Abstract
Objective
Provide benchmarking information for a large national sample of patients receiving inpatient rehabilitation following traumatic brain injury.
Design
Secondary data analysis from 893 medical rehabilitation facilities located in the United States that contributed information to the Uniform Data System for Medical Rehabilitation (UDSMR) from January 2000 through December 2007. Variables analyzed included demographic information (age, sex, marital status, race/ethnicity, pre-hospital living setting, discharge setting), hospitalization information (length of stay, program interruptions, payer, onset date, rehabilitation impairment group, ICD-9 codes for admitting diagnosis, comorbidities), and functional status information (FIM® instrument [“FIM”] ratings at admission and discharge, FIM efficiency, FIM gain).
Results
Descriptive statistics from 101,188 patients showed length of stay decreasing from a mean of 22.7 (±20.5) days to 16.6 (±14.8) over the 8-year study period. FIM total admission and discharge ratings also decreased. Mean admission ratings decreased from 58.6 (±24.7) to 54.8 (±21.2). Mean discharge ratings decreased from 92.4 (±24.2) to 85.0 (±24.0). Accordingly, mean FIM change decreased from 33.8 (±20.5) to 30.2 (±18.4). The percent of persons discharged to the community ranged from 81.3% in 2000 to 74.1% in 2007. All results are likely influenced by various policy changes affecting classification and/or documentation processes.
Conclusions
National rehabilitation data from persons with traumatic brain injury in 2000-2007 indicate patients are spending less time in an inpatient care setting than in previous years and are experiencing improvements in functional independence during their stay. In addition, a majority of patients are discharged to community settings following inpatient rehabilitation.
Keywords: Rehabilitation Outcomes, Benchmark, Quality Improvement, Traumatic Brain Injury
INTRODUCTION
This article represents the second in the series of impairment-specific longitudinal reports from the Uniform Data System for Medical Rehabilitation (UDSMR®) database. The purpose of these reports is to provide important benchmarking information for key rehabilitation outcomes such as length of stay, functional status, and discharge setting within common inpatient rehabilitation impairment groups. This report includes information on patients with traumatic brain injury who received comprehensive inpatient rehabilitation services in facilities that subscribed to the UDSMR from 2000 through 2007. A previous report presented the same information on patients receiving inpatient rehabilitation for stroke.1 This current series is a continuation of prior reports published in this journal (1990 through 1999).2-11 Those reports contained single-year summaries from several rehabilitation impairment categories. The new format facilitates the recognition of trends in rehabilitation outcomes over time while still providing thorough yearly summaries that can serve as valuable reference resources for rehabilitation outcomes researchers and can help guide facility-level quality improvement efforts moving forward.
Data Source
The UDSMR, a not-for-profit organization affiliated with the UB Foundation Activities, Inc. at the State University of New York at Buffalo, maintains the largest non-governmental database for medical rehabilitation outcomes. Since 1987 the UDSMR has collected data from rehabilitation hospitals and units, long-term care hospitals, skilled nursing facilities, as well as pediatric and outpatient rehabilitation programs. Approximately 70% of inpatient rehabilitation facilities in the United States utilize UDSMR services. Subscribing facilities receive detailed summaries comparing their patient data to both regional and national benchmarks. This information is often used to evaluate quality management efforts and to comply with criteria required by The Joint Commission and the Commission on Accreditation of Rehabilitation Facilities as well as other accrediting organizations. Additional information on the UDSMR is available from their web site at: http://www.udsmr.org/
This report contains information for persons receiving inpatient medical rehabilitation services from 1/1/2000 through 12/31/2007. The data are aggregated and presented using an October to September fiscal year schedule (see Variable Definitions below). Thus, in all tables and figures 2000 includes only three-quarters (1/1/2000 – 9/30/2000) of the calendar year and 2008 includes only one-quarter (10/1/2007 – 12/31/2007) of the calendar year.
Data Set
The UDSMR® database contains comprehensive demographic, hospitalization, diagnostic, and functional status data. Demographic data includes age, sex, marital status, race or ethnicity, pre-hospital living setting and discharge setting. Hospitalization and diagnostic information include length of stay, program interruptions, payer, impairment/event onset date, the rehabilitation impairment group, and ICD-9 codes for the admitting diagnosis and complications or comorbidities. Functional status information includes ratings from the FIM® instrument (“FIM”) for admission and discharge, FIM efficiency and FIM gain (see descriptions below).
The FIM includes 18 items covering six domains (self-care, sphincter control, mobility, locomotion, communication and social cognition). Each item is rated on a scale from 1 (complete dependence) to 7 (complete independence) with higher ratings representing greater functional independence (range 18 to 126). The FIM was designed as an indicator of disability, which is measured in terms of assistance required to complete a task. FIM ratings are also presented as Motor and Cognitive subscales. The Motor subscale includes 13 items assessing self-care, sphincter control, mobility and locomotion. The Cognitive subscale includes 5 items examining communication and social cognition. The reliability, validity and responsiveness of the FIM have been documented by independent investigators.12-14
The data collected in 2000 and 2001 included the original UDSMR protocol for administering the FIM instrument (version 5.1). In 2002, the FIM was integrated into the Inpatient Rehabilitation Facilities-Patient Assessment Instrument (IRF-PAI) developed by the Centers for Medicare and Medicaid Services (CMS) as part of the prospective payment system for inpatient rehabilitation facilities.15 Some changes were made to the FIM protocol and rating procedures. These changes have been described in documents produced by CMS16 and in recent publications and will not be presented in detail here.17,18 The major changes potentially impacting comparisons between pre-PPS and PPS FIM data include the following: 1) admission and discharge assessment time frame, 2) use of 0 for some admission motor items, 3) change in recording for bowel and bladder management, and 4) change in definition for program interruption.
Variable Definitions
Case-mix groups (CMGs) is the patient classification system that helps determine the reimbursement that a facility is paid for Medicare Part A fee-for-service inpatient care. Each Medicare eligible patient is assigned to a CMG at admission to rehabilitation based on his or her primary impairment or medical condition, adjusted FIM rating, and (for select CMGs) age.19 There are currently 7 CMGs for traumatic brain injury rehabilitation.
CMG comorbidity tiers represent another factor that affects facility reimbursement from Medicare. Relative weightings (which are converted to payments) are stratified by tier across each CMG based on the presence of specific comorbidities that are likely to increase costs.20 These payment adjustments for comorbidities consist of a four-tier system: Tier 1 (high cost), Tier 2 (medium cost), Tier 3 (low cost), and no Tier.21
Community discharge identifies patients discharged to a community-based setting: home or an assisted living, a board and care, or a transitional living setting.
FIM efficiency refers to the average change in total FIM instrument ratings per day. It is calculated for each patient by subtracting FIM admission from FIM discharge ratings and then dividing by length of stay in days.
FIM gain is the difference between total FIM instrument admission and total FIM discharge ratings.
Length of stay is the total number of days spent in the rehabilitation facility. Interim days spent in an acute care setting resulting in a program interruption are not included in this value.
Onset to admit quantifies the duration (in days) from impairment onset to rehabilitation admission. In traumatic brain injury, onset date and acute-care admission (hospitalization) date are typically the same.
Program interruption identifies patients who were temporarily (≤ 30 days in 2000 and 2001 and ≤ 3 days beginning in 2002) transferred to an acute care setting and then returned for additional inpatient rehabilitation services.
Year discharged refers to the date of discharge from inpatient rehabilitation in relation to the Federal fiscal year. The Federal fiscal year runs from October 1 through September 30; e.g., fiscal year 2006 includes 10/1/2005 – 9/30/2006. CMS policy changes governing inpatient rehabilitation are traditionally implemented at the beginning of the fiscal rather than the calendar year.
Inclusion Criteria
We applied five basic criteria for cases to be included in this report: 1) the patient must have been receiving initial rehabilitation services (i.e., no admits for evaluation or readmissions, etc.), 2) the record could not have missing data for key benchmarking variables such as discharge setting or FIM ratings (this excludes patients who died during their rehabilitation stay), 3) the patient had to be between the ages of 7 and 105 years at admission, 4) the duration from impairment onset to rehabilitation admission could not exceed 365 days (1 year), and 5) the total length of stay could not exceed 548 days (1.5 years).
Descriptive Summary of Aggregate Data
The number of contributing facilities ranged from 785 to 893 per year over the 8-year study period. The percentage of patients receiving care in hospital-based rehabilitation units was substantially greater than in freestanding facilities across all years (see Table 1).
Table 1.
Facility and patient characteristics stratified by discharge year: percentage or mean (sd).
| Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Patients, N | 101,188 | 8,185 | 12,790 | 11,277 | 11,251 | 11,801 | 13,447 | 14,330 | 14,458 | 3,649 |
| Hospital unit | 62.6% | 61.7% | 54.1% | 55.8% | 63.6% | 65.6% | 66.4% | 65.4% | 65.6% | 66.2% |
| Freestanding | 37.4% | 38.2% | 45.9% | 44.2% | 36.4% | 34.4% | 33.6% | 34.6% | 34.4% | 33.8% |
| Age, yrs | 54.2 (24.0) | 47.1 (22.9) | 48.5 (23.0) | 51.2 (23.8) | 53.4 (24.2) | 55.0 (24.0) | 56.3 (23.9) | 57.7 (23.6) | 58.6 (23.6) | 59.1 (23.3) |
| <45 | 38.0% | 51.0% | 48.0% | 43.5% | 39.9% | 36.3% | 34.0% | 31.6% | 30.0% | 28.6% |
| 45-64 | 21.2% | 21.0% | 22.2% | 20.8% | 19.7% | 20.8% | 21.3% | 21.8% | 21.6% | 22.5% |
| 65-74 | 12.1% | 9.6% | 10.2% | 11.3% | 12.5% | 13.0% | 12.5% | 12.7% | 13.1% | 13.9% |
| 75+ | 28.7% | 18.4% | 19.7% | 24.5% | 28.0% | 29.9% | 32.2% | 33.9% | 35.2% | 35.0% |
| Gender | ||||||||||
| Men | 65.0% | 68.2% | 66.9% | 66.2% | 65.3% | 64.0% | 63.5% | 64.3% | 64.0% | 63.6% |
| Women | 35.0% | 31.8% | 33.1% | 33.8% | 34.7% | 36.0% | 36.5% | 35.7% | 36.0% | 36.4% |
| Married | ||||||||||
| No | 59.9% | 62.9% | 62.0% | 60.8% | 60.2% | 59.5% | 59.4% | 58.9% | 58.0% | 58.6% |
| Yes | 40.1% | 37.1% | 38.0% | 39.2% | 39.8% | 40.5% | 40.6% | 41.1% | 42.0% | 41.4% |
| Race / ethnicity | ||||||||||
| White | 79.6% | 77.7% | 79.0% | 79.2% | 78.9% | 80.0% | 80.6% | 79.9% | 80.6% | 78.6% |
| Black | 9.2% | 11.7% | 10.8% | 9.8% | 9.4% | 8.6% | 8.4% | 8.6% | 7.9% | 8.3% |
| Hispanic | 7.1% | 6.9% | 6.5% | 7.2% | 7.6% | 7.5% | 6.9% | 6.8% | 6.8% | 8.5% |
| Other | 4.1% | 3.7% | 3.7% | 3.8% | 4.1% | 3.8% | 4.2% | 4.8% | 4.6% | 4.6% |
| Primary insurance | ||||||||||
| Medicare | 36.9% | 24.7% | 26.4% | 33.7% | 36.9% | 39.7% | 41.6% | 42.5% | 42.3% | 41.7% |
| Medicare managed care | 2.6% | 1.3% | 1.4% | 1.8% | 2.0% | 2.3% | 2.6% | 3.4% | 4.5% | 5.5% |
| Commercial | 22.8% | 27.9% | 28.0% | 25.1% | 23.2% | 21.7% | 20.5% | 20.3% | 19.8% | 19.6% |
| Managed care | 7.5% | 11.3% | 11.7% | 7.7% | 6.6% | 6.4% | 6.2% | 5.9% | 6.2% | 5.9% |
| Medicaid | 9.0% | 13.0% | 12.2% | 10.2% | 8.3% | 8.0% | 8.1% | 7.4% | 7.5% | 6.9% |
| Other | 21.1% | 21.8% | 20.2% | 21.4% | 22.9% | 21.9% | 21.0% | 20.5% | 19.7% | 20.4% |
| Living situation | ||||||||||
| With others | 75.0% | 76.4% | 75.5% | 76.3% | 76.2% | 74.8% | 74.4% | 73.6% | 74.2% | 73.8% |
| Alone | 24.1% | 22.0% | 23.1% | 23.0% | 23.2% | 24.5% | 24.9% | 25.5% | 25.0% | 25.3% |
| Admitted from | ||||||||||
| Acute care | 94.6% | 93.3% | 94.4% | 94.5% | 94.5% | 94.6% | 94.7% | 94.9% | 95.0% | 94.8% |
| LTCF | 2.5% | 2.5% | 2.1% | 2.5% | 2.8% | 2.5% | 2.7% | 2.4% | 2.5% | 2.7% |
| Community | 1.9% | 3.1% | 2.5% | 2.1% | 1.8% | 1.8% | 1.6% | 1.7% | 1.5% | 1.3% |
| Discharge setting | ||||||||||
| Community | 76.9% | 81.3% | 80.7% | 78.1% | 77.2% | 76.5% | 75.9% | 74.5% | 74.1% | 74.2% |
| Acute care | 8.8% | 4.6% | 5.0% | 7.9% | 9.1% | 9.6% | 10.7% | 10.1% | 10.9% | 10.4% |
| LTCF | 8.7% | 9.0% | 9.1% | 8.8% | 8.3% | 8.5% | 8.0% | 9.2% | 8.8% | 8.5% |
| Rehab / subacute | 4.7% | 3.7% | 4.0% | 4.0% | 4.6% | 4.7% | 4.7% | 5.3% | 5.4% | 5.9% |
| Onset to admission, days | 19.7 (29.4) | 20.9 (30.2) | 20.5 (29.1) | 20.4 (29.5) | 20.8 (32.0) | 19.6 (29.0) | 19.5 (30.4) | 18.7 (29.2) | 18.3 (26.8) | 18.2 (26.1) |
| Length of Stay | 18.7 (16.8) | 22.7 (20.5) | 22.4 (20.9) | 19.5 (17.0) | 18.4 (15.9) | 17.9 (15.6) | 17.5 (15.2) | 17.1 (15.1) | 16.8 (14.4) | 16.6 (14.8) |
| FIM® total admission | 56.6 (22.8) | 58.6 (24.7) | 58.7 (24.3) | 57.5 (23.9) | 57.1 (23.2) | 56.5 (22.5) | 56.0 (21.9) | 55.0 (21.7) | 55.0 (21.2) | 54.8 (21.1) |
| FIM® total discharge | 87.7 (24.5) | 92.4 (24.2) | 92.1 (23.9) | 89.5 (25.0) | 87.6 (24.9) | 86.8 (24.4) | 86.3 (24.5) | 85.2 (24.3) | 84.7 (24.0) | 85.0 (24.0) |
| FIM® total change | 31.1 (19.9) | 33.8 (20.5) | 33.4 (20.0) | 31.9 (20.6) | 30.5 (20.3) | 30.3 (19.8) | 30.3 (19.7) | 30.3 (19.5) | 29.7 (19.0) | 30.2 (18.4) |
| Efficiency, change/day | 2.2 (2.0) | 2.1 (1.7) | 2.1 (1.8) | 2.2 (2.1) | 2.2 (2.1) | 2.2 (1.9) | 2.3 (2.1) | 2.3 (1.9) | 2.3 (2.1) | 2.4 (2.0) |
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. FIM total ratings include all 13 motor items across all years.
The original sample included 111,093 patients; however, 7,614 were not admitted for initial rehabilitation, 251 either died or their discharge setting was missing, 15 did not fit the desired age range, and 2,835 experienced their traumatic brain injury more than 1 year prior to rehabilitation admission. All descriptive statistics (means, standard deviations, counts, and percentages) represent unadjusted aggregate values from the remaining 101,188 patients meeting the inclusion criteria. Thus, 90% of the original sample is summarized in this report.
The text below describes summary statistics and potentially interesting trends in the data for select variables. While the contents and format of this report suggest longitudinal comparisons, caution must be used when interpreting trends. As noted in the previous section, the IRF-PAI developed for PPS contained assessment and coding changes beginning in 2002. Moreover, other PPS-related modifications have been introduced in subsequent years. Thus, some of the year-to-year differences may not reflect true changes in rehabilitation services or patient care/outcomes. Rather, these differences may be the consequence of changes in classification and/or documentation processes.17,18
Patient Characteristics
Table 1 displays total and yearly summary statistics for general characteristics of traumatic brain injury rehabilitation patients. Mean age of the entire sample was 54.2 years, but this value steadily increased from a low of 47.1 years in 2000 to a high of 59.1 years in 2008. Distributions within age-group categories show that the proportion of cases from the 75 years and older cohort nearly doubled over the 8-year study period.
Gender, marital status, and race / ethnicity demonstrated consistent patterns across all years; men consistently outnumbered women by nearly a 2-to-1 ratio, approximately 60% of patients were not married at the time of injury, and non-Hispanic white patients made up about 80% of each yearly cohort. Medicare was the most common primary payer category followed by commercial insurance; approximately 37% and 23% of the entire sample, respectively. Both Medicare and Medicare managed care programs showed distinct percentage increases in 2002 followed by continued gradual expansion through the first quarter of 2008. Conversely, commercial insurance, Medicaid, and private managed care coverage dropped precipitously in 2002 followed by further gradual declines over the remaining years of the study.
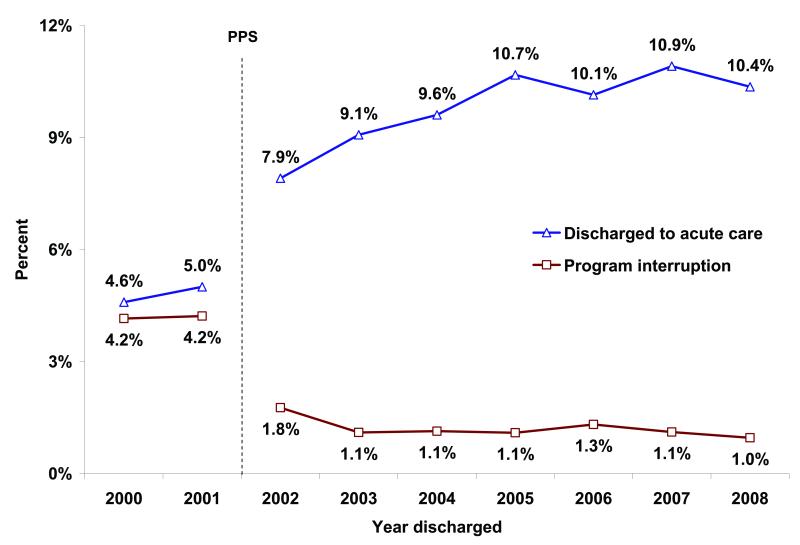
Nearly 95% of patients were admitted to inpatient rehabilitation directly from acute care and this pattern was stable across all 8 years. More than three-quarters of the entire sample was discharged to the community following rehabilitation, but this majority diminished over the 8-year study period: 81% (2000) to 74% (2008). The sudden decline in community discharges and corresponding rise in acute-care readmissions in 2002 reflect PPS-related changes in data definitions and coding as well as real changes in the percentage of patients who returned home.17 Figure 1 shows these abrupt changes in terms of discharges to acute care and program interruptions.
Figure 1.
Percentage of program interruptions* and cases discharged to acute care by discharge year.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. * In 2002 the definition for program interruption changed from ≤ 30 days to ≤ 3 days.
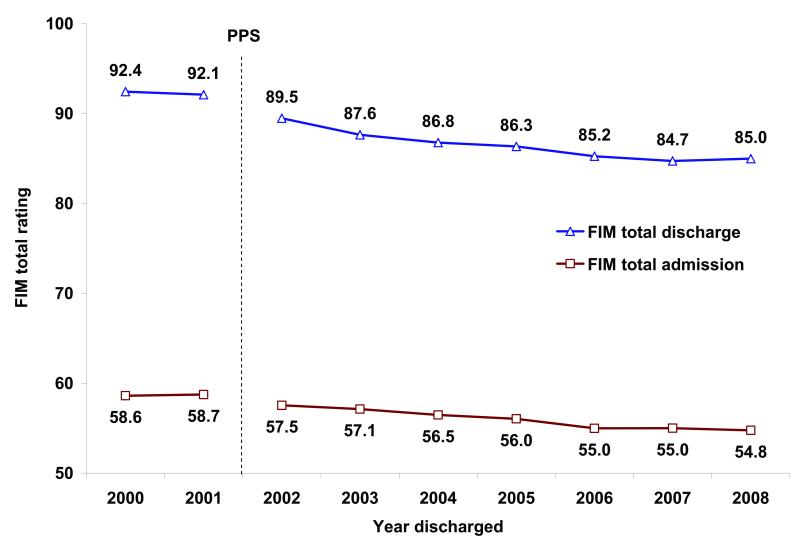
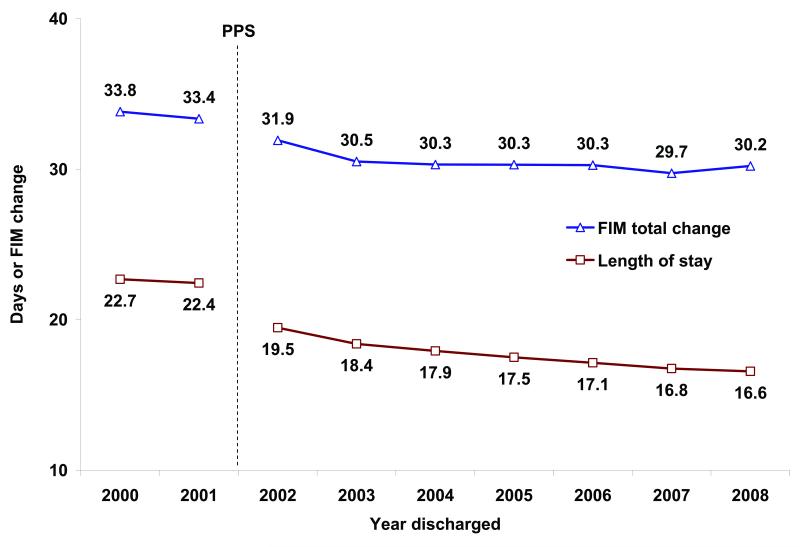
Length of Stay and Functional Status
Table 1 also provides descriptive summaries for length of stay and functional status (FIM total) at admission and discharge as well as gains in functional status. Figures 2 and 3 display the trends in these outcomes over time. Beyond the PPS-related changes from 2001 to 2002, length of stay and both FIM admission and FIM discharge ratings demonstrated gradual, yet consistent, year-to-year decreases. The three most recent cohorts (2006-2008) experienced mean lengths of stay around 17 days and demonstrated mean FIM admission and discharge ratings of approximately 55 and 85, respectively.
Figure 2.
Mean admission and discharge FIM® total ratings* by discharge year.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. * In 2002 some rules for completing the FIM instrument items were changed.
Figure 3.
Mean FIM® total change* and length of stay by discharge year.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. * In 2002 the rules for rating FIM items were modified and the procedure for coding program interruptions changed.
Table 2 shows mean admission, discharge, and change ratings for individual items within each of the 6 functional domains of the FIM. Among the 4 domains in the FIM motor subscale, items within the locomotion domain show the lowest mean ratings at both admission and discharge across all years. Regarding the 2 cognition domains, mean ratings within the social cognition domain were consistently about a half-point lower than for the communication domain.
Table 2.
Mean ratings for individual items within each FIM® subscale stratified by discharge year: mean (sd).
| Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Admission | ||||||||||
| Self-care | 3.3 (1.4) | 3.4 (1.5) | 3.4 (1.5) | 3.4 (1.5) | 3.3 (1.5) | 3.3 (1.4) | 3.2 (1.4) | 3.2 (1.4) | 3.2 (1.4) | 3.2 (1.3) |
| Sphincter | 3.5 (2.1) | 3.6 (2.2) | 3.7 (2.2) | 3.5 (2.1) | 3.5 (2.1) | 3.4 (2.0) | 3.4 (2.0) | 3.4 (2.0) | 3.4 (2.0) | 3.4 (2.0) |
| Transfer | 2.9 (1.3) | 3.0 (1.5) | 3.0 (1.5) | 3.0 (1.4) | 2.9 (1.4) | 2.9 (1.3) | 2.8 (1.3) | 2.7 (1.3) | 2.7 (1.2) | 2.7 (1.2) |
| Locomotion | 2.0 (1.3) | 2.2 (1.4) | 2.1 (1.4) | 2.1 (1.4) | 2.1 (1.3) | 2.0 (1.3) | 1.9 (1.2) | 1.9 (1.2) | 1.9 (1.2) | 1.9 (1.2) |
| Communication | 3.9 (1.8) | 3.9 (1.9) | 4.0 (1.9) | 3.9 (1.8) | 3.9 (1.8) | 3.9 (1.8) | 3.9 (1.8) | 3.8 (1.8) | 3.9 (1.7) | 3.8 (1.7) |
| Social Cognition | 3.2 (1.6) | 3.2 (1.7) | 3.2 (1.7) | 3.2 (1.7) | 3.2 (1.7) | 3.2 (1.6) | 3.2 (1.6) | 3.2 (1.6) | 3.2 (1.6) | 3.2 (1.6) |
| Discharge | ||||||||||
| Self-care | 5.1 (1.5) | 5.4 (1.5) | 5.4 (1.5) | 5.2 (1.5) | 5.1 (1.5) | 5.1 (1.5) | 5.0 (1.5) | 5.0 (1.5) | 5.0 (1.5) | 5.0 (1.5) |
| Sphincter | 5.2 (1.9) | 5.6 (1.8) | 5.7 (1.8) | 5.4 (1.9) | 5.2 (1.9) | 5.1 (1.9) | 5.1 (1.9) | 5.1 (1.9) | 5.0 (1.9) | 5.0 (1.9) |
| Transfer | 4.9 (1.5) | 5.2 (1.5) | 5.2 (1.5) | 5.0 (1.6) | 4.9 (1.6) | 4.8 (1.5) | 4.7 (1.5) | 4.6 (1.5) | 4.6 (1.5) | 4.6 (1.5) |
| Locomotion | 4.3 (1.7) | 4.6 (1.7) | 4.6 (1.7) | 4.4 (1.7) | 4.3 (1.7) | 4.2 (1.7) | 4.2 (1.8) | 4.1 (1.7) | 4.1 (1.7) | 4.1 (1.7) |
| Communication | 5.1 (1.5) | 5.2 (1.5) | 5.2 (1.5) | 5.1 (1.6) | 5.0 (1.6) | 5.0 (1.5) | 5.0 (1.5) | 5.0 (1.5) | 5.0 (1.5) | 5.0 (1.5) |
| Social Cognition | 4.4 (1.5) | 4.5 (1.5) | 4.5 (1.5) | 4.4 (1.6) | 4.4 (1.5) | 4.4 (1.5) | 4.4 (1.5) | 4.4 (1.6) | 4.4 (1.5) | 4.4 (1.6) |
| Change | ||||||||||
| Self-care | 1.8 (1.3) | 2.0 (1.3) | 2.0 (1.3) | 1.9 (1.4) | 1.8 (1.3) | 1.8 (1.3) | 1.8 (1.3) | 1.8 (1.3) | 1.8 (1.3) | 1.8 (1.2) |
| Sphincter | 1.8 (1.9) | 2.0 (2.0) | 2.0 (2.0) | 1.9 (2.0) | 1.8 (2.0) | 1.7 (1.9) | 1.7 (1.9) | 1.7 (1.9) | 1.6 (1.9) | 1.7 (1.9) |
| Transfer | 2.0 (1.3) | 2.2 (1.4) | 2.2 (1.4) | 2.1 (1.4) | 2.0 (1.4) | 2.0 (1.3) | 2.0 (1.3) | 1.9 (1.3) | 1.9 (1.3) | 1.9 (1.3) |
| Locomotion | 2.3 (1.6) | 2.4 (1.6) | 2.4 (1.5) | 2.3 (1.6) | 2.2 (1.5) | 2.2 (1.5) | 2.2 (1.5) | 2.2 (1.5) | 2.2 (1.5) | 2.2 (1.5) |
| Communication | 1.2 (1.3) | 1.3 (1.3) | 1.2 (1.3) | 1.2 (1.3) | 1.1 (1.3) | 1.1 (1.3) | 1.1 (1.3) | 1.2 (1.3) | 1.1 (1.3) | 1.1 (1.3) |
| Social Cognition | 1.2 (1.2) | 1.3 (1.2) | 1.3 (1.2) | 1.2 (1.2) | 1.2 (1.2) | 1.2 (1.2) | 1.2 (1.2) | 1.2 (1.2) | 1.1 (1.2) | 1.2 (1.2) |
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. Cell values represent mean ratings for individual FIM items within the particular subscale.
Summaries of patient age, length of stay, and functional status stratified by discharge setting (community versus institutional settings) provides unique perspective on the differential characteristics and experiences of these two groups (Table 3). In general, persons discharged to the community were younger, experienced shorter lengths of stay, and demonstrated higher functional status at admission and discharge compared to patients discharged to an institution. The community discharge group also showed greater response (functional gain and efficiency) to rehabilitative care. Table 3 also reveals that the institution discharge group experienced greater reductions in both length of stay and functional gain over the 8-year study period; with the largest drops coinciding with the introduction of the PPS. In 2000, differences in mean length of stay and FIM total gain between the two groups were approximately 8 days and 13 FIM points, respectively. By 2008, these differences were less than 2 days and nearly 15 FIM points, respectively, with the majority of these changes coming from the relatively shorter lengths of stay and smaller FIM gains within the institutional discharge group over time.
Table 3.
Patient characteristics according to discharge setting stratified by discharge year: mean (sd).
| Community Discharge |
Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, yrs |
Yes | 51.5 (23.9) | 44.9 (22.5) | 46.5 (22.7) | 48.8 (23.6) | 50.9 (24.1) | 52.3 (24.1) | 53.4 (24.0) | 55.0 (23.9) | 55.8 (23.9) | 56.5 (23.5) |
| No | 63.0 (21.9) | 56.3 (22.4) | 57.0 (22.4) | 60.0 (22.5) | 61.9 (22.3) | 63.6 (21.6) | 65.3 (21.2) | 65.6 (21.0) | 66.7 (20.5) | 66.6 (21.0) | |
| Length of stay, days |
Yes | 18.0 (15.6) | 21.1 (18.7) | 21.0 (19.5) | 18.7 (15.7) | 17.7 (14.7) | 17.4 (14.6) | 17.0 (13.9) | 16.6 (13.8) | 16.3 (13.2) | 16.1 (14.7) |
| No | 21.1 (20.2) | 29.4 (26.1) | 28.3 (25.1) | 22.2 (20.7) | 20.8 (19.3) | 19.7 (18.7) | 19.1 (18.5) | 18.8 (18.4) | 18.1 (17.3) | 17.9 (15.2) | |
| FIM® total admission |
Yes | 60.3 (22.2) | 61.9 (24.0) | 62.1 (23.7) | 61.2 (23.2) | 60.9 (22.6) | 60.1 (21.9) | 59.8 (21.3) | 58.8 (21.0) | 58.7 (20.7) | 58.5 (20.5) |
| No | 44.3 (20.3) | 44.1 (22.1) | 44.7 (21.5) | 44.3 (21.5) | 44.4 (20.8) | 44.6 (20.2) | 44.2 (19.6) | 43.9 (19.7) | 44.3 (19.2) | 44.1 (19.0) | |
| FIM® motor admission |
Yes | 41.9 (16.7) | 43.6 (18.3) | 43.5 (18.1) | 43.0 (17.6) | 42.5 (17.0) | 41.8 (16.4) | 41.3 (15.9) | 40.5 (15.7) | 40.4 (15.4) | 40.3 (15.3) |
| No | 30.0 (14.9) | 30.8 (16.9) | 30.8 (16.1) | 30.5 (15.9) | 30.2 (15.2) | 30.3 (14.7) | 29.6 (14.0) | 29.4 (14.2) | 29.6 (13.8) | 29.6 (13.7) | |
| FIM® cognition admission |
Yes | 18.4 (8.1) | 18.3 (8.2) | 18.6 (8.3) | 18.3 (8.3) | 18.4 (8.1) | 18.3 (8.1) | 18.5 (8.0) | 18.3 (8.0) | 18.3 (7.9) | 18.2 (7.9) |
| No | 14.3 (7.8) | 13.3 (7.6) | 13.9 (7.8) | 13.8 (7.8) | 14.2 (7.8) | 14.2 (7.8) | 14.6 (7.9) | 14.4 (7.8) | 14.7 (7.7) | 14.5 (7.7) | |
| FIM® total discharge |
Yes | 95.0 (18.3) | 98.1 (19.0) | 97.9 (18.6) | 96.6 (18.6) | 95.1 (18.5) | 94.3 (18.1) | 94.2 (17.8) | 93.2 (17.9) | 92.5 (17.9) | 92.5 (18.2) |
| No | 63.4 (26.7) | 67.7 (28.6) | 67.7 (28.1) | 63.9 (28.0) | 62.5 (27.3) | 62.4 (26.2) | 61.7 (26.2) | 62.0 (25.8) | 62.4 (25.2) | 63.3 (25.4) | |
| FIM® motor discharge |
Yes | 70.0 (14.6) | 72.8 (15.1) | 72.6 (14.7) | 71.7 (14.7) | 70.2 (14.7) | 69.4 (14.3) | 69.2 (14.2) | 68.3 (14.2) | 67.8 (14.3) | 67.8 (14.3) |
| No | 45.4 (21.1) | 49.7 (22.9) | 49.3 (22.2) | 46.3 (22.2) | 45.0 (21.5) | 44.7 (20.7) | 43.7 (20.5) | 44 (20.4) | 44.2 (19.8) | 45.1 (19.9) | |
| FIM® cognition discharge |
Yes | 25.0 (6.3) | 25.3 (6.3) | 25.4 (6.3) | 25.0 (6.5) | 24.9 (6.4) | 24.8 (6.3) | 25.0 (6.2) | 24.9 (6.3) | 24.7 (6.3) | 24.7 (6.5) |
| No | 17.9 (8.0) | 18.1 (8.0) | 18.4 (8.1) | 17.6 (8.1) | 17.5 (8.1) | 17.6 (7.9) | 18.0 (8.1) | 18.0 (8.0) | 18.2 (7.9) | 18.2 (7.8) | |
| FIM® total change |
Yes | 34.7 (18.4) | 36.2 (19.7) | 35.8 (19.1) | 35.4 (19.3) | 34.2 (18.9) | 34.2 (18.3) | 34.4 (17.9) | 34.4 (17.8) | 33.8 (17.3) | 34.0 (16.7) |
| No | 19.1 (19.8) | 23.6 (21.1) | 23.0 (20.6) | 19.5 (20.5) | 18.1 (20.3) | 17.8 (19.2) | 17.5 (19.6) | 18.2 (19.3) | 18.1 (18.6) | 19.2 (18.7) | |
| FIM® motor change |
Yes | 28.1 (14.6) | 29.2 (15.6) | 29.0 (15.2) | 28.7 (15.3) | 27.7 (15.0) | 27.7 (14.6) | 27.8 (14.1) | 27.8 (14.0) | 27.4 (13.8) | 27.6 (13.3) |
| No | 15.4 (15.9) | 18.9 (17.1) | 18.6 (16.6) | 15.8 (16.5) | 14.8 (16.3) | 14.4 (15.5) | 14.2 (15.6) | 14.6 (15.4) | 14.6 (14.9) | 15.4 (15.0) | |
| FIM® cognition change |
Yes | 6.6 (5.7) | 7.0 (5.8) | 6.8 (5.7) | 6.7 (5.7) | 6.5 (5.7) | 6.5 (5.6) | 6.5 (5.6) | 6.6 (5.7) | 6.4 (5.6) | 6.5 (5.6) |
| No | 3.7 (5.6) | 4.7 (5.4) | 4.5 (5.5) | 3.8 (5.7) | 3.3 (5.6) | 3.4 (5.4) | 3.4 (5.8) | 3.6 (5.7) | 3.5 (5.6) | 3.8 (5.5) | |
| Efficiency, change/day |
Yes | 2.6 (1.8) | 2.4 (1.7) | 2.4 (1.7) | 2.5 (2.0) | 2.5 (1.8) | 2.6 (1.7) | 2.7 (1.8) | 2.7 (1.7) | 2.7 (1.8) | 2.8 (1.8) |
| No | 1.1 (2.2) | 1.1 (1.4) | 1.1 (1.7) | 1.0 (2.1) | 1.0 (2.5) | 1.0 (2.0) | 1.0 (2.7) | 1.1 (2.0) | 1.2 (2.3) | 1.2 (1.9) |
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
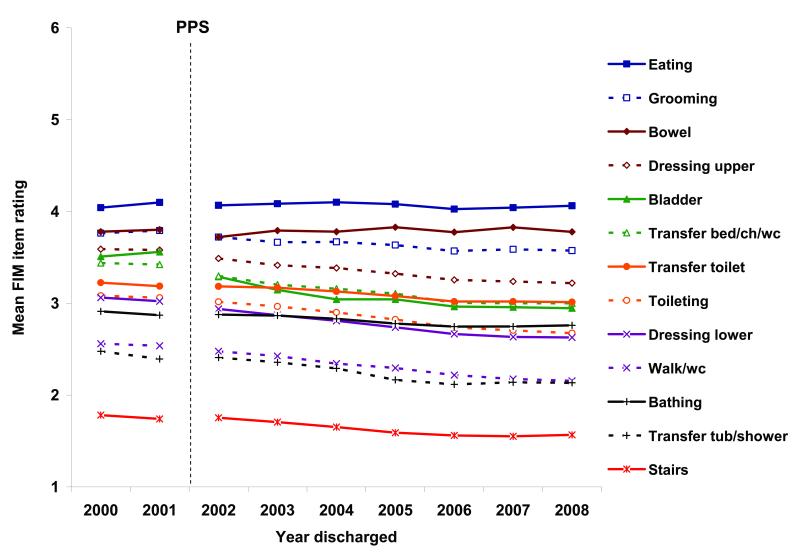
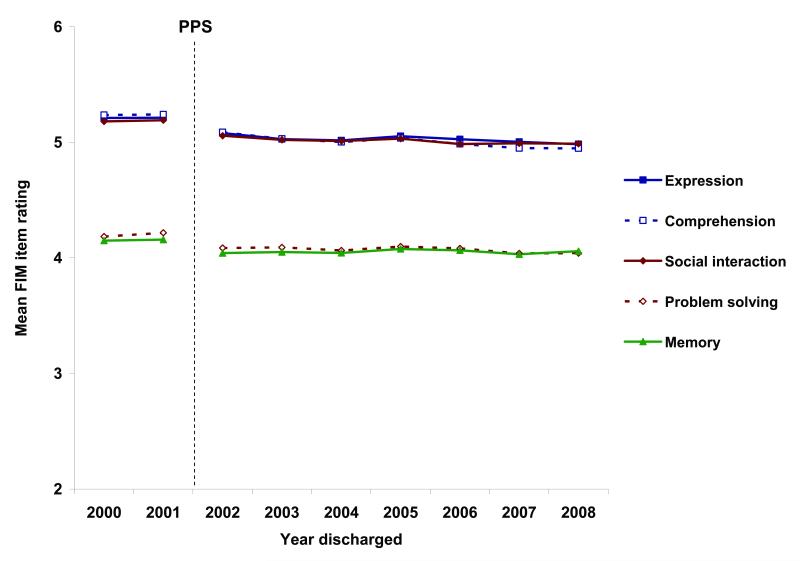
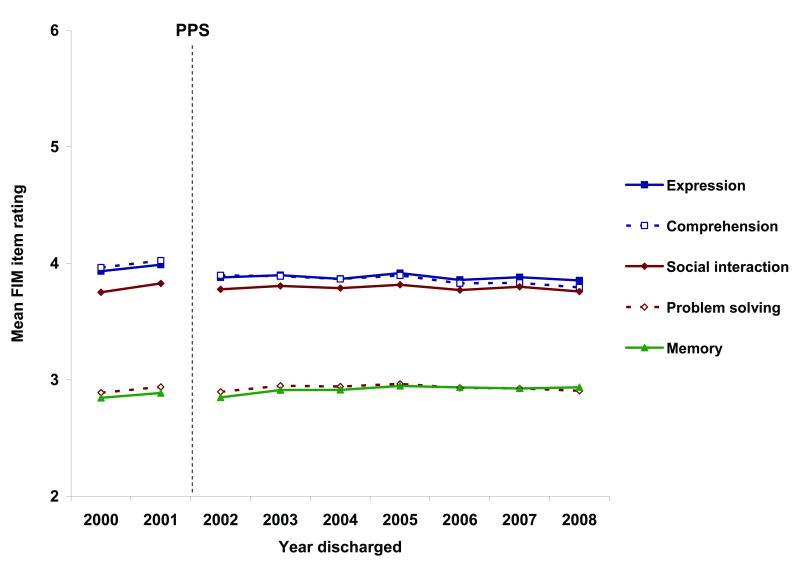
Figures 4-7 display mean ratings for all 18 FIM items. The figure legends present the hierarchies of average discharge ratings over all 8 years for the motor and cognitive subscale items. Among the 13 motor items, patients with traumatic brain injury showed the most independence in eating and grooming activities and the most difficulty with transferring from a tub or shower and climbing stairs (see Figures 4 and 5). The five cognitive items were essentially grouped into two levels of difficulty. Overall, patients were rated approximately one level higher on expression, comprehension, and social interaction activities than on problem solving and memory tasks at both admission and discharge.
Figure 4.
Mean ratings for individual FIM® motor items at admission to inpatient rehabilitation.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Figure 7.
Mean ratings for individual FIM® cognitive items at discharge from inpatient rehabilitation.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Figure 5.
Mean ratings for individual FIM® motor items at discharge from inpatient rehabilitation.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Case Severity
Case-mix Group (CMG) assignment was introduced as part of the PPS in 2002 so data are presented from that point forward (Table 4). The number of CMGs for traumatic brain injury was increased from 5 to 7 in fiscal year 2006. Prior to the expansion to 7 categories, the most severe category (CMG 0205) was the most common category assigned: greater than one-third of cases in 2002 – 2005. Following the switch to 7 categories, the more severe categories still represented a greater percentage of cases; however, CMG assignment was more evenly distributed between categories 0205 and 0207.
Table 4.
Case-mix groups (CMG)* stratified by discharge year: percentage.
| CMG | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|---|---|
| 0201 | 10.9% | 10.5% | 8.8% | 7.9% | 3.3% | 3.5% | 3.2% |
| 0202 | 9.4% | 9.5% | 10.2% | 10.9% | 5.9% | 5.2% | 5.4% |
| 0203 | 28.3% | 27.8% | 27.3% | 25.9% | 12.2% | 11.9% | 11.2% |
| 0204 | 17.3% | 17.8% | 19.4% | 20.4% | 8.7% | 8.2% | 8.5% |
| 0205 | 34.1% | 34.3% | 34.3% | 35.0% | 27.7% | 28.6% | 28.6% |
| 0206 | 13.2% | 14.2% | 14.8% | ||||
| 0207 | 29.0% | 28.5% | 28.2% |
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services.
The number of CMGs and criteria for determining them changed for fiscal year 2006.
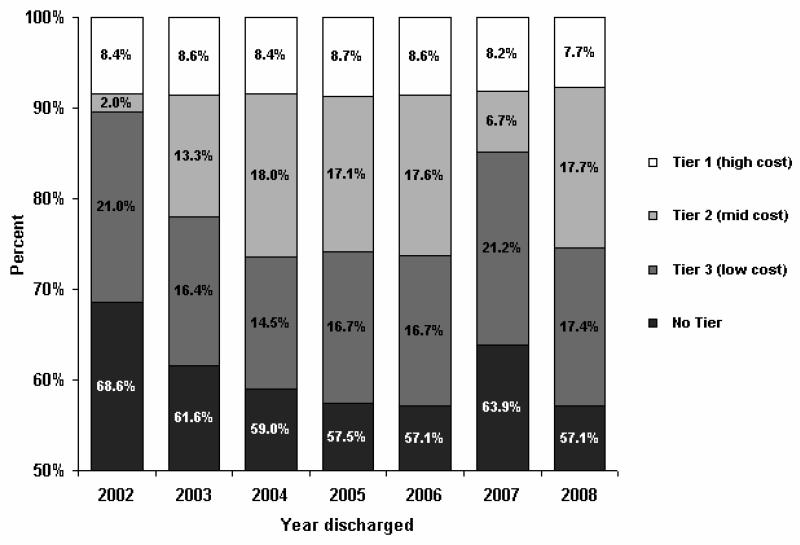
Figure 8 shows the percentages of patients assigned to each of the 4 possible CMG comorbidity tier levels. The tier criteria have been revised over the years and the Figure displays the tier structure in place for that year. Overall, more than 60% of cases were classified as non-tier. Among the 3 tier levels that affect Medicare reimbursement, tier 1 (high cost) was the least common across all years, ranging from 7.7% to 8.7%.
Figure 8.
Relative proportions of CMG comorbidity tier* assignment under the prospective payment system by discharge year.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. * The CMG comorbidity tier system changed over the years.
Deaths
Overall, less than one-quarter of one percent of patients died during their rehabilitation stay. Comparing yearly cohort mean values for those who died (Table 5) with those who survived (Table 1) reveals that patients who died were generally older and less functionally independent at admission compared to survivors. The difference in overall sample means for age was approximately 18 years and for FIM admission ratings it was approximately 21 points.
Table 5.
Characteristics of patients who died during inpatient rehabilitation by year of death: mean (sd).
| Died | Total | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|---|---|---|---|---|
| Died, N | 204 | 8 | 19 | 23 | 36 | 25 | 25 | 35 | 24 | 9 |
| Died, % | 0.20% | 0.10% | 0.15% | 0.20% | 0.32% | 0.21% | 0.19% | 0.24% | 0.17% | 0.25% |
| Age, yrs | 72.2 (18.1) | 74.6 (11.6) | 72.1 (20.8) | 65.1 (21.7) | 69.6 (18.8) | 76.2 (15.9) | 74.8 (15.7) | 73.4 (17.1) | 70.8 (19.5) | 78.4 (16.8) |
| FIM® total admission | 35.5 (18.5) | 35.4 (16.5) | 31.1 (16.3) | 34.3 (19.8) | 33.3 (16.2) | 39.1 (21.6) | 37.4 (20.5) | 35.9 (17.5) | 35.3 (20.3) | 39.9 (17.7) |
| Onset to admission, days | 20.6 (30.1) | 27.4 (27.4) | 28.4 (24.2) | 18.7 (17.8) | 17.0 (15.3) | 15.6 (20.5) | 26.8 (65.4) | 21.5 (29.8) | 20.2 (15.6) | 11.1 (6.9) |
| Length of stay, days | 12.1 (20.2) | 6.0 (4.1) | 28.3 (49.2) | 12.8 (23.5) | 12.6 (13.1) | 10.5 (9.7) | 10.4 (9.2) | 7.3 (6.1) | 11.2 (20.1) | 10.4 (5.5) |
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes. Note: % is calculated from sample with complete data, N = 101,416.
CONCLUSIONS
This report provides aggregated national summary statistics for a broad range of patient characteristics and outcomes from more than 100,000 patients with traumatic brain injury discharged from inpatient medical rehabilitation programs in 2000 through 2007. Beyond the distinct changes related to the introduction of the PPS in 2002, the data show some interesting trends over the 8-year study period. However, it is imperative to exercise caution when interpreting year-to-year comparisons as some longitudinal changes may not reflect actual variations in rehabilitative care or patient experiences. Instead, some changes may be directly related to CMS-mandated modifications in documentation, eligibility, and/or reimbursement processes implemented at different times in the PPS era. Thus, the value of this report is best described as providing year-specific benchmark information for patient characteristics and outcomes, based on the stability of the rules and regulations within a specified fiscal year.
Given the gender disparity in risk for traumatic brain injury,22 it was not surprising to see that males substantially outnumbered females in each yearly cohort. It is interesting to note, however, that the proportion of older adults, particularly those 75 years and older, within the traumatic brain injury inpatient rehabilitation population steadily increased throughout the 8-year study period. Accordingly, Medicare was the most common payer of inpatient rehabilitation services following traumatic brain injury. In recent years (2005-2008), Medicare covered more than twice as many patients as the next most common provider category, commercial insurance.
In terms of rehabilitation outcomes, both admission and discharge functional ratings displayed consistent and parallel declines over all 8 years of the study period, resulting in relatively stable FIM change in the later years. Length of stay likewise demonstrated steady year-over-year decreases. As a result, rehabilitation Efficiency (average FIM gain per day) remained stable to slightly improved over time. Nearly 3 out of 4 patients were discharged to a community setting following inpatient medical rehabilitation. The abrupt decline in the percentage of community discharges in 2002 coincided with PPS-related changes in the definition for program interruption, which resulted in more cases being classified as acute-care discharges. In subsequent years, rates of community discharge continued to show a gradual but steady downward trend. In the prior report, we offered the following reminder for utilizing these data. The UDSMR recommends that when facilities compare their own data to published benchmark information they should: 1) identify by the discharge date the period of interest using at least a full year’s data, 2) include information on all patients within the pertinent impairment group and period under review, and 3) include statistics that show patient variability such as standard deviations. More meaningful comparisons of outcomes data across settings (e.g., facility vs. national data) require case-mix adjustment. The process of adjusting the data “levels the playing field” by removing factors (i.e., impairment severity and type, patient age) other than treatment that may influence the outcome.23 Given this caveat, cross sectional comparisons within a single year using UDSMR national data should provide valuable benchmarking information for rehabilitation researchers and individual rehabilitation facilities. As noted previously, comparisons across multiple years involving pre-PPS and PPS data should be made with caution. Eventually, the research currently being conducted will allow investigators to develop algorithms to compare pre-PPS and PPS FIM instrument items in a standardized manner. Until that time, longitudinal comparisons should be made and reported with the appropriate caution. Moving forward, quality research is needed to evaluate the comprehensive, long-term healthcare needs and functional recovery of patients with traumatic brain injury. Combining information from intensive rehabilitation services with costs and outcomes data from other components across the continuum of care will provide a better understanding of the current trends in rehabilitative care and how they affect patients and their families.
Figure 6.
Mean ratings for individual FIM® cognitive items at admission to inpatient rehabilitation.
Yearly summaries represent fiscal year periods (Oct 1 through Sep 30) from the Centers for Medicare and Medicaid Services. Dashed vertical line signifies introduction of the prospective payment system (PPS), resulting in substantial changes to functional evaluation and patient management processes.
Acknowledgments
This work was funded in part by grants H133G080163 (Ottenbacher, PI) and H133F090030 (Graham) from the National Institute on Disability and Rehabilitation Research, U.S. Department of Education. The FIM® instrument is a registered trademark of the Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities, Inc.
Footnotes
Disclosures: Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Granger CV, Markello S, Graham JE, Deutsch A, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation report of patients with stroke discharged from comprehensive medical programs in 2000 through 2007. Am J Phys Med Rehabil. 2009 doi: 10.1097/PHM.0b013e3181c1ec38. (in press) [DOI] [PubMed] [Google Scholar]
- 2.Granger CV, Hamilton BB. The Uniform Data System for Medical Rehabilitation Report of First Admissions for 1990. Am J Phys Med Rehabil. 1992;71(2):108–113. [PubMed] [Google Scholar]
- 3.Granger CV, Hamilton BB. The Uniform Data System for Medical Rehabilitation report of first admissions for 1991. Am J Phys Med Rehabil. 1993;72(1):33–38. doi: 10.1097/00002060-199302000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Granger CV, Hamilton BB. The Uniform Data System for Medical Rehabilitation report of first admissions for 1992. Am J Phys Med Rehabil. 1994;73(1):51–55. [PubMed] [Google Scholar]
- 5.Granger CV, Ottenbacher KJ, Fiedler RC. The Uniform Data System for Medical Rehabilitation. Report of first admissions for 1993. Am J Phys Med Rehabil. 1995;74(1):62–66. doi: 10.1097/00002060-199501000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Fiedler RC, Granger CV, Ottenbacher KJ. The Uniform Data System for Medical Rehabilitation: report of first admissions for 1994. Am J Phys Med Rehabil. 1996;75(2):125–129. doi: 10.1097/00002060-199603000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Fiedler RC, Granger CV. Uniform data system for medical rehabilitation: report of first admissions for 1995. Am J Phys Med Rehabil. 1997;76(1):76–81. doi: 10.1097/00002060-199701000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Fiedler RC, Granger CV. Uniform data system for medical rehabilitation: report of first admissions for 1996. Am J Phys Med Rehabil. 1998;77(1):69–75. [PubMed] [Google Scholar]
- 9.Fiedler RC, Granger CV, Russell CF. Uniform Data System for Medical Rehabilitation: report of first admissions for 1997. Am J Phys Med Rehabil. 1998;77(5):444–450. doi: 10.1097/00002060-199809000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Fiedler RC, Granger CV, Post LA. The Uniform Data System for Medical Rehabilitation: report of first admissions for 1998. Am J Phys Med Rehabil. 2000;79(1):87–92. doi: 10.1097/00002060-200001000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Deutsch A, Fiedler RC, Granger CV, Russell CF. The Uniform Data System for Medical Rehabilitation report of patients discharged from comprehensive medical rehabilitation programs in 1999. Am J Phys Med Rehabil. 2002;81(2):133–142. doi: 10.1097/00002060-200202000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74(5):531–536. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 13.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 14.Segal ME, Gillard M, Schall R. Telephone and in-person proxy agreement between stroke patients and caregivers for the functional independence measure. Am J Phys Med Rehabil. 1996;75(3):208–212. doi: 10.1097/00002060-199605000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Inpatient Rehabilitation Facility Patient Assessment Instrument (IRF-PAI) Training Manual. Uniform Data System for Medical Rehabilitation; Buffalo, NY: 2001. [Google Scholar]
- 16.Carter GM, Relles DA, Ridgeway GK, Rimes CM. Measuring function for Medicare inpatient rehabilitation payment. Health Care Financ Rev. 2003;24(3):25–44. [PMC free article] [PubMed] [Google Scholar]
- 17.Deutsch A, Granger C, Russel C, Heinemann A, Ottenbacher K. Apparent changes in inpatient rehabilitation facility outcomes due to change in the definition of program interuption. Arch Phys Med Rehabil. 2008;89:2274–2277. doi: 10.1016/j.apmr.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Granger CV, Deutsch A, Russell C, Black T, Ottenbacher KJ. Modifications of the FIM instrument under the inpatient rehabilitation facility prospective payment system. Am J Phys Med Rehabil. 2007;86(11):883–892. doi: 10.1097/PHM.0b013e318152058a. [DOI] [PubMed] [Google Scholar]
- 19.UB Foundation Activities . The Inpatient Rehabilitation Facility - Patient Assessment Instrument (IRF-PAI) Training Manual. Centers for Medicare and Medicaid Services; 2004. http://www.cms.hhs.gov/InpatientRehabFacPPS/downloads/irfpaimanual040104 pdf. Available from: [Google Scholar]
- 20.Carter GM, Buchanan JL, Buntin MB, Hayden O, Paddock S, Relles DA, et al. Executive Summary of Analyses for the Initial Implementation of the Inpatient Rehabilitation Facility Prospective Payment System. Rand Corporation; Santa Monica, CA: 2002. [Google Scholar]
- 21.US Department of Health and Human Services Federal Register. 2003;Vol. 68(Num. 148):45674–45728.
- 22.Langlois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; Atlanta, GA: 2006. [Google Scholar]
- 23.Stineman MG, Maislin G, Fiedler RC, Granger CV. A prediction model for functional recovery in stroke. Stroke. 1997;28(3):550–556. doi: 10.1161/01.str.28.3.550. [DOI] [PubMed] [Google Scholar]