Abstract
The carbon dioxide (CO2) laser is a versatile tool that has applications in ablative lasing and caters to the needs of routine dermatological practice as well as the aesthetic, cosmetic and rejuvenation segments. This article details the basics of the laser physics as applicable to the CO2 laser and offers guidelines for use in many of the above indications.
Keywords: CO2 laser, CO2 pixel, dermatological surgery
INTRODUCTION
The carbon dioxide (CO2) laser is the gold standard in ablative lasers. Detailed knowledge of the machines is essential. Over the past decade, advances in laser technology have allowed dermatologists to improve the appearance of scars and wrinkles and to remove benign skin growths using both ablative and nonablative lasers. CO2 laser treatment ensures minimal discomfort and rapid recovery, enabling a quick return to daily routine. The CO2 laser emits an invisible infrared beam at 10,600 nm, targeting both intracellular and extracellular water. When light energy is absorbed by water-containing tissue, skin vaporization occurs.
INDICATIONS
Therapeutic
Actinic and seborrheic keratosis,[1‐5] warts,[6‐9] moles, skin tags, epidermal and dermal nevi,[10‐15] xanthelasma.[16‐19]
Other conditions that have been shown to respond favorably to CO2 laser resurfacing include dermatofibroma,[20] rhinophyma,[21‐25] severe cutaneous photodamage (observed in Favre-Racouchot syndrome), sebaceous hyperplasia, syringomas,[1,26‐29] actinic cheilitis,[30‐33] angiofibroma,[34‐36] scar treatment,[37‐39] keloid,[40‐43] skin cancer,[44‐47] neurofibroma,[48‐50] diffuse actinic keratoses, granuloma pyogenicum,[51] and pearly penile papules.[52]
Aesthetic
Periorbital and perioral wrinkles,[53‐55] facial resurfacing[56‐60] and acne scars,[61‐65] dyschromias including solar lentigines.[66,67]
CONTRAINDICATIONS
Isotretinoin use within the previous six months, active cutaneous bacterial or viral infection in the area to be treated, history of keloid formation or hypertrophic scarring, ongoing ultraviolet exposure, prior radiation therapy to treatment area, collagen vascular disease, chemical peel and dermabrasion.
PREOPERATIVE PREPARATION
Informed consent
Informed consent should be obtained before the procedure according to guidelines.[68] The consent form should specifically state the possible postoperative appearance of the treated area, possible pigmentation changes and need for post-treatment care.
Position
Position the patient according to the area of lesion such that the area to be treated is close to the laser [Table 1].
Table 1.
Appropriate positioning of the area to be treated
| Area to be treated | Position |
|---|---|
| Face, chest and abdomen | Supine position |
| Sides of face, neck and body | Lateral position |
| Nape of neck and back | Prone position |
| Palms | Supine position with palms above his head |
| Soles | Prone position with extended ankle |
Aseptic measures
Gloves, mask and cap should be used by surgeons and assistants. Clean the area with povidone iodine 5% solution (spirit should not be used because it is inflammable).
Anesthesia
Depending upon the site and type of lesions, one of the following types of anesthesia can be given:
Topical anesthesia
Eutectic Mixture of Local Anesthesia (EMLA) cream is used. Apply 2mg/cm2 topically under occlusion for 60 min. The occlusion should be removed just before the procedure.
Local infiltration
Lignocaine 2% with or without adrenaline 1:100000 is used. Dosage of lignocaine plain is 3 mg/kg and lignocaine with adrenaline is 7 mg/kg. Lignocaine with adrenaline should be avoided at areas with end arteries like fingers, toes, earlobes, nose, and penis. Local anesthesia (LA) is injected as follows:
Using 30G needle with bevel pointing upward LA is injected immediately below the planned area of laser. Pinching the lesion before injection will reduce the pain.
In case of palms and soles, insert the needle with 45° angulation to the skin surface.
Inject the anesthesia while withdrawing and slowly to minimize the pain.
Insert the needle at a distance from the lesion such that the tip of the needle is below the lesion after it is pushed in to its full length, failing which anesthesia will be deposited distal to the lesion
Anesthesia must be infiltrated slowly and not pushed in briskly to avoid pain.
Ring block
Ring block is employed to anesthetize fingers, toes and penis. The needle is inserted at the base of the fingers and toes on either side or a ring of anesthesia is deposited around the digit. The LA is injected while withdrawing. A distal digital nerve block on either sides of lateral nail folds can supplement a ring block for nail surgeries. In case of penile region, LA is given at the base of the shaft.
Field block
LA is infiltrated circumferentially around the site blocking the nerve impulse from leaving the area. The actual surgical site is not injected. They are particularly useful when a large area needs to be anesthetized.
Eye protection
Patient's eye should be protected with the eye shield or with wet gauze. Dermatologist and assistants should use wavelength-rated spectacles.
GENERAL INSTRUCTIONS FOR THE OPERATION OF LASER
Hold the hand piece perpendicular to the lesion and press the foot pedal to fire the laser. Vaporize the lesion in coiled, whorled, centrifugal, vertical or horizontal fashion. Vaporize the flat lesions from the top.
Pedunculated lesions can be excised by lasing from the base of the lesion. Hold the lesion with toothed forceps on the top, pull it to the side on the top of the wet gauze (to prevent charring of the normal skin). Always use wet gauze as dry gauze can catch fire.
Wipe the vaporized lesions with wet gauze. Always make sure to dry the area or wipe the water with dry gauze. Look for the raw areas. Coagulate the bleeding spots if any by defocusing the laser beam.
LASER SPECIFICATIONS FOR VARIOUS DERMATOLOGICAL CONDITIONS AND SPECIAL CONCERNS
In additions to the above general measures that have to be adopted for lasing various cutaneous lesions, there are special considerations for some. The same and the laser settings are summarized in Table 2. Figures 1‐14 show the results after CO2 laser in different conditions. It is important to know the relation between the power, irradiance and fluence before performing the procedure [Table 3].
Table 2.
Laser specifications and special considerations for various cutaneous lesions
| Dermatological conditions | Laser settings | Comments |
|---|---|---|
| Actinic and seborrhoeic keratoses | 4 to 7 watts super pulse mode | Topical local anesthesia applied under occlusion at lesions for 45 to 60 min prior to procedure. |
| Dermatosis papulosa nigra | 3.5 to 4.5 watts super-pulsed repeat mode with 0.1 second on and 0.1 second off | Procedure carried out after applying topical LA at each lesion under occlusion. |
| Warts | 9 to 15 watts continuous mode, continuous wave for common warts, use 4 to 6 watts superpulse for flat warts | Precede the vaporization of all types of warts with superficial vaporization of a 1-mm margin of normal skin at half the fluence, before treating the actual lesion, to reduce lesional recurrence. |
| Filiform warts can be excised by vaporizing the base | ||
| Palmoplantar warts | 8 to 15 watts continuous mode, continuous wave | Precede the vaporization of all types of warts with superficial vaporization of a 1-mm margin of normal skin at half the fluence, before treating the actual lesion, to reduce lesional recurrence |
| Skin tags | 4.5 to 7.5 watts continuous mode | Cut the base of the lesion in focused cutting mode, and avulse the skin tag, in case of giant skin tags, exsanguinate the lesion by applying hemostats to peduncle of anesthetized lesion for 5 min prior to laser avulsion |
| Epidermal and dermal nevi | 4.5 to 7.5 watts super pulse mode | The procedure is repeated till the pigmented areas are visible. Do not go too deep to prevent scar formation |
| Intradermal and melanocytic nevi on face | 4.5 to 7.5 watts super pulse mode | Always send the excised specimen for histopathology and keep a close watch for recurrence for lesions with reported junctional activity. Review the patient on Days 30, 120, 360. If any pigment is noted at treated area, vaporize and repeat follow-up as above |
| Syringomas, angiofibroma, sebaceous hyperplasia, senile comedones | 4.5 to 6.5 watts super pulse mode | In case of syringomas, mark all the lesions with skin marking pen, as they will be rendered invisible after infiltration of anesthetic. The marks must be made with a thin-tipped surgical pen and must circumambulate each lesion |
| Scars | 2.5 to 4.5 watts super pulse mode | |
| Granuloma pyogenicum | 9 to 15 watts continuous mode, continuous wave | Coagulate the lesion including the cuff with slight defocusing to avoid puncturing the lesions which will lead to torrential bleeding |
| To attain hemostasis during the procedure, pinch the lesion between the thumb and index finger of the left, hand or apply tourniquet at proximal end | ||
| Earlobe keloids | 9 to 15 watts continuous mode, continuous wave for large earlobe lesions and 4 to 7 watts super pulse for smaller lesions | Follow up the patient at Day 3, 7, 14 and 30, and inject intralesional triamcinalone at site of healed keloids showing early signs of recurrence |
| Mucocele | 3.5 to 4.5 watts super pulse mode | Mark the outer border of the lesion with dotted lines |
| Pearly penile papules | 3.5 to 4.5 watts super pulse mode using single fixed pulses of 0.1 to 0.5 sec | |
| Nail bed reconstruction | 8 to 12 watts continuous mode | Mark the part of the nail to be avulsed with marker pen. Vaporize the nail in vertical fashion running from the proximal to distal end over the marked line. Separate the nail fold from the nail bed with nail elevator, separate proximal and lateral nail folds from nail plate with curved nail elevator. Avulse the part of the nail from the laser marked line to the lateral nail fold. Vaporize the overhanging mass of lateral nail fold tissue that contributes to onychocryptosis |
| Nail bed biopsy | 6.5 to 8.5 watts super pulse mode | Mark a round of 4 to 5 mm on the nail plate just above the site of biopsy |
| Perform the punch biopsy from the nail bed, the size being 1 mm lesser than the avulsed nail plate | ||
| Put back the circular piece of nail bed on the top of the biopsy area to seal the wound |
Figure 1.

Earlobe keloid before laser
Figure 14.
Dermatosis papulosa nigra effectively cleared with laser
Table 3.
The relation between irradiance and fluence
| Power | Irradiance [w/cm2] | Fluence |
|---|---|---|
| 0.5 | 6369.43 | 5.14 |
| 1.0 | 12738.85 | 11.46 |
| 2.0 | 25477.7 | 22.93 |
| 3.0 | 38216.56 | 34.39 |
| 4.2 | 53503.18 | 48.15 |
| 6 | 76433.12 | 68.79 |
| 6.3 | 80254.78 | 72.23 |
| 9 | 114547.54 | 103.09 |
Figure 2.

Earlobe keloid after laser
Figure 3.

Melanocytic nevi before laser
Figure 4.

Melanocytic nevi has healed without scarring after laser
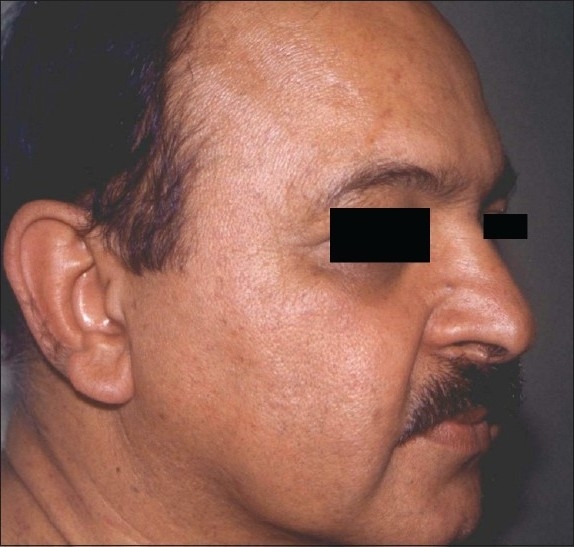
Figure 5.

Pre-treatment photograph of rhinophyma
Figure 6.
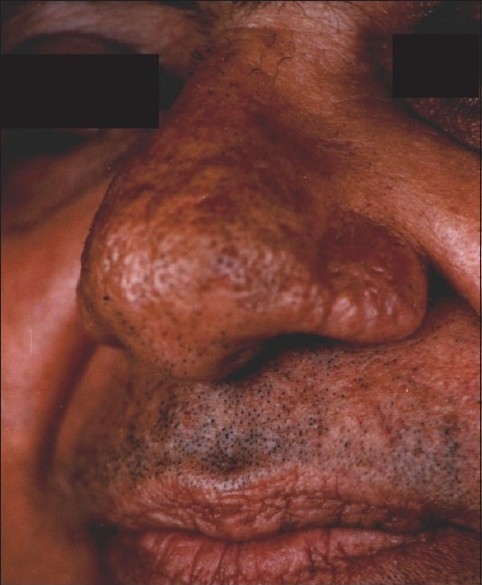
Laser ablation of rhinophyma has healed well with mild residual surface irregularity
Figure 7.

Beckers melanosis on face before treatment
Figure 8.

Significant reduction in pigmentation due to Beckers melanosis after laser
Figure 9.

Verrucous epidermal nevus involving left cheek and neck
Figure 10.

Verrucous epidermal nevus on cheek cleared with mild post-inflammatory hypopigmentation and scarring
Figure 11.
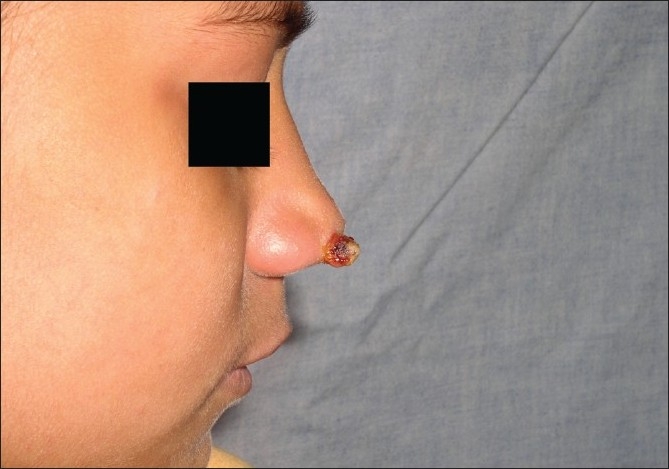
Granuloma telangiectaticum, pre-treatment
Figure 12.

Effective ablation of granuloma telangiectaticum by laser
Figure 13.

Multiple, brown-black papules of Dermatosis papulosa nigra on face
POSTOPERATIVE CARE
Always apply hydrocolloid dressings on facial procedures, never undertake a facial procedure, if hydrocolloid dressings are unavailable. [See Appendix for instructions on use of hydrocolloid dressings].
Apply topical antibiotics for the superficial lesions for one week.
Allow the scabs to fall on own. Avoid picking.
Emphasize on sunscreen application three times a day from day one for the lesions on the face and neck.
Treat for post-inflammatory hyperpigmentation if any with Kligman's formula.
Allow occlusive pressure dressing to remain in place for three to seven days.
Look for healthy granulation tissue after removal of the occlusive dressing.
Avoid contact with dust. Use handyplast if needed for a couple of days for protection.
Appendix.
| How to use hydrocolloid dressings? |
| Remove the dressing before bath |
| Wipe the pus-like material with wet cotton |
| Wash the area with soap and water when you take bath |
| Press the area dry after bath |
| Paint the area and skin around it with povidone iodine 5% solution Wait for 3 min for the solution to dry |
| Apply the dressing, so that the sticky side of the dressing which adheres to the paper sticks to the wound |
| Please remember that when you change the dressing you will find a yellowish brown material which may look and smell like pus, but this is not pus, it is the material in the dressing which melts when it comes into contact with the wound |
| Calibration of CO2 laser fluence[69] |
| Power = joules/sec watts |
| Spot size = πR2 |
| R = Radius = Diameter/2 cm |
| Irradiance = Power/spot size |
| Fluence = Irradiance × Time in sec |
| If |
| Diameter = 0.1 mm = 0.01 cm |
| Time = 0.9 m sec = 0.0009 sec |
| Radius = 0.005 cm |
| Radius2 = 0.000025 cm |
| Spot size = πR2 = 0.00007857 |
| Calibration of CO2 pixel laser |
| W = J/sec |
| 21 W = 21J/1 sec ⇒ 21W × 1 sec = 21J |
| ⇒ 21 W × 0.5 sec = 10.5J |
| We are using the 7*7 tip, hence 49 pixel dots. |
| For each pixel dot: 10.5 W/49 pixels = 0.21 W/pixel dot |
| The diameter of each pixel dot is 100 micron: |
| J = W/A ⇒ 0.21/(0.1)2*II/4 = 26.75 J/P/cm2 |
COMPLICATIONS
Minor complications although frequent, are usually of minimal consequence and include post-inflammatory hyperpigmentation, milia formation, perioral dermatitis, acne and/or rosacea exacerbation and contact dermatitis. Hyperpigmentation or erythema over the treated area is common in colored skin and causes anxiety to patients. However, this is temporary, lasting for only about six weeks and gradually improves.
More serious complications include localized viral, bacterial, and candidial infection, delayed hypopigmentation, persistent erythema, and prolonged healing. The most severe complications are hypertrophic scarring, disseminated infection, and ectropion. Early detection of complications and rapid institution of appropriate therapy are extremely important. Delay in treatment can have severe deleterious consequences including permanent scarring and dyspigmentation.
PRACTICAL TIPS ON USE OF CO2 LASER
Always use hand piece pointer on skin to cut.
Remember, lens focuses beam and renders it collimated.
Moving hand piece away [defocusing] leads to logarithmic fall in irradiance; use this to coagulate.
Super-pulse CO2 laser reduces dwell time, maximizes power.
Use continuous wave in highly vascular lesions and areas, debulking and where esthetics is not an issue e.g., foot.
Under-treat, eschew therapeutic greed.
Laser settings in texts are often for collimated hand pieces, read carefully before applying. One-third to one-fourth the irradiance suggested in the texts seems to deliver the results.
The newer CO2 lasers with advanced output control software when used in the super-pulsed mode for carrying out free hand procedures are versatile devices with numerous therapeutic options.
GUIDELINES FOR CO2 PIXEL LASER
Apply topical anesthesia liberally. Occlude the anesthetic cream with provided plastic sheets and 3M transpore and leave it for 30-45 min.
After 30-45 min, remove the occlusion and wipe the anesthesia completely with dry gauze.
Set the pixel laser at 21 watts.
Give single pass using 7*7 tip, that is, 49 pixel dots. Avoid overlapping but give two passes if scars are deep.
Apply hydrocolloid dressing for 12 h.
Procedure has to be repeated every month for four months.
Multiple-Choice Questions
- Which of the following is true about CO2 laser?
- It is an ablative laser
- It is a non-ablative laser
- It is a semi-ablative laser
- It is a minimally ablative laser
- The wavelength of the CO2 laser is
- 10,600 nm
- 1,064 nm
- 2,640 mm
- 10,640 nm
- The chromophore for CO2 laser is
- Air
- Water
- Melanin
- Hemoglobin
- The following is not an absolute contraindication for CO2 laser therapy:
- Patient on isotretinoin
- Keloidal tendency
- Active viral infection
- Skin phototype 4 and 5
- The following must not be used to sterilize the treatment area in CO2 laser therapy:
- Povidone iodine
- Chlorhexidine
- Cetrimide
- Ethanol
- This equipment is mandatory while carrying out a CO2 laser procedure
- Cold air blower
- Airconditioning
- Smoke evacuator
- Operating theatre lights
- Dermatosis papulosa nigra is treated with the following type of anesthesia:
- Ring block
- Field block
- Topical anesthesia
- General anesthesia
- To cut with the CO2 laser, which mode is most suited?
- Focused
- Defocused
- Fractionated
- Collimated
Answers
1. a, 2. a, 3. b, 4. d, 5. d, 6. c, 7. c, 8. a.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Trimas SJ, Ellis DA, Metz RD. The carbon dioxide laser: An alternative for the treatment of actinically damaged skin. Dermatol Surg. 1997;23:885–9. [PubMed] [Google Scholar]
- 2.Phahonthep R, Sindhuphak W, Sriprajittichai P. Lidocaine iontophoresis versus EMLA cream for CO2 laser treatment in seborrheic keratosis. J Med Assoc Thai. 2004;87:S15–8. [PubMed] [Google Scholar]
- 3.Fulton JE, Rahimi AD, Helton P, Dahlberg K, Kelly AG. Disappointing results following resurfacing of facial skin with CO2 lasers for prophylaxis of keratosis and cancers. Dermatol Surg. 1999;25:729–32. doi: 10.1046/j.1524-4725.1999.99035.x. [DOI] [PubMed] [Google Scholar]
- 4.Fitzpatrick RE, Goldman MP, Ruiz-Esparza J. Clinical advantage of the CO2 laser superpulsed mode.Treatment of verruca vulgaris, seborrheic keratosis, lentigines and actinic cheilitis. J Dermatol Surg Oncol. 1994;20:449–56. doi: 10.1111/j.1524-4725.1994.tb03215.x. [DOI] [PubMed] [Google Scholar]
- 5.Quaedvlieg PJ, Ostertag JU, Krekels GA, Neumann HA. Delayed wound healing after three different treatments for widespread actinic keratosis on the atrophic bald scalp. Dermatol Surg. 2003;29:1052–6. doi: 10.1046/j.1524-4725.2003.29301.x. [DOI] [PubMed] [Google Scholar]
- 6.Lauchli S, Kempf W, Dragieva G, Burg G, Hafner J. CO2 laser treatment of warts in immunosuppressed patients. Dermatology. 2003;206:148–52. doi: 10.1159/000068459. [DOI] [PubMed] [Google Scholar]
- 7.Geronemus RG, Kauvar AN, McDaniel DH. Treatment of recalcitrant verrucae with both the ultrapulse CO2 and PLDL pulsed dye lasers. Plast Reconstr Surg. 1998;101:2010. doi: 10.1097/00006534-199806000-00057. [DOI] [PubMed] [Google Scholar]
- 8.Landsman MJ, Mancuso JE, Abramow SP. Carbon dioxide laser treatment of pedal verrucae. Clin Podiatr Med Surg. 1992;9:659–69. [PubMed] [Google Scholar]
- 9.Lim JT, Goh CL. Carbon dioxide laser treatment of periungual and subungual viral warts. Australas J Dermatol. 1992;33:87–91. doi: 10.1111/j.1440-0960.1992.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 10.Hohenleutner U, Wlotzke U, Konz B, Landthaler M. Carbon dioxide laser therapy of a widespread epidermal nevus. Lasers Surg Med. 1995;16:288–91. doi: 10.1002/lsm.1900160311. [DOI] [PubMed] [Google Scholar]
- 11.Khoo L. Carbon dioxide laser treatment of benign skin lesions. National Skin Centre Experience. 2001;12:2. [Google Scholar]
- 12.Verma KK, Ovung EM. Epidermal and sebaceous nevi treatment with CO2 laser. Indian J Dermatol Venereol Leprol. 2002;68:23–4. [PubMed] [Google Scholar]
- 13.Ratz JL, Bailin PL, Wheeland RG. Carbon dioxide laser treatment of epidermal nevi. J Dermatol Surg Oncol. 1986;12:567–70. doi: 10.1111/j.1524-4725.1986.tb01953.x. [DOI] [PubMed] [Google Scholar]
- 14.Boyce S, Alster TS. CO2 laser treatment of epidermal nevi: Long-term success. Dermatol Surg. 2002;28:611–4. [PubMed] [Google Scholar]
- 15.Hohenleutner U, Landthaler M. Laser therapy of verrucous epidermal naevi. Clin Exp Dermatol. 1993;18:124–7. doi: 10.1111/j.1365-2230.1993.tb00991.x. [DOI] [PubMed] [Google Scholar]
- 16.Raulin C, Schoenermark MP, Werner S, Greve B. Xanthelasma palpebrarum: Treatment with the ultrapulsed CO2 laser. Lasers Surg Med. 1992;24:122–7. doi: 10.1002/(sici)1096-9101(1999)24:2<122::aid-lsm7>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 17.Alster TS, West TB. Ultrapulse CO2 laser ablation of xanthelasma. J Am Acad Dermatol. 1996;34:848–9. doi: 10.1016/s0190-9622(96)90042-0. [DOI] [PubMed] [Google Scholar]
- 18.Ullmann Y, Harshai Y, Peled IJ. The use of CO2 laser for the treatment of xanthelasma palpebrarum. Ann Plast Surg. 1993;31:504–7. doi: 10.1097/00000637-199312000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Gladstone GJ, Beckman H, Elson LM. CO2 laser excision of xanthelasma lesion. Arch Ophthalmol. 1985;103:440–2. doi: 10.1001/archopht.1985.01050030136040. [DOI] [PubMed] [Google Scholar]
- 20.Krupa Shankar DS, Kushalappa AA, Suma KS, Pai SA. Multiple dermatofibromas on face treated with carbon dioxide laser. Indian J Dermatol Venereol Leprol. 2007;73:194–5. doi: 10.4103/0378-6323.32747. [DOI] [PubMed] [Google Scholar]
- 21.Simo R, Sharma VL. The use of the CO2 laser in rhinophyma surgery: Personal technique and experience, complications and long-term results. Fac Plast Surg. 1998;14:287–95. doi: 10.1055/s-2008-1064459. [DOI] [PubMed] [Google Scholar]
- 22.Goon PK, Dalal M, Peart FC. The gold standard for decortication of rhinophyma: Combined erbium-YAG/CO2 laser. Aesthetic Plast Surg. 2004;28:456–60. doi: 10.1007/s00266-004-0012-x. [DOI] [PubMed] [Google Scholar]
- 23.Bohigian RK, Sharpshay SM, Hybels RL. Management of rhinophyma with carbon dioxide laser: Lahey Clinic experience. Lasers Surg Med. 1988;8:397–401. doi: 10.1002/lsm.1900080410. [DOI] [PubMed] [Google Scholar]
- 24.Sharpshay SM, Strong MS, Anatasi GW, Vaughan CW. Removal of Rhinophyma with the CO2 laser: A preliminary report. Arch Otolaryngol. 1980;106:257–9. doi: 10.1001/archotol.1980.00790290009004. [DOI] [PubMed] [Google Scholar]
- 25.Greenbauns SS, Krull EA, Watrick K. Comparison of CO2 laser and electrosurgery in the treatment of rhinophyma. J Am Acad Dermatol. 1988;18:363–8. doi: 10.1016/s0190-9622(88)70053-5. [DOI] [PubMed] [Google Scholar]
- 26.Wang JI, Roenigk HH., Jr Treatment of multiple facial syringomas with the carbon dioxide laser. Dermatol Surg. 1999;25:136–9. doi: 10.1046/j.1524-4725.1999.08111.x. [DOI] [PubMed] [Google Scholar]
- 27.Wheeland RG, Bailin PL, Reynolds OD, Ratz JL. Carbon dioxide laser vaporization of multiple facial syringomas. J Dermatol Surg Oncol. 1986;12:225–8. doi: 10.1111/j.1524-4725.1986.tb01457.x. [DOI] [PubMed] [Google Scholar]
- 28.Nerad JA, Anderson RL. CO2 laser treatment of eyelid syringomas. Ophthal Plast Reconstr Surg. 1988;4:91–4. doi: 10.1097/00002341-198804020-00006. [DOI] [PubMed] [Google Scholar]
- 29.Kang WH, Kim NS, Kim YB, Shim WC. A new treatment for syringoma: Combination of carbon dioxide laser and trichloroacetic acid. Dermatol Surg. 1998;24:1370–4. [PubMed] [Google Scholar]
- 30.Duane C, Whitaker MD. Microscopically proven cure of actinic cheilitis by CO2 laser. Lasers Surg Med. 2005;7:520–3. doi: 10.1002/lsm.1900070615. [DOI] [PubMed] [Google Scholar]
- 31.Laws RA, Wilde JL, Grabski WJ. Comparison of electrodessication with CO2 laser for the treatment of actinic cheilitis. Dermatol Surg. 2000;26:349–53. doi: 10.1046/j.1524-4725.2000.99286.x. [DOI] [PubMed] [Google Scholar]
- 32.Alamillos-Granados FJ, Naval-Gias L, Dean-Ferrer A, Alonso del Hoyo JR. Carbon dioxide laser vermilionectomy for actinic cheilitis. J Oral Maxillofac Surg. 1993;51:118–21. doi: 10.1016/s0278-2391(10)80004-7. [DOI] [PubMed] [Google Scholar]
- 33.Zelickson BD, Roenigk RK. Actinic cheilitis: Treatment with the carbon dioxide laser. Cancer. 1990;65:1307–11. doi: 10.1002/1097-0142(19900315)65:6<1307::aid-cncr2820650609>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 34.Belmar P, Boixeda P, Baniandres O, Fernandez-Lorente M, Arrazola JM. Long-term follow up of angiofibromas treated with CO2 laser in 23 patients with tuberous sclerosis. Actas Dermosifiliogr. 2005;96:498–503. doi: 10.1016/s0001-7310(05)73121-5. [DOI] [PubMed] [Google Scholar]
- 35.Papadavid E, Markey A Bellaney G, Walker NP. Carbon dioxide and pulsed dye laser treatment of angiofibromas in 29 patients with tuberous sclerosis. Br J Dermatol. 2002;147:337–42. doi: 10.1046/j.1365-2133.2002.04968.x. [DOI] [PubMed] [Google Scholar]
- 36.Verma KK, Ovung EM, Sirka CS. Extensive facial angiofibromas in tuberous sclerosis treated with carbon dioxide laser abrasion. Dermato Surg. 2001;67:326–8. [PubMed] [Google Scholar]
- 37.Lupton JR, Alster TS. Laser scar revision. Dermatol Clin. 2002;20:55–65. doi: 10.1016/s0733-8635(03)00045-7. [DOI] [PubMed] [Google Scholar]
- 38.Ostertag JU, Theunissen CC, Neumann HA. Hypertrophic scars after therapy with CO2 laser for treatment of multiple cutaneous neurofibromas. Dermatol Surg. 2002;28:296–8. doi: 10.1046/j.1524-4725.2002.01145.x. [DOI] [PubMed] [Google Scholar]
- 39.Kand DH, Park SH, Koo SH. Laser resurfacing of smallpox scars. Plast Reconst Surg. 2005;116:259–65. doi: 10.1097/01.prs.0000170093.62733.e5. [DOI] [PubMed] [Google Scholar]
- 40.Nowak KC, McCormack M, Koch RJ. The effect of superpulsed carbon dioxide laser energy on keloid and normal dermal fibroblast secretion of growth factors: A serum-free study. Plast Reconstr Surg. 2000;105:2039–48. doi: 10.1097/00006534-200005000-00019. [DOI] [PubMed] [Google Scholar]
- 41.Apfelberg DB, Maser MR, Lash H, White D, Weston J. Preliminary results of argon and carbon dioxide laser treatment of keloid scars. Lasers Surg Med. 1984;4:283–90. doi: 10.1002/lsm.1900040309. [DOI] [PubMed] [Google Scholar]
- 42.Cheng ET, Pollard JD, Koch RJ. Effect of blended CO2 and erbium: YAG laser irradiation on normal and keloid fibroblasts: A serum-free study. J Clin Laser Med Surg. 2003;21:337–43. doi: 10.1089/104454703322650130. [DOI] [PubMed] [Google Scholar]
- 43.Krupa Shankar DS, Gupta V. Management of ear rim keloid with carbon dioxide laser. Indian J Dermatol Venereol Leprol. 2007;73:445. doi: 10.4103/0378-6323.32747. [DOI] [PubMed] [Google Scholar]
- 44.Kim ES, Kim KJ, Chang SE, Lee MW, Choi JH, Moon KC, et al. Metaplastic ossification in a cutaneous pyogenic granuloma: A case report. J Dermatol. 2004;31:326–9. doi: 10.1111/j.1346-8138.2004.tb00679.x. [DOI] [PubMed] [Google Scholar]
- 45.Vaosse V, Clerici T, Fusade T. Bowen disease treated with scanned pulsed high energy CO2 laser.Follow-up of 6 cases. Ann Dermatol Venereol. 2001;128:1220–4. [PubMed] [Google Scholar]
- 46.Nouri K, Chang A, Trent JT, Jiminez GP. Ultrapulse CO2 used for the successful treatment of basal cell carcinomas found in patients with basal cell nevus syndrome. Dermatol Surg. 2002;28:287–90. doi: 10.1046/j.1524-4725.2002.01080.x. [DOI] [PubMed] [Google Scholar]
- 47.Humphreys TR, Malhotra R, Scharf MJ, Marcus SM, Starkus L, Calegari K. Treatment of superficial basal cell carcinoma and squamous cell carcinoma in situ with a high-energy pulsed carbon dioxide laser. Arch Dermatol. 1998;134:1247–52. doi: 10.1001/archderm.134.10.1247. [DOI] [PubMed] [Google Scholar]
- 48.Lapid-Gortzak R, Lapid O, Monos T, Lifshitz T. CO2 -laser in the removal of a plexiform neurofibroma from the eyelid. Ophthalmic Surg Lasers. 2000;31:432–4. [PubMed] [Google Scholar]
- 49.Becker DW. Use of the carbon dioxide laser in treating multiple cutaneous neurofibromas. Ann Plast Surg. 1991;26:582–6. doi: 10.1097/00000637-199106000-00016. [DOI] [PubMed] [Google Scholar]
- 50.Roenigk RK, Ratz JL. CO2 laser treatment of cutaneous neurofibromas. J Dermatol Surg Oncol. 1987;13:187–90. doi: 10.1111/j.1524-4725.1987.tb00517.x. [DOI] [PubMed] [Google Scholar]
- 51.Raulin C, Petzoldt D, Werner S. Granuloma pyogenicum—Removal with the CO2 laser. Hautarzt. 1997;48:402–5. doi: 10.1007/s001050050601. [DOI] [PubMed] [Google Scholar]
- 52.Magid M, Garden JM. Pearly penile papules: Treatment with the carbon dioxide laser. J Dermatol Surg Oncol. 1989;15:552–4. doi: 10.1111/j.1524-4725.1989.tb03416.x. [DOI] [PubMed] [Google Scholar]
- 53.Fitzpatrick RE, Goldman MP, Satur NM, Tope WD. Pulsed carbon dioxide laser resurfacing of photo-aged facial skin. Arch Dermatol. 1996;132:395–402. [PubMed] [Google Scholar]
- 54.Pitanguy I, Soares GL, Machado BH, de Amorim NF. CO2 laser peeling associated with the 'round lifting' technique. J Cosmet Laser Ther. 1999;1:145–52. doi: 10.1080/14628839950516797. [DOI] [PubMed] [Google Scholar]
- 55.Papadavid, Evangelia MD, Katsambas, Andreas MD. Lasers for facial rejuvenation: A review. Int J Dermatol. 2003;42:480–7. doi: 10.1046/j.1365-4362.2003.01784.x. [DOI] [PubMed] [Google Scholar]
- 56.Alster T, Hirsch R. Single-pass CO2 laser skin resurfacing of light and dark skin: Extended experience with 52 patients. J Cosmet Laser Ther. 2003;5:39–42. [PubMed] [Google Scholar]
- 57.Tanzi EL, Alster TS. Single-pass carbon dioxide versus multiple-pass Er:YAG laser skin resurfacing: A comparison of postoperative wound healing and side-effect rates. Dermatol Surg. 2003;29:80–4. doi: 10.1046/j.1524-4725.2003.29012.x. [DOI] [PubMed] [Google Scholar]
- 58.Huilgol SC, Poon E, Calonje E, Seed PT, Huilgol RR, Markey AC, et al. Scanned continuous wave CO2 Laser resurfacing: A closer look at the different scanning modes. Dermatol Surg. 2001;27:467–70. doi: 10.1046/j.1524-4725.2001.00108.x. [DOI] [PubMed] [Google Scholar]
- 59.Lent WM, David LM. laser resurfacing: A safe and predictable method of skin resurfacing. J Cutan Laser Ther. 1999;1:87–94. doi: 10.1080/14628839950516913. [DOI] [PubMed] [Google Scholar]
- 60.Goodman GJ. Carbondioxide Laser resurfacing: Preliminary observations on short-term follow up.A subjective study of 100 patients attitudes and outcomes. Dermatol Surg. 1998;24:665–72. doi: 10.1111/j.1524-4725.1998.tb04225.x. [DOI] [PubMed] [Google Scholar]
- 61.Weinstein C. Carbon dioxide Laser resurfacing: Long-term follow-up in 2123 patients. Clin Plast Surg. 1998;25:109–30. [PubMed] [Google Scholar]
- 62.Sawcer D, Lee HR, Lowe NJ. Lasers and adjunctive treatments for facial scars. J Cutan Laser Ther. 1999;1:77–85. doi: 10.1080/14628839950516904. [DOI] [PubMed] [Google Scholar]
- 63.Goh CL, Khoo L. Laser skin resurfacing treatment outcome of facial scars and wrinkles in Asians with skin type III-IV with the Unipulse CO2 laser system. Singapore Med J. 2002;43:28–32. [PubMed] [Google Scholar]
- 64.Tanzi EL, Alster TS. Single-pass carbon dioxide versus multiple-pass Er:YAG Laser skin resurfacing: A comparison of postoperative wound healing and side-effect rates. Dermatol Surg. 2003;29:80–4. doi: 10.1046/j.1524-4725.2003.29012.x. [DOI] [PubMed] [Google Scholar]
- 65.Goodman GJ. Carbon dioxide laser resurfacing: Preliminary observations on short-term follow up: A subjective study of 100 patients' attitudes and outcomes. Dermatol Surg. 1998;24:665–72. doi: 10.1111/j.1524-4725.1998.tb04225.x. [DOI] [PubMed] [Google Scholar]
- 66.Stern RS, Dover JS, Levin JA, Arndt KA. Laser therpy versus cryo therapy of lentigines: A comparative trial. J Am Acad Dermatol. 1994;30:985–7. doi: 10.1016/s0190-9622(94)70123-7. [DOI] [PubMed] [Google Scholar]
- 67.Dover JS, Smoller BR, Stern RS, Rosen S, Arndt KA. Low-fluence carbon dioxide laser irradiation of lentigines. Arch Dermatol. 1986;124:8. [PubMed] [Google Scholar]
- 68.Krupashankar DS. Standard guidelines of care: CO2 laser for removal of benign skin lesions and resurfacing. Indian J Dermatol Venereol Leprol. 2008;74:61–7. [PubMed] [Google Scholar]
- 69.Rosio TJ. Basic laser physics. In: Roenigk RK, Ratz JL, Roenigk HH, editors. Roenigk's dermatologic surgery. 3rd ed. New York: Informa Healthcare; 2007. pp. 607–24. [Google Scholar]


