Abstract
Adult mood disturbances are highly correlated with obesity, although little is known about the developmental relationship between mood disorders and weight. This study investigated the relationship between childhood psychopathology and weight over the course of 3 years. Body Mass Index (BMI) percentiles and demographic data of children (ages 8–18) with depression (n = 143) or anxiety (n = 43) were compared to healthy controls (n = 99). Both childhood depression (χ2 = 4.6, p = 0.03) and anxiety (χ2 = 6.0, p = 0.01) were associated with increased BMI percentiles. Compared to controls, BMI percentiles of depressed females over the course of the study differed profoundly (χ2 = 7.0, p = 0.01) and BMI percentiles of anxious females approached significance (χ2 = 3.7, p = 0.06). Males with anxiety showed a greater trend towards overweight (χ2 = 3.3, p = 0.07) in comparison to controls. The major finding that depression and anxiety are associated with increased BMI percentiles in a non-obese sample suggests that childhood psychopathology is an important factor that should be carefully monitored.
Keywords: Weight, Depression, Anxiety, Adolescent, Body mass index
Introduction
Over the past three decades, childhood obesity rates have more than tripled for children 6–11 years-old and more than doubled for preschool children 2–5 years old and adolescents 12–19 years old [1]. Based on the National Health and Nutrition Examination Survey (NHANES), 31% of children ages 6–19 are at risk for overweight and obesity and 16% of children ages 6–19 are already overweight [2]. This obesity epidemic highlights the need to increase prevention and intervention efforts, possibly by targeting younger and less overweight children. Thus, it is critical to identify factors that are associated with increased weight in childhood.
One approach to controlling the national obesity epidemic involves an increased understanding of and attention to the relationship between weight and mood disturbances [3, 4]. Given the strong correlations among clinically significant weight gain, depression, and anxiety [5, 6], a current area of focus is the connection between psychopathology and weight in childhood. Affective disturbances commonly occur during development [7, 8], and recent studies suggest that increased weight is correlated with depressive and anxiety symptoms in childhood, as demonstrated by greater Body Mass Index (BMI, defined as height to weight ratio [kilograms/meters squared]) [6, 9–11]. Given that adolescence is a significant period of emotional and physical maturation [12], it is fundamental to acknowledge the influence of mood/anxiety disorders on weight and to explore this relationship to better understand, treat, and prevent pediatric obesity [3, 12, 13].
An important area to explore is the role of gender in weight and mood/anxiety trajectories. The child and adult literature discuss gender differences in the relationships between overweight and mood, although there are divergent findings about the distinctions between males and females. Many studies suggest that obesity and emotional disorders tend to occur more frequently among females [3, 14–16]. Anderson et al. [3] suggest that, for girls, anxious and depressive symptomatology in childhood predicts higher weight in adulthood. Furthermore, some research suggests that the relationship between weight and mood is more pronounced among women than men [17], whereas the association between weight and anxiety is stronger among men than women [18]. Some research, however, suggests that these relationships are similar across genders [19], which may indicate that those who are obese or overweight are at a greater risk for emotional disorders, regardless of gender.
While the knowledge base for overweight and obesity continues to expand, the specific mechanisms promoting weight gain in children remain unclear. Existing research has not investigated children with major depressive disorders or anxiety disorders and tracked BMI prospectively over significant periods of time [20]. This study will advance knowledge in the field by examining the longitudinal trajectory of children and adolescents with depression (i.e., major depressive disorder) and anxiety (i.e., generalized anxiety disorder, social phobia) who are not obese at baseline in comparison to psychologically healthy controls. For this study, we have two main hypotheses. First, we predict significantly greater BMI percentiles for children with depression or anxiety than normal controls. Second, we hypothesize that gender will be associated with BMI. This study is the first to address some of the methodological caveats and to explore these relationships longitudinally using validated objective measures of weight, height, depression, and anxiety in non-obese children with clinical diagnoses.
Methods
Participants
This sample includes data from 285 children participating in a longitudinal study examining psychobiological underpinnings of depression [21, 22]. Children (49% female, 81% Caucasian and 10% African American) ranged in age from 8 to 18 (M = 11.71; SD = 2.25) at baseline. Participants were divided into three groups based on the child’s current psychiatric diagnoses at the time of the baseline assessment: (a) Major Depressive Disorder (MDD), n = 143; (b) Anxiety Disorder, n = 43; and (c) Low-risk for depression/Healthy controls, n = 99.
Inclusion Criteria
For our analyses, we restricted the sample to the 285 children with baseline data on BMI percentile and a baseline diagnosis of depression, anxiety or control. Children with MDD met diagnostic criteria according to DSM-III-R [23] or DSM-IV [24] classification for major depressive disorder (with or without dysthymic disorder). Children with anxiety met diagnostic criteria for generalized anxiety disorder, separation anxiety disorder, or social phobia, according to DSM-III-R [23] or DSM-IV [24] classification. For children with both depression and anxiety, the primary Axis I diagnosis was defined as the disorder that caused the most clinical distress and impairment to the participant. If this decision was not able to be made by the clinician, the participant was not included in the current sample. To be in the low-risk/control group, children were required to be free of any lifetime psychopathology and to have no first-degree relatives with a lifetime episode of any mood or psychotic disorder; no second-degree relatives could have a lifetime history of childhood-onset, recurrent, psychotic, or bipolar depression or schizoaffective or schizophrenic disorder; and no more than 20% of second-degree relatives could have a lifetime episode of MDD.
Exclusion Criteria
Since the children in this study were originally recruited to participate in a broader set of biological protocols [25], the following exclusionary criteria applied at the time of the initial interview: (1) the use of any medication with central nervous system effects within the past 2 weeks (including psychotropics); (2) significant medical illness; (3) extreme obesity or growth failure; (4) IQ of 70 or less; (5) inordinate fear of intravenous needles; and (6) specific learning disabilities.
Furthermore, for the purposes of this paper, children in the larger sample were also excluded if they were healthy but high-risk for developing MDD or an anxiety disorder, based on their family history. Children were considered to be at high risk if they had at least one-first-degree and one-second-degree relative with a history of childhood-onset, recurrent, bipolar, or psychotic depression and they were required never to have had a lifetime episode of any mood disorder [25].
Procedures
All study procedures were approved by the University of Pittsburgh’s Institutional Review Board. Between January 1987 and April 2002, children were recruited from three sources: (1) community advertisements (primarily radio and newspaper ads), (2) inpatient and outpatient clinics at a major medical center in which children or their parents were being treated, and (3) referrals from other research studies or other participants in the present study. Interested participants contacted research staff and completed a phone screen to determine initial eligibility for the study. They were invited to the laboratory to complete more comprehensive structured interviews if the phone screen suggested that they might meet criteria for the study. At the laboratory visit they completed psychiatric interviews, questionnaires, a physical examination, and psychophysiological assessments [25]. A sociodemographic questionnaire was used to obtain sociodemographic information from parent and child such as age, gender and socioeconomic status [26].
Structured diagnostic interviews were administered to establish lifetime and present psychiatric diagnoses and familial risk for affective disorder. In the initial years of the study, children were administered the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic version (K-SADS-E) [27] to assess lifetime history and the Schedule for Affective Disorders and Schizophrenia for School-Age Children (6–18 years)-Present Episode version (K-SADS-P) [28] to assess current episodes. During the later years of the study, the Schedule for Affective Disorders and Schizophrenia in School-Age Children-Present and Lifetime version (K-SADS-PL) [29] was used, which combines aspects of the K-SADS-P and K-SADS-E into one interview. Parents and children were interviewed and if discrepancies were found, clinicians integrated information from both sources to make final decisions. Qualifying children completed a battery that included psychophysiological tests and questionnaires about the psychosocial environment [25]. Upon completion of the baseline visit, children were invited to return for annual follow-up visits that included follow-up psychiatric interviews for children and re-administration of tasks. The present report focuses on psychiatric evaluations completed each year over the 3 years following the baseline assessment. BMI was measured by research associates at each psychiatric evaluation utilizing a calibrated SECA™ scale and stadiometer; EpiInfo NutStat computer program was used to analyze anthropometric data based on the Center for Disease Control’s 2000 standards.
All interviews were carried out by trained Bachelor of Arts- and Master of Arts-level research clinicians. Interrater reliabilities for diagnoses assessed during the course of this study were estimated to be k ≥ 0.70. The results of the interview were presented at a consensus case conference with a child psychiatrist, who reviewed the findings and preliminary diagnosis and provided a final diagnosis based on DSM-III-R or DSM-IV criteria.
Statistical Analyses
Baseline assessments of the relationships between our covariates and diagnoses were performed using ANOVA, chi-squared, or Fisher’s exact tests, as appropriate. Comparisons of BMI percentile with diagnosis and the other covariates were conducted using the nonparametric Wilcoxon or Kruskal–Wallis tests and Spearman correlation coefficients due to the skewed distribution of BMI percentile. The longitudinal associations between diagnosis and BMI percentile for the three time periods included in our study were evaluated using generalized estimating equations (GEE) and linear contrasts were constructed to assess the BMI percentile differences between the depression and control and between anxiety and control subgroups. GEE models allowed the use of all available data for each subject, while also accounting for the correlated structure of the data due to the repeated measures over time. BMI percentile was modeled as a continuous variable assuming compound symmetry. Given that GEE are fairly robust to the normality assumption, untransformed BMI percentiles were used. Alternative GEE approaches (e.g., multinomial) also yielded similar results. In addition to the overall model, separate models were fitted for females and males. The reference models included fixed effects for diagnosis group and time. The interaction between diagnosis group and time was tested to see if the rates of change over time in BMI percentile differ among the three groups, but was not significant for either gender. Adjustments were considered to control for the effects of gender, age, race, and SES. Only terms that added significantly to the model were retained. Missing observations were treated as missing completely at random and all GEE analyses were implemented using SAS PROC GENMOD.
Results
Of the 285 children included in this study, 143 had major depressive disorder, 43 had an anxiety disorder, and 99 were identified as low-risk/control children. Ages at baseline ranged from 8 to 18 (11.71 ± 2.25 years old) with 49% female, 81% Caucasian and 10% African American. The average BMI percentile was 56.34 ± 27.82 and the average SES score was 37.79 ± 14.23, as measured by the Hollingshead Four-Factor Index [26].
Table 1 presents demographic characteristics of participants by diagnostic group. Table 2 shows the results of the GEE models. Both the depressed and the anxious groups had higher BMI percentiles than the control group (differences of 7%, χ2 = 4.6, p = 0.03 for the depressed group and 12, χ2 = 6.0, p = 0.01, for the anxious group respectively). Even more pronounced differences were found for females with an estimated BMI percentile difference of 11 (χ2 = 7.0, p = 0.01) for depressed compared to low risk children. The difference was 14 (χ2 = 3.7, p = 0.06) for anxiety disorder compared to low risk females. For male children neither comparison reached statistical significance. Males with anxiety showed a greater trend towards overweight (difference = 11, χ2 = 3.3, p = 0.07) in comparison to controls. For all males, there was a significant 9% drop in BMI percentile after a year (χ2 = 9.7, p = 0.01).
Table 1.
Demographic characteristics of participants by diagnostic group
| MDD | Anxiety | Low risk | p | |
|---|---|---|---|---|
| N | 143 | 43 | 99 | |
| Age, mean ± SD | 12.1 ± 2.3 | 11.6 ± 2.2 | 11.2 ± 2.1 | 0.01 |
| Sex, % female | 53.1 | 39.5 | 47.5 | 0.27 |
| Race, % black, % other | 14.0, 7.0 | 11.6, 9.3 | 3.0, 12.1 | 0.03 |
| SES (Hollingshead), mean ± SD | 34.1 ± 14.5 | 35.7 ± 13.7 | 43.7 ± 12.3 | 0.00 |
| BMI, mean ± SD | 19.2 ± 3.3 | 19.2 ± 3.1 | 17.5 ± 3.4 | 0.00 |
| BMI percentile, mean ± SD | 59.1 ± 26.8 | 61.9 ± 26.7 | 49.9 ± 28.7 | 0.02 |
MDD major depressive disorder; SES socioeconomic status; BMI Body Mass Index (kg/m2)
Table 2.
Summary of GEE models assessing the relationship of diagnosis and time with BMI percentile
| Model term | Overall model |
Females only |
Males only |
|||
|---|---|---|---|---|---|---|
| Estimate (SE) | p | Estimate (SE) | p | Estimate (SE) | p | |
| ANX–LR difference | 11.6 (4.7) | 0.01 | 13.6 (7.1) | 0.06 | 11.3 (6.2) | 0.07 |
| MDD–LR difference | 7.1 (3.3) | 0.03 | 11.5 (4.3) | 0.01 | 2.4 (3.3) | 0.63 |
| T2–T1 difference | −4.5 (1.8) | 0.01 | − 0.9 (2.4) | 0.72 | − 9.4 (2.5) | 0.01 |
| T3–T1 difference | 0.3 (1.6) | 0.84 | − 0.6 (2.4) | 0.80 | −0.3 (1.8) | 0.87 |
ANX Anxiety; LR Low-risk; MDD Depression; T time; p p—value
While BMI and diagnosis data existed for 285 children at baseline, this decreased to 229 by the second year and 196 children by the third year. No differences existed on key demographic or dependent variables between those who completed the third assessment and those who dropped out. GEE approach estimates parameters using all available data from each year and provides better estimates of the “average” performance at each time point. Figure 1 plots the estimated BMI percentiles by diagnosis across the 3 years for both males and females using the GEE models, and Figs. 2 and 3 display the estimated BMI percentile data separately for females and males, respectively. For females, the depressed and anxiety disorder groups have similar BMI percentiles over time that are higher than low risk group, whereas for males, the anxious group is elevated, while the depressed group is similar to the low risk group.
Fig. 1.
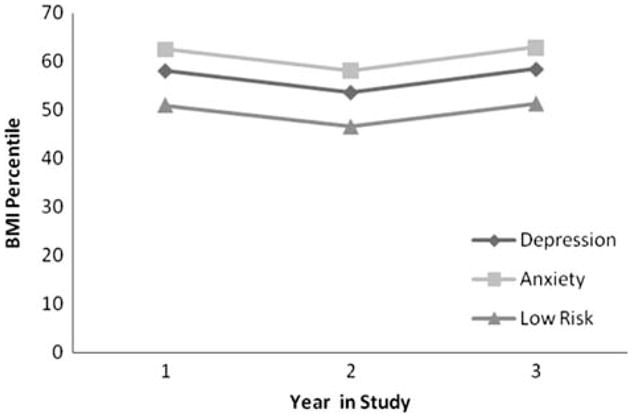
BMI Percentile for Depression, Anxiety, and Low-risk Participants
Fig. 2.
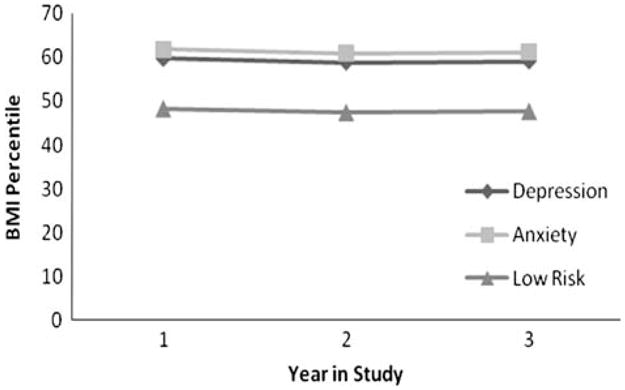
BMI Percentile for Depression, Anxiety, and Low-risk Females
Fig. 3.
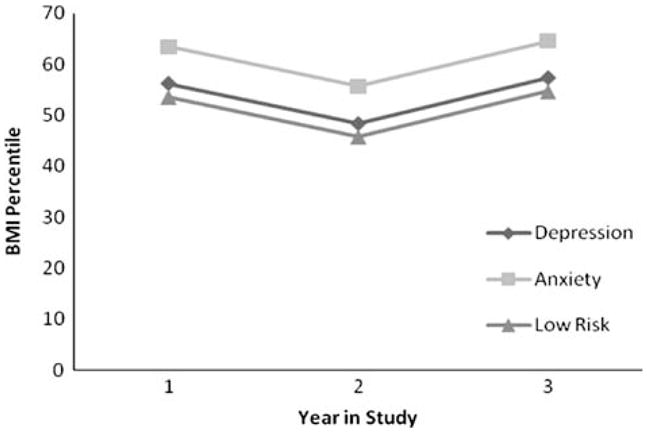
BMI Percentile for Depression, Anxiety, and Low-risk Males
Discussion
This study provides the unique opportunity to examine body weight throughout childhood in non-obese children with psychiatric diagnoses. The major finding that adolescent depression and anxiety are associated with BMI percentile in a non-obese sample replicates previous work in obese samples [3, 6, 9, 10, 30, 31]. The results of this study add to the growing literature suggesting that psychiatric status is related to elevated BMI in childhood and adolescence. Our study found that children with emotional disorders have greater BMI percentiles than their non-clinical counterparts. This difference was maintained throughout the course of the study, indicating that the presence of anxiety and depression is associated with increases in the likelihood for elevated BMI. The results also indicate that there are gender differences in these relationships. Anxiety is associated with elevated BMIs in both boys and girls, although depression is related to elevated BMIs only for girls.
Adolescent girls and boys demonstrate differences on various psychosocial variables; these distinctions have been hypothesized to be linked to gender differences in adolescent emotional and physical development [32]. One difference that may distinguish female weight gain is the internal attitude toward weight and physical appearance [33]. Girls, especially those with MDD or anxiety, are more likely than boys to engage in dysfunctional thinking pertaining to body image, self-worth, and well-being [34]. Such thoughts may serve to discourage them from participating in physical activity or in seeing the value of making nutritious food choices [33], thus resulting in weight gain over time. Societal pressures may also differ for boys and girls, especially in terms of the stereotyped ideal of female thinness, which can lead to decreased body satisfaction and increased anxiety, depression, anger, and body dissatisfaction among females [35].
The relationship between BMI percentile and depression/anxiety could be due to several plausible mechanisms [10]. First, elevated depressive or anxious symptoms could exacerbate the likelihood of weight gain over time [3]. For example, depression or anxiety could affect diet or activity levels that could lead to elevations in sedentary behavior, increase in emotional eating, and decrease in exercise. Second, psychiatric medication use may affect weight directly or indirectly, as in practice of eating in the absence of hunger (i.e., an increase in reported psychological hunger) and may contribute to this complicated relationship [36]. Third, depression, anxiety, and weight could be influenced by additional social and biological risk factors. It is crucial to better understand the social pressures for thinness and consequential effects on mood. For instance, there may be different types of depression and anxiety among overweight children and adolescents that influence their eating behavior and physical activity levels. Additionally, preliminary data [4] provide evidence that hormonal factors, including adolescents’ menstrual cycles, may shed light on mood fluctuations. Such hypotheses warrant further investigation, which may offer future directions for prevention or treatment interventions.
These findings offer important clinical implications: upon identifying children with depression or an anxiety disorder, clinicians should recognize the increased risk of such patients to struggle with weight-related issues, possibly due to the various psychosocial and biological factors involved. Future investigations are needed to determine the most efficacious treatment protocol, including the effects on outcome measures of treating depression or weight first, versus providing simultaneous treatment for both issues. Additionally, it would be interesting to compare children with depression, anxiety, and controls who stay in the same BMI category (i.e., do not become obese) versus those who become obese. Furthermore, another area of future study is to examine the role of mood disturbances and emotion regulation as mediating factors for weight gain. Preliminary data [4] show that self-esteem and depression improve over time with weight loss preventions or interventions, thus it is possible that a broader cognitive behavioral approach may be fitting.
One limitation of this study is the inclusion criteria because these data were embedded within a larger study investigating the psychobiological underpinnings of mood disorders in children. Furthermore, this study is limited in its ability to draw conclusions about the causal effects of childhood emotional disorders upon adult BMI and is intended to provide information about the co-occurrence of childhood depression/anxiety and increased weight. As is the case with most longitudinal studies, participant drop-out can also be identified as a limitation.
These limitations notwithstanding, our data indicate the importance of addressing concurrent depressive/anxiety symptoms and overweight in childhood, as well as the need to track these issues longitudinally. It is crucial to understand the interplay of emotional disorders (primarily anxiety and depression) and weight gain from a behavioral, neurobiological, and physiological perspective for future studies. These data show that group differences begin to appear during childhood. The results also suggests that further study of the causal relationships between weight and mood/anxiety may lead to the development of more effective interventions to treat or prevent weight gain during childhood, a period of both developmental and behavioral plasticity. In providing a preventative program, it is possible and advantageous to teach children various physical and mental health strategies that can be engrained into lifestyle changes and utilized throughout their lifetime.
Summary
The present study examined the relationships between mood disorders and weight in children. Our results indicate that in comparison to controls, over the course our study, children who suffer from depression or anxiety are more likely to have increased BMI percentiles. The analyses also revealed gender differences in the relationships. While both girls and boys with anxiety have elevated BMI percentiles, girls with depression have elevated BMI percentiles, as well, whereas boys with depression follow the same weight trajectory as low-risk boys. These findings offer insight into the developmental relationships between emotional state and weight. Clinical implications suggested by these results include the importance of considering weight during psychotherapy interventions and of considering depressive and anxiety symptomatology during weight-related interventions. The results highlight the intricate connections between child mental and physical health.
Acknowledgments
The author would like to acknowledge the dedicated assistance of Stefanie Weiss, Psychology Research Fellow, University of Michigan, and Megan Barna, Guided Research Assistant, University of Pittsburgh. This research was supported by grant P01-MH41712 (Dr. Ryan) from the National Institute of Mental Health.
Contributor Information
Dana L. Rofey, Email: dana.rofey@chp.edu, Children’s Hospital of Pittsburgh, Weight Management & Wellness Center, University of Pittsburgh Medical Center, 3510 Fifth Avenue, Pittsburgh, PA 15213, USA, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Rachel P. Kolko, Email: kolkorp@upmc.edu, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Ana-Maria Iosif, Department of Public Health Sciences, Division of Biostatistics, University of California Davis, Davis, CA, USA.
Jennifer S. Silk, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
James E. Bost, Center for Research on Healthcare—Data Center, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Wentao Feng, Center for Research on Healthcare—Data Center, University of Pittsburgh Medical Center, Pittsburgh, PA, USA.
Eva M. Szigethy, Children’s Hospital of Pittsburgh, Weight Management & Wellness Center, University of Pittsburgh Medical Center, 3510 Fifth Avenue, Pittsburgh, PA 15213, USA. Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Robert B. Noll, Children’s Hospital of Pittsburgh, Weight Management & Wellness Center, University of Pittsburgh Medical Center, 3510 Fifth Avenue, Pittsburgh, PA 15213, USA
Neal D. Ryan, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Ronald E. Dahl, Children’s Hospital of Pittsburgh, Weight Management & Wellness Center, University of Pittsburgh Medical Center, 3510 Fifth Avenue, Pittsburgh, PA 15213, USA. Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
References
- 1.Institute of Medicine. Preventing childhood obesity. National Academy of Science; Washington, DC: 2004. [Google Scholar]
- 2.Center for Disease Control. Prevalence of overweight and obesity among adults. U.S. Department of Health and Human Services; Hyattsville: 2003. [Google Scholar]
- 3.Anderson SE, Cohen P, Naumova EN, Must A. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Arch Pediatr Adolesc Med. 2006;160:285–291. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- 4.Rofey DL, Szigethy E, Noll RB, Dahl RE, Iobst E, Arslanian SA. Cognitive-behavioral therapy for physical and emotional disturbances in adolescents with polycystic ovary syndrome: a pilot study. J Pediatr Psychol. 2009;34:156–163. doi: 10.1093/jpepsy/jsn057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faith MS, Allison DB, Geliebter A. Emotional eating and obesity: theoretical considerations and practical recommendations. In: Dalton S, editor. Obesity and weight control: the health professional’s guide to understanding and practice. Aspen; Gaithersburg: 1997. pp. 439–465. [Google Scholar]
- 6.Franko DL, Striegel-Moore RH, Thompson D, Schreiber GB, Daniels SR. Does adolescent depression predict obesity in black and white young adult women? Psychol Med. 2005;35:1505–1513. doi: 10.1017/S0033291705005386. [DOI] [PubMed] [Google Scholar]
- 7.Dahl RE. Adolescent brain development: a period of vulnerabilities and opportunities. Ann N Y Acad Sci. 2004;1021:1–22. doi: 10.1196/annals.1308.001. [DOI] [PubMed] [Google Scholar]
- 8.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol. 1993;102:133–144. doi: 10.1037/0021-843X.102.1.133. [DOI] [PubMed] [Google Scholar]
- 9.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 10.Pine DS, Goldstein RB, Wolk S, Weissman MM. The association between childhood depression and adulthood body mass index. Pediatrics. 2001;107:1049–1056. doi: 10.1542/peds.107.5.1049. [DOI] [PubMed] [Google Scholar]
- 11.Vila G, Zipper E, Dabbas M, Bertrand C, Robert JJ, Ricour C, Mouren-Simeoni MC. Mental disorders in obese children and adolescents. Psychosom Med. 2004;66:387–394. doi: 10.1097/01.psy. 0000126201.12813.eb. [DOI] [PubMed] [Google Scholar]
- 12.Pietrobelli A, Flodmark CE, Lissau I, Moreno LA, Widhalm K. From birth to adolescence: Vienna 2005 European childhood obesity group international workshop. Int J Obes. 2005;29:1–6. doi: 10.1038/sj.ijo.0803080. [DOI] [PubMed] [Google Scholar]
- 13.O’Dea JA, Wilson R. Socio-cognitive and nutritional factors associated with body mass index in children and adolescents: possibilities for childhood obesity prevention. Health Educ Res. 2006;21:796–805. doi: 10.1093/her/cyl125. [DOI] [PubMed] [Google Scholar]
- 14.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–257. doi: 10.2105/AJPH.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Istvan J, Zavela K, Weidner G. Body weight and psychological distress in NHANES I. Int J Obes Relat Metab Disord. 1992;16:999–1003. [PubMed] [Google Scholar]
- 16.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? results from the third national health and nutrition examination survey. Am J Epidemiol. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 17.White MA, O’Neil PM, Kolotkin RL, Byrne TK. Gender, race, and obesity-related quality of life at extreme levels of obesity. Obes Res. 2004;12:949–955. doi: 10.1038/oby.2004.116. [DOI] [PubMed] [Google Scholar]
- 18.Chiriboga DE, Ma Y, Li W, Olendzki BC, Pagoto SL, Merriam PA, Matthews CE, Herbert JR, Ockene IS. Gender differences in predictors of body weight and body weight change in healthy adults. Obesity (Silver Spring) 2008;16:137–145. doi: 10.1038/oby.2007.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, Reynolds JC, Yanovski JA. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117:1203–1209. doi: 10.1542/peds.2005–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barbe RP, Williamson DE, Bridge JA, Birmaher B, Dahl RE, Axelson DA, Ryan ND. Clinical differences between suicidal and non suicidal depressed children and adolescents. J Clin Psychiatry. 2005;66:492–498. doi: 10.4088/jcp.v66n0412. [DOI] [PubMed] [Google Scholar]
- 22.Williamson DE, Birmaher B, Axelson DA, Ryan ND, Dahl RE. First episode of depression in children at low and high familial risk for depression. J Am Acad Child Psychiatry. 2004;43:291–297. doi: 10.1097/00004583-200403000-00010. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3. American Psychiatric Association; Washington, DC: 1987. revised (DSM-III-R) [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. American Psychiatric Association; Washington, DC: 1994. (DSM-IV) [Google Scholar]
- 25.Birmaher B, Dahl RE, Williamson DE, Perel JM, Brent DA, Axelson DA, Kaufman J, Dorn LD, Stull S, Rao U, Ryan ND. Growth hormone secretion in children and adolescents at high risk for major depressive disorder. Arch Gen Psychiatry. 2000;57:867–872. doi: 10.1001/archpsyc.57.9.867. [DOI] [PubMed] [Google Scholar]
- 26.Hollingshead AF. Four factor index of social status. Yale University; New Haven: 1975. [Google Scholar]
- 27.Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Retrospective assessment of child psychopathology with the K-SADS-E. J Am Acad Child Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- 28.Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Arch Gen Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- 29.Kaufman J, Birmaher B, Brent D, Rao U. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL): initial reliability and validity data. J Am Acad Child Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 30.McElroy SL, Kotwal R, Malhotra S, Nelson EB, Keck PE, Nemeroff CB. Are mood disorders and obesity related? a review for the mental health professional. J Clin Psychiatry. 2004;65:634–651. doi: 10.4088/jcp.v65n0507. [DOI] [PubMed] [Google Scholar]
- 31.Pine DS, Cohen P, Brook J, Coplan JD. Psychiatric symptoms in adolescence as predictors of obesity in early adulthood: a longitudinal study. Am J Public Health. 1997;87:1303–1310. doi: 10.2105/AJPH.87.8.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCauley OC, Lerner RM, Lerner JV, Von EA. Does self-competence predict gender differences in adolescent depression and anxiety? J Adolesc. 1999;22:397–411. doi: 10.1006/jado.1999.0231. [DOI] [PubMed] [Google Scholar]
- 33.Dishman RK, Hales DP, Pfeiffer KA, Felton GA, Saunders R, Ward DS, Dowda M, Pate RR. Physical self-concept and self-esteem mediate cross-sectional relations of physical activity and sport participation with depression symptoms among adolescent girls. Health Psychol. 2006;25:396–407. doi: 10.1037/0278-6133.25.3.396. [DOI] [PubMed] [Google Scholar]
- 34.Hasnain M, Vieweg WV, Hettema JM, Colton D, Fernandez A, Pandurangi AK. The risk of overweight in children and adolescents with major mental illness. South Med J. 2008;101:367–372. doi: 10.1097/SMJ.0b013e3181683f8e. [DOI] [PubMed] [Google Scholar]
- 35.Cahill S, Mussap AJ. Emotional reactions following exposure to idealized bodies predict unhealthy body change attitudes and behaviors in women and men. J Psychosom Res. 2007;62:631–639. doi: 10.1016/j.jpsychores.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 36.Tanofsky-Kraff M, Theim KR, Yanovski SZ, Bassett AM, Burns NP, Ranzenhofer LM, Glasofer DR, Yanovski JA. Validation of the emotional eating scale adapted for use in children and adolescents (EES-C) Int J Eat Disord. 2007;40:232–240. doi: 10.1002/eat.20362. [DOI] [PMC free article] [PubMed] [Google Scholar]


