Abstract
Background:
Hallux rigidus is a common problem characterized by localized osteoarthritis and limited range of motion of the hallux. First metatarsophalangeal joint arthrodesis has been the accepted procedure for the treatment of late-stage disease. Despite the success of arthrodesis, some patients object to the notion of eliminating motion at the metatarsophalangeal joint. For this reason, motion-sparing procedures such as the modified oblique Keller capsular interpositional arthroplasty have been developed.
Methods:
We compared a cohort of ten patients (ten toes) who had undergone the modified Keller arthroplasty with a group of twelve patients (twelve toes) who had undergone a first metatarsophalangeal joint arthrodesis at an average of sixty-three and sixty-eight months, respectively. Clinical outcomes were evaluated, and range of motion, great toe dynamometer strength, plantar pressures, and radiographs were assessed.
Results:
Clinical outcome differences existed between the groups, with the American Orthopaedic Foot and Ankle Society score being significantly higher for the arthroplasty group than for the arthrodesis group. The arthroplasty group had a mean of 54° of passive and 30° of active range of motion of the first metatarsophalangeal joint. The plantar pressure data revealed significantly higher pressures in the arthrodesis group under the great toe but not under the second metatarsal head.
Conclusions:
The modified oblique Keller capsular interpositional arthroplasty appears to be a motion-sparing procedure with clinical outcomes equivalent to those of arthrodesis, and it is associated with a more normal pattern of plantar pressures during walking.
Level of Evidence:
Therapeutic Level III. See Instructions to Authors for a complete description of levels of evidence.
Hallux rigidus is a common condition characterized by first metatarsophalangeal joint pain and limited hallux range of motion due to localized osteoarthritis of that joint. Patients who have had a failure of nonoperative treatment have several operative procedures available. Dorsal metatarsophalangeal joint cheilectomy has been recommended when there is mild to moderate joint damage and pain only at the end of the range of motion. Arthrodesis, implant arthroplasty, or interpositional/resection arthroplasty are options in cases in which the joint is not salvageable and there is pain throughout the range of motion. Each option offers specific advantages and disadvantages. Arthrodesis is associated with malunion, nonunion, shortening, and transfer metatarsalgia1. It eliminates motion and pain in most patients, but the concept of eliminating motion at the first metatarsophalangeal joint is not easily accepted by many patients. Implant arthroplasty with silicone or high-density polyethylene/metal composites is associated with stiffness, wear debris-related synovitis, and high failure rates2,3. The Keller resection arthroplasty maintains some metatarsophalangeal joint motion. It initially was described for the correction of a hallux valgus deformity4 with resection of a substantial portion (as much as one-third) of the proximal portion of the proximal phalanx and was associated with a high rate of complications, including lateral transfer metatarsalgia, decreased great toe strength, excessive shortening of the first ray, great toe cock-up deformity, and clawing of the interphalangeal joint5,6. Modified versions of the resection arthroplasty have been introduced for the treatment of hallux rigidus in an attempt to reduce these complications, to maintain hallux metatarsophalangeal joint range of motion, and to provide more predictable pain relief. Hamilton et al.7 modified the Keller procedure to reduce the amount of the proximal phalanx that is removed (only the proximal one-fourth) and interposed the dorsal metatarsophalangeal joint capsule into the joint to act as a soft-tissue spacer between the ends of the bone in the decompressed metatarsophalangeal joint space. Mroczek and Miller8 further modified Hamilton's procedure by changing the obliquity of the proximal phalangeal bone resection to retain the plantar base of the proximal phalanx and thereby change the sesamoid ligament insertion. The modified oblique Keller capsular interpositional arthroplasty is a motion-preserving procedure that is appealing to younger or more active patients, those with adjacent arthritis, and those who do not desire a fusion. The purpose of the present study was to determine whether this arthroplasty is an effective procedure for relieving pain and for maintaining range of motion and hallux strength and whether it results in a more normal plantar pressure distribution in comparison with a hallux metatarsophalangeal arthrodesis in a similar group of patients.
Materials and Methods
Patient Selection
We conducted an institutional review board-approved retrospective review of patients who had been managed with a modified oblique Keller capsular interpositional arthroplasty for the treatment of hallux rigidus from 1999 to 2005 by a single surgeon (J.E.J.). All patients had had a failure of nonoperative measures such as orthotics and turf toe plates, activity modification, anti-inflammatory medications, and injections of corticosteroids. Patients were identified by means of a search of our surgical database. From 1999 to February 2005, nineteen such arthroplasties (including three bilateral procedures) were identified. Ten patients were willing to return for a clinical evaluation after a mean duration of follow-up of sixty-three months (range, twenty-three to 101 months). Five of the patients were male, and five were female. Three patients had had a bilateral procedure. Our final statistical evaluation excluded the results for one of the sides in the patients who had undergone a bilateral procedure because bilateral procedures could not be considered to be independent. One patient had had both procedures done the same day, another patient had had the two procedures fifty-four months apart, and the third patient had had the two procedures two months apart. For the purposes of statistical computation, we excluded the second procedure in the latter two patients and randomly excluded the right side in the patient who had had both sides done on the same day. One patient underwent a right-sided modified Keller capsular interpositional arthroplasty and, on the same day, a left-sided dorsal cheilectomy and proximal phalangeal osteotomy for the correction of hallux valgus interphalangeus. During our inclusion time frame, more of the arthroplasty procedures were performed in the latter years because the procedure was relatively new in our practice. The procedure was performed for a select group of patients: those with end-stage hallux rigidus who desired a motion-preserving procedure and who otherwise would have undergone an arthrodesis.
The arthrodesis comparison group was obtained by means of a search of our surgical database. During the inclusion period from 1999 to 2005, a total of seventy-six first metatarsophalangeal joint arthrodeses were performed by the senior author (J.E.J.), of which thirty-four met the inclusion criteria for the purposes of comparison with the arthroplasty group. The inclusion criterion for the arthrodesis group was painful osteoarthritis of the first metatarsophalangeal joint, with or without a hallux valgus deformity. The exclusion criteria for the arthrodesis group were a history of infection, neuropathy, inflammatory arthritis, and neuromuscular disease. Of the twenty-nine patients (thirty-four feet) who were identified, twelve patients (twelve feet), including six male patients and six female patients, were willing to return for an evaluation. Of the twelve feet in this group, seven had been treated for hallux rigidus and five had been treated for painful hallux valgus with secondary degenerative changes. One of the patients with hallux valgus had previously received a silicone implant and underwent a salvage arthrodesis. In this group, the average time after surgery was sixty-eight months (range, twenty-seven to ninety-six months).
Operative Technique
A dorsal medial longitudinal incision over the first metatarsophalangeal joint was utilized. The dorsal cutaneous nerve of the great toe was retracted laterally. A medial longitudinal capsulotomy provided access to the joint and then subperiosteal dissection was carried out over the dorsal aspect of the first metatarsal head. With use of a sagittal saw, the dorsal one-third of the metatarsal head with any associated osteophytes was removed (Fig. 1). The dorsal capsule and the short extensor tendon to the great toe were removed from their attachments along the dorsal ridge of the base of the proximal phalanx. An oblique osteotomy from medial to lateral was used to remove a wedge-shaped portion of the base of the proximal phalanx, with more bone being removed dorsally in order to preserve the insertion of the short flexors on the plantar aspect of the base of the proximal phalanx. Intraoperative motion was evaluated to ensure at least 80° of dorsiflexion relative to the first metatarsal shaft. The dorsal capsule was then advanced over the metatarsal head and was sutured into the plantar plate with absorbable sutures in an interrupted fashion (Figs. 2 and 3). An extensor hallucis brevis tenotomy was performed to allow complete excursion of the dorsal capsule over the metatarsal head deep into the space (Fig. 4). Imbrication of the medial capsule was carried out with absorbable sutures to hold the toe in a corrected position. This technique requires manual distraction of the joint and the use of a small curved needle to place the intracapsular suture. Intraoperative fluoroscopy was used to determine the degree of osseous resection as well as to assess alignment (Figs. 5-A and 5-B). Figure 6 graphically depicts the extent of osseous decompression and preservation of the insertion of the short toe flexors on the base of the proximal phalanx, the extensor hallucis brevis tenotomy, and the placement of the dorsal capsule into the space created.
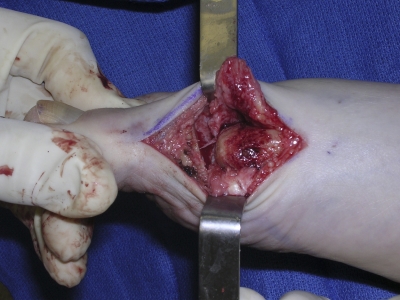
Fig. 1.
Bone resection is performed to decompress the first metatarsophalangeal joint. Care is taken to avoid excessive dorsal resection, which may destabilize the metatarsophalangeal joint.
Fig. 2.
The dorsal capsule has been dissected away from the metatarsophalangeal joint.
Fig. 3.
The dorsal capsule is draped over the first metatarsal head and is interposed between the joint surfaces.
Fig. 4.
The dorsal capsule has been sutured to the plantar plate, and the medial capsule has been repaired. Note that the tendon of the extensor hallucis brevis has been released proximally to allow full distal excursion of the capsule to provide full coverage over the metatarsal head.
Fig. 5-A Fig. 5-B.
Intraoperative anteroposterior (Fig. 5-A) and lateral (Fig. 5-B) radiographs demons-trating the extent and obliquity of the ostectomy of the base of the phalanx and the metatarsal head.
Fig. 6.
A: This drawing depicts the amount of osseous resection while the insertion of the short flexors on the base of the proximal phalanx is preserved. B: This drawing depicts the extensor hallucis brevis tenotomy and excursion of the dorsal capsule into the joint. (Reprinted, with permission, from: Mroczek KJ, Miller SD. The modified oblique Keller procedure: a technique for dorsal approach interposition arthroplasty sparing the flexor tendons. Foot Ankle Int. 2003;24:522.)
Clinical Assessment
Clinical outcome analysis was done in a similar fashion for both groups. All patients returned for weight-bearing anteroposterior, oblique, and lateral radiographs, and all completed the Foot and Ankle Ability Measure (FAAM). The American Orthopaedic Foot and Ankle Society (AOFAS) clinical rating system for the hallux was administered independently by one of us (O.K.). The FAAM consists of twenty-one items on activities of daily living and an eight-item sports subscale9. The AOFAS clinical rating system for the hallux evaluates function, pain, and alignment10. This system provides a score ranging from 0 to 100 points, which takes into consideration both subjective and objective elements of pain (maximum score, 40 points), functional capacity (maximum score, 45 points), and hallux alignment (maximum score, 15 points).
Plantar Pressure Analysis
All subjects had a dynamic plantar force and pressure distribution assessment while walking barefoot at their preferred, self-selected walking speed with use of an EMED-ST P-2 pressure platform (Novel Electronics, St. Paul, Minnesota). The two-step method of data collection was used for all trials as previously described by Meyers-Rice et al.11. Each patient performed three walking trials, while barefoot or while wearing socks, over a raised walkway, with the pressure platform embedded flush with the walkway surface. The walkway had a length of 7 m. Pressure was recorded in N/cm2, and the mean peak pressure of the three trials was calculated. Walking speed was recorded with a digital stopwatch.
Range-of-Motion Evaluation
Range-of-motion measurements were performed in a standardized fashion with use of a goniometer by a single independent observer (O.K.). Passive and active range-of-motion data were gathered for the metatarsophalangeal joint, the interphalangeal joint, and the ankle joint. The point of reference was neutral alignment of the non-weight-bearing foot.
Strength Testing
Toe flexion muscle strength was measured by a single independent observer (O.K.) with use of a digital dynamometer (Chatillon MSC-100; AMETEK, Largo, Florida) mounted vertically on a stable wood board. A thin (1.5-cm-wide) leather cuff was connected to the hook attachment of the dynamometer and was placed around the distal aspect of the great toe. Toe flexor muscle strength was measured with the patient in the sitting position, with the knee at 90° of flexion and the ankle in a neutral position (0° of dorsiflexion and plantar flexion). After the participant became familiar with the test, three trials were performed and the mean of the three trials was used.
Statistical Evaluation
Independent t tests were performed to determine differences between the two groups in terms of the passive and active range of motion of the first metatarsophalangeal and interphalangeal joints, first toe plantar flexor strength, plantar pressure, the AOFAS score, and the FAAM score. The Levene test was used to determine equality of variances. The level of significance was set at p < 0.05.
Source of Funding
This project was funded by the Midwest Stone Institute, a nonprofit organization that did not participate in this investigation. Funding was used to pay for patient expenses, radiographs, pedobarographic analysis, and materials.
Results
The results were evaluated in ten patients (ten great toes) at a mean of sixty-three months (range, twenty-three to 101 months) after the modified Keller arthroplasty and in twelve patients (twelve toes) at a mean of sixty-eight months (range, twenty-seven to ninety-six months) after arthrodesis.
At the time of testing, the average age was sixty-four years (range, fifty-eight to eighty years) for the patients in the arthroplasty group and fifty-nine years (range, forty-six to sixty-eight years) for those in the arthrodesis group. The self-reported average weight was 84 kg for the patients in the arthroplasty group as well as for those in the arthrodesis group. The average body mass index (based on self-reported weight and height at the time of the latest evaluation) was 28 kg/m2 in the arthroplasty group and 27 kg/m2 in the arthrodesis group.
The total AOFAS scores were higher for the arthroplasty group than for the arthrodesis group. We could identify no significant difference between the two groups in terms of the FAAM measures (Table I).
TABLE I.
Clinical Outcomes Results
| Arthroplasty* | Arthrodesis* | P Value | |
| American Orthopaedic Foot and Ankle Society score for the hallux†(points) | 89.55 | 64.48 | 0.006 |
| Foot and Ankle Ability Measure | |||
| Total percent ADL‡(% of maximum possible score) | 92.18 | 84.58 | 0.223 |
| Total percent sport (% of maximum possible score) | 87.5 | 71.35 | 0.135 |
The values are given as the mean.
Maximum possible score, 100 points.
ADL = activities of daily living.
Peak plantar pressures under the great toe during walking were considerably lower in the arthroplasty group as compared with the arthrodesis group (33 compared with 67 N/cm2; p = 0.007). There were no differences between the two groups with respect to the plantar pressures beneath the second and third metatarsal heads (see Appendix).
The active and passive ranges of motion of the ipsilateral ankle joint were not significantly different between the groups (see Appendix). The active and passive ranges of motion of the great toe interphalangeal joint were significantly greater in the arthrodesis group. In the arthroplasty group, the active and passive ranges of motion of the first metatarsophalangeal joint averaged 30° and 54°, respectively. The groups were not significantly different with regard to toe flexor muscle strength as measured at the distal phalanx (9.3 kg compared with 10.79 kg; p = 0.393).
Radiographic Results
In the arthrodesis group, the average postoperative alignment was 12° (range, 2° to 23°) of valgus on the standing anteroposterior radiograph and 14° (range, 0° to 24°) of dorsiflexion on the standing lateral radiograph. There was one nonunion and interphalangeal joint arthritis in another patient. In the arthroplasty group, the average postoperative alignment was 8° (range, 1° to 18°) of valgus on the standing anteroposterior radiograph and 16° (range, 10° to 24°) of dorsiflexion on the standing lateral radiograph.
Power Analysis
A post hoc power analysis indicated that there was not sufficient power in our study to determine whether there truly was a difference between the two groups with regard to the FAAM activities-of-daily-living or sports subscores or the second metatarsal head pressures.
Discussion
The optimal treatment of moderate to severe hallux rigidus remains controversial; arthrodesis or some form of arthroplasty are the two procedures that are usually recommended.
Arthrodesis is often utilized for the treatment of advanced hallux rigidus, especially when deformity is present, and it remains the gold standard for the operative treatment of late-stage hallux rigidus. Arthrodesis is a durable procedure, but eliminating motion at the hallux metatarsophalangeal joint may limit certain activities and may prove unacceptable to some patients. In a recent long-term follow-up study, Coughlin and Shurnas12 reported good or excellent outcomes for thirty of thirty patients at a mean of 6.7 years after arthrodesis. The fusion rate was 94%, and there were only two reoperations for hardware removal. No progression of interphalangeal joint arthritis was noted in that study. Residual pain at the first metatarsophalangeal joint after arthrodesis was rated at 0.4 on a 10-point visual analog scale. A recent report on arthrodesis for the treatment of hallux valgus deformity demonstrated a 33% rate of progression of interphalangeal joint arthritis after an average duration of follow-up of 8.6 years, although not all patients were symptomatic1. Despite the success of arthrodesis in terms of reducing pain and providing excellent functional improvements, some patients object to the joint stiffness and the real or perceived functional limitations incurred in association with arthrodesis. For this reason, there is a demand for motion-sparing procedures that will relieve pain, improve or maintain function, and provide a durable result.
Resection arthroplasty, or the original Keller procedure, was introduced for the treatment of hallux valgus in 19044. It has also been recommended for older, less active individuals with severe hallux rigidus, and there is Level-I evidence in the literature supporting the use of the Keller procedure for the treatment of painful osteoarthritis of the first metatarsophalangeal joint in elderly patients. A randomized prospective trial in which arthrodesis was compared with the Keller procedure in patients over forty-five years of age demonstrated a similar incidence of metatarsalgia and similar patient satisfaction following the two procedures13. However, the rate of revision surgery was higher in the arthrodesis group, mainly because of a 44% nonunion rate that was attributed to Kirschner wire fixation at the site of the arthrodesis. Metatarsalgia, cock-up deformities of the hallux, shortening of the first ray, and clawing of the hallux interphalangeal joint have been reported as complications after the original Keller procedure, in which the proximal one-third of the proximal phalanx was resected with or without capsular interposition5,6,14. For these reasons, the Keller procedure in its original form has been largely abandoned for hallux valgus correction.
In 1997, Hamilton et al. reported the results of treatment of hallux rigidus with a modification of the Keller resection arthroplasty that renewed interest in interpositional arthroplasty7. The modification consisted of adding a dorsal capsular interpositional arthroplasty by advancing the dorsal capsule over the first metatarsal head and suturing it to the short toe flexors. Judicious resection of approximately 25% of the base of the proximal phalanx and a dorsal cheilectomy allowed osseous decompression of the metatarsophalangeal joint. The authors advocated detaching the plantar plate and the short toe flexors at their attachment on the base of the proximal phalanx to create a “hanging toe” before suturing the dorsal capsule to the free distal stump of the short toe flexors. The objective was to prevent the metatarsophalangeal joint from hinging with dorsiflexion. A proximal extensor hallucis brevis tenotomy was performed to gain capsular length, and the extensor hallucis longus was lengthened if necessary. The authors reported the outcomes of this procedure for thirty-four feet (thirty patients) and concluded that pain and function were significantly improved and that the average dorsiflexion after the procedure was 50° (as compared with <10° preoperatively). No cock-up deformities of the hallux were noted, and no patient complained of weakness with push-off. Hamilton and Hubbard subsequently reported on a total of fifty-four patients15. They again noted a high degree of patient satisfaction but reported lesser toe metatarsalgia requiring the use of an orthosis in 30% of the patients. Plantar flexion was not reported, and all patients had hallux plantar flexion strength of at least 4 of 5.
Lau and Daniels recently reported on the results of interpositional arthroplasty and cheilectomy in patients with hallux rigidus16. Dorsal cheilectomy was performed for the treatment of stage-II hallux rigidus, whereas interpositional arthroplasty was utilized for the treatment of stage-III hallux rigidus. The authors found that cheilectomy was associated with a higher mean AOFAS score in comparison with interpositional arthroplasty. Substantial weakness of the great toe occurred in 72.7% of patients managed with interpositional arthroplasty but was present in only 16.7% of patients managed with cheilectomy. Plantar pressure measurements demonstrated postoperative weight transfer to the lesser metatarsal heads in both cheilectomy and interpositional arthroplasty patients, but the transfer was greater following interpositional arthroplasty. These results must be interpreted with caution given the bias imposed by the selection of interpositional arthroplasty for the patients with more severe hallux rigidus.
The modified Keller arthroplasty or capsular interpositional arthroplasty as described by Hamilton et al.7 was subsequently modified further by Mroczek and Miller8. Those authors attempted to preserve the attachment of the flexor hallucis brevis to the base of the proximal phalanx by utilizing an oblique proximal phalangeal osteotomy that exits at the level of the subchondral bone of the plantar aspect of the proximal phalanx. The procedure also utilized a dorsal cheilectomy and interposition of the dorsal capsule. The authors noted anecdotally that they were pleased with the results of this procedure, had not seen any postoperative cock-up hallux deformities, and expected a hallux metatarsophalangeal joint range of motion of approximately 50°, although a clinical series was not reported.
To date, there have been limited published reports on outcomes after the modified oblique Keller interpositional arthroplasty. Kennedy et al. reported favorable outcomes after interpositional arthroplasty with preservation of the flexor hallucis brevis insertion17.
Our results suggest that the modified oblique Keller capsular interpositional arthroplasty is a motion-sparing procedure that provides a clinical outcome equivalent to arthrodesis. In our group of patients, arthrodesis resulted in increased plantar pressures at the great toe during walking as compared with arthroplasty. In normal feet, Brown et al. reported an average great toe peak pressure of 236 kPa (23.6 N/cm2) and a first metatarsal peak pressure of 443 kPa (44.3 N/cm2)18. In the present study, the patients in the arthroplasty group exhibited more normal pressures (great toe, 33.26 N/cm2; first metatarsal, 36.18 N/cm2) in comparison with those in the arthrodesis group (great toe, 67.13 N/cm2; first metatarsal, 47.75 N/cm2). We hypothesize that the retained motion of the hallux following arthroplasty allows passive dorsiflexion during the stance phase of gait, thereby allowing a more normal pressure distribution, which we believe to be mechanically beneficial. In addition, we hypothesize that the increase in interphalangeal joint range of motion and the increased great toe pressures may be important factors in the development of degenerative changes at the interphalangeal joint in patients managed with arthrodesis.
There have been previous reports of transfer metatarsalgia after resection arthroplasty6. In the present study, none of the patients in the arthroplasty group reported pain under the lesser metatarsals and the plantar pressure measurements revealed that the pressure under the second metatarsal head was comparable between the arthroplasty and arthrodesis groups. The pressure findings are limited because the study did not have adequate power to detect a clinically relevant between-group difference.
None of the patients exhibited clinical or radiographic evidence of failure after twenty-three to 101 months of follow-up. In the arthrodesis group, there was one case of nonunion and one case of interphalangeal joint arthritis. In comparison, no interphalangeal joint arthritis was noted at the time of follow-up in the arthroplasty group.
An important limitation of our study is the composition of the arthrodesis group. Five patients underwent arthrodesis because of hallux valgus with deformity, and one patient underwent arthrodesis because of a failed silicone implant. Patients with prior failed procedures are not as likely to have a good outcome following surgery. We believe, however, that the arthrodesis group serves as a reasonable comparison group as the surgical approach, technique, methods of fixation, arthrodesis position, and postoperative management are essentially the same despite the underlying reason for the fusion procedure. Another obvious limitation of the study is its retrospective nature. The clinical outcomes data are limited by the fact that the AOFAS score is not validated, and the number of patients was underpowered for meaningful interpretation of the FAAM data.
In summary, these results suggest that the modified oblique Keller capsular interpositional arthroplasty may be an appropriate procedure for patients with late-stage hallux rigidus who want to maintain range of motion while obtaining pain relief as it appears to provide equivalent clinical outcomes to arthrodesis and a more normal pattern of plantar pressures during walking.
Appendix
Tables showing plantar pressure measurements and the range-of-motion results are available with the electronic version of this article on our web site at jbjs.org (go to the article citation and click on “Supporting Data”).
Supplementary Material
Acknowledgments
Note: The authors acknowledge the efforts of Kay Bohnert, research coordinator for the program in physical therapy, as well as the pedobarographic data collection team. They also acknowledge the help of Karen Steger-May, Division of Biostatistics, Washington University School of Medicine.
This publication was made possible by Grant Numbers 1 UL1 RR024992-01, 1 TL1 RR024995-01, and 1 KL2 RR 024994-01 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the Midwest Stone Institute. In addition, one or more of the authors or a member of his or her immediate family received, in any one year, payments or other benefits in excess of $10,000 (Midwest Stone Institute and OrthoHelix Surgical Designs, Inc. [OSDI]) and of less than $10,000 (Midwest Therapy) or a commitment or agreement to provide such benefits from these commercial entities.
References
- 1.Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: intermediate results. Foot Ankle Int. 2005;26:783-92 [DOI] [PubMed] [Google Scholar]
- 2.Fuhrmann RA, Wagner A, Anders JO. First metatarsophalangeal joint replacement: the method of choice for end-stage hallux rigidus? Foot Ankle Clin. 2003;8:711-21, vi [DOI] [PubMed] [Google Scholar]
- 3.Shereff MJ, Jahss MH. Complications of Silastic implant arthroplasty in the hallux. Foot Ankle. 1980;1:95-101 [DOI] [PubMed] [Google Scholar]
- 4.Keller WL. The surgical treatment of bunions and hallux valgus. N Y State J Med. 1904;80:741-2 [Google Scholar]
- 5.Flamme CH, Wülker N, Kuckerts K, Gossé F, Wirth CJ. Follow-up results 17 years after resection arthroplasty of the great toe. Arch Orthop Trauma Surg. 1998;117:457-60 Erratum in: Arch Orthop Trauma Surg. 1999;119:243 [DOI] [PubMed] [Google Scholar]
- 6.Majkowski RS, Galloway S. Excision arthroplasty for hallux valgus in the elderly: a comparison between the Keller and modified Mayo operations. Foot Ankle. 1992;13:317-20 [DOI] [PubMed] [Google Scholar]
- 7.Hamilton WG, O'Malley MJ, Thompson FM, Kovatis PE. Capsular interposition arthroplasty for severe hallux rigidus. Foot Ankle Int. 1997;18:68-70 [DOI] [PubMed] [Google Scholar]
- 8.Mroczek KJ, Miller SD. The modified oblique Keller procedure: a technique for dorsal approach interposition arthroplasty sparing the flexor tendons. Foot Ankle Int. 2003;24:521-2 [DOI] [PubMed] [Google Scholar]
- 9.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26:968-83 [DOI] [PubMed] [Google Scholar]
- 10.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating system for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-53 [DOI] [PubMed] [Google Scholar]
- 11.Meyers-Rice B, Sugars L, McPoil T, Cornwall MW. Comparison of three methods for obtaining plantar pressures in nonpathologic subjects. J Am Podiatr Med Assoc. 1994;84:499-504 [DOI] [PubMed] [Google Scholar]
- 12.Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am. 2003;85:2072-88 [PubMed] [Google Scholar]
- 13.O'Doherty DP, Lowrie IG, Magnussen PA, Gregg PJ. The management of the painful first metatarsophalangeal joint in the older patient. Arthrodesis or Keller's arthroplasty? J Bone Joint Surg Br. 1990;72:839-42 [DOI] [PubMed] [Google Scholar]
- 14.Sherman KP, Douglas DL, Benson MK. Keller's arthroplasty: is distraction useful? A prospective trial. J Bone Joint Surg Br. 1984;66:765-9 [DOI] [PubMed] [Google Scholar]
- 15.Hamilton WG, Hubbard CE. Hallux rigidus. Excisional arthroplasty. Foot Ankle Clin. 2000;5:663-71 [PubMed] [Google Scholar]
- 16.Lau JT, Daniels TR. Outcomes following cheilectomy and interpositional arthroplasty in hallux rigidus. Foot Ankle Int. 2001;22:462-70 [DOI] [PubMed] [Google Scholar]
- 17.Kennedy JG, Chow FY, Dines J, Gardner M, Bohne WH. Outcomes after interposition arthroplasty for treatment of hallux rigidus. Clin Orthop Relat Res. 2006;445:210-5 [DOI] [PubMed] [Google Scholar]
- 18.Brown M, Rudicel S, Esquenazi A. Measurement of dynamic pressures at the shoe-foot interface during normal walking with various foot orthoses using the FSCAN system. Foot Ankle Int. 1996;17:152-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.