Abstract
Aim
We aim to determine the safety and effectiveness of a standard therapeutic package of Korean medicine for the treatment of unexplained infertility in a cross-section of women who sought treatment at an integrative hospital in Seoul, Korea.
Background
Infertility affects more than 1.2 million women in the United States alone. Treatment options for infertility vary, yet the barriers of invasiveness, cost, and access inhibit treatment use for many women. Alternative medical approaches exist for this indication, and sustain certain popularity. Therefore, we systematically studied a standard therapeutic package of Korean medicine to treat unexplained infertility in women.
Methods
Female participants included in this observational study met inclusion criteria before receiving a set of treatments including herbal medicine, acupuncture, and moxibustion. A study physician screened each patient in accordance with inclusion criteria, provided study information, and after the patients consented, performed the baseline assessment. Assessments included age, the history of assisted reproductive technology, and duration of infertility. The key outcome measure included the number who achieved pregnancy and any neo-natal morbidity and mortality at follow-up stage for those who got pregnant. Any other adverse events including aggravation of existing symptoms, and the number of dropouts, were recorded. Treatments were supposed to be completed after 6 menstrual cycles between February 2005 and April 2006.
Results
One hundred and four (104) women with unexplained infertility were included in this observational study. Participant mean age was 32 years (SD: 2.7), with a range between 26 and 41 years. The median duration of infertility after diagnosis was 33.5 weeks (interquartile range: 20.8–50.3). In total, 41 participants (39.4%) had undergone a mean number of 1.4 (SD: 2.2) assisted reproductive technology treatments prior to joining the study. The number of patients remaining in or achieving pregnancy throughout the 6-month study period was 23 (14 pregnancies), 22.1%. Six (6) participants (4.8%) reported minor adverse events including rash in the face (n = 1), diarrhea (n = 2), dizziness (n = 1), and heartburn (n = 2). Of the 14 pregnancies, there were 10 normal births, and 4 miscarriages; otherwise, no neonatal morbidity/mortality occurred. According to per protocol analysis, 14 pregnancies out of 23 total were achieved by those who remained for the entire six menstruation cycle treatments, yielding a pregnancy rate of 60.9%.
Conclusions
The standard therapeutic package for unexplained infertility in women studied here is safe for infants and the treated women, when administered by licensed professionals. While it remains challenging to have the target population complete a 6-month treatment course, during which most patients have to pay out of pocket, the extent of successfully achieved pregnancy in those who received full treatment provides meaningful outcomes, warranting further attention. A future study that includes subsidized treatment costs, encouraging the appropriate compliance rate, is warranted.
Introduction
Of the approximately 62 million American women of reproductive age in 2002, 1.2 million (2%), had an infertility-related medical appointment within the previous year, and 10% had an infertility-related medical visit at some point in the past.1 This common and frustrating medical condition can take a significant emotional and physical toll on women and their partners. The burden of infertility includes the frequent psychopathologic consequences of anxiety, depression, crisis within the relationship, divorce, and lack of self-reliance.2,3 Because of such negative consequences, it is desirable to find cost-effective and successful therapies for infertility.
Typical Western treatments for infertility include medication (hormone stimulation), surgical correction of anatomical defects, or artificial insemination. For couples who do not benefit from these treatments, the remaining options include gamete intrafallopian transfer, intracytoplasmic sperm injection, in vitro fertilization, and zygote intrafallopian transfer. Although all of these therapies can be successful, they are often expensive, invasive, and time consuming. With the introduction and integration of Eastern medicine into Western practices, there has been an increase in the acceptance and use of complementary practices in dealing with infertility.4,5 The anxiety and depression that are often associated with infertility has made alternative and combination therapies a realistic and beneficial option for those faced with varied types of infertility. Any noninvasive, non-time-consuming, and cost-effective manner of alternative therapies can also be viewed as a patient benefit. The now common use of acupuncture has proven effective for endocrine stimulatory and regulatory interventions.6
While conventional treatment options are well established, there have been few systematic reviews of CAM approaches for the treatment of infertility.7 Several studies have reported the use of acupuncture as a treatment for various gynecologic conditions,8 while others have reported case studies on the use of Traditional Chinese Medicine (including herbs and acupuncture) for treating infertility.9,10 While the proponents of these therapies value their safety, minimally invasive approaches, and minimal side-effects, there have not been thorough reviews or studies to assess the effectiveness of traditional approaches for treating infertility. Bridging the gap in knowledge and practice between Western and Eastern medicine as well as looking at how medicine is practiced in under studied medical systems11 are important issues in the fertility field.
In South Korea, where the traditional system of medicine has evolved into an integrative approach, a significant population of infertile patients seeks health services from clinics and hospitals of Korean medicine. Medicine in Korea, while it has evolved with influence from and exchange with Traditional Chinese Medicine, has developed and sustained various unique aspects. This is the rationale to use the term, Korean medicine. The Conmaul Hospital (Seoul, Korea) is well known as an infertility specialty clinic, where an integrated service between Medical Doctor (M.D.) and Korean Medicine Doctor (K.M.D.)12 is provided. The scope of its service includes diagnosis and treatment packages including herbs, moxibustion, and acupuncture. This study is a prospective observational study of the integrative care package provided to treat specifically “unexplained female infertility.” Herein we describe the participation, outcomes, and any adverse events related to this integrative care package. This population either has few established conventional treatment options, or has experienced a substantial number of failures from the prior use of conventional treatments.
Methods
This study evaluates the outcome of 104 women who received treatment using a standard therapeutic package for unexplained infertility at Conmaul Hospital in Seoul, Korea. All participants were treated for six menstrual cycles between February 2005 and April 2006. The women received treatment with a standard therapeutic package of Korean Herbal Medicine, acupuncture, and moxibustion for their unexplained infertility. Treatment was cumulative and not contingent upon use of the standard therapeutic package in consecutive months. Those study participants who missed three consecutive monthly treatments were contacted by a physician to determine the reason for discontinuation.
Inclusion criteria for study participation included all of the following: unexplained infertility confirmed with laparoscopy and ultrasonography, regular menstrual cycle of 25–35 days, no infertility factor in their male partner, clear communication skills with hospital researchers, and normal hormonal test result range. If all of the inclusion criteria were verified within the 12 months prior to initiation of participation, women were included. Women were excluded from the study when the inclusion criteria were not met, or if hormone supplementation (including clomiphene citrate13), in vitro fertilization or intrauterine insemination treatments were undertaken during the 6-month study period. Those women with minimal/mild endometriosis were included in the study, as were women over the age of 35 (age typically classified as the cutoff for high-risk pregnancies to develop).
Standard therapeutic package intervention
A study physician screened each patient in accordance with inclusion criteria, provided study information, and after obtaining consent, completed a baseline assessment. After screening, women were subjected to the standard therapeutic package for unexplained infertility for up to six menstruation cycles and ceased treatment when conception was confirmed with ultrasonography. This package included (1) water-extracted decoction (120 mL) of herbal prescription prepared through individual diagnosis given three times a day 30 minutes after meals; (2) a pack of Song Keum Dan taken with warm water 30 minutes before meals 3 times daily. This herbal medicine pill, referred to in Dong-Yi-Bo-Gam, an encyclopedia-style Korean medical text published in 1659, contains 214 mg of dried powder of Paeonia moutan, Angelica tenuissima, Panax ginseng, Angelica sinensis, Poria cocos, Angelica dahurica, Cinnamomum cassia, Marsdenia longipes, Cnidium officinale, Corydalis ternata, Paeonia albifloria, and Atractylodes japonica; and 107 mg of dried powder of Glycyrrhiza glabra and Achyranthes japonica per each pack; (3) moxibustion on umbilicus (CV8) done once daily except during the menstrual cycle; and (4) herb acupuncture (injection of extracted solution of dried Cervi Parvum Cornu and Hominis Placenta onto acupuncture points, at each point 0.3 mL containing 0.06 mg of the two herbs) on mainly CV4, BL19, and BL22. All women who achieved pregnancy during the observational period were followed up until birth.
Outcome measures
The baseline data included age, the history of assisted reproductive technology, and duration of infertility. The key outcome measure was the number of participants achieving pregnancy. Patients were also asked to inform the study physician whether they complied with the standard therapeutic package, and whether they have attempted to conceive, and to report the aggravation of any existing symptoms. Also, the number of dropouts and adverse events in the patient population were recorded.
The study protocol included the collection of details on menstruation period and related symptoms including length of menstrual cycle, the color of menstrual blood on the second or third day of menstruation using the Munsell color system, the amount of menstrual blood per day of significant bleeding during the total menstrual period, the number of pads used, and the existence of blood clots observed with the naked eye (score 0 if no clot, 1 with the diameter <1 cm, and 2 with the diameter ≥1 cm). A visual analogue scale of menstrual pain, breast pain, and breast swelling was also asked. All of the above data were to be used as indicators of reproductive health status in the patient base, including infertility and ovulation. However, these data were not analyzed due to the lack of compliance on the part of patients.
The assessment forms for each participant were given a unique identifier number and kept in a locked filing cabinet. All data analysis was done offsite at Harvard Medical School, Boston, and was securely maintained. The study IDs for each participant were maintained such that participant anonymity was never compromised. Approval for this primary study was obtained from the Institutional Review Board at Conmaul Hospital, and the data analysis of the de-identified data was approved by the Harvard Medical School Institutional Review Board. After the completion of data analysis and the drafting of the manuscript, the Principal Investigator (J.P.) moved to the University of North Carolina at Chapel Hill and finalized the manuscript.
Results
One hundred and four (104) women with unexplained infertility were included in this observational study. Their mean age was 32 years old (SD: 2.7), ranging between 26 and 41. The median duration of infertility after diagnosis was 33.5 weeks (interquartile range: 20.8–50.3). In total, 41 participants (39.4%) had undergone a mean number of 1.4 (SD: 2.2) assisted reproductive technology treatment attempts prior to joining the study.
The flow of the study is shown in Figure 1. The number of patients remaining in or achieving pregnancy throughout the entire study period of 6 months was 23 (14 pregnancies), or 22.1%. Slightly more than half (n = 55) dropped out before reporting their third menstruation cycle. The trend of dropout was high in the early stage and gradually decreased. Out of 14 pregnancies, there were 10 normal births, 4 miscarriages, and no stillbirth. Otherwise, there was no neonatal morbidity/mortality. Total monthly cost for the treatment package was about $500.
FIG. 1.
Flow of an outcome study of an infertility clinic of Korean Medicine for unexplained women's infertility.
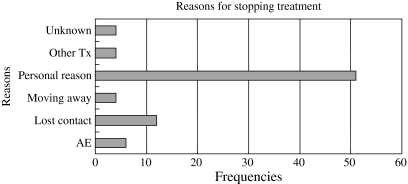
Six (6) participants (5.8%) reported minor adverse events including rash in the face (n = 1), diarrhea (n = 2), dizziness (n = 1), and heartburn (n = 2). All of the symptoms were mild, and eased after patients stopped taking the specific herbal medicine; no hospitalization was required. Figure 2 shows reasons stated for individual dropouts. The most frequently cited reason was “personal reasons,” which may be a polite way of expressing difficulty or unwillingness to afford this treatment ($500/month).
FIG. 2.
Reasons for dropouts from an outcome study of an infertility clinic of Korean Medicine for unexplained women's infertility. Tx, treatment; AE, adverse events.
Regarding the success rate for achievement of pregnancy, 14 of 23 patients remained in the study for six menstrual cycles achieving a pregnancy rate of 60.9%. This success rate must be considered in light of the high dropout rate for participants in this study.
Discussion
The use of acupuncture, moxibustion, and herbal medicine has deep roots in women's health in Korea. In this study, we attempted to record the results of such practices pertaining to unexplained female infertility. The use of the standard therapeutic package used in this study is safe and minimally, if at all, risky. The absence of teratogenic or reported neonatal morbidity and mortality solidifies the place of such treatment packages alongside other established medical, natural, and self-administered (drug) infertility interventions. The adherent group of women achieved a successful pregnancy outcome at a rate of 60.9%. Upon assuring appropriate compliance rates (through insurance support, availability of services, positive outcomes reported in the literature, etc.), a promising outcome can be anticipated. Meanwhile, the patients' full comprehension regarding scope of treatment and willingness to comply with it when entering into the course of treatment seems crucial, as the high number of dropouts in the early study stages adversely affected the overall study.
The outcomes that were obtained in the group that completed the study as well as those that dropped out are significant. Although the success for achieving pregnancy is downplayed by the number of dropouts in the study, if more than 22.1% of the initial subject group had followed through until the end, the outcomes might have provided a strong call for the implementation of noninvasive Eastern medical practices to be more than an adjuvant therapy for infertility. Although completion rates for observational studies on infertility may range as high as 90% in studies that involve a stipend,14 it is our understanding that our completion rate of 22.1% in an observational study (which should be markedly less than any designed cohort or case–control study) that asked for a capitation payment from the subjects was acceptable. In contrast to studies where treatments were provided free of charge, in this observational study participants had to pay for their individual treatment. The personal reasons for dropping out could also include unreported illness, emotional or psychologic burden, and loss of interest, which the investigators regret we did not classify in detail. The movement of patients out of the area as well as the desire to seek other treatment options, and administrative issues in contacting participants accounted for the remainder of patients who did not complete the treatment course.
It is important to understand the complex array of effects that play into the seeking out of and adherence to treatment in regard to fertility. In the realm of unexplained in fertility, especially where patients have no pointed abnormality with hormone levels, or physical impediments that have been diagnosed, the emotional and psychologic toll is overarching. To achieve success and completion with the standard package of care in this difficult situation is promising. One interesting point to interpret in future study results will be to look at the demographic composition of women who did complete the treatment. As such a large percentage of dropouts stated that “personal reasons” were the impetus for lack of completion, it brings forth the question, why did personal reasons not get in the way of adherence for those women who completed treatment? Is this group older and therefore more prone to follow through without regard to time constraints or economic detriment? Is this group more inclined to participate in this traditional and noninvasive type of care in other aspects of their lives? Or simply, does this group live closer or have substantial economic means to achieve the final outcome of visiting for a combined six menstrual periods? In addition, are women in this group more desperate for conception than the others?
As we look at previous studies of traditional care for infertility, there is insufficient literature looking at Korean medical practices and their influence on infertility. Much of the current literature on traditional medicine and infertility deals with male infertility, includes the use of medical procedures in conjunction to Eastern medicine,7 or comes from Indian or Chinese researchers who use similar but decisively different methods from those of this study. These alternatives include the use of numerous similar yet different herbs, but exclude the use of acupuncture and herbal pills. Therefore, research in this area is to an extent novel and in its own right a worthwhile endeavor.
The use of traditional Korean medicine has become very appealing to patients as a primary or adjuvant therapeutic tool. The mixed results reported by many researchers in regard to fertility-related outcomes can be explained by the standardization of treatments and therefore lack of personalized care plans.15,16 While further discussion of the individual treatments included in the package is beyond the scope of this study, there may certainly be a benefit to this method of treatment.
This observational study into unexplained infertility treatment would further benefit from work done in the following aspects: (1) investigating the outcomes of consecutive treatment in contrast to a cumulative treatment over a number of months on the success of pregnancy and other symptoms of menstruation; (2) studying detailed categories of reasons for the discontinuation of treatments, including cost and confidence in the treatment; (3) carrying out matched comparative studies on women with unexplained infertility who did not use the standard therapeutic package from Conmaul Hospital versus women who did (introduction of a specific control); (4) investigating outcomes of the standard care package for this unexplained infertility in regard to general health and wellness. What other benefits or detriments can be associated with the package, as most herbal therapeutic packages have extensive effects; (5) looking at distinct groups of women younger than and older than 35, the age commonly designated as when pregnancies become high risk, and the possible difference in treatment outcomes; and (6) performing a similar study with free treatment. Through looking at women who are not self-selected based upon access to hospital care (through economic and motivational means), a better understanding of the population-level effectiveness of CAM fertility package therapy as a whole could be understood.
Upon completion of this study, the limitations of an observational study in the Conmaul Hospital were typified by the relatively low adherence rate of participants. At the same time, the success rate of the standard therapeutic package for treatment of unexplained infertility was strengthened. Overall, whether or not pregnancy was achieved, and whether or not participants finished treatment, or infertility persisted, the multiple psychologic and physiologic problems associated with unexplained infertility were studied and provided a baseline for future research on this meaningful complementary subject field.
In summary, this study is a starting point for future research. Although a large percentage dropped out of the study for myriad nonspecified reasons, the treatment for infertility was beneficial in the small cohort who utilized it as prescribed. Therefore, future research into the mechanisms of action for individual treatment components, the cost effectiveness of the treatment versus conventional infertility methods, and the overall success rate in a double-blind placebo-controlled study, could act to solidify this treatment method as a positive option for women with unexplained infertility.
Acknowledgments
Jongbae Park and Bonghyun Nam acknowledge the grant provided to the Harvard Medical School by the Myung Kyung Medical Foundation (account number #520-45578-225011). Ted J. Kaptchuk was supported by NIH-NCCAM grant #K24 AT004095. In addition, the assistance of Stephen Flaherty in manuscript preparation is sincerely appreciated.
Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control and Prevention. Assisted Reproductive Technology. http://www.cdc.gov/ART/ [Jun 16;2008 ]. http://www.cdc.gov/ART/
- 2.Fassino S. Garzaro L. Peris C, et al. Temperament and character in couples with fertility disorders: A double-blind, controlled study. Fertil Steril. 2002;77:1233. doi: 10.1016/s0015-0282(02)03115-1. [DOI] [PubMed] [Google Scholar]
- 3.Fassino S. Piero A. Boggio S, et al. Anxiety, depression and anger suppression in infertile couples: A controlled study. Hum Reprod. 2002;17:2986–2994. doi: 10.1093/humrep/17.11.2986. [DOI] [PubMed] [Google Scholar]
- 4.Beal MW. Women's use of complementary and alternative therapies in reproductive health care. J Nurse-Midwifery. 1998;43:224–234. doi: 10.1016/s0091-2182(98)00009-3. [DOI] [PubMed] [Google Scholar]
- 5.Stankiewicz M. Smith C. Alvino H. Norman R. The use of complementary medicine and therapies by patients attending a reproductive medicine unit in South Australia: A prospective survey. Aust N Z J Obstet Gynaecol. 2007;47:145–149. doi: 10.1111/j.1479-828X.2007.00702.x. [DOI] [PubMed] [Google Scholar]
- 6.Dong C. Chen SR. Jiang J, et al. Clinical observation and study of mechanisms of needle-picking therapy for primary infertility of abnormal sperm. Chin Acupuncture Moxibustion. 2006;26:389–391. [PubMed] [Google Scholar]
- 7.Manheimer E. Zhang G. Udoff L, et al. Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: Systematic review and meta-analysis. BMJ Clin Res Ed. 2008;336:545–549. doi: 10.1136/bmj.39471.430451.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang R. Chung P. Rosenwaks Z. Role of acupuncture in the treatment of female infertility. Fertil Steril. 2002;78:1149–1153. doi: 10.1016/s0015-0282(02)04348-0. [DOI] [PubMed] [Google Scholar]
- 9.Stone JA. Yoder KK. Case EA. Delivery of a full-term pregnancy after TCM treatment in a previously infertile patient diagnosed with polycystic ovary syndrome. Altern Ther Health Med. 2009;15:50–52. [PubMed] [Google Scholar]
- 10.Du Y. Zhao Y. Ma Y, et al. Clinical observation on treatment of 2,062 cases of immune infertility with integration of traditional Chinese medicine and western medicine. J Tradit Chin Med. 2005;25:278–281. [PubMed] [Google Scholar]
- 11.van Balen F. Visser AP. Perspectives of reproductive health. Patient Educ Counseling. 1997;31:1–5. doi: 10.1016/s0738-3991(97)01015-x. [DOI] [PubMed] [Google Scholar]
- 12.Stevens L. Duarte H. Park J. Promising implications for integrative medicine for back pain: A profile of a Korean hospital. J Altern Complement Med. 2007;13:481–484. doi: 10.1089/acm.2007.6263. [DOI] [PubMed] [Google Scholar]
- 13.Costello MF. Emerson S. Miranda T, et al. Case series case series of a single centre's treatment of ovulatory infertility with clomiphene citrate and intrauterine insemination in 2002. Aust N Z J Obstet Gynaecol. 2004;44:156–159. doi: 10.1111/j.1479-828X.2004.00191.x. [DOI] [PubMed] [Google Scholar]
- 14.Hakim R. Gray R. Zacur H. Infertility and early pregnancy loss. Am J Obstet Gynecol. 1995;172:1510–1517. doi: 10.1016/0002-9378(95)90489-1. [DOI] [PubMed] [Google Scholar]
- 15.Anderson BJ. Rosenthal L. Acupuncture and IVF controversies. Fertil Steril. 2007;87:1000. doi: 10.1016/j.fertnstert.2007.01.137. [DOI] [PubMed] [Google Scholar]
- 16.Stener-Victorin E. Humaidan P. Use of acupuncture in female infertility and a summary of recent acupuncture studies related to embryo transfer. Acupunct Med. 2006;24:157–163. doi: 10.1136/aim.24.4.157. [DOI] [PubMed] [Google Scholar]