry was 51.7 ± 14 years; 88.3% were white, and 69.3% were female. The mean ± SD age of the healthy control subjects at the time of entry was 44.7 ± 12.9 years; 86.9% were white, and 89.7% were female. The group of patients with other diseases and the group of healthy control subjects were significantly older and more likely to be white compared with the SLE group (P < 0.001). However, E-C3d and E-C4d levels were not influenced by age or ethnicity (data not shown). The median disease duration for lupus patients was 8.8 years (IQR 2.4–14.9 years), and the median SLAM and SELENA–SLEDAI scores at the time of entry were 5 (IQR 3–8) and 2 (IQR 2–4), respectively (Table 1). Patients with other diseases predominantly had connective tissue diseases, including systemic sclerosis, inflammatory myopathy, and rheumatoid arthritis.
Table 1.
Baseline clinical characteristics of the 157 patients with systemic lupus erythematosus*
| Age at diagnosis, mean ± SD years | 31.4 ± 13.2 |
| Disease duration, median (IQR) years from diagnosis to study entry |
8.8 (2.4–14.9) |
| Malar rash | 47 |
| Discoid rash | 16 |
| Photosensitivity | 50 |
| Oral ulcer | 52 |
| Arthritis | 86 |
| Serositis | 42 |
| Renal disease | 41 |
| Neurologic disease (seizure or psychosis) | 12 |
| Hematologic manifestations | 59 |
| Hemolytic anemia | 44 |
| Leukopenia | 57 |
| Thrombocytopenia | 17 |
| Immunologic test result ever positive | 80 |
| Antinuclear antibodies | 99 |
| Anti–double-stranded DNA antibody | 66 |
| Anti-Sm | 16 |
| Antiphospholipid antibody† | 50 |
| Anti-SSA/Ro or anti-SSB/La | 17 |
| Anti–U1 RNP | 14 |
| Rheumatoid factor | 5 |
| Raynaud’s phenomenon | 57 |
| Complete blood cell count at entry | |
| White blood cells × 1,000/µl, mean ± SD | 5.9 ± 2.8 |
| Hemoglobin, mean ± SD gm/dl | 12.4 ± 1.5 |
| Platelets × 1,000/µl, mean ± SD | 252.3 ± 88.4 |
| Thrombocytopenia | 2 |
| SLAM score, median (IQR) | 5 (3–8) |
| SELENA–SLEDAI score, median (IQR) | 2 (2–4) |
| Reduced serum C3 level | 52 |
| Reduced serum C4 level | 56 |
| Elevated erythrocyte sedimentation rate | 55 |
Except where indicated otherwise, values are the percent of patients. IQR = interquartile range; SLAM = Systemic Lupus Activity Measure; SELENA–SLEDAI = Safety of Estrogens in Lupus Erythematosus: National Assessment version of the Systemic Lupus Erythematosus Disease Activity Index.
Includes abnormal levels of anticardiolipin antibodies (67 patients), positive test result for lupus anticoagulant (25 patients), or a false-positive test result for syphilis (13 patients).
At baseline, patients with SLE had significantly higher levels of E-C3d (median 2.5 versus 0.5 and 0.8 specific MFI, respectively) and E-C4d (median 12.9 versus 4.9 and 7.0 specific MFI, respectively) than did healthy control subjects and patients with other diseases (all P < 0.0001). The within-patient and between-patient variances for E-C3d and E-C4d were high in the SLE group compared with the other 2 groups (Table 2). The high variability in the levels of the erythrocyte-bound complement activation products (EB-CAPs) E-C3d and E-C4d in lupus patients demonstrated that the levels of these biomarkers vary not only among patients with lupus but also within the same lupus patient over time. Multivariable analysis of variance demonstrated the correlation matrices of serum C3 and C4 and the companion markers E-C3d and E-C4d within patients over time. The within-patient correlation matrices demonstrated significant but weak negative correlations (−0.16 ≤ r ≤ −0.14; all P < 0.05) between the EB-CAP biomarkers and the serum biomarkers (C3 and C4). Therefore, any information that the EB-CAPs contribute regarding lupus disease activity can be expected to be additive to the information provided by serum C3 and C4 levels. Of note, the highly significant correlation between E-C3d and E-C4d levels (r = 0.79) may mask the respective individual contributions of these biomarkers, and this must be considered in multivariable models using both E-C3d and E-C4d.
Table 2.
Within-subject and between-subject variance of the erythrocyte biomarkers in SLE patients, patients with other diseases, and healthy controls*
| Lupus biomarker | Patients with SLE (n = 157) |
Patients with other diseases (n = 290) |
Healthy controls (n = 256) |
|---|---|---|---|
| E-C3d | |||
| Grand mean | 3.44 | 1.12 | 0.71 |
| Variance within | 5.87 | 3.08 | 0.47 |
| Variance between | 16.06 | 0.94 | 0.45 |
| E-C4d | |||
| Grand mean | 16.79 | 8.23 | 6.03 |
| Variance within | 86.96 | 13.80 | 4.27 |
| Variance between | 217.63 | 25.3 | 20.2 |
SLE = systemic lupus erythematosus; E-C3d = erythrocyte-bound C3d.
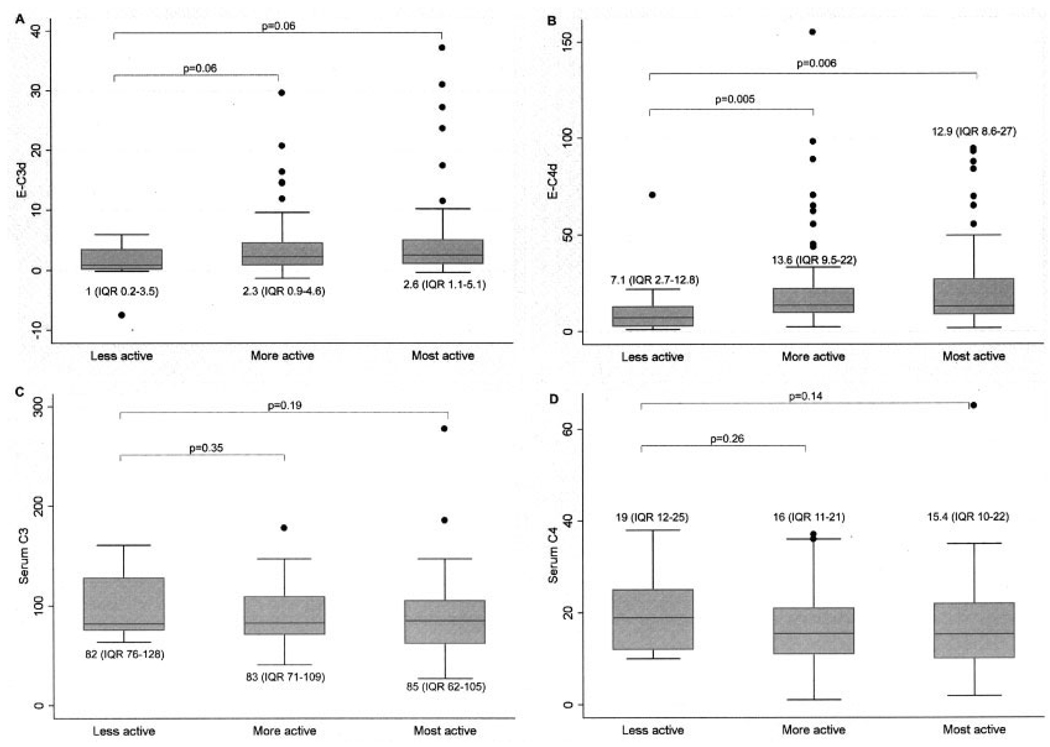
In an initial exploration of the relationship between SLE disease activity and the biomarkers, the baseline levels of SLE activity were categorized as “less active” (modified SELENA–SLEDAI score of 0 and SLAM score of <2), “more active” (modified SELENA–SLEDAI score of 1–3 or SLAM score of 2–6), and “most active” (modified SELENA–SLEDAI score of ≥4 or SLAM score of ≥7). Using this categorization, Figure 1 shows that E-C3d (both P = 0.06) and E-C4d levels (P = 0.005 and P = 0.006, respectively) were higher in SLE patients with “more active” and “most active” disease compared with those whose disease was less active at the initial visit. The traditional serum C3 and C4 measurements were not associated with SLE disease activity. One patient with “most active” disease had extremely high serum C3 and C4 levels at the initial and followup visits due to cryoglobulin interference in the serum C3 and C4 assays; thus, this patient was excluded from the multivariable analysis. This patient had severe fatigue, vasculitis, lymphopenia, renal insufficiency, and proteinuria. Interestingly, the levels of E-C3d and E-C4d were appropriately elevated in this patient. The results of this cross-sectional analysis remained unchanged even after this patient was excluded.
Figure 1.
Levels of lupus biomarkers in patients with systemic lupus erythematosus, according to disease activity categories as defined by Systemic Lupus Activity Measure and Safety of Estrogens in Lupus Erythematosus: National Assessment version of the Systemic Lupus Erythematosus Disease Activity Index scores at the initial visit. Data are presented as box plots, where the boxes represent the 25th to 75th percentiles (interquartile range [IQR]), the lines within the boxes represent the median, and the lines outside the boxes represent the 10th and 90th percentiles. Circles indicate outliers. E-C3d = erythrocyte-bound C3d.
Longitudinal linear mixed-effects model analysis of disease activity in the 156 lupus patients over time demonstrated that E-C3d and E-C4d levels tracked the clinical activity of lupus patients, with a high degree of statistical significance. As shown in Table 3, the levels of both E-C3d and E-C4d were univariately associated with the SLAM (both P < 0.001) and the modified SELENA–SLEDAI (P = 0.02 and P = 0.003, respectively). Although serum C3 was associated with the SLAM and the modified SELENA–SLEDAI (P < 0.001), serum C4 was not associated with either disease activity index (P = 0.07 and P = 0.21, respectively).
Table 3.
Longitudinal analysis of univariate association between lupus biomarkers and SLE disease activity, using SLAM and modified SELENA–SLEDAI scores in a cohort of 156 SLE patients*
| SLAM score | Modified SELENA-SLEDAI score† | |||||||
|---|---|---|---|---|---|---|---|---|
| Biomarker | Partial R2‡ | Coefficient | SE | P | Partial R2‡ | Coefficient | SE | P |
| EB-CAP | ||||||||
| E-C3d | 0.018 | 0.10 | 0.03 | 0.0004 | 0.008 | 0.05 | 0.02 | 0.02 |
| E-C4d | 0.019 | 0.03 | 0.01 | 0.0003 | 0.013 | 0.02 | 0.01 | 0.003 |
| Traditional | ||||||||
| Serum C3 | 0.020 | −1.49 | 0.40 | 0.0002 | 0.021 | −1.10 | 0.29 | 0.0001 |
| Serum C4 | 0.005 | −0.44 | 0.25 | 0.07 | 0.002 | −0.21 | 0.17 | 0.21 |
| Anti-dsDNA | 0.018 | 1.02 | 0.29 | 0.0005 | 0.009 | 0.68 | 0.27 | 0.01 |
SLE = systemic lupus erythematosus; SLAM = Systemic Lupus Activity Measure; EB-CAP = erythrocyte-bound complement activation product; E-C3d = erythrocyte-bound C3d.
The modified Safety of Estrogens in Lupus Erythematosus: National Assessment version of the Systemic Lupus Erythematosus Disease Activity Index (SELENA–SLEDAI) excluded serum C3, C4, and anti–double-stranded DNA (anti-dsDNA) antibody parameters.
Type II sums of squares tests.
A linear mixed-effects model analysis (Table 4) showed that the E-C4d level continued to be significantly associated with both the SLAM (P = 0.006) and modified SELENA–SLEDAI (P = 0.03) scores, whereas E-C3d was associated only with the SLAM score (P = 0.005), after adjusting for levels of serum C3, serum C4, and the presence of anti-dsDNA antibodies. Serum C4 was not associated with the SLAM or SELENA–SLEDAI scores in the multivariable analysis. The EB-CAP biomarkers had partial R2 values similar to those of the traditional biomarkers in the multivariable analysis.
Table 4.
Longitudinal analysis of association between lupus biomarkers and SLE disease activity, using SLAM and modified SELENA–SLEDAI scores in 156 SLE patients*
| Partial R2† | Coefficient | SE | P | |
|---|---|---|---|---|
| SLAM | ||||
| Regression model 1 | ||||
| C3 | 0.007 | −1.09 | 0.48 | 0.025 |
| C4 | 0.001 | 0.27 | 0.29 | 0.36 |
| Anti-dsDNA | 0.030 | 1.17 | 0.26 | <0.0001 |
| E-C3d | 0.011 | 0.08 | 0.03 | 0.005 |
| Regression model 2 | ||||
| C3 | 0.007 | −1.09 | 0.48 | 0.023 |
| C4 | 0.001 | 0.27 | 0.29 | 0.35 |
| Anti-dsDNA | 0.029 | 1.16 | 0.26 | <0.0001 |
| E-C4d | 0.011 | 0.02 | 0.008 | 0.006 |
| Modified SELENA-SLEDAI‡ | ||||
| Regression model 3 | ||||
| C3 | 0.013 | −1.05 | 0.36 | 0.003 |
| C4 | 0.004 | 0.33 | 0.21 | 0.11 |
| Anti-dsDNA | 0.014 | 0.61 | 0.19 | 0.002 |
| E-C3d | 0.004 | 0.032 | 0.02 | 0.11 |
| Regression model 4 | ||||
| C3 | 0.012 | −1.03 | 0.36 | 0.004 |
| C4 | 0.004 | 0.35 | 0.21 | 0.099 |
| Anti-dsDNA | 0.014 | 0.60 | 0.19 | 0.002 |
| E-C4d | 0.007 | 0.01 | 0.01 | 0.03 |
SLE = systemic lupus erythematosus; SLAM = Systemic Lupus Activity Measure; E-C3d = erythrocyte-bound C3d.
Type II sums of squares test.
The modified Safety of Estrogens in Lupus Erythematosus: National Assessment version of the Systemic Lupus Erythematosus Disease Activity Index (SELENA–SLEDAI) excluded serum C3, C4, and anti–double-stranded DNA (anti-dsDNA) parameters.
DISCUSSION
To our knowledge, this is the most extensive longitudinal cohort study of lupus biomarkers reported to date, as measured by the number of patients, the number of patient visits, and the duration of the investigation. The results of our study suggest that E-C3d and E-C4d levels are informative measures of complement activation and lupus disease activity and convey information independent of that provided by serum C3 and C4 levels, which are the assays currently used in routine clinical practice. These observations contribute at several levels to our understanding of the intimate link between complement and lupus.
First, the findings of this study further support the hypothesis that an inflammatory state should be more accurately reflected by measurement of complement activation products as compared with complement precursors. The results of previous studies suggested that soluble complement activation products may be useful measures of lupus disease activity (11,13). However, despite extensive study, soluble products of complement activation have not replaced serum C3 and C4 as biomarkers of lupus disease activity. Several considerations regarding the biology of soluble complement activation products might explain their failure to emerge as superior measures of complement activation. For instance, the half-life of these peptides in the circulation is likely to be short, all circulating cells have receptors for C3- and C4-derived complement activation products, and products of C3 and C4 activation are capable of covalent attachment to other molecules and cell surfaces. This rationale led to our investigation of cell-bound CAPs as more informative complement-based lupus biomarkers.
Second, the results of this study confirm prior reports indicating that the serum C4 level is not a useful marker of disease activity in lupus. C4 may be inferior to C3 as a lupus biomarker because of the frequency of C4-null alleles in lupus patients, because it is not a component of the alternative complement pathway, because it occurs earlier in the complement cascade than does C3, or due to a combination of these and other factors yet to be identified. Thus, the results of this study, together with data from prior studies, question the usefulness of repeated measurement of serum C4 levels in lupus patient care.
Third, the significantly higher interpatient and intrapatient variances of E-C3d and E-C4d levels among SLE patients support the view that there may be a unique role for complement in the pathogenesis of lupus compared with other autoimmune and inflammatory diseases. The presence of low levels of E-C4d on normal erythrocytes and on erythrocytes from patients with other diseases, in contrast to the significantly higher levels observed on the erythrocytes of patients with lupus, could be interpreted in 1 of at least 2 ways. First, excessive generation of complement activation products may overwhelm normal regulatory mechanisms that are present in the circulation and on the surfaces of erythrocytes. Second, deficient regulation of normal complement activation may be responsible for the high levels of E-C4d that are relatively unique to lupus. These 2 possibilities are not mutually exclusive but, taken together, they suggest that SLE may be a particularly suitable target for therapeutic anticomplement intervention. E-C3d and E-C4d levels would be particularly informative as biomarkers for such clinical trials.
Fourth, the relatively low partial R2 values observed for all of the candidate biomarkers in this study indicate that despite the recognized utility of serum complement levels and anti-dsDNA antibody titers in monitoring patients with lupus, the complexity and heterogeneity of the disease are such that any single biomarker will provide limited information regarding the patient’s clinical state. This is consistent with decades of studies that demonstrated limited usefulness of even those biomarkers, especially serum C4, when used in routine clinical practice to monitor disease flares and response to treatment. Ultimately, a panel of lupus biomarkers may be required to effectively monitor patients in both clinical practice and clinical trials. In addition to monitoring overall lupus disease activity, further clinical validation of these assays may also demonstrate their utility in monitoring organ-specific manifestations of the disease.
Finally, there is general acceptance that biomarkers are needed to aid physicians in the diagnosis of lupus and monitoring patients with lupus and to minimize subjectivity. It is often difficult distinguishing disease activity from infection in a lupus patient who has fevers, fatigue, and joint pain. A biomarker with better specificity for disease activity would be extremely helpful. Pilot data from our group indicate that these cell-bound complement assays can distinguish infection from changes in disease activity. It is unlikely that any biomarker will be useful if it is taken completely out of clinical context. The clinical impression and judgment of individual physicians will always be important.
In conclusion, there is an urgent need for lupus biomarkers to monitor disease activity in clinical care, clinical research, and clinical trials. This longitudinal 5-year cohort study has demonstrated that E-C3d and E-C4d levels are informative measures of complement activation and disease activity in lupus as determined by the SLAM and the SELENA–SLEDAI. Further investigation of E-C3d and E-C4d levels should be considered for potential use in routine patient care, clinical research, and testing of potential new therapeutic agents.
ACKNOWLEDGMENTS
We gratefully acknowledge the following colleagues for providing patient blood samples and clinical information for this study: Dr. Dana Ascherman, Dr. Brian Berk, Dr. Thomas Medsger, Dr. Chester Oddis, Dr. Margaret Ragni, Dr. William Ridgway, and Dr. Mary Chester Wasko. We also thank Abbey Nilson and Dana Wright for skilled technical assistance.
Supported by the NIH (grants R01-HL-074335, R01-AR-4676402, R01-AR-46588, NCRR/GCRC M01-RR-00056, K24-AR-02213, and K23-AR-051044), the Alliance for Lupus Research, the Arthritis Foundation, the Lupus Research Institute, and the Lupus Foundation of America.
Footnotes
Ms Navratil has received royalties (less than $10,000) for the cell-bound C4d/C3d assay licensed to Cypress Bioscience, Inc. Dr. Hawkins has received consulting fees from Cellatope, Inc. (more than $10,000). Dr. Ahearn has received consulting fees, speaking fees, and/or honoraria from Cellatope, Inc. (more than $10,000) and has received licensing fees from Cypress Bioscience, Inc. Dr. Manzi has received consulting fees, speaking fees, and/or honoraria from Cellatope, Inc. (more than $10,000) and has received licensing fees from Cypress Bioscience, Inc.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Kao had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Kao, Navratil, Ruffing, Liu, Danchenko, Ahearn, Manzi.
Acquisition of data. Kao, Navratil, McKinnon, Danchenko, Manzi.
Analysis and interpretation of data. Kao, Liu, Hawkins, Ahearn, Manzi.
REFERENCES
- 1.Illei G, Lipsky P. Biomarkers in systemic lupus erythematosus. Curr Rheumatol Rep. 2004;6:382–390. doi: 10.1007/s11926-004-0013-4. [DOI] [PubMed] [Google Scholar]
- 2.Illei G, Tackey E, Lapteva L, Lipsky P. Biomarkers in systemic lupus erythematosus. II. Markers of disease activity. Arthritis Rheum. 2004;50:2048–2065. doi: 10.1002/art.20345. [DOI] [PubMed] [Google Scholar]
- 3.Liang M, Socher S, Larson M, Schur P. Reliability and validity of six systems for the clinical assessment of disease activity in systemic lupus erythematosus. Arthritis Rheum. 1989;32:1107–1118. doi: 10.1002/anr.1780320909. [DOI] [PubMed] [Google Scholar]
- 4.Buyon J, Petri M, Kim M, Kalunian KC, Grossman J, Hahn BH, et al. The effect of combined estrogen and progesterone hormone replacement therapy on disease activity in systemic lupus erythematosus: a randomized trial. Ann Intern Med. 2005;142:953–962. doi: 10.7326/0003-4819-142-12_part_1-200506210-00004. [DOI] [PubMed] [Google Scholar]
- 5.Gordon C, Sutcliffe N, Skan J, Stoll T, Isenberg D. Definition and treatment of lupus flares measured by the BILAG index. Rheumatology (Oxford) 2003;42:1372–1379. doi: 10.1093/rheumatology/keg382. [DOI] [PubMed] [Google Scholar]
- 6.Schur P, Sandson J. Immunological factors and clinical activity in systemic lupus erythematosus. N Engl J Med. 1968;278:533–538. doi: 10.1056/NEJM196803072781004. [DOI] [PubMed] [Google Scholar]
- 7.Walport M. Complement and systemic lupus erythematosus. Arthritis Res. 2002;4 Suppl 3:S279–S293. doi: 10.1186/ar586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lloyd W, Schur P. Immune complexes, complement, and anti-DNA in exacerbations of systemic lupus erythematosus (SLE) Medicine (Baltimore) 1981;60:208–217. doi: 10.1097/00005792-198105000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Hopkins P, Belmont H, Buyon J, Philips M, Weissmann G, Abramson S. Increased levels of plasma anaphylatoxins in systemic lupus erythematosus predict flares of the disease and may elicit vascular injury in lupus cerebritis. Arthritis Rheum. 1988;31:632–641. doi: 10.1002/art.1780310508. [DOI] [PubMed] [Google Scholar]
- 10.Sturfelt G, Jonasson L, Sjoholm A. Sequential studies of complement activation in systemic lupus erythematosus. Scand J Rheumatol. 1985;14:184–196. doi: 10.3109/03009748509165503. [DOI] [PubMed] [Google Scholar]
- 11.Buyon J, Tamerius J, Belmont H, Abramson S. Assessment of disease activity and impending flare in patients with systemic lupus erythematosus: comparison of the use of complement split products and conventional measurements of complement. Arthritis Rheum. 1992;35:1028–1037. doi: 10.1002/art.1780350907. [DOI] [PubMed] [Google Scholar]
- 12.Falk R, Agustin M, Dalmasso P, Kim Y, Lam S, Michael A. Radioimmunoassay of the attack complex of complement in serum from patients with systemic lupus erythematosus. N Engl J Med. 1985;312:1594–1599. doi: 10.1056/NEJM198506203122502. [DOI] [PubMed] [Google Scholar]
- 13.Manzi S, Rairie JE, Carpenter AB, Kelly RH, Jagarlapudi SP, Sereika SM, et al. Sensitivity and specificity of plasma and urine complement split products as indicators of lupus disease activity. Arthritis Rheum. 1996;39:1178–1188. doi: 10.1002/art.1780390716. [DOI] [PubMed] [Google Scholar]
- 14.Mollnes TE, Haga HJ, Brun JG, Nielsen EW, Sjoholm A, Sturfeldt G, et al. Complement activation in patients with systemic lupus erythematosus without nephritis. Rheumatology (Oxford) 1999;38:933–940. doi: 10.1093/rheumatology/38.10.933. [DOI] [PubMed] [Google Scholar]
- 15.Abrass C, Nies K, Louie J, Border W, Glassock R. Correlation and predictive accuracy of circulating immune complexes with disease activity in patients with systemic lupus erythematosus. Arthritis Rheum. 1980;23:273–282. doi: 10.1002/art.1780230302. [DOI] [PubMed] [Google Scholar]
- 16.Esdaile J, Joseph L, Abrahamowicz M, Danoff D, Clarke A. Routine immunologic tests in systemic lupus erythematosus: is there a need for more studies? J Rheumatol. 1996;23:1891–1896. [PubMed] [Google Scholar]
- 17.Esdaile J, Abrahamowicz M, Joseph L, MacKenzie T, Li Y, Danoff D. Laboratory tests as predictors of disease exacerbations in systemic lupus erythematosus: why some tests fail. Arthritis Rheum. 1996;39:370–378. doi: 10.1002/art.1780390304. [DOI] [PubMed] [Google Scholar]
- 18.Liu CC, Ahearn J, Manzi S. Complement as a source of biomarkers in systemic lupus erythematosus: past, present, and future. Curr Rheumatol Rep. 2004;6:85–88. doi: 10.1007/s11926-004-0046-8. [DOI] [PubMed] [Google Scholar]
- 19.Manzi S, Navartil JS, Ruffing MJ, Liu CC, Danchenko N, Nilson SE, et al. Measurement of erythrocyte C4d and complement receptor 1 in systemic lupus erythematosus. Arthritis Rheum. 2004;50:3596–3604. doi: 10.1002/art.20561. [DOI] [PubMed] [Google Scholar]
- 20.Liu CC, Manzi S, Kao AH, Navartil JS, Ruffing MJ, Ahearn JM. Reticulocytes bearing C4d as biomarkers of disease activity for systemic lupus erythematosus. Arthritis Rheum. 2005;52:3087–3099. doi: 10.1002/art.21305. [DOI] [PubMed] [Google Scholar]
- 21.Tieley C, Romans D, Crookston M. Localization of Chido and Rodgers determinants to the C4d fragment of human C4. Nature. 1978;276:713–715. doi: 10.1038/276713a0. [DOI] [PubMed] [Google Scholar]
- 22.Atkinson JP, Chan AC, Karp DR, Killion CC, Brown R, Spinella D, et al. Origin of the fourth component of complement related Chido and Rodgers blood group antigens. Complement. 1988;5:65–76. doi: 10.1159/000463037. [DOI] [PubMed] [Google Scholar]
- 23.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 24.Hochberg MC for the Diagnostic and Therapeutic Criteria Committee of the American College of Rheumatology. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus [letter] Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]