Abstract
Purpose
The purpose of this investigation was to use Leventhal’s Common Sense Model (CSM) to describe older breast cancer survivors’ symptom representations, symptom management strategies, and perceived barriers to symptom management.
Design
A secondary analysis was conducted using data from three pilot studies testing a theory-based intervention to improve symptom management in older breast cancer survivors.
Setting
Advanced practice nurses conducted open-ended interviews among older breast survivors either in the women’s home or via telephone.
Sample
The women were recruited from the community, an oncology clinic, and a state tumor registry. The women (n = 61, mean age = 69.5) were an average of 4.7 years post-breast cancer diagnosis and reported an average of 17 symptoms.
Methods
Content analysis was conducted of field notes taken during baseline interviews. Two coders independently coded responses. Inter-rater reliability was 82.3%.
Main Research Variables
Symptom representations, symptom management strategies, and perceived barriers to symptom management.
Findings
Women described their symptoms as chronic, with multiple causes (but rarely due to aging), with numerous negative consequences, and not curable or controllable. Women described an average of six symptom management strategies, most typically self-care. The most frequent barrier to symptom management was problems communicating with health care providers.
Conclusions
The CSM is a useful framework for understanding the symptom beliefs of older breast cancer survivors.
Implications for Nursing
Addressing women’s beliefs and barriers may result in better communication with health care providers and more effective interventions for symptom management.
Keywords: Breast Cancer, Coping, Geriatric Oncology, Quality of Life, Survivorship
Older women who have survived breast cancer (BC) commonly report multiple symptoms that may be due to normal age-related physiological changes, multiple comorbid health problems, or late effects of cancer and its treatment (Heidrich et al., in press; Heidrich, Egan, Hengudomsub, & Randolph, 2006) Unfortunately, these symptoms can interfere with daily functioning and reduce quality of life (Deimling, Sterns, Bowman, & Kahana, 2005; Deimling, Bowman, Sterns, Wagner, & Kahana, 2006; Keating, Norredam, Landrum, Huskamp, & Meara, 2005; Sherwood et al., 2005; Yancik et al., 2001). Older cancer survivors are faced with the tasks of interpreting the meaning of the symptom (Is this just aging or could this be a cancer recurrence?), deciding if and when to seek medical care for the symptom, and engaging in self-care practices to manage the symptom. However, little is known about how women accomplish this task when faced with the dual issues of breast cancer survivorship and aging.
Many symptoms experienced by older persons, such as fatigue and sleep problems, are perceived as “normal aging,” however, this perception is associated with a decreased likelihood of reporting the symptom, with less active engagement in self-care of symptoms, and with perceiving medical treatment as less beneficial (Dawson et al., 2005; Hofland, 1992; Maxwell, 2000; Miaskowski, 2000; Morgan, Pendleton, Clague & Horan 1997; Schroevers, Ranchor, & Sanderman, 2006). On the other hand, for cancer survivors, any symptom can lead to worry about whether or not to seek care for that symptom because of the ongoing concern about the possibility of a cancer recurrence (Clayton, Mishel, & Belyea, 2006). Thus, women’s beliefs about their symptoms can drive their choice of coping strategies, including their self-care of symptoms as well as seeking health care. Appropriate self-care and health care for symptoms is important for long-term health and well-being, thus, it is important to understand older women’s beliefs about their symptoms and how these beliefs drive their symptom management behaviors. Such knowledge could lead to better assessment and symptom management interventions on the part of health care providers when caring for older cancer survivors.
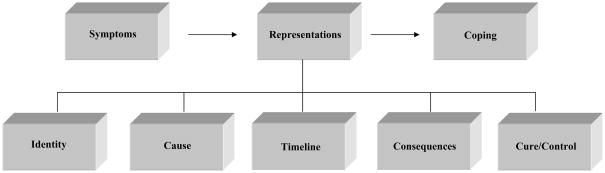
Leventhal’s Common Sense Model (CSM) (Leventhal & Dieffenbach, 1991; Leventhal, Meyer, & Nerenz, 1980) has been extensively used to understand “lay theories” of a variety of illnesses including asthma (Halm, More, & Leventhal, 2006), myocardial infarction (Cooper, Lloyd, Weinman, & Jackson, 1999; Lau-Walker, 2004) and sexually transmitted infections (Royer, 2008) just to name a few. According to the CSM, people have common sense beliefs or representations about their illness, and these representations guide coping behaviors. An illness representation is a set of beliefs – whether medically sound or not – that a person has about a symptom and consists of five dimensions: identity, cause, timeline, consequences, and cure/control (see Figure 1). Although not previously explored, it may be that women also have representations of their symptoms. For the purposes of exploring symptom representations (versus illness representations) the definitions of the five dimensions were slightly re-conceptualized from the original dimensions of the CSM. Identity refers to the attributes (e.g., quality, quantity) used to describe a symptom. Cause refers to an individual’s beliefs about the origin of the symptom. Timeline relates to temporal ideas, such as the acute, chronic, or cyclic nature of the symptom. Consequences are ideas about the short- and long-term outcomes of the symptom. Cure/control refers to beliefs about the extent to which one can control or cure the symptom.
Figure 1.
The Common Sense Model of Symptom Representations
In addition to identifying the dimensions of a representation, the CSM also posits that these representations drive how one copes with an illness. One way individuals cope is through behaviors (strategies) they employ to manage the impact of an illness (or symptoms). In addition, some representations may act as barriers to symptom management. For instance, the belief that a particular symptom is ‘caused’ by aging and therefore normal and not amenable to intervention could be a barrier to self-care or seeking treatment. There may be other barriers, other than representations, which may also interfere with symptom management. Because previous research has shown evidence of positive health behavior change when representations are targeted in interventions (Donovan & Ward, 2001; Donovan et al., 2007; Ward et al., 2008) identification of women’s symptom representations may lead to insight to improve symptom management among older breast cancer survivors. To date, few studies have systematically examined the symptom representations of older breast cancer survivors nor identified their specific symptom management strategies or barriers (Heidrich et al., 2006). Therefore, the purpose of this investigation was to describe older breast cancer survivors’ symptom representations, symptom management strategies, and perceived barriers to symptom management using the CSM as the guiding framework.
Method
Design
A secondary analysis was conducted of data collected from baseline interviews with older breast cancer survivors in three pilot studies testing a theory-based intervention to improve symptom management.
Sample
Eligibility criteria for the parent studies were: women aged 65 and over, community dwelling, English-speaking, a history of self-reported local or regional breast cancer, at least one year post BC diagnosis and three months post BC treatment (other than hormonal therapies). Age 65 was selected because that is the age typically used to define old age in research on health and aging.
Sixty-one women completed baseline intervention interviews (pilot study 1, n = 21; pilot study 2, n = 18; pilot study 3, n = 22). The mean age of this sample was 69.5 years (SD = 5.2, range = 65 – 86). Women were mostly Caucasian (95%), married (62%), generally well-educated (M =15 years), and of moderate income ($30K or greater). The women reported multiple health problems other than breast cancer (M = 4.8, range = 1 – 11) and experienced numerous symptoms (M = 17, range = 5 – 30) (see Table 1). The women were an average of 4.7 years post diagnosis of BC (range = 1 – 35). Past BC treatments included mastectomy (65%), lumpectomy (48%), chemotherapy (23%), radiation (51%), and hormonal therapies (35%).
Table 1.
Frequency and Percent of Health Problems and Symptoms among Women (N = 61)
| n* | %* | |
|---|---|---|
| Health Problems | ||
| Arthritis | 41 | 67 |
| Hypertension | 33 | 54 |
| Depression | 15 | 25 |
| Bronchitis/Emphysema | 13 | 21 |
| Osteoporosis | 8 | 13 |
| DM | 6 | 10 |
| Heart Trouble | 4 | 7 |
| Stroke | 1 | 2 |
| Symptoms | ||
| Stiffness | 51 | 84 |
| Joint Pain | 49 | 80 |
| Aching | 48 | 79 |
| Fatigue | 47 | 77 |
| Pain | 46 | 75 |
| Waking too Often | 41 | 67 |
| Dry Skin | 35 | 57 |
| Memory Problems | 34 | 56 |
| Weight Gain or Loss | 32 | 53 |
| Swelling in Hands and Feet | 29 | 48 |
| Difficulty Falling Asleep | 29 | 48 |
| Thinning Hair or Hair Loss | 29 | 48 |
| Depression | 28 | 46 |
| Balance Problem | 28 | 46 |
| Decreased Sex Drive | 28 | 46 |
| Shortness of Breath | 27 | 44 |
| Increased Urination | 27 | 44 |
| Hot Flashes | 27 | 44 |
| Incontinence | 26 | 43 |
| Numbness/Tingling in Hands, Arms or Legs | 26 | 43 |
| Waking too Early | 26 | 43 |
| Weakness | 25 | 41 |
| Irritated Eyes | 24 | 39 |
| Headaches | 24 | 39 |
| Trouble Concentrating | 22 | 36 |
| Itching | 21 | 34 |
| Vaginal Dryness | 20 | 33 |
| Nightmares or Disturbing Dreams | 19 | 31 |
| Feeling Anxious | 19 | 31 |
| Constipation | 18 | 30 |
| Thirst | 15 | 25 |
| Dizziness | 15 | 25 |
| Lymphedema | 15 | 25 |
| Vaginal Discharge | 15 | 25 |
Women could indicate more than one health problem or symptom hence the percentages are greater than 100%.
Measures
Self-report questionnaires were used to collect information regarding age, level of education, marital status, race/ethnicity, income level, breast cancer history, and comorbid health problems. A baseline symptom assessment was conducted using the Symptom Bother-Revised (SB-R) scale (Heidrich et al., 2006). The SB-R consists of 34 symptoms common to aging, age-related chronic conditions, and breast cancer and late effects of treatment. Respondents are asked if they have each symptom and how much they are bothered by it on a 0 (“don’t have”), 1 (“have, but not at all bothered”) to 5 (“extremely bothered”) scale. The SB-R scale has demonstrated reliability (alpha =.89) and validity (significant correlations with health problems and quality of life) in older adults with cancer (Heidrich et al., 2006). For the purposes of this study, the SB-R was used to describe the number of symptoms women experienced.
Procedure
In the original three studies, women were recruited from the community, oncology clinics, and state tumor registry and enrolled in a symptom management intervention study. Information about demographic, breast cancer and health history, and number and kinds of symptoms was collected using structured questionnaires at baseline. Open-ended interviews with advanced practice nurses (APNs) were conducted as part of the intervention (for details see Donovan et al., 2007). The interviews were conducted either in the women’s homes (n = 39) or via telephone (n = 22). The length of the interviews ranged from 48 to 180 minutes.
The interview was conducted to gather women’s representations of their symptom. The women were asked to identify a bothersome symptom (called the “target symptom”) and asked “what is this symptom like for you?” If needed, APNs used open-ended questions to prompt further discussion. Advanced practice nurses also asked women to describe what strategies they used to manage the symptom (both successful and unsuccessful). APNs used field notes to record the content of the baseline interviews.
All three studies received Institutional Review Board approval from the local Health Science Institutional Review Board.
Data Analysis
Field notes taken during baseline interviews were transcribed for coding purposes and entered into NVivo Edition 7. Content analysis was then performed using procedures described by Krippendorf (1980). The unit of measure was phrases from the field notes. Two coders independently coded phrases into seven pre-determined major categories: the five CSM dimensions (identity, cause, timeline, cure/control, consequences), symptom management strategies, and barriers to symptom management. Once categorized, the phrases were then coded into minor categories by the coders independently. Inter-rater reliability (percent agreement) for each major and minor category ranged from 64%–95%, according to the formula proposed by Krippendorf, (NA-NB)/Total where NA=number of agreement, NB = number of disagreement, Total = the total number of units (1980). Overall inter-rater reliability was 82.3%. Disagreements were resolved through discussion until consensus was reached.
Results
The mean number of symptoms per woman was 17.22 (SD = 6.92). The most frequently chosen target symptoms were pain (primarily musculoskeletal) (n = 15) and sleep disruption (n = 9).
Symptom Representations
Major and minor themes of symptom representations identified in the content analysis are shown in Table 2. For this study, the identity dimension was defined as attributes (e.g., quality, quantity) women used to describe their symptom. However, women did not spontaneously describe their symptom using such attributes. Thus the identity dimension did not appear to be present for these women.
Table 2.
Frequency and Percent of Women (N = 61) Who Described Their Symptom by each Category
| Major Category | n* | %* |
|---|---|---|
| Minor Category | ||
| Cause | ||
| Multiple Factors | 59 | 97 |
| Chronic or comorbid conditions | 41 | 67 |
| Cancer or cancer treatment | 21 | 34 |
| Aging | 5 | 8 |
| Timeline | ||
| Chronic | 35 | 57 |
| Cyclic | 7 | 11 |
| Acute | 6 | 10 |
| Cure/Control | ||
| Not curable | 17 | 28 |
| Not controllable | 21 | 34 |
| Controllable | 18 | 30 |
| Have to learn to live with it | 10 | 16 |
| Consequences | ||
| Negative impact on life | 60 | 98 |
| Limits physical activity | 38 | 62 |
| Negative effect on mental health | 32 | 52 |
| Negative effect on relationships | 21 | 34 |
| Constant need to be vigilant | 7 | 11 |
| Not limiting | 5 | 8 |
Women’s responses could be coded into more than one minor category; hence the percentages across categories are greater than 100%.
Cause was defined as beliefs about the origin of the symptom and what exacerbates a symptom. Nearly all of the women (n = 59, 97%) identified that their symptom was caused by multiple factors. For example, one participant identified that her constipation was the result of a number of causes: “I wonder if [my constipation] is due to Metamucil I’ve taken for years…[the] more bulk I eat the worse it gets…when I get anxious or nervous [I] get more constipated…[my doctor] said my colon is all corkscrewed around and it’s hard for things to move through…my metabolism is slow making me constipated…[I] don’t think it’s related to aging.”
Two-thirds (n = 41, 67%) stated that their symptom was caused by a chronic health problem other than cancer. For example, a woman had “been told it is osteoarthritis” causing her joint pain. Twenty-one (34%) participants believed that their symptom was related to either a cancer recurrence or a result of their prior cancer treatment. One woman believed that “radiation may have caused some of her [arm pain] too”. Only five women (8%) attributed their symptom to aging, “aging probably contributes [to my constipation].
The timeline dimension was defined as beliefs about the expected future course of the symptom; that is whether it is acute, chronic, or cyclical. A majority of the women (n = 35, 57%) identified that their symptom was chronic, “I see [my weight concern] as a long term chronic problem.” The remainder of the women believed that their symptom was either cyclic (n = 7, 11%), “[my abdominal cramping] comes and goes” or that the symptom was acute (n = 6, 10%). For example, one woman with difficulty sleeping explained that she “feel[s] [that] this is all temporary and I’ll be able to get back to normal.”
The cure/control dimension was defined as the belief about whether the symptom can or cannot be controlled or cured through medical treatment or one’s own behavior. More than a quarter of the women (n = 17, 28%) believed that their symptom was not curable; one woman stated, “[I] felt it will always be there.” A number of women (n = 10; 16%) believed that they will simply have to learn to live with the symptom. For instance, one woman told the APN, “I’ve given up and adjusted my life to less activity... [I] have to live with it.” In addition to the belief that their symptom is not curable, one third of the women indicated that they were not able to control their symptom (n = 21, 34%). One woman reported, I “don’t feel it’s very manageable.” On the other hand, thirty percent (n = 18) of the woman believed that they were able to control their symptom, “[I] can try to have it cause less disruption in my life.” Interestingly, perceptions of control or lack of control did not appear to be symptom-specific. That is, women reporting symptoms of fatigue, pain, urinary incontinence, and constipation were found in both groups.
The consequence dimension was defined as beliefs about the short- and long-term outcomes related to the symptom. Functional, psychological, and social consequences of the symptom were mentioned by the participants. Ninety-eight percent of the participants reported that the symptom that they were experiencing had negative consequences. Two-thirds of the women indicated that their symptom caused them to limit their physical activities (n = 38, 62%). For example, one woman explained that the pain she was experiencing “limits me in vacuuming, heavy lifting, [and] carrying.” Half of the women indicated that their symptom had a negative impact on their mental health (n = 32, 52%). One woman explained that joint stiffness results in feelings of “worthlessness.” One-third of the women indicated that the symptom had a negative effect on a personal relationship (n = 21, 34%). A participant told the APN that her relationship with her husband was strained because her knee discomfort “limits my husband and I doing things together.” A final consequence was the constant need to be vigilant (n = 7, 11%) in managing the symptom. For example, a women with a fear of falling said, “well, I really worry about falling, especially when I’m outside…I never was so worried before…I used to be able to get up if I fell, but not anymore and that is scary…[it] makes me afraid…I have to pay attention to the weather and sidewalk.”
Although 60 of the 61 women (98%) reported a negative consequence of their symptom, five women (8%) made a specific statement that the symptom had, “not much impact on most of my life.”
Symptom Management Strategies
Symptom management strategies were coded as either self-directed (i.e., self-care strategies) or health care provider directed (e.g., a medical treatment). Ninety percent of women (n = 55) identified strategies that were “self-directed.” For example, one woman discussed managing her fatigue by developing the ability to “prioritize and let things go.” Another woman with fatigue said she “takes a nap after lunch every day…and I cut down a bit on the really heavy work like hauling wood…I still do everything but I pace myself or do less at a time.”
Sixty-seven percent (n = 41) described symptom management strategies that were health care provider directed. One woman explained that to manage her joint pain she had been, “using pain pills…cortisone shots…the heart rehab program.”
On average, women reported using six strategies (M = 6.20, range= 1 – 15) to manage their symptom. A woman with sleep problems stated “[I] cut down on caffeine…from 7 PM on, [I] don’t drink much liquids to keep myself from having to get up for the bathroom during the night…I prioritize and pace myself to get done what I can…[I] do only what has to be done [until] I’m too tired to do more…an hour or so before bed I try to keep things quiet…[when I wake at night] I walk around the house…I pray the rosary…I lay down in the spare bedroom. I tried mild sleeping pills but did not renew the prescription.” Sixty-one percent (n = 37) of the women indicated that one or more of the strategies were unsuccessful. One participant said, “[I] have tried most things [the doctor] know[s] of” to manage her constipation without success.
Barriers to Symptom Management
Although not specifically elicited by the APN, six major barriers to symptom management were identified including: communication problems with the health care provider, medication concerns, symptom management too difficult, lack of resources, physical or psychological distress, and fear of diagnostic or surgical procedures (see Table 3).
Table 3.
Frequency and Percent of Women (N = 61) Who Described Barriers to Symptom Management
| Barrier | Major Category | Minor Category | ||
|---|---|---|---|---|
| n* | %* | n* | %* | |
| Communication with health care provider* | 23 | 38 | ||
| Concerns minimized by provider | 8 | 35 | ||
| Perceived symptom too minor to mention | 8 | 35 | ||
| Not adequate information | 6 | 26 | ||
| Differences with provider over management | 5 | 22 | ||
| Unsure of which provider to report symptom | 4 | 17 | ||
| Limited time with provider | 3 | 13 | ||
| Medication concerns | 19 | 31 | ||
| Symptom management too difficult | 16 | 26 | ||
| Lack of resources | 13 | 21 | ||
| Physical or psychological distress | 12 | 20 | ||
| Fear of diagnostic or surgical procedures | 7 | 11 | ||
Women’s responses could contain more than one barrier or minor category of barrier; hence the percentages across categories are greater than 100%.
The most common barrier to symptom management was communication problems with their health care provider (n = 23, 38%). Six minor categories of communication problems were identified: concerns minimized by provider, perceived symptoms too minor to mention, not adequate information, differences with provider over management, unsure of which provider to report symptom, and limited time with provider.
Eight women perceived that their concerns were minimized by the provider. One woman with lymphedema recalled her provider telling her, “I just have to live with it and I am lucky it’s not worse.” A number of women perceived that their symptom was to minor to mention to their provider (n = 8, 35%), a woman with constipation indicated that “[I am] not sure it’s really a problem major enough to tell [the] doctor.” Several women (n = 6, 26%) believed that they did not have adequate information regarding symptom management. One participant recalled mentioning her concern about knee pain to her provider yet, “[she received] no recommendation for exercise or physical therapy from the doctor.” Some women (n = 5, 22%) had difficulty communicating with their provider because they disagreed with their provider regarding the best way to manage their symptoms. A woman with weight concerns explained that she and her provider did not agree about the obesity medication recommended, “being on Cytomel helped so much, why shouldn’t I keep taking Cytomel?” Several women were unsure of which provider to report symptom to (n = 4, 17%). One women with knee pain mentioned that her doctor “was a sports medicine doctor and I think I need to see someone more attuned to dealing with older people with arthritis.” Another barrier was the perception that appointment times were limited and discussing the symptom would be a waste of valuable time (n = 3, 13%). For example, a participant reported “doctors are usually so busy and in a hurry and ready to rush out the door that it’s hard to ask all my questions and expect to get answers, especially regarding nutrition and exercise in regard to my colon problems.”
The second most common major barrier was concerns about medications (n = 19, 31%). This barrier included concerns about side effects, medications being ineffective, or fears related to taking medication. The following comments are reflective of these medication barriers: “[I] tried over-the-counter sleeping pills but it made my heart race and I never used it again,” “I’m on lots of medications for [shortness of breath] but sometimes the medications don’t work,” “usual arthritis meds are too dangerous, [they] scare me,” “[the provider] gave me a prescription but I haven’t filled it yet because I’m a bit worried about getting dependent or addicted to it.”
The third barrier was that women found the plan too challenging, unacceptable, or too difficult to integrate into a daily routine (n = 16, 26%). For example, one woman with lower abdominal cramping found that “drinking all that fluid is so difficult [it] puts me off from doing it.” A woman with constipation struggled with the plan being unacceptable for her because, “[I] hate drinking water…[I] have never been a water drinker and just can’t fit in the 8–10 glasses of water I understand is recommended.” When attempting to manage her weight concerns one woman stated, “[I have] tried things: [but] not much has really helped or been feasible to maintain.”
A fourth barrier was a lack of resources which included lack of social support, finances, or health care provider resources to manage a symptom (n = 13, 21%). One woman explained that to manage her symptom (fear of falling) she wanted to implement a walking program but she was “reluctant to walk outdoors without a friend and it’s not always possible to find someone who wants to go walking when I do.” To manage her urinary incontinence one participant needed to purchase incontinence pads but found the “pads expensive [which is] a big problem for me since [I am] on [a] limited income.” Others were unable to manage their symptom because of difficulty accessing health care providers, “I don’t see any specialists because it’s nearly impossible for me to get to where all the specialists are,” while another explained, “[the insurance company] wouldn’t pay…[they] would only pay every two years, not for a one year follow-up.”
In the fifth barrier, women described physical restrictions or psychological distress that interfered with symptom management (n = 12, 20%). For example, one woman explained that “because of problems with breathing I can’t exercise and do anything regarding my weight.” Another woman who was implementing a symptom management plan that included walks with friends became discouraged with this activity because she “doesn’t like to have to stop and say [to her friends that] I need rest.”
The final barrier to symptom management was fear of diagnostic or surgical procedures necessary to manage symptoms (n = 7, 11%). One woman reported that “because of past experience with [a] breast needle biopsy being inconclusive and having breast cancer, I am not reassured by a negative biopsy and ultrasound this time.” A woman in need of surgery reported, “I was so surprised and distraught about the mention of surgery, I didn’t hear or understand what [the surgeon] said about it.”
Discussion
The purpose of this investigation was to describe older breast cancer survivors’ symptom representations, symptom management strategies, and perceived barriers to symptom management using the Common Sense Model as the guiding framework. According to the CSM, people have common sense beliefs or representations about their health problems, and these representations guide coping behaviors. The beliefs can act as motivators to engage in self-care or treatment-seeking. On the other hand, these beliefs can act as barriers to effective coping. This investigation has established that women do have representations of their symptoms that are largely consistent with the dimensions of the CSM. Health care providers may be able to provide better care if they understand and take into account the representations (beliefs) that motivate or act as barriers to more effective symptom management strategies. Previous research provides evidence for the effectiveness of this approach to improve health outcomes in other patient populations (Donovan & Ward, 2001; Ward et al., 2008). Future research could utilize this approach in symptom management interventions.
The CSM has been useful in understanding patients’ beliefs about many health problems, including asthma (Halm, Mora, & Levanthal, 2006), HIV/AIDS (Keller, 1993), hypertension (Horne, Clatworthy, Polmear, & Weiman, 2001; Leventhal, Brissette, & Leventhal, 2003), myocardial infarction (Cooper, Lloyd, Weinman, & Jackson, 1999; Lau-Walker, 2004), sexually transmitted infections (Royer, 2008), and many others. In a recent meta-analytic review of empirical studies (n = 45) based on the CSM, Hagger and Orbell (2003) reported that the CSM dimensions of consequences, control/cure, identity, and timeline were supported across many different illness types. The results of this investigation largely provide support for the dimensions of the CSM as useful categories for describing women’s beliefs about their symptoms. The only dimension that was not consistent with the CSM was identity. Historically, the CSM defines identity as beliefs regarding the symptoms attached to an illness. Because in this investigation a symptom, rather than an illness, was being investigated, a modified definition was developed by the authors. Identity was defined as the attributes women used to describe their symptom. However, the participants did not spontaneously describe their symptom using such attributes. Thus the identity dimension did not appear to be salient for these women.
The most salient dimension of the CSM for these women was consequences; 98% of the women reported negative consequences of their symptom. Women’s descriptions of the negative consequences of their symptoms underscore the findings from previous research suggesting that symptoms have a major, negative impact on quality of life in older adults and in cancer survivors (Heidrich et al., 2006; Heidrich, Forsthoff, & Ward, 1994; Kurtz, Kurtz, Stommel, Given, & Given, 1999). The types of negative consequences women described were varied, including a broad negative impact on life in general as well as more specific consequences for physical activity, mental health, and relationships with others. In addition, for some women, the need to be vigilant about the management of their symptom was viewed as a negative consequence of having a symptom. These findings suggest the importance of developing new interventions to address and improve symptom management for older breast cancer survivors given the high prevalence of a negative impact on quality of life.
Almost all women believed that their symptoms were chronic. However, very few women attributed their symptoms to aging. This was contradictory to previous research wherein symptoms experienced by older persons were commonly perceived to be normal aging and thus little effort was made to resolve the symptom (Dawson et al., 2005; Hofland, 1992; Maxwell, 2000; Miaskowski, 2000; Morgan et al., 1997; Schroevers et al., 2006). Interestingly, most of the women attributed their symptom to multiple causes, which may explain why the women reported using, on average, six different strategies to manage their symptom. These findings suggest that a single strategy symptom management intervention for a patient will be less likely to ‘fix’ the problem. Consequently, managing symptoms believed to be due to a variety of causes may require ongoing communication with the health care provider, including addressing women’s beliefs and misconceptions about the cause of the symptom.
Women also described chronic or comorbid health problems and cancer or cancer treatment as the causes of their symptoms. This makes sense given that these women reported an average of 4.6 chronic health conditions, the most common being arthritis. Because most health problems in old age are both age-related and chronic, there is some overlap between beliefs about cause and beliefs about timeline. Furthermore, in old age, breast cancer is considered a chronic illness and is also age-related. It may be that, for older breast cancer survivors, the cause dimension is both salient and potentially more useful than, for instance, timeline for understanding how women understand and manage symptoms.
The cure/control dimension also reflects the chronic nature of most women’s symptoms. Almost all of the women stated that their symptoms were either not curable or not controllable. The belief that the symptoms were not curable is probably medically accurate for the majority of the symptoms these women reported. For example, the most frequently occurring target symptoms were musculosketal pain and sleep problems, both of which are age-related, chronic, and typically not ‘curable’. However, these symptoms, and many of the other symptoms the women experienced, can potentially be managed more effectively to lessen their impact on quality of life or prevent worsening of symptoms (i.e., are controllable). These results do suggest that older breast cancer survivors may have some misperceptions about the controllability of their symptoms. One implication of this is that asking women about their symptoms and about their beliefs about cause, timeline, and cure/control may provide health care providers with information they can use to provide better symptom management.
The CSM would suggest that beliefs that symptoms are not curable or controllable would result in not seeking treatment or engaging in self-care behaviors. This study could not address that question directly. However, in spite of these beliefs, almost all of the women described engaging in self-care behaviors (albeit often unsuccessfully) to manage their symptoms. Over half of the women also used medical treatments to manage their symptoms. Thus, these women seemed to be motivated to engage in behaviors to lessen the impact of the symptoms on their lives, but their efforts were not very successful. We could not ascertain from this study whether the symptom management strategies used were appropriate or why many strategies were not successful. However, it is clear that these women did continue to try to manage their symptoms in spite of beliefs that would suggest that they would not do so (e.g., that symptoms are chronic and not controllable).
On the other hand, the barriers to symptom management described by these women provide some insight into why they have difficulty in managing symptoms. The most frequently mentioned barrier was communication problems with health care providers. This category included numerous issues such as not having enough time, concerns about symptoms being minimized by the provider, perception that the symptom was too minor to mention, and not getting enough information from providers. Some of these barriers may reflect age-related stereotypes on the part of health care providers. Previous research suggests that health care providers often perceive that older adults are unwilling to try new treatments or that, due to their age, intervention would not be effective (Kane, 2006; Knobf, 2007; Lovell, 2006; Miaskowski, 2000; Ory, Hoffman, Hawkins, Scanner, & Mockenhaupt, 2003). Unfortunately, older adults report that their health care providers communicate these negative attitudes to them (Miaskowski, 2000; Ory et al., 2003). The two most common communication barriers were the belief that concerns were minimized by the provider and the perception that the symptom was too minor to mention to the provider. Although not examined, there may be a relationship between these barriers. Women may feel that the symptom is too minor to mention because they have experienced a provider minimizing their concerns in the past. Some of these barriers have also been identified in research on symptom management in cancer patients (Avis, Crawford, & Manuel, 2005) and in older adults (Miaskowski, 2000; Morgan et al., 1997). For instance, both may think that discussing symptoms may detract from more important topics (Avis et al., 2005), distract the physician from more essential care (Miaskowski, 2000), or result in being labeled a problem patient (Hofland, 1992; Maly, Leake, & Silliman, 2004; Maxwell, 2000; Miaskowski, 2000). For cancer survivors, these communication barriers may not only detract from better symptom management but prevent health care providers from addressing patients’ ongoing worry that symptoms may mean a cancer recurrence.
Addressing barriers to symptom management may be necessary in order to provide patient-centered care (Lauver et al., 2002); that is, care that takes into account patient preferences and values. If a patient does not agree with the symptom management strategies proposed by the provider, but these differences and preferences are not communicated, effective care will not take place. If patients’ preferences or goals were clearly communicated and discussed, many of the barriers mentioned by women in this study might not exist.
Limitations
This study was a secondary analysis of interviews conducted during three pilot studies, and the content analysis was based on field notes rather than verbatim interviews. The sample lacked ethnic and racial diversity, although the sample was diverse in terms of socioeconomic status and health status. The women in this study were volunteers in a study aimed at testing an intervention for symptom management and thus could be considered to be highly motivated to address their symptoms. Thus, there may be a selection bias that should be taken into account when considering these results. Finally, the reliability calculation (percent agreement) may overestimate agreement because it does not take into account chance agreement.
Conclusion
The findings from this study suggest that the CSM is a useful framework for identifying and describing older breast cancer survivors’ beliefs about symptoms and symptom management. Specifically addressing women’s beliefs and barriers may result in better communication with health care providers and more effective interventions for symptom management.
Key Points.
The Common Sense Model is a useful framework for identifying and describing women's beliefs about symptoms and symptom management.
In spite of the fact that most women perceived their symptom as not curable or controllable, almost all of the women engaged in self-care behaviors to manage their symptom.
Women perceived their symptoms to be caused by multiple factors and used multiple strategies to manage their symptoms.
Communication problems with provider was the most common barrier to symptom management.
Acknowledgments
This research was supported in part by the Helen Denne Schulte fund, School of Nursing, University of Wisconsin-Madison (Dr. Phelan) and by NIH R55 NR07741-01, P20 CA103697, P20NR008987, and a University of Wisconsin-Madison School of Nursing Research Committee Award (Dr. Heidrich).
Contributor Information
Heather Rhea Royer, Email: hroyer@wisc.edu, Center for Patient-Centered Interventions, School of Nursing, University of Wisconsin - Madison, Clinical Science Center – K6/374, 600 Highland Ave, Madison, WI 53792, Phone: (608) 263-9040, Fax: (608) 263-5458.
Cynthia H. Phelan, Email: phelanhcc@tznet.com, William S. Middleton Veteran’s Hospital, 2500 Overlook Terrace, Madison, WI 53705, Phone (608) 256-1901 ext 11683, Fax (608) 280-7291.
Susan M. Heidrich, Email: smheidrich@wisc.edu, School of Nursing University of Wisconsin - Madison, Box 2455 Clinical Science Center - K6/362 600, Highland Ave, Madison, WI 53792, Phone (608) 263-5191, Fax: (608) 263-5458.
References
- Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. Journal of Clinical Oncology. 2005;23(15):3322–3330. doi: 10.1200/JCO.2005.05.130. [DOI] [PubMed] [Google Scholar]
- Clayton MF, Mishel MH, Belyea M. Testing a model of symptoms, communication, uncertainty, and well-being, in older breast cancer survivors. Research in Nursing & Health. 2006;29(1):18–39. doi: 10.1002/nur.20108. [DOI] [PubMed] [Google Scholar]
- Cooper A, Lloyd G, Weinman J, Jackson G. Why patients do not attend cardiac rehabilitation: Role of intentions and illness beliefs. Heart. 1999;82(2):234–236. doi: 10.1136/hrt.82.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson R, Sellers DE, Spross JA, Jablonski ES, Hoyer DR, Solomon MZ. Do patients' beliefs act as barriers to effective pain management behaviors and outcomes in patients with cancer-related or noncancer-related pain? Oncology of Nursing Forum. 2005;32(2):363–374. doi: 10.1188/05.ONF.363-374. [DOI] [PubMed] [Google Scholar]
- Deimling GT, Bowman KF, Sterns S, Wagner LJ, Kahana B. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psycho-Oncology. 2006;15(4):306–320. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- Deimling GT, Sterns S, Bowman KF, Kahana B. The health of older-adult, long-term cancer survivors. Cancer Nursing. 2005;28(6):415–424. doi: 10.1097/00002820-200511000-00002. [DOI] [PubMed] [Google Scholar]
- Donovan H, Ward S. A representational approach to patient education. Journal of Nursing Scholarship. 2001;33:221–216. doi: 10.1111/j.1547-5069.2001.00211.x. [DOI] [PubMed] [Google Scholar]
- Donovan HS, Ward SE, Song MK, Heidrich SM, Gunnarsdorrir S, Phillips CM. An update on the representational approach to patient education. Journal of Nursing Scholarship. 2007;39(3):259–265. doi: 10.1111/j.1547-5069.2007.00178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halm EA, Mora P, Leventhal H. No symptoms, no asthma: The acute episodic disease belief is associated with poor self-management among inner-city adults with persistent asthma. Chest. 2006;129(3):573–580. doi: 10.1378/chest.129.3.573. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychology and Health. 2003;18(2):141–184. [Google Scholar]
- Heidrich SM, Brown RL, Egan JJ, Perez OA, Phelan CH, Yeom H, et al. An individualized representational intervention to improve symptom management in older breast cancer survivors: Three pilot studies. Oncology Nursing Forum. doi: 10.1188/09.ONF.E133-E143. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidrich SM, Egan JJ, Hengudomsub P, Randolph SM. Symptoms, symptom beliefs, and quality of life of older breast cancer survivors: A comparative study. Oncology Nursing Forum. 2006;33(2):315–322. doi: 10.1188/06.ONF.315-322. [DOI] [PubMed] [Google Scholar]
- Heidrich SM, Forsthoff CA, Ward SE. Adjustment to cancer: The self as mediator. Health Psychology. 1994;13(4):346–353. doi: 10.1037//0278-6133.13.4.346. [DOI] [PubMed] [Google Scholar]
- Hofland SL. Elder beliefs: blocks to pain management. Journal of Gerontological Nursing. 1992;18(6):19–23. doi: 10.3928/0098-9134-19920601-05. [DOI] [PubMed] [Google Scholar]
- Horne R, Clatworthy J, Polmear A, Weinman J. Do hypertensive patients' beliefs about their illness and treatment influence medication adherence and quality of life? Journal of Human Hypertension. 2001;15(Supplement 1):S65–S68. doi: 10.1038/sj.jhh.1001081. [DOI] [PubMed] [Google Scholar]
- Kane MN. Social work students' perceptions about incompetence in elders. Journal of Gerontological Social Work. 2006;47(3–4):153–171. doi: 10.1300/J083v47n03_10. [DOI] [PubMed] [Google Scholar]
- Keating NL, Norredam M, Landrum MB, Huskamp HA, Meara E. Physical and mental health status of older long-term cancer survivors. Journal of the American Geriatrics Society. 2005;53(12):2145–2152. doi: 10.1111/j.1532-5415.2005.00507.x. [DOI] [PubMed] [Google Scholar]
- Keller M. Why don’t young people protect themselves against sexual transmission of HIV? Possible answers to a complex question. AIDS Education and Prevention. 1993;5(3):220–233. [PubMed] [Google Scholar]
- Knobf MT. Psychosocial responses in breast cancer survivors. Seminars in Oncology Nursing. 2007;23(1):71–83. doi: 10.1016/j.soncn.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Krippendorf K. Content analysis. Thousand Oaks: Sage Publications; 1980. [Google Scholar]
- Kurtz ME, Kurtz JC, Stommel M, Given CW, Given B. The influence of symptoms, age, comorbidity and cancer site on physical functioning and mental health of geriatric women patients. Women & Health. 1999;29(3):1–12. doi: 10.1300/J013v29n03_01. [DOI] [PubMed] [Google Scholar]
- Lauver D, Ward SE, Heidrich SM, Keller ML, Bowers BJ, Brennan PF, et al. Patient-centered interventions. Research in Nursing and Health. 2002;25:246–255. doi: 10.1002/nur.10044. [DOI] [PubMed] [Google Scholar]
- Lau-Walker M. Relationship between illness representation and self-efficacy. Journal of Advanced Nursing. 2004;48(3):216–225. doi: 10.1111/j.1365-2648.2004.03190.x. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Diefenbach M. The active side of illness cognition. In: Skelton J, Croyle R, editors. Mental representation in health and illness. New York: Springer-Verlag; 1991. pp. 247–272. [Google Scholar]
- Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. In: Rachman S, editor. Contributions to medical psychology. 2 . Oxford: Pergamon Press; 1980. pp. 7–30. [Google Scholar]
- Leventhal H, Brissette I, Leventhal EA. The Common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behavior. Londonm UK: Routledge; 2003. pp. 42–65. [Google Scholar]
- Lovell M. Caring for the elderly: Changing perceptions and attitudes. Journal of Vascular Nursing. 2006;24(1):22–26. doi: 10.1016/j.jvn.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Maly RC, Leake B, Silliman RA. Breast cancer treatment in older women: impact of the patient-physician interaction. Journal of American Geriatrics Society. 2004;52(7):1138–1145. doi: 10.1111/j.1532-5415.2004.52312.x. [DOI] [PubMed] [Google Scholar]
- Maxwell T. Cancer pain management in the elderly. Geriatric Nursing. 2000;21(3):158–163. doi: 10.1067/mgn.2000.108267. [DOI] [PubMed] [Google Scholar]
- Miaskowski C. The impact of age on a patient's perception of pain and ways it can be managed. Pain Management Nursing. 2000;1(3 Supplement):2–7. doi: 10.1053/jpmn.2000.9760. [DOI] [PubMed] [Google Scholar]
- Morgan R, Pendleton N, Clague JE, Horan MA. Older people's perceptions about symptoms. British Journal of General Practice. 1997;47(420):427–430. [PMC free article] [PubMed] [Google Scholar]
- Ory M, Hoffman MK, Hawkins M, Scanner B, Mockenhaupt R. Challenging aging stereotypes: Strategies for creating a more active society. American Journal of Preventive Medicine. 2003;25(3, Supplement 2):164–171. doi: 10.1016/s0749-3797(03)00181-8. [DOI] [PubMed] [Google Scholar]
- Royer HR. Doctoral dissertation. University of Wisconsin-Madison; 2008. Young women’s representations of sexually transmitted infections and sexually transmitted infection testing. [Google Scholar]
- Sherwood P, Given BA, Given CW, Champion VL, Doorenbos AZ, Azzouz F. A cognitive behavioral intervention for symptom management in patients with advanced cancer. Oncology Nursing Forum. 2005;32(6):1190–1198. doi: 10.1188/05.ONF.1190-1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroevers M, Ranchor AV, Sanderman R. Adjustment to cancer in the 8 years following diagnosis: A longitudinal study comparing cancer survivors with healthy individuals. Social Science & Medicine. 2006;63(3):598–610. doi: 10.1016/j.socscimed.2006.02.008. [DOI] [PubMed] [Google Scholar]
- Ward S, Donovan H, Gunnarsdottir S, Serlin RC, Shapiro G, Hughes S. A randomized trial of a representational intervention to decrease cancer pain (RIDcancerPain) Health Psychology. 2008;27(1):59–67. doi: 10.1037/0278-6133.27.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancik R, Wesley MN, Ries LA, Havlik RJ, Edwards BK, Yates JW. Effect of age and comorbidity in postmenopausal breast cancer patients aged 55 years and older. Journal of the American Medical Association. 2001;285(7):885–892. doi: 10.1001/jama.285.7.885. [DOI] [PubMed] [Google Scholar]