Abstract
Pharmacotherapy and psychotherapy are generally effective treatments for major depressive disorder (MDD); however, research suggests that patient preferences may influence outcomes. We examined the effects of treatment preference on attrition, therapeutic alliance, and change in depressive severity in a longitudinal randomized clinical trial comparing pharmacotherapy and psychotherapy. Prior to randomization, 106 individuals with MDD reported whether they preferred psychotherapy, antidepressant medication, or had no preference. A mismatch between preferred and actual treatment was associated with greater likelihood of attrition, fewer expected visits attended, and a less positive working alliance at session 2. There was a significant indirect effect of preference match on depression outcomes, primarily via effects of attendance. These findings highlight the importance of addressing patient preferences, particularly in regard to patient engagement, in the treatment of MDD.
Keywords: patient preferences, depression treatment, working alliance, attrition, indirect effects, multiple mediation
Major depressive disorder (MDD) remains a significant public health problem worldwide. Clinical research suggests that the use of pharmacotherapy and psychotherapy, both singly and in combination, are efficacious treatments for depression (see Hollon, Thase, & Markowitz, 2002). However, it is widely recognized that the efficacy of treatments for depression in clinical practice is limited by multiple factors, including premature dropout and non-adherence (e.g., Keller, Hirschfeld, Demyttenaere, & Baldwin, 2002; Melfi, Chawla, Croghan, Hanna, Kennedy, & Sredl, 1998). The preferences of patients for a given type of treatment for depression may influence their willingness to start treatment, complete treatment, and engage fully in the course of treatment (Corrigan & Salzer, 2003; Raue & Schulberg, 2007). Patient preference has been identified as a predictor of randomized trial recruitment (King et al., 2005) and attrition, with typically small effects on primary outcomes (Preference Collaborative Review Group, 2008), in randomized trials across clinical domains.
Studies examining patient preference as a predictor of outcome in randomized clinical trials (RCT) for the treatment of depression have provided equivocal evidence regarding the hypothesis that patient preferences directly affect clinical outcomes, with various studies reporting no relationship between preference and outcome (Dobscha, Corson, & Gerrity, 2007), small, inconsistent, non-significant relationships (Leykin, DeRubeis, Gallop, Amsterdam, Shelton, & Hollon, 2007), or significant effects (Kocsis et al., 2009). However, as suggested by TenHave and colleagues (2003), it is possible that preference matching may not have a robust effect on changes in severity of depression, but may have indirect benefits such as enhanced engagement with treatment protocols and better therapeutic relationships.
There appears to be some support for this indirect effect. Relationships between patient predilections for a specific depression treatment and early attrition and engagement in therapy have been demonstrated (Elkin, Yamaguchi, Arnkoff, Glass, Sotsky, & Krupnick, 1999). Iacoviello and colleagues (2007) determined that lack of congruence between patients’ treatment preference and actual treatment was associated with decreasing therapeutic alliance over time, but only for those initially preferring psychotherapy over medication. Qualitative data show that those who drop out from psychotherapy cite a mismatch with the therapeutic approach as a reason for their decision (Wilson & Sperlinger, 2004).
Given the limited and at times equivocal findings, greater clarity of the relationship between preference and key clinical outcomes such as dropout, alliance, and clinical improvement is needed. Previous studies typically have not examined the relationship between preference and multiple direct (i.e., clinical improvement) and indirect (alliance, attendance, dropout) outcomes. A further limitation of previous studies is a lack of concrete assessment of preferences. For example, treatment attrition is often equated with non-preference, but explicit measurement of preference prior to the initiation of treatment often has not been carried out.
The current study builds on prior research by assessing preferences directly and examining multiple indirect and direct outcomes in the context of a large randomized clinical trial (RCT). This RCT compared two psychotherapies (behavioral activation and cognitive therapy) and pharmacotherapy (paroxetine plus clinical management) in a placebo controlled trial for adults with MDD. Specifically, we examined the role of patient preferences in predicting willingness to start treatment, treatment completion, development of a positive working alliance, and improvement in depressive severity over the course of acute treatment. We further examined whether there were significant indirect effects of preference match on changes in depression via attendance and early alliance. We hypothesized: 1) compared to those randomized to their non-preferred treatment, those randomized to their preferred treatment would be more likely to demonstrate acceptance of the intervention as defined by being more likely to a) start treatment, b) attend more sessions, and c) to complete treatment; 2) compared to those randomized to their non-preferred treatment, those randomized to their preferred treatment would have higher early ratings of alliance with their clinician; and 3) there would be a significant indirect effect of preference match on depression outcomes via attendance and early alliance.
Method
Participants
The University of Washington Institutional Review Board approved the protocol.1 All participants provided written informed consent prior to participation. Details regarding recruitment, eligibility criteria and screening are available elsewhere (Dimidjian et al., 2006). For the current study, the final sample consisted of the 106 individuals who completed a treatment preference questionnaire. See Table 1 for sample characteristics.
Table 1.
Sample Characteristics
| Sample means/frequencies | |
|---|---|
| (N = 106) | |
| Age: M (SD) | 38.4 (11.7) |
| Gender: N (%) | |
| Female | 68 (64.2) |
| Race: N (%) | |
| White | 84 (79.2) |
| Black/African American | 4 (3.8) |
| Hispanic/Latino(a) | 7 (6.6) |
| Other | 11 (10.3) |
| Relationship status: N (%) | |
| Never married | 46 (43.4) |
| Married | 24 (22.6) |
| Separated/Divorced | 24 (22.6) |
| Living with partner | 11 (10.4) |
| Widowed | 1 (.9) |
| Highest education achieved: N (%) | |
| Some high school | 2 (1.9) |
| High school degree | 36 (34.0) |
| College degree | 50 (47.2) |
| Graduate degree | 17 (16.0) |
| Income level: N (%) | |
| < 10000 | 13 (12.3) |
| 10-19999 | 8 (7.5) |
| 20-29999 | 18 (17.0) |
| 30-39999 | 20 (18.9) |
| 40-49999 | 12 (11.3) |
| ≥50,000 | 33 (31.1) |
Procedures
Participants were randomly assigned to condition according to a computer generated randomization list: psychotherapy [behavioral activation (BA) or cognitive therapy (CT)], antidepressant medication (ADM; paroxetine), or pill placebo. The placebo group was only included in the analysis of who started treatment vs. withdrew following randomization, as we were primarily interested in the relationship between preference and active treatments. Participants completed a baseline questionnaire prior to randomization that included an assessment of treatment preferences. Participants completed standard outcome assessments at baseline, mid-, and post-treatment (approximately 8 and 16 weeks), and at nonstandard time points as clinically indicated (e.g., early termination). Participants and clinicians also completed a measure of working alliance at Session 2 and at 4, 8, and 16 weeks after beginning therapy. For the purposes of this study, only the Session 2 ratings of the working alliance are included, as we were particularly interested in the effects of preference on alliance formation and later alliance ratings may be influenced by many factors, including symptomatic improvement (e.g., Feeley, DeRubeis, & Gelfand, 1999).
Measures and Criteria
Depression severity measures
Depressive severity was assessed at pre-, mid-, and post-treatment with the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) and a modified 17-item Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). The BDI-II is a widely used self-report measure of depression and is psychometrically sound (Beck et al., 1996). The HRSD is a widely used interviewer-administered measure of depression and has been shown to be valid and reliable (Williams, 1988).
Treatment preferences
Preferences were assessed using the Expectations for Treatment Inventory (ETI; e.g., Leykin et al., 2007). At intake, participants reported whether they preferred “pharmacotherapy,” “talking therapy,” or had “no preference.” They also reported whether they expected pharmacotherapy or talking therapy to be more effective in treating their depression, or if they did not expect one to be any more effective than the other.
Therapeutic alliance
The therapeutic alliance between patient and therapist was assessed using a short form of the Working Alliance Inventory (WAI; Horvath & Greenberg, 1989). The short form of the WAI is a 12-item scale with three subscales, each with four items, for task, bond, and goal alliance. A total composite score represents overall alliance, with higher scores indicating greater perceived alliance (client: α = .93; therapist: α = .96).
Refusal of Randomization
Those who terminated after being informed of their random assignment and prior to attending a single session were defined as “refusing randomization.” These participants are only included in the analysis of randomization refusal.
Study Attrition
Participants were categorized according to whether or not they completed the study. Study completion was defined as attendance at the final expected treatment session.
Session attendance
Session attendance was calculated as percent of allowable sessions attended. The maximal number of expected sessions varied by treatment condition. The protocol allowed 10 sessions for ADM and 24 for psychotherapy.
Treatments
CT was provided in a manner consistent with standard CT for depression, including an integration of behavioral and cognitive strategies (Beck, Rush, Shaw, & Emery, 1979; Beck, 1995). BA was provided as an expanded version of the behavioral interventions described by Beck et al. (1979) and consistent with Martell, Addis, and Jacobson (2001). Participants in BA or CT were seen up to 24 sessions over a 16 week period, with visits largely occurring twice a week for the first 8 weeks and once weekly after that point. The ADM condition followed the clinical management protocol developed for the TDCRP, modified for use with an SSRI (Fawcett, Epstein, Fiester, Elkin, & Autry, 1987). Participants in ADM were seen weekly for the first 4 weeks, and then biweekly through 16 weeks (with those in the placebo condition terminating at 8 weeks). All therapists were trained and supervised by experienced study personnel (see Dimidjian et al., 2006, for more details).
Analysis Overview
The General Linear Model procedure was used for continuous outcomes and Binary Logistic Regression for dichotomous outcomes, using contrast codes for the preference variable. Individuals matched with their preferred treatment condition were coded +1. Those mismatched were coded −1, and those who had no preference were coded 0. Polynomial contrasts were specified in the GLM procedure. This allowed us to maximize power by utilizing all participants, including those who reported no preference. The linear contrasts compared means for the matched vs. the mismatched groups, ignoring the no-preference group, while quadratic contrasts compared means for the no-preference group to the preference groups. Where cell sizes permit, we examined interactions between experimental condition and preference to determine if the effect of preference on the dependent variables varied based on whether a patient received psychotherapy or ADM. Multilevel modeling was used to examine the direct effect of preference on changes in HRSD and BDI scores over time.
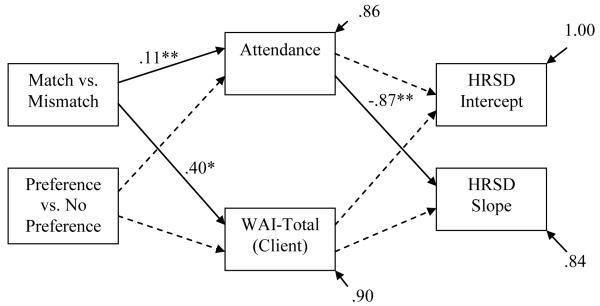
Indirect effects of preference match on changes in HRSD scores were estimated using a path analysis in AMOS 17.0, in which attendance and WAI-total scores were specified as mediators of the effect of preference match on depression. Two orthogonal contrast codes for preference match were specified as exogenous variables, one for the contrast of match vs. mismatch and one for the contrast of preference vs. no preference. Within-subject intercepts and slopes for changes in HRSD scores were calculated using individual regression models, and used as outcome variables. The model tested included direct paths from the preference codes to alliance and attendance, and from these mediators to HRSD slopes and intercepts. Following the recommendations of Preacher and Hayes (2008) for multiple mediator models, we performed a bootstrapping analysis, using 1000 samples and bias-corrected confidence intervals.
Results
Treatment Preferences
On the ETI, 51 participants (48.1%) preferred psychotherapy, 19 (17.9%) preferred ADM, and 36 (34.0%) expressed no preference.
Intervention Acceptance
Refusing Randomization
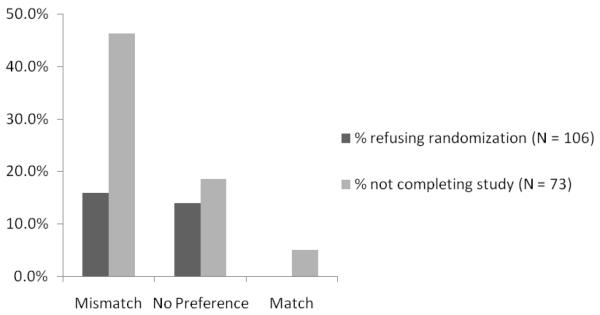
Twelve of 106 participants (11.3%) refused randomization. Of those randomized to their non-preferred group, 7 out of 44 (15.9%) refused randomization. Five out of 36 individuals (13.9%) who expressed no preference refused randomization. No participants randomized to their preferred group refused randomization (vs. non-preferred, χ2 (N = 70, df = 1) = 4.60, p = .03; See Figure 1). Among those who were mismatched, most (84.1%) did in fact start treatment; however, among those who refused randomization, none had been matched to their preferred treatment.
Figure 1.
Failure to start or complete treatment by preference match
Of those randomized to psychotherapy (CT or BA), 2 out of 33 (6.1%) refused randomization. Of those randomized to pharmacotherapy (Placebo or ADM), 10 out of 73 (13.7%) refused randomization. Those randomized to pharmacotherapy had about 50% greater odds of refusing randomization than those randomized to psychotherapy, OR = 1.57, Wald χ2(1) = 1.25, p = .26, although this effect was not statistically significant. The effect of preference mismatch on refusing randomization appeared about equal for those randomized to ADM but preferring psychotherapy (16.2% refused randomization) and those randomized to psychotherapy but preferring ADM (14.3% refused randomization). Logistic regression could not be used to test the interaction between condition and preference on refusing randomization because of the “empty” cell – i.e., there were no participants matched to their preferred treatment who refused randomization.
Study Completion
Not including individuals randomized to placebo or refusing randomization, 73 participants started psychotherapy or ADM; of these, 18 (24.6%) did not complete the study. Of the 26 randomized to their non-preferred group, 12 (46.2%) did not complete the study as compared to 5 out of 27 (18.5%) of those expressing no preference, and 1 out of 20 (5.0%) of those randomized to their preferred group. Participants had significantly higher odds of dropping out of treatment if they had been randomized to their non-preferred treatment group as compared to those randomized to their preferred treatment group, OR = 7.19, Wald χ2(n = 73, df = 1) = 6.45, p = .01 (Figure 1).
Most of those who did not complete the study (77.8%) were in the ADM condition. The odds of completing the study were about 50 percent lower (OR = .54, Wald χ2 = 3.75, p = .05) for those in the ADM condition compared to the psychotherapy conditions. The effect of preference match on study completion did not depend on treatment group (Wald χ2 = .22, p = .9). However, the effect of preference mismatch on study completion appeared slightly lower for those randomized to ADM but preferring psychotherapy (50.0% completed) than those randomized to psychotherapy but preferring ADM (66.7% completed).
Attendance
Among all patients who started treatment, individuals matched to their preferred group attended 89.1% of expected visits, individuals without a preference attended 84.9% of expected visits, and mismatched individuals attended 70.4% of expected visits. Those randomized to their preferred treatment group attended a significantly greater proportion of expected sessions (M = .89, SD = .12) than those randomized to their non-preferred group (M = .70, SD = .31), partial η2 = .10, F(1,70) = 7.56, p = .007. There were no differences in the proportion of sessions attended between those in ADM (M = .80, SD = .26) and those in BA/CT (M = .82, SD = .20), partial η2 = .00, F(1, 71) = .08, p = ns. The effect of preference (match vs. mismatch) on session attendance did not depend on treatment group, partial η2 = .01, F(1,67) = .65, p = .42.
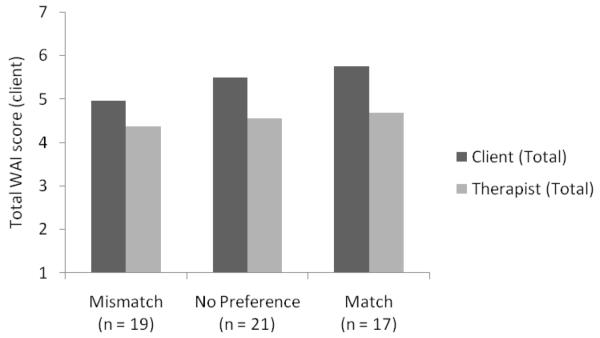
Working Alliance
At session 2, patient-rated working alliance (total score) was significantly higher among those randomized to their preferred treatment condition (M = 5.76, SD = .80) than those randomized to their non-preferred treatment (M = 4.96, SD = 1.12), Partial η2 = .10, F(1,54) = 5.86, p = .022 (Figure 2). The effect of preference match on WAI total scores did not depend on condition, β = .14, SE = .17, Partial η2 = .01, F(1,51) = .64, p = ns. There were no significant differences in therapist-rated WAI total scores for patients randomized to their preferred group (M = 4.68, SD = .64) compared to those randomized to their non-preferred group (M = 4.38, SD = .87), Partial η2 = .02, F(1,57) = 2.28, p = .26. There were no effects of condition on the relationship between preference match and therapist-rated WAI scores, partial η2 = .00, F(1,54) = .14, p = ns.
Figure 2.
Client- and Therapist-rated Session 2 WAI scores by preference match
There were significant differences between conditions in both patient and therapist WAI ratings from session two. Patients in BA/CT rated the working alliance (total score) significantly higher than those in ADM (M = 5.90, SD = .67 and M = 4.88, SD = 1.08, respectively), partial η2 = .25, F(1,55) = 18.14, p < .001. Similarly, BA/CT therapists rated the working alliance more positively than pharmacotherapists (M = 4.79, SD = .70 and M = 4.30, SD = .79, respectively), partial η2 = .10, F(1,58) = 6.45, p < .05. Also, on average, patient-ratings were .86 (SD = .96) points higher than therapist-ratings, t(52) = 6.56, p < .001.
Preference and Outcome
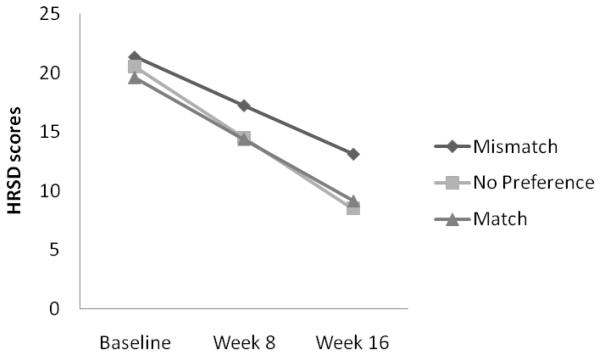
Figure 3 shows changes in HRSD scores over time by preference match. The direct effect of preference match on change in HRSD over time was not significant, β = −.07, SE = .08, F(1,101) = .79, p = .38 (effect size = .21, a small effect). A three-way interaction between condition, preference and time was also not significant, β = −.08, SE = .09, F(1,98) = .77, p = .38, although directionally this suggests slightly greater effects of preference match on changes in HRSD scores over time for those in ADM than those in psychotherapy. There was also no significant effect of match vs. mismatch on changes in BDI scores over time, β = −1.07, SE = 1.01, F(1,101) = 1.12, p = .29 (effect size = .25, a small effect).
Figure 3.
Changes in depression severity by preference match. Note: Means at each time point were calculated based on the results of multilevel modeling.
Indirect effects of preference match on HRSD scores were tested according to the model illustrated in Figure 4. Initially, this model was not a good fit to the data, χ2(N = 57, df = 4) = 10.14, p = .038, CFI = .733, RMSEA = .17 (90% CI: .035, .296). Upon closer inspection of the covariance matrix, we noted a significant negative correlation between match vs. mismatch and HRSD intercepts. When allowing these variables to covary, the model fit was excellent, χ2(N = 57, df = 3) = 1.72, p = .632, CFI = 1.00, RMSEA = .00 (90% CI: .000, .18). In both models, there was a significant indirect effect of match vs. mismatch on HRSD slopes, est = −.12 (90% CI: −.21, −.05), p = .003, and 16% of the variance in HRSD slopes was explained (primarily by attendance). An identical analysis using BDI scores produced similar results.
Figure 4.
Testing indirect effects of preference match on changes in HRSD scores. Paths represented with dashed lines were specified but not significant. Covariances between the preference match codes, between the mediators, and between HRSD slope and intercept were specified but not shown for clarity of presentation. *p < .05, ** p < .01
Discussion
This study examined the effects of patient preferences on a range of outcomes in an RCT of the treatment of major depression. Results suggest several negative implications of being randomly assigned to a non-preferred mode of treatment. Mismatch had an effect on whether patients started treatment, such that none of those who refused randomization received a preferred treatment. Similarly, those randomized to a non-preferred treatment were more likely to drop out of the study and attend fewer expected visits.3 Patients assigned to a non-preferred treatment also reported a less positive early therapeutic alliance than those assigned to a preferred treatment. These findings converge with efforts in collaborative care highlighting the importance of patient preferences in staying in treatment for depression (Byrne et al., 2006). These results are thus consistent with the suggestion that preference matching influences indirect outcomes (TenHave et al., 2003).
We did not find significant direct effects of preference mismatch on improvement in depression over the course of treatment. This is consistent with the findings of Leykin and colleagues (2007), who also found small, nonsignificant effects of preference matching on depression outcomes, using a similar study design. MacKinnon et al (2002) have noted that a lack of such direct effects of distal factors on primary outcomes is not uncommon when effect sizes and sample sizes are small and that it is possible to observe significant indirect effects via more proximal mediators. Given the significant effects of preference match on both attendance and early alliance, we used a path analysis to examine whether these variables mediated the effect of preference match on improvement in depression. This hypothesis was supported by our data, with 16% of the variance in depressive severity improvement explained (a medium effect size), primarily by a direct effect of attendance.
Thus, preferences appear to have an indirect effect on depression outcomes via commitment to and engagement in therapy. When patients do not receive a preferred treatment, they may be less likely to start treatment, stay in treatment, and attend an adequate number of treatment sessions. Even for the most efficacious treatments, patients needs to remain in treatment long enough to provide an opportunity to benefit from the treatment procedures. In fact, we may have underestimated the indirect effect of preference match on depression outcomes if symptom severity persisted or worsened for those who failed to start treatment (strongly predicted by preference match) or dropped out prior to 8 weeks (in which case their data were not available to be included in the analysis of change in depression). Furthermore, there are potentially other mediators of the preference-depression relationship not tested here (e.g., treatment adherence). It is also possible that some participants were generally unwilling to express a preference for fear of being excluded from the study.
These findings highlight the need to discuss a patient’s preferences at the outset of treatment or even prior to treatment assignment. A skilled therapist may help a patient who prefers one treatment see the value of alternative interventions, such as a more empirically-supported treatment. Persuasive strategies could be individually tailored to consider patients’ specific knowledge, beliefs and opinions about various treatment options (Hawkins, Kreuter, Resnicow, Fishbein, & Dijkstra, 2008). Preferences may be based on beliefs about the etiology of depression, beliefs about the purpose of emotion, and cultural or religious beliefs (Givens et al., 2006, 2007). Ignoring preferences could discount patients’ own valid perspectives on disease and alienate them in the process of seeking treatment. Inquiring about patient preferences may be especially important among specific patient populations who are highly vulnerable to non-engagement with recommended clinical interventions. For instance, a lack of attention to treatment preferences and beliefs is a barrier to the depression referral process for perinatal women, a group that experiences marked problems with depression treatment engagement (Flynn, O’Mahen, Massey, & Marcus, 2006).
A potential implication of these findings is that preferences may need to be addressed even before a patient has contact with a mental health professional. Although a mental health clinician may have the skills and time to address effectively a patient’s reluctance to try a treatment about which the patient is skeptical, providers in primary care settings who are most likely to have first contact with depressed patients may have fewer resources for addressing such preference related barriers to care. Thus, as preferences seem to matter especially for starting treatment, effectively managing treatment preferences could be an important skill for those involved in referral processes.
These data also suggest that many people may prefer not to use medication as treatment for depression. It is possible that the greater preference for psychotherapy was reflective of selection factors, with individuals preferring psychotherapy being more likely to enroll in the trial given the greater availability of pharmacotherapy versus psychotherapy in routine clinical service delivery systems. However, it is also possible that greater preference for psychotherapy reflects the treatment preferences of many depressed adults, highlighting the importance of focusing on training, policy and service delivery to support empirically-supported psychotherapy for the treatment of depression and other mental disorders, allowing those who do prefer this option to have their preferences met.
It is important to emphasize potential limitations regarding generalizabilty of these findings. Preferences may impact outcomes differently (and may need to be addressed differently) outside the context of a randomized trial. Other research designs may be better suited to studying the effects of preferences on direct and indirect outcomes (e.g., patient preference trials). The results also do not speak to the question of for whom preferences are more important. Indeed, some studies suggest that not all patients want to participate in shared decision making. Schneider and colleagues (2006) found that those with high external health locus of control expressed lower preference for involvement in decision making. Thus, individuals with more external health locus of control may be more content with any assigned or prescribed treatment, whereas those with more internal health locus of control may respond poorly to receiving a non-preferred mode of treatment.
Other methodological limitations are of note. The preference measure was administered to only a sub-sample of participants in this study. Although we found no significant differences in demographic or clinical characteristics between these groups, the limited administration did reduce statistical power. Also, although the use of the ETI was an improvement over other studies in that it explicitly assessed treatment preference, the ETI asks patients to make a forced choice response indicating discretely (rather than continuously) whether they preferred drug therapy, talking therapy, or had no preference. This measure does not allow for ambivalence or indication of to what degree a patient finds either mode of treatment acceptable. Also, it is not clear what “no preference” indicates for each individual. For example, it could mean that either treatment was acceptable, the patient had no opinion, or that the patient was unwilling to express an opinion.
In summary, patient preferences were important predictors of engagement in treatment, including starting treatment, staying in treatment, attending expected visits, and forming positive early therapeutic alliances, which ultimately predicted depression outcomes. Such findings underscore the importance of patient preferences in the design of RCTs, the provision of treatment recommendations, and the development of clinical services. It will be important for future research to address innovative ways of assessing, accommodating and modifying patient preferences, among general clinical populations and among specific groups vulnerable to non-engagement in treatment.
Acknowledgments
This research was supported by National Institute of Mental Health Grants MH55502 (R01), and MH079636 (F31), a predoctoral fellowship awarded to Bethany Kwan. We wish to acknowledge the investigator group for the National Institute of Mental Health Grant MH55502 (R01): Bob Kohlenberg, Karen Schmaling, David Dunner, Keith Dobson, and Steve Hollon, for their willingness to make data for this report available. GlaxoSmithKline provided medications and pill placebos for the trial.
Footnotes
Institutional Review Board (IRB) approval inadvertently lapsed for approximately 6 weeks at the time of the death of the original principal investigator; the IRB subsequently granted use and publication of data collected during that time.
Data on early working alliance was only available for a portion of the sample (57 out of 73; 78.1% patients and therapists). Due to administrative error, fewer patients and providers completed the WAI in the pharmacotherapy condition (29 out of 42; 69.0%) than in the psychotherapy (28 out of 31, or 90.3%).
A reviewer noted that there were different numbers of expected visits for those in psychotherapy vs pharmacotherapy, and our results might have been influenced by this discrepancy. However, the differential frequency and number of sessions is likely to be an inherent aspect of each of the treatments and thus cannot be separated from the other components of treatment.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy for depression. Guilford Press; New York: 1979. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the BDI-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Beck JS. Cognitive therapy: Basics and beyond. Guilford Press; New York: 1995. [Google Scholar]
- Byrne N, Regan C, Livingston G. Adherence to treatment in mood disorders. Current Opinion in Psychiatry. 2006;19:44–49. doi: 10.1097/01.yco.0000191501.54034.7c. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Salzer MS. The conflict between random assignment and treatment preference: implications for internal validity. Evaluation and Program Planning. 2003;26:109–121. doi: 10.1016/S0149-7189(03)00014-4. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74(4):658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Dobscha SK, Corson K, Gerrity MS. Depression treatment preferences of VA primary care patients. Psychosomatics. 2007;48:482–488. doi: 10.1176/appi.psy.48.6.482. [DOI] [PubMed] [Google Scholar]
- Elkin I, Yamaguchi JL, Arnkoff DB, Glass CR, Sotsky SM, Krupnick JL. “Patient-Treatment Fit” and early engagement in therapy. Psychotherapy Research. 1999;9(4):437–451. [Google Scholar]
- Fawcett J, Epstein P, Fiester SJ, Elkin I, Autry JH. Clinical management: Imipramine/placebo administration manual. Psychopharmacological Bulletin. 1987;23:309–324. [PubMed] [Google Scholar]
- Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67:578–582. doi: 10.1037//0022-006x.67.4.578. [DOI] [PubMed] [Google Scholar]
- Flynn HA, O’Mahen HA, Massey L, Marcus S. The impact of a brief obstetrics clinic-based intervention on treatment use for perinatal depression. Journal of Women’s Health. 2006;15(10):1195–1204. doi: 10.1089/jwh.2006.15.1195. [DOI] [PubMed] [Google Scholar]
- Givens JL, Datto CJ, Ruckdeschel K, Knott K, Zubritsky C, Oslin DW, et al. Older patients’ aversion to antidepressants: A qualitative study. Journal of General Internal Medicine. 2006;21:146–161. doi: 10.1111/j.1525-1497.2005.00296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givens JL, Houston TK, Van Voorhees BW, Ford DE, Cooper LA. Ethnicity and preferences for depression treatment. General Hospital Psychiatry. 2007;29:182–193. doi: 10.1016/j.genhosppsych.2006.11.002. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Education Research. 2008;23:454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, Thase ME, Markowitz JC. Treatment and prevention of depression. Psychological Science in the Public Interest. 2002;3(2):39–77. doi: 10.1111/1529-1006.00008. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36(2):223–233. [Google Scholar]
- Iacoviello BM, McCarthy KS, Barrett MS, Rynn M, Gallop R, Barber JP. Treatment preferences affect the therapeutic alliance: Implications for randomized controlled trials. Journal of Consulting and Clinical Psychology. 2007;75(1):194–198. doi: 10.1037/0022-006X.75.1.194. [DOI] [PubMed] [Google Scholar]
- Keller MB, Hirschfeld RM, Demyttenaere K, Baldwin DS. Optimizing outcomes in depression: focus on antidepressant compliance. International Clinical Psychopharmacology. 2002;17(6):265–271. doi: 10.1097/00004850-200211000-00001. [DOI] [PubMed] [Google Scholar]
- King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al. Impact of participants and physician intervention preferences on randomised trials: a systematic review. Journal of the American Medical Association. 2005;293:1089–1099. doi: 10.1001/jama.293.9.1089. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Leon AC, Markowitz JC, Manber R, Arnow B, Klein DN, Thase ME. Patient preference as a moderator of outcome for chronic forms of major depressive disorder treated with Nefazodone, Cognitive Behavioral Analysis System of Psychotherapy, or their combination. Journal of Clinical Psychiatry. 2009;70(3):354–361. doi: 10.4088/jcp.08m04371. [DOI] [PubMed] [Google Scholar]
- Leykin Y, DeRubeis RJ, Gallop R, Amsterdam JD, Shelton RC, Hollon SD. The relation of patients’ treatment preferences to outcome in a randomized clinical trial. Behavior Therapy. 2007;38:209–217. doi: 10.1016/j.beth.2006.08.002. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martell CR, Addis ME, Jacobson NS. Depression in context: Strategies for guided action. Norton; New York: 2001. [Google Scholar]
- Melfi CA, Chawla AJ, Croghan TW, Hanna MP, Kennedy S, Sredl K. The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Archives of General Psychiatry. 1998;55(12):1128–1132. doi: 10.1001/archpsyc.55.12.1128. [DOI] [PubMed] [Google Scholar]
- Preference Collaborative Review Group Patients’ preferences within randomised trials: systematic review and patient level meta-analysis. British Medical Journal. 2008;337:a1864. doi: 10.1136/bmj.a1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Raue P, Schulberg HC. Psychotherapy and patient preferences for the treatment of major depression in primary care. In: Henri MJ, editor. Trends in Depression Research. Nova Science Publishers, Inc.; 2007. pp. 31–51. [Google Scholar]
- Schneider A, Korner T, Mehring M, Wensing M, Elwyn G, Szecsenyi J. Impact of age, health locus of control and psychological co-morbidity on patients’ preferences for shared decision making in general practice. Patient Education and Counseling. 2006;61:292–298. doi: 10.1016/j.pec.2005.04.008. [DOI] [PubMed] [Google Scholar]
- TenHave TR, Coyne J, Salzer M, Katz I. Research to improve the quality of care for depression: alternatives to the simple randomized clinical trial. General Hospital Psychiatry. 2003;25:115–123. doi: 10.1016/s0163-8343(02)00275-x. [DOI] [PubMed] [Google Scholar]
- Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- Wilson M, Sperlinger D. Dropping out or dropping in? A re-examination of the concept of dropouts using qualitative methodology. Psychoanalytic Psychotherapy. 2004;18(2):220–237. [Google Scholar]