Abstract
Background:
There are limited data on the effectiveness of organized stroke care in different ischemic stroke subtypes in the real-world setting. We analyzed the effect of organized stroke care in all stroke subtypes in a longitudinal cohort study using data from the Registry of the Canadian Stroke Network.
Methods:
Between July 2003 and September 2007, there were 6,223 consecutive patients with ischemic stroke subtype information by Trial of Org 10172 in Acute Stroke Treatment criteria. Subtypes were categorized as large artery atherosclerotic disease, lacunar, cardioembolic, or other. The amount of organized stroke care was quantified using the previously published organized care index (OCI), graded 0-3 based on the presence or absence of occupational therapy or physiotherapy, stroke team assessment, and admission to a stroke unit.
Results:
Mortality at 30 days was associated with both stroke subtype and OCI. Higher OCI (defined as score 2-3 compared to 0-1) was strongly associated with lower odds of 30-day mortality in each ischemic stroke subtype (adjusted odds ratio estimates ranged from 0.16 to 0.43, p < 0.001, controlling for age, gender, stroke severity, and medical comorbidities by logistic regression). These estimates were essentially unchanged after excluding patients treated with palliative care. Numbers needed to treat, to prevent 1 death at 30 days, ranged from 4 to 9 across the subtypes.
Conclusions:
A strong association between higher OCI and lower 30-day mortality was apparent in each ischemic stroke subtype. These data suggest that organized stroke care should be provided to stroke patients regardless of stroke subtype.
GLOSSARY
- aOR
= adjusted odds ratio;
- CI
= confidence interval;
- OCI
= organized care index;
- RCSN
= registry of the Canadian Stroke Network.
Stroke unit care is one of the most effective interventions to reduce mortality and morbidity following acute stroke.1,2 Stroke unit care is often assumed to be widely applicable across patient groups. However, the subtypes of ischemic stroke have widely different underlying causes, risk factors, and prognoses.3,4 It is therefore far from clear whether the effect of stroke unit care is the same across the ischemic stroke subtypes. For example, it has been hypothesized, based on limited data,5 that patients with lacunar stroke may benefit less from acute stroke care, because of milder stroke severity, lower mortality, and lower rate of early recurrence compared to nonlacunar stroke. Defining the relative benefits of stroke unit care in different stroke subtypes could allow a rational allocation of resources to those who are most likely to benefit.
One of the limitations of research on stroke unit care has been the varying definition of a stroke unit.1 Stroke units may consist of some combination of a geographically defined unit with skilled nursing care, access to physician specialists with expertise in stroke, and evaluation by therapists with stroke experience. Not all elements may be present in each hospital with a stroke unit, particularly in the setting of real-world clinical practice outside the context of prospective clinical research. To overcome this limitation, we have previously created an organized care index (OCI) as a scale of the amount of specialized stroke care, and shown that higher OCI is associated with better outcomes following ischemic stroke.6
In this study, we hypothesized that higher levels of organized stroke care, as measured by the OCI, would be associated with lower mortality across all ischemic stroke subtypes. We tested this hypothesis in the registry of the Canadian Stroke Network (RCSN), a hospital-based prospective cohort study of consecutive patients with acute ischemic stroke that was designed to provide information on stroke-related care and stroke outcomes in the real-world setting.
METHODS
Subject population and study measurements.
The methods of the RCSN have been previously published.7 For the present study, we used data from phase 3 of the RCSN, and included all consecutive patients with acute ischemic stroke seen at 12 Ontario stroke centers between July 1, 2003, and September 30, 2007, with documented ischemic stroke subtype information. Median hospital bed size was 396.5 beds (interquartile range 290.5-442.5 beds). Eight of the hospitals had a stroke unit in place during the entire study period, while 2 hospitals established stroke units in 2004 and the remaining 2 established stroke units in 2005.
Detailed clinical data were collected by chart abstraction performed during and after the hospital admission by trained neurology research nurses using custom software. The medical care for each patient was determined at the discretion of each patient's physician. Hospitals were aware of the data being collected but had no beforehand knowledge of the study hypotheses tested here. The presence of stroke units was verified by on-site audit. Stroke severity was assessed on admission using the Canadian Neurological Scale; in this scale, higher scores indicate lower severity.8,9 Ischemic stroke subtype was assigned, according to the Trial of Org 10172 in Acute Stroke Treatment criteria,10 by the study coordinator based on documentation by the treating physician and the investigations recorded in the chart. For the purpose of this analysis we analyzed ischemic stroke subtype as the following categories: cardioembolic, large artery atherosclerosis, lacunar, or other (including both other determined causes of stroke as well as undetermined causes). Palliative care was defined as a physician's order in the chart to provide comfort care only rather than active medical management. Prior studies have shown excellent agreement for the abstracted data elements, with kappa scores of >0.8 for key variables, including stoke subtype.11 To capture all-cause mortality after stroke, both during and after hospitalization, the RCSN database was linked to the Ontario Registered Persons Database.7
The OCI was used to categorize exposure to various stroke services, as in our previous study.6 The OCI is a summary score for each individual patient that assigns 1 point for receipt of each of the following services: 1) occupational therapy or physiotherapy, 2) stroke team assessment, and 3) admission to a stroke unit. A score of zero indicates that stroke patients received none of these services, and higher scores indicate access to more services. A stroke team was defined as a multidisciplinary group of stroke specialists including physicians, nurses, occupational therapists, physiotherapists, and speech language pathologists. Assessment by any of these allied health professionals was recorded in the RCSN as a visit at any point during the hospitalization. A previous study found that receipt of physical therapy and occupational therapy were moderately correlated, but there was little correlation between stroke team assessment, stroke unit admission, and physical therapy or occupational therapy.6
Standard protocols, registrations, and patient consents.
The RCSN is prescribed under Ontario's Personal Health Information Protection Act, and patient data are collected without consent for the purpose of facilitating the provision of stroke care in the province of Ontario. The overall project is approved by the Research Ethics Board of Sunnybrook Health Sciences Centre as well as the Research Ethics Board of each participating stroke center. The design of the current study was approved by the Ethics Review Boards at St. Michael's Hospital and Sunnybrook Health Sciences Centre, as well as by the RCSN publications committee.
Statistical analysis.
First, we examined the relationship between OCI category and 30-day mortality, stratified by ischemic stroke subtype. Mortality was chosen as the primary outcome because the study does not include assessments of postdischarge functional status. χ2 tests were used to compare categorical variables; analysis of variance or Kruskal-Wallis tests were used to compare mean and median differences for continuous variables in baseline characteristics. Age was categorized as <60, 60-79, and ≥80 years, and stroke severity on admission was categorized as mild (Canadian Neurological Scale ≥8), moderate (Canadian Neurological Scale 5-7), or severe (Canadian Neurological Scale ≤4) on the basis of previous studies. We used the Charlson-Deyo index to quantify the number of medical comorbidities for each patient, based on the presence or absence of 17 medical conditions12; a score of zero indicates that no comorbidities are present, and higher scores indicate a greater burden of comorbidity.13 The Charlson-Deyo index was categorized as 0, 1-2, or ≥3 for the purpose of analysis, as in our previous study.14 Multivariable logistic regression models were used to determine the association between OCI and mortality, with adjustment for age, sex, Charlson-Deyo index score, and Canadian Neurological Scale score. The OCI was categorized as high (OCI 2-3) or low (OCI 0-1) for incorporation as a predictor in the regression model and to calculate effect sizes including risk ratios and absolute risk differences. We used ischemic stroke subtype-by-OCI interaction terms to determine whether the effect of OCI on 30-day mortality was significantly different between ischemic stroke subtypes.
As some patients with very severe strokes may be treated with a palliative approach, and be both less likely to receive organized care and more likely to die following stroke, secondary analyses excluded patients where the RCSN database indicated that they were treated with a palliative approach during their stroke hospitalization.
Statistical analysis was performed using SAS statistical software version 9.1.3 (SAS Institute Inc.; Cary, NC). All tests were 2-tailed, and p values <0.05 were considered significant.
RESULTS
During the study period, there were 6,965 consecutive eligible patients with an ischemic stroke and ischemic stroke subtype information. We excluded 568 (8.2%) without a valid unique health care identifier number and 174 repeat admissions for stroke for the same patient (2.5%). Therefore there were 6,223 patients for analysis. There were 3,215 consecutive unique patient admissions that could not be analyzed because ischemic stroke subtype was not recorded in the chart (representing 34.0% of all ischemic stroke admissions).
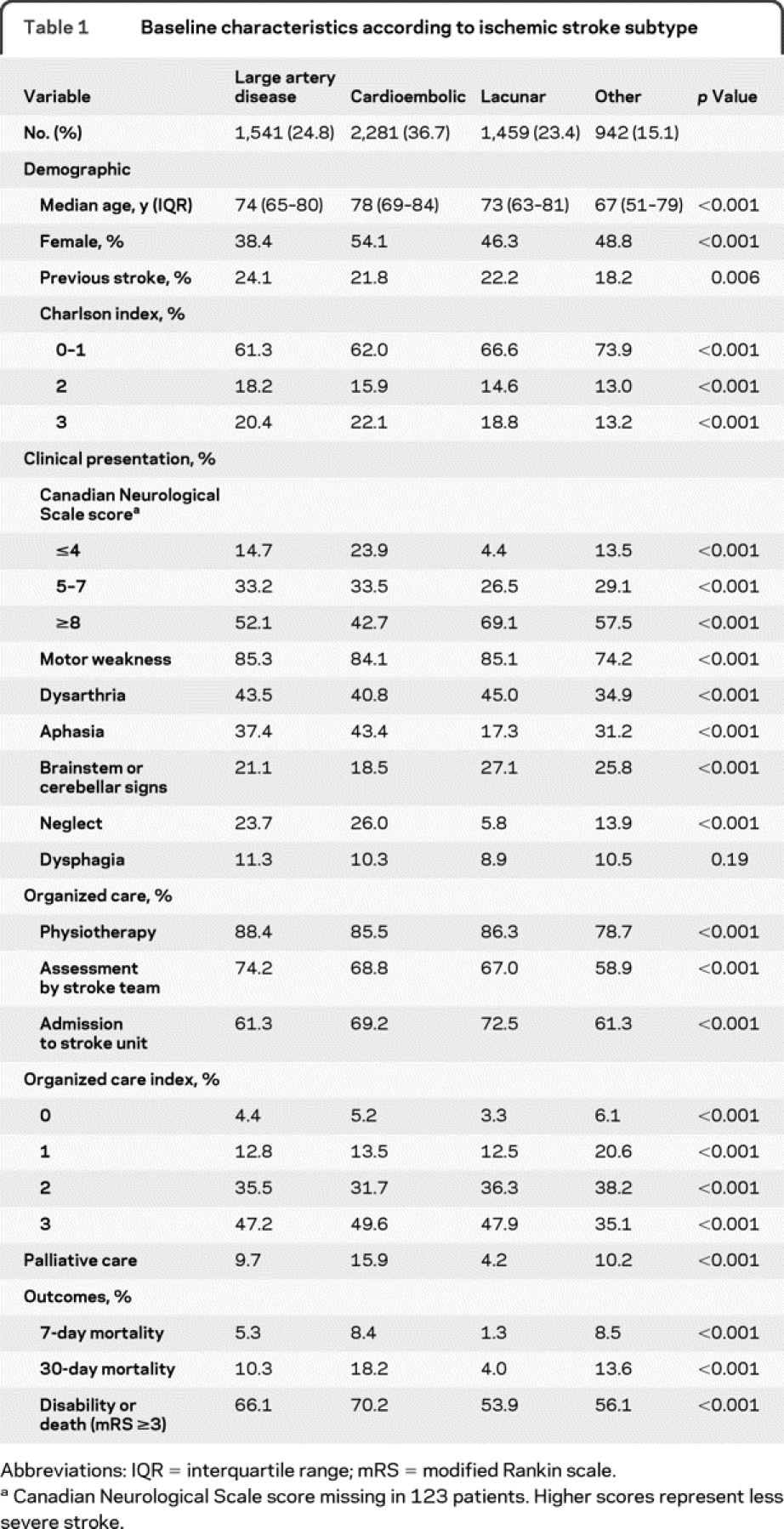
Characteristics of the study population, according to ischemic stroke subtype, are shown in table 1. Significant differences across subtypes were seen for many characteristics, partly reflecting the large size of the database. Cardioembolic stroke was most common; patients with cardioembolic stroke were older, had higher stroke severity, had higher mortality and more poststroke disability, and were more likely to be treated with palliation. Patients with lacunar stroke or other stroke (including both determined and undetermined causes) had lower initial stroke severity and better outcomes. Patients with large artery atherosclerosis had intermediate outcomes, and were more likely to be male. Patients with other causes of stroke had lower OCI; otherwise, the distribution of OCI was similar among the subtypes.
Table 1 Baseline characteristics according to ischemic stroke subtype
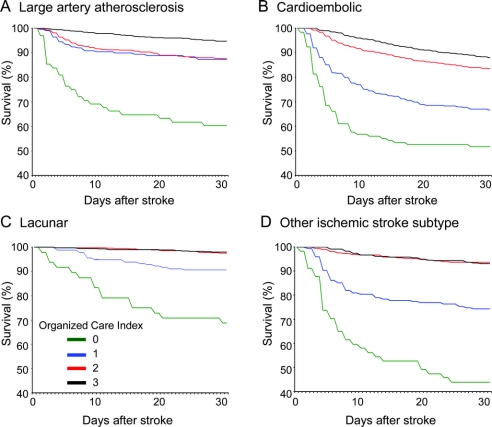
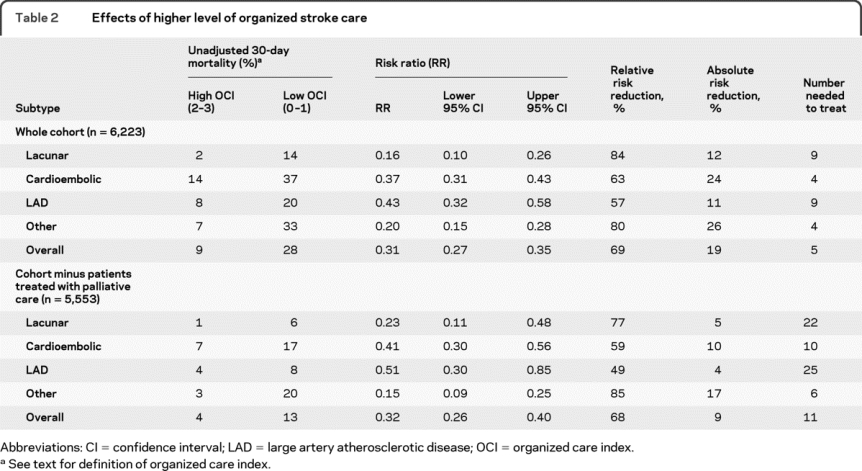
A strong graded relationship between OCI category and the rate of death by 30 days was seen in each ischemic stroke subtype (figure e-1 on the Neurology® Web site at www.neurology.org). Likewise, Kaplan-Meier curves showed the same graded relationship between OCI category and cumulative survival following stroke, with the greatest separation of the curves occurring in the first 10-15 days poststroke (figure 1). The effects of high OCI (2-3) compared to low OCI (0-1), calculated as risk ratios, relative risk reductions, absolute risk differences, and numbers needed to treat, are shown in table 2. In a sensitivity analysis excluding patients treated with palliative care, essentially similar relative risk reductions for mortality were seen (table 2). As expected, the corresponding absolute risk reductions for higher OCI were lower following the exclusion of patients treated with palliative care, because of the overall lower mortality (table 2).
Figure 1 Survival after ischemic stroke according to organized care index level
See text for definition of organized care index. (A) Large artery atherosclerosis, (B) cardioembolic, (C) lacunar, (D) other ischemic stroke subtype. For all survival curves, p < 0.001 by Wilcoxon log-rank test. Organized care index levels: 0 = green, 1 = blue, 2 = red, 3 = black.
Table 2 Effects of higher level of organized stroke care
The multivariable-adjusted independent predictors of 30-day mortality are shown in table 3. OCI and ischemic stroke subtype were both independent predictors of mortality in the overall cohort. Higher OCI was associated with a lower adjusted odds ratio (aOR) for mortality (aOR 0.23, 95% confidence interval [CI] 0.19-0.28); exclusion of the 670 patients with palliative care had only a small effect on the estimate (aOR 0.28, excluding palliative care patients). Higher OCI was a strong predictor of lower 30-day mortality in each ischemic stroke subtype, adjusting for other covariates (table 4). Only relatively small differences were seen between the univariate and multivariable-adjusted ORs (tables 3 and 4). The reduction in mortality was slightly lower in patients with large artery stroke (aOR 0.34) compared to lacunar stroke (aOR 0.16, p = 0.04) or other stroke (aOR 0.17, p = 0.02) (table 4).
Table 3 Multivariable-adjusted independent predictors of 30-day mortality
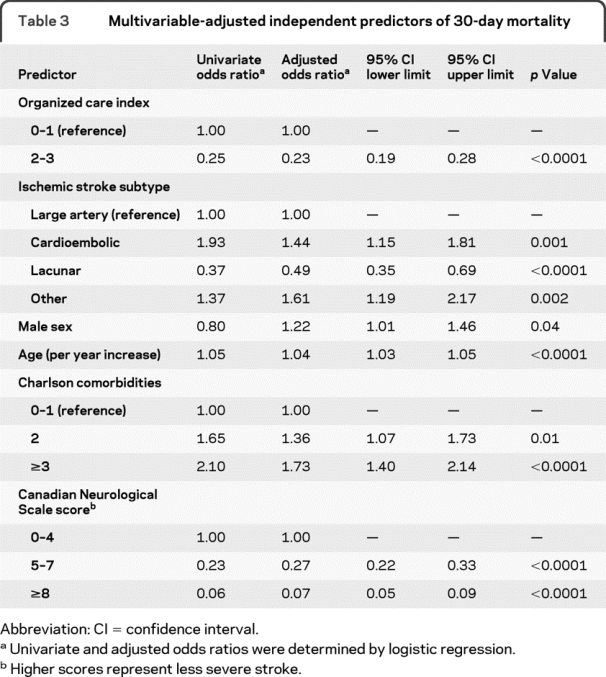
Table 4 Multivariable-adjusted relationships between higher organized care index and 30-day mortality in each ischemic stroke subtype
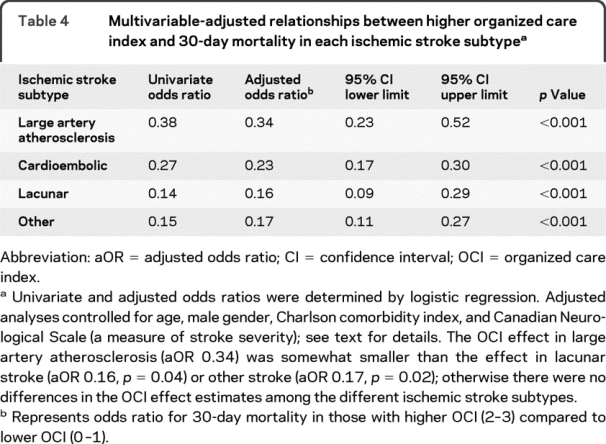
To assess for selection bias we compared patients with ischemic stroke subtype information (n = 6,223) to patients where ischemic stroke subtype was not recorded in the chart (n = 3,215). Patients without ischemic stroke subtype recorded, compared to those with ischemic stroke subtype recorded, were slightly older (72.8 vs 71.9 years), had more medical comorbidities (Charlson-Deyo index ≥3 in 21.6% vs 19.6%), had higher stroke severity (Canadian Neurological Scale score 0-4 in 17.7% vs 15.5%), were more likely to be treated with palliative care (15.0% vs 10.8%), were less likely to receive higher levels of organized care (OCI 2-3 in 74.0% vs 81.1%), and had higher 30-day mortality (16.1% vs 12.2%) (p < 0.05 for all comparisons). The relationship between higher OCI and mortality was very similar in those with missing ischemic stroke subtype information (aOR 0.24, 95% CI 0.19-0.30) compared to those where ischemic stroke subtype was present (table 4), however.
DISCUSSION
Prior literature, including studies of the RCSN, shows that stroke unit care is associated with better outcomes following stroke.1,6,14 Here, we show in a real-world setting that increasing level of organized stroke care is strongly associated with decreased mortality in each of the main ischemic stroke subtypes. In this study, we analyzed escalating levels of organized stroke care as using the OCI, as in previous studies,6 rather than dichotomize stroke unit care into present or absent, an imprecise task given expected variability in the composition of stroke units across hospitals. OCI levels from 0 to 3 were assigned to each patient based on the presence or absence of occupational therapy or physiotherapy, stroke team assessment, or admission to a geographically defined stroke ward. By doing this we were able to show that increasing levels of OCI were associated with graded decreases in stroke mortality across each of the ischemic stroke subtypes. The effect of higher OCI on mortality was independent of other predictors of mortality, and was also seen in sensitivity analyses excluding patients treated with palliative care, who would be less likely to receive intensive care or rehabilitative services. The effect of OCI was somewhat weaker in the large artery group. Even so, the effect of higher OCI on mortality in patients with large artery disease was strong and highly statistically significant, with the odds of 30-day mortality more than halved compared to those with lower OCI.
The strong association between higher OCI and lower mortality in each ischemic stroke subtype was seen despite large differences among the subtypes in age, sex, initial stroke severity, and stroke signs. Consistent with other reports, we found that cardioembolic stroke was associated with older age and higher mortality, while lacunar stroke was associated with lower mortality.4,15,16 Not surprisingly, lacunar stroke patients had fewer cortical signs, such as aphasia and neglect, than other stroke patients. The fact that strong associations between higher OCI and lower mortality were observed in each subtype, despite these differences, suggests that the effect of organized stroke care is not limited to a narrow range of age, stroke severity, or stroke symptoms.
Few previous studies have attempted to determine whether the effect of organized stroke care is affected by ischemic stroke subtype, because most previous studies have not collected stroke subtype information, particularly in the real-world setting outside the context of clinical trials. A post hoc analysis of a randomized trial of comprehensive stroke unit care, comparing comprehensive stroke unit care to general medical ward care with specialist stroke team support, found that stroke unit care reduced 30-day mortality in patients with nonlacunar stroke (n = 164) but not in patients with lacunar stroke (n = 103).5 In the lacunar stroke group, mortality at 30 days was 1/49 in those with stroke unit care, compared to 1/54 in those with stroke team consultation only. This contrasts with our finding of substantially reduced 30-day mortality in lacunar stroke patients with higher OCI compared to lower OCI (aOR 0.16, 95% CI 0.09-0.29, p < 0.001). It is clear that the low number of lacunar stroke patients and mortality events gave little power to detect the effect of organized stroke care in the randomized trial, however. In fact, in the randomized trial there was a trend toward greater 1-year survival in lacunar stroke patients randomized to comprehensive stroke unit care (odds ratio 2.8, 95% CI 0.8-59, p = 0.07).5 Additional differences between the trial population and our study population are that the randomized trial only enrolled patients with moderately severe stroke, not mild or severe stroke, and that all the trial patients received some form of organized care (because the control arm included stroke specialist consultation), whereas our study of organized care in clinical practice included all stroke severities and included patients who received no organized care. In light of our findings, we suggest that lacunar stroke patients be provided organized stroke care, pending additional larger adequately powered randomized trials to prove or disprove the effect of organized stroke care in this subgroup.
There are some limitations to this analysis. We do not have information on the cause of mortality. Longer-term outcomes were not analyzed and warrant further study. We did not analyze the impact of individual medical treatments that may have differed between patients with higher or lower OCI; therefore we cannot determine all of the mechanisms by which higher OCI might lead to lower mortality. Further research will be needed to investigate the mechanisms by which organized stroke care improves outcomes. A substantial number of patients did not have ischemic stroke subtype information recorded in the chart (34.0%) and there were differences between those with and without ischemic stroke subtype information, although some of the differences were fairly small. This raises the possibility of selection bias, although the magnitude of this bias may be relatively small because the relationship between higher OCI and lower mortality was very similar in those with or without ischemic stroke subtype information. The possibility of residual confounding of our results cannot be completely excluded because this was an observational study, not a randomized trial. Although we controlled for confounding by regression, there remains the possibility that unmeasured confounders could explain some of the relationship between OCI and mortality. We considered whether the relationship between higher OCI and lower mortality could be explained by decreased provision of organized stroke care to patients with severe stroke, or advanced age, which were deemed to have a poor prognosis. The association of higher OCI with lower mortality remained robust and consistent when adjusting for age and stroke severity, however. Additionally, we found that the results were similar when excluding patients treated with palliation.
Our finding, that organized stroke care is associated with lower mortality in each of the ischemic stroke subtypes, has important implications for the organization of stroke systems of care. Access to organized stroke care is limited in many health care systems because of scarce financial or physical resources, or geographic disparities in resources.17 In this context, determining which patients are likely to benefit most from organized care, and which patients are not likely to benefit at all, could be important for patient selection for more intensive stroke-related services. Based on these data, patient selection for organized stroke care based on ischemic stroke subtype does not seem warranted. Our data suggest that all ischemic stroke subtypes benefit from organized care, including mild lacunar strokes and severe cardioembolic strokes.
COINVESTIGATORS
The Investigators of the Canadian Stroke Registry are as follows: Frank Silver, MD, FRCPC (Coordinating Centre at the Institute for Clinical Evaluative Sciences [ICES], Toronto); Moira Kapral, MD, MSc, FRCPC (ICES); Jack Tu, MD, MSc, PhD, FRCPC (ICES); R. Hall, BASc, MSc, PhD (ICES); J. Richards, RN (ICES); Annette Robertson, RN, RDCS (ICES); Neville Bayer, MD (St. Michael's Hospital, Site Principal Investigator); Sandra Black, MD (Sunnybrook & Women's College Health Sciences Centre, Site Principal Investigator); Donald Brunet, MD (Kingston General Hospital, Site Principal Investigator); Vladimir Hachinski, MD (London Health Sciences Centre, Site Principal Investigator); David Howse, MD (Thunder Bay Regional Health Sciences Centre, Site Principal Investigator); John Maher, MD (Royal Victoria Hospital, Site Principal Investigator); Wieslaw Oczkowski, MD (Hamilton Health Science Centre, Site Principal Investigator); Stephen Phillips, MD (Queen Elizabeth II Health Sciences Centre, Site Principal Investigator); Dan Selchen, MD (Trillium Health Centre, Site Principal Investigator); Mukul Sharma, BSc, MD, FRCPC, MSc (The Ottawa Hospital, Site Principal Investigator); Frank Silver, MD (University Health Network/Toronto Western Hospital, Site Principal Investigator); Peter Zalan, MD (Hôpital Régional de Sudbury Regional Hospital, Site Principal Investigator). The Stroke Outcome Research Canada (SORCan) Working Group members are as follows: Gustavo Saposnik, MD, MSc, BCN (Arg), FAHA (Project Leader, University of Toronto); Sandra E. Black, MD, FRCPC (University of Toronto); Robert Côté, MD (McGill University); Shelagh B. Coutts, BSc, MBChB, MD, FRCPC, FRCP (Glasg) (University of Calgary); Andrew M. Demchuk, MD, FRCPC (University of Calgary); David J. Gladstone, MD, PhD, FRCPC (University of Toronto); Vladimir Hachinski, MD, FRCPC, MSc, DSc, Hon Dr Med (University of Western Ontario); Antoine Hakim, OC, MD, PhD, FRCPC (Ottawa University); Michael D. Hill, MD, MSc, FRCPC (University of Calgary); Thomas Jeerakathil, BSc, MSc, MD, FRCPC (University of Alberta); Moira K. Kapral, MD, MSc, FRCPC (University of Toronto); Muhammad Mamdani, PharmD, MA, MPH (University of Toronto); Martin O'Donnell, MB, PhD, MRCPI (McMaster University); Stephen J. Phillips, BSc (Hons), MBBS, FRCPC (Dalhousie University); Frank L. Silver, MD, FRCPC (University of Toronto); Eric Smith, MD, MPH, FRCPC (University of Calgary).
DISCLOSURE
Dr. Smith has received speaker honoraria from the Canadian Consortium on Dementia; serves on speakers' bureaus for QuantiaMD and BMJ Best Practice; and has received/receives research support from the NIH (5R01NS062028 [PI] and K23NS046327 [PI]), the CIHR, the Canadian Stroke Network, and the Hotchkiss Brain Institute. Dr. Hassan and Dr. Fang report no disclosures. Dr. Selchen serves on scientific advisory boards for Teva Pharmaceutical Industries Ltd., Novartis, Biogen Idec, Merck Serono, and Bayer Schering Pharma; and has received speaker honoraria from Sanofi-Aventis, Bristol-Myers Squibb, Teva Pharmaceutical Industries Ltd., and Biogen Idec. Dr. Kapral serves on the editorial board of Stroke and receives research support from the CIHR, the Canadian Stroke Network, and the University Health Network Women's Health Program. Dr. Saposnik receives research support from the Ontario Stroke System, the SE Toronto Stroke Program, the Heart and Stroke Foundation Ontario, CIHR, the Department of Research at St. Michael's Hospital, and Connaught Foundation (University of Toronto).
Supplementary Material
Address correspondence and reprint requests to Dr. Eric E. Smith, Foothills Medical Centre, Room C1212, 1403 29th Street NW Calgary, AB, Canada T2N 2T9 eesmith@ucalgary.ca
Supplemental data at www.neurology.org
e-Pub ahead of print on June 30, 2010, at www.neurology.org.
Study funding: The Registry of the Canadian Stroke Network is funded by the Canadian Stroke Network and the Ontario Ministry of Health and Long-Term Care. The Institute for Clinical Evaluative Sciences is funded by the Ontario Ministry of Health and Long-Term Care. The investigators acted as the sponsors of the study. None of the supporting agencies had input into the design, access to the data, analyses, interpretation, or publication of the study.
Disclosure: Author disclosures are provided at the end of the article.
Received January 23, 2010. Accepted in final form April 9, 2010.
REFERENCES
- 1.Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2007:CD000197. [DOI] [PubMed]
- 2.Stroke Unit Trialists Collaboration. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke 1997;28:2139–2144. [DOI] [PubMed] [Google Scholar]
- 3.Sacco RL. Risk factors, outcomes, and stroke subtypes for ischemic stroke. Neurology 1997;49(5 suppl 4):S39–S44. [DOI] [PubMed] [Google Scholar]
- 4.Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke 2001;32:2735–2740. [DOI] [PubMed] [Google Scholar]
- 5.Evans A, Harraf F, Donaldson N, Kalra L. Randomized controlled study of stroke unit care versus stroke team care in different stroke subtypes. Stroke 2002;33:449–455. [DOI] [PubMed] [Google Scholar]
- 6.Saposnik G, Fang J, O'Donnell M, Hachinski V, Kapral MK, Hill MD. Escalating levels of access to in-hospital care and stroke mortality. Stroke 2008;39:2522–2530. [DOI] [PubMed] [Google Scholar]
- 7.Kapral MK, Laupacis A, Phillips SJ, et al. Stroke care delivery in institutions participating in the Registry of the Canadian Stroke Network. Stroke 2004;35:1756–1762. [DOI] [PubMed] [Google Scholar]
- 8.Cote R, Battista RN, Wolfson C, Boucher J, Adam J, Hachinski V. The Canadian Neurological Scale: validation and reliability assessment. Neurology 1989;39:638–643. [DOI] [PubMed] [Google Scholar]
- 9.Bushnell CD, Johnston DC, Goldstein LB. Retrospective assessment of initial stroke severity: comparison of the NIH Stroke Scale and the Canadian Neurological Scale. Stroke 2001;32:656–660. [DOI] [PubMed] [Google Scholar]
- 10.Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial: TOAST: Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35–41. [DOI] [PubMed] [Google Scholar]
- 11.Kapral MK, Silver FL, Richards JA, et al. Registry of the Canadian Stroke Network: Progress Report 2001-2005. Toronto: Institute of Clinical Evaluative Sciences; 2005. [Google Scholar]
- 12.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613–619. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein LB, Samsa GP, Matchar DB, Horner RD. Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke 2004;35:1941–1945. [DOI] [PubMed] [Google Scholar]
- 14.Saposnik G, Kapral MK, Coutts SB, Fang J, Demchuk AM, Hill MD, on behalf of the Investigators of the Registry of the Canadian Stroke Network (RCSN) for the Stroke Outcome Research Canada (SORCan) working group. Do all age groups benefit from organized inpatient stroke care? Stroke 2009;40:3321–3327. [DOI] [PubMed] [Google Scholar]
- 15.Petty GW, Brown RD Jr, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of incidence and risk factors. Stroke 1999;30:2513–2516. [DOI] [PubMed] [Google Scholar]
- 16.Petty GW, Brown RD Jr, Whisnant JP, Sicks JD, O'Fallon WM, Wiebers DO. Ischemic stroke subtypes: a population-based study of functional outcome, survival, and recurrence. Stroke 2000;31:1062–1068. [DOI] [PubMed] [Google Scholar]
- 17.Mayor S. Stroke care is improving in England but not in Wales, audit shows. BMJ 2007;334:969. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.