Ventricular tachycardia (VT) is an abnormal rapid heart rhythm originating from the lower pumping chambers of the heart (ventricles). The normal heart usually beats between 60–100 times per minute, with the atria contracting first, followed by the ventricles in a synchronized fashion. In ventricular tachycardia, the ventricles beat at a rapid rate, typically from 120 – 300 beats per minute (bpm), and are no longer coordinated with the atria.
The controlled contraction of the ventricles is important for the heart to pump blood to the brain and the rest of the body and maintain a normal blood pressure. Abnormal and fast rhythms from the ventricle may impair the ability of the pump to supply blood to the brain and rest of the body due to the rapid rate and weak contractions. This may result in palpitations (a feeling of rapid or abnormal heart beat), dizziness, lightheadedness, or syncope (loss of consciousness). If the heart rate increases more than 300 bpm, and becomes totally uncoordinated, this is usually called ventricular fibrillation (VF) which will cause sudden cardiac death.
VT occurs most commonly in patients with weakened heart muscle (cardiomyopathy), or when scar tissue develops in the heart. In patients with coronary artery disease (blockage of blood vessels on the surface of the heart), this scar is the result of a prior heart attack (myocardial infarction) where the muscle dies as a result of a blockage in blood flow. Scar, or fibrosis, can interfere with the normal electrical impulse in the heart, leading to a short-circuiting of the rhythm, called reentry. VT can also occur in patients with normal hearts by a different mechanism, whereby the electrical conduction is overly excitable, like a muscle twitch.
Sudden cardiac death causes about 450,000 fatalities each year in the United States alone. It is most commonly caused by VT deteriorating into ventricular fibrillation (VF), which is fatal within a few minutes if not defibrillated (shocked) back to a normal rhythm. (Figure 1A) This may be accomplished by an automated external defibrillator (AED) or implantable cardiac defibrillator (ICD). It is important to distinguish VT and VF, which are electrical problems of the heart, from a heart attack which is due to the sudden blockage of an artery. Heart attacks are treated with clot busting drugs, balloon angioplasty, or stents. Sometimes, VT and VF are seen in that setting and are treated with electrical shocks and drugs. The treatment of abnormal rhythms is discussed below.
FIGURE 1.
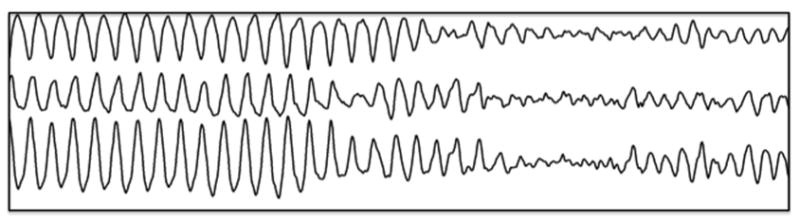
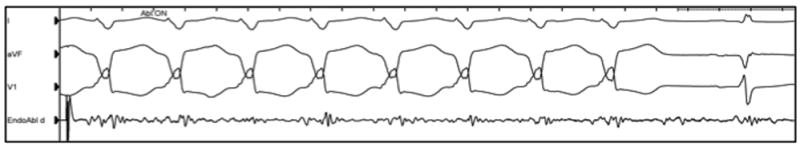
FIGURE 1A: Ventricular tachycardia (VT) often deteriorates into ventricular fibrillation (VF)-a lethal heart rhythm.
FIGURE 1B: Ablation of VT. Radiofrequency ablation is delivered (Abl:ON) at a site determined by mapping. The VT stops after two seconds of burning and the normal heart rhythm is restored.
Treatment Options
There are three treatment options for VT, although many patients require a combination: 1) implantable cardiac defibrillator (ICD) 2) antiarrhythmic medications, or 3) catheter ablation. Many patients at risk for VT are treated with an ICD. This is the most effective method of restoring a potentially life-threatening rhythm such as VT or VF back to a normal rhythm. However, an ICD does nothing to prevent the heart from going into VT. The ICD is a ‘safety net’ and is like having an ambulance crew accompany you 24 hours a day.
Antiarrhythmic medications that modify the conduction of the electrical impulse of the heart can be effective in suppressing VT. These medications can reduce the risk of recurrence by 75% but have potential side effects that includes proarrhythmia, or worsening of the heart rhythm. For this reason, initiation of antiarrhythmic agents often requires close monitoring. Amiodarone, the most effective drug, has many side effects, which can involve toxicity to the vital organs like the liver, thyroid, lungs, eyes, and skin.
Because of the discomfort associated with frequent ICD shocks and the side effects of antiarrhythmic drugs, catheter ablation is an important additional treatment option for many patients already on these therapies.
Catheter Ablation Therapy
Catheter ablation has been used to treat heart rhythm disorders for more than 25 years. This procedure targets the origin of the VT by placing a long, thin wire or catheter into the heart chambers through the veins of the leg. When areas that are critical to the arrhythmia are identified, a localized delivery of radiofrequency energy is applied, which produces a small burn about 4–5 mm in diameter.(1) The number of burns required to treat the VT varies among patients. In patients with scar tissue in the heart, ablations may be performed within the scar and around the perimeter of it to cauterize or ablate the abnormal electrical circuit responsible for the VT. (Fig 1B)
What to Expect Before and After Ablation
Before the procedure, special cardiac imaging with computerized tomography (CT) scan or echocardiography is usually performed to assess the location of scarring, if any, in the heart. Immediately before the procedure, a transesophageal echocardiogram may be performed to exclude the presence of blood clots in the heart. Additionally, echocardiography helps to assess the overall pumping function of the heart. Magnetic resonance imaging (MRI) is traditionally contraindicated in patients with an ICD, but can be performed at experienced centers under close supervision.
Precautions are taken to prevent the formation of blood clots before, during, and after ablation. During the procedure, an intravenous blood thinner called heparin is administered. After the procedure, many patients will be continued on warfarin, an oral anticoagulant, for up to a month to prevent blood clot formation when the heart is healing from the ablation. A short-acting injectable blood thinner, known as “low molecular weight heparin”, is often used for the first several days, because warfarin requires 5–10 days to become completely effective.
The procedure is usually performed under deep sedation or general anesthesia to minimize patient discomfort and movement. The catheters are inserted through intravenous ports, or sheaths, placed in the veins in the groin, and sometimes through a vein on the side of the neck. To access the left ventricle, a needle may be used to create a small puncture in the wall between the right and left side of the heart under ultrasound guidance (called transseptal catheterization). Alternatively, a catheter can be inserted into the heart through an artery in the groin (similar to heart catheterization procedures). The ablation catheter is moved around the ventricle, and a virtual three-dimensional image of the heart is created with a computer mapping system that acts like a GPS system (Fig 2). The location of the catheter is determined by use of fluoroscopy (X-ray) and this mapping system. Typically, the procedure lasts from 3 to 6 hours.
FIGURE 2. Mapping of VT.
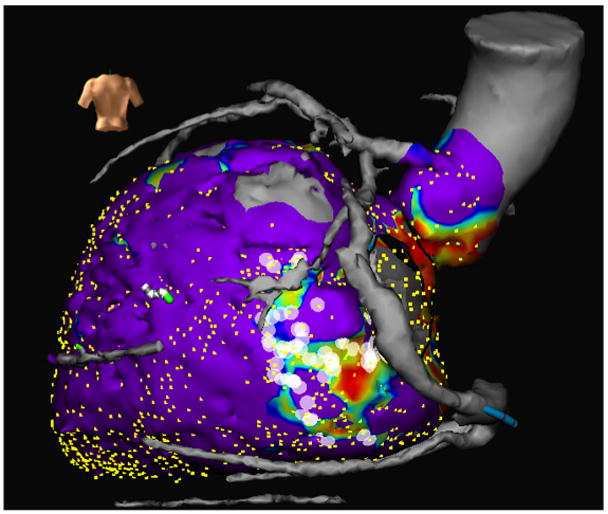
A three-dimensional real-time map of the ventricle (created during the procedure), merged with a CT scan (obtained before the procedure). The image shows the left ventricle (lower heart chamber) and the aorta (the larger artery that receives the blood pumped by the heart) and the blood vessels on the surface of the heart. The purple areas represent normal heart muscle with normal voltage registered on contact mapping. The area with blue, yellow, and red represents abnormal myocardium represented by progressively lower voltage, respectively, indicative of scar. Once a scar area is identified, the ablation is focused within and around this region. The white dots are the areas where ablation is performed within the scar.
In some instances, the physician determines that the VT may originate from a circuit on the outer surface of the heart, or epicardium. If this is the case, a puncture into the sac, or pericardium, around the heart is performed just beneath the breastbone. This enables the ablation catheter to be inserted and maneuvered within the pericardium to determine if the VT originates there. If a patient has a previous history of open heart surgery, a small surgical incision may be necessary to access the pericardium due to presence of scar tissue that can make the pericardium stick to the heart. These procedures to access the epicardium are usually performed at highly experienced centers.
Afterwards, the catheters are removed, but the sheaths are left in until the blood thinner wears off. Typically, this requires the patient to lie still for several hours to prevent bleeding from the puncture sites. Slight discomfort and bruising in the groin area can occur, and some patients experience self-limited mild chest pain due to inflammation caused by the ablation lesions. When the procedure is successful, antiarrhythmic medications may be stopped at the discretion of the physician.
What are the risks from the procedure and chance of success?
Major risks of the procedure include stroke (<1%) or puncture of the heart with bleeding in the sac around the heart (pericardial effusion) requiring drainage with another catheter (1–2%). The risks of epicardial puncture include bleeding that can require surgery is less than 1%. If ablation is performed on the epicardium, damage to the coronary arteries, which can lead to a heart attack, is a potential risk. In these instances, a picture of the blood vessels on the surface of the heart (coronary angiogram) can be performed to minimize this risk.
The success of VT ablation varies depending on the patient’s specific heart condition that caused VT. The procedure is most effective in patients with otherwise normal hearts, where the success rate is above 90%. In patients with structural heart disease due to scar or cardiomyopathy, success rates range between 50–75% at 6–12 months. In cases where a patient experiences a recurrence, 2 out of 3 patients will still have less VT than prior to the initial ablation. (2)
When is catheter ablation an appropriate treatment?
Since radiofrequency (RF) catheter ablation was first described 20 years ago, it has played an increasing role in the treatment of ventricular arrhythmias. Initially used in the treatment of patients with multiple ICD shocks for VT (VT storm), it is now used more frequently and earlier in the management of VT, particularly in centers with a high volume of patients and experience. Catheter ablation is an excellent choice for patients when medications are not effective, tolerated, or preferred.
Acknowledgments
KS was supported by NHLBI (R01HL084261)
Footnotes
DISCLOSURES:
Drs. Tung, Boyle and Shivkumar have received lecture honoraria from Boston Scientific, Biotronik and St Jude Medical respectively.
Institutional Disclosure: UCLA has received grants from Biosense-Webster US and St Jude Medical for their fellowship training program.
References
- 1.Miller JM, Zipes DP. Catheter ablation of arrhythmias. Circulation. 2002;106:e203–205. doi: 10.1161/01.cir.0000046082.16495.8f. [DOI] [PubMed] [Google Scholar]
- 2.Stevenson WG, Tedrow U. Preventing ventricular tachycardia with catheter ablation. Lancet. 2010;375:4–6. doi: 10.1016/S0140-6736(09)61915-2. [DOI] [PubMed] [Google Scholar]


