Abstract
Background
There are few data about use of catheter ablation for atrial fibrillation (AF) nationally. We analyzed data from the National Hospital Discharge Survey (NHDS) to examine trends in the rate of catheter ablation for hospitalized patients with AF over a fifteen year period.
Objectives
We examined rates of catheter ablation in patients with AF over time.
Design
All adult patients in the NHDS with an ICD-9-CM code for AF from years 1990 to 2005 were identified and assessed for the presence of a cardiac catheter ablation procedure code. Clinical characteristics associated with ablation were identified and multivariable logistic regression used to determine trends in the rate of ablation therapy over time.
Results
We identified 269,471 adults with AF. The rate of catheter ablation in AF patients increased from 0.06% in 1990 to 0.79% in 2005, (p<0.001 for trend). Compared to those not undergoing ablation, ablated patients were younger (mean age 66 vs. 76 years, p<0.001), more likely to be male (57% vs. 43%, p<0.001), have private insurance (22% vs. 11%, p<0.001), and have a CHADS2 stroke risk score of 0 (37% vs. 16%, p<0.001). Catheter ablation in AF patients increased by 15% per year over the time period (95% confidence interval: 13% to 16%) and across all age groups, including in patients aged ≥ 80 years (0.0% in 1990 and 0.26% in 2005, p<0.001 for trend).
Conclusions
The rate of catheter ablation in patients with AF is increasing significantly over time, even in the oldest patients.
Keywords: atrial fibrillation, catheter ablation, national trends, elderly
Introduction
Atrial fibrillation, the most common clinically significant cardiac arrhythmia, affects over 2.3 million people in the United States (1). Atrial fibrillation is associated with an increased risk of stroke and heart failure and independently increases the risk of all cause mortality (2–6). As such, atrial fibrillation confers a staggering healthcare cost burden (7–8). Pharmacologic treatments to restore sinus rhythm in patients with atrial fibrillation are associated with a considerable relapse rate (9–11) and the development of non-pharmacologic treatments for atrial fibrillation, such as catheter ablation procedures (12–14), may be significantly more successful in restoring and maintaining sinus rhythm (15–16). Despite relatively poor results from early catheter ablation techniques, the practice has evolved and boasts short term success rates as high as 73% to 91% depending on the specific type of procedure (17).
In light of the success of ablative therapy, an approach once used primarily in younger patients with structurally intact hearts has been expanded to include more medically complex patients, including elderly patients, those with cardiomyopathy, and those with implanted devices (16, 18). At the same time, catheter ablation is not without complications, with major complications observed in up to 6% of cases (19), and significant costs (20). Moreover, while the most optimistic randomized control data demonstrate the ability of catheter ablation to prevent the recurrence of atrial fibrillation at one year (12, 21–22), long term outcome data are lacking, particularly in patients older than 65 years or those with heart failure (17, 23).
The encouraging results supporting catheter ablation continue to stimulate the utilization of catheter ablation practices and spur innovations in ablation techniques (24). The American College of Cardiology/American Heart Association/European Society of Cardiology consensus guidelines recommend consideration of ablative therapy in many instances of atrial fibrillation (17). Atrial fibrillation is primarily a disease of older adults (25) and although most studies have focused on younger individuals (26), it is possible that increasing numbers of older patients are receiving ablation therapy (16). Although single center studies are available (16), there are few data about the characteristics of patients undergoing ablative therapy on a national level. In order to better understand the current use of catheter ablation treatment for atrial fibrillation, we analyzed data from the National Hospital Discharge Survey (NHDS) to explore trends in patient characteristics and rates of ablation procedures in hospitalized patients with atrial fibrillation from years 1990 to 2005.
Methods
The NHDS is a nationally representative study of hospitalized patients conducted annually by the National Center for Health Statistics (27), which collects data from approximately 270,000 inpatient records using a representative sample of about 500 short-stay nonfederal hospitals in the United States. Data for each patient are obtained about age, sex, hospital geographic region (Northeast, Midwest, South, West), and hospital bed size, as well as up to 7 diagnostic codes and 4 procedural codes using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). Of note, data on race/ethnicity were not consistently coded in the NHDS and therefore not included in this analysis.
We searched for all patients aged 18 years or older who had an ICD-9-CM diagnosis of atrial fibrillation (427.31). Of these patients, we then identified those who had a procedure code for non-surgical ablation of lesions or tissues of the heart via peripherally inserted catheter or endovascular approach (37.34). We also searched for specific ICD-9-CM coded diagnoses corresponding to higher stroke risk according to the CHADS2 risk index (congestive heart failure, hypertension, diabetes mellitus, and stroke or transient ischemic attack) (28) and calculated a CHADS2 score for each patient.
Statistical Analysis
Ablation rates were calculated as the number of patients with a diagnosis of atrial fibrillation and a code for catheter ablation divided by all patients with atrial fibrillation. The change in ablation rate over time was determined using simple logistic regression. Differences in ablation rates by patient and hospital characteristics were tested using chi-squared tests for categorical variables and t-tests for continuous variables. All variables that were tested in univariate analysis (age, sex, insurance status, year of procedure, and hospital region and bed-size, and CHADS2 score) were forced into the final multivariable model examining predictors of ablation. The fit of the final model was tested using the Hosmer-Lemeshow test for goodness-of-fit. Nationally representative estimates were calculated from the sample weights provided by the NHDS to account for the complex sampling design of the survey. All analyses were conducted using SAS Version 9.1 (SAS Institute Inc., Cary, NC).
Results
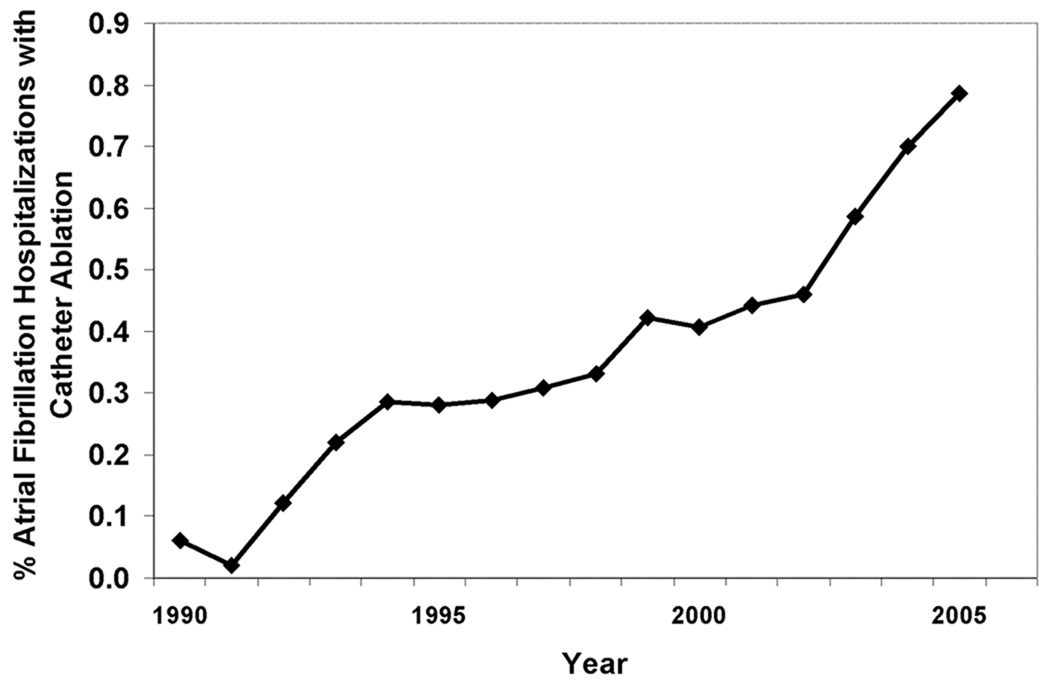
From years 1990 to 2005, we identified 269,471 hospitalizations in the NHDS with a diagnosis of atrial fibrillation, of which 1144 (0.42%) had a procedure code for catheter ablation. When extrapolated to national estimates, this corresponds to 32 million hospitalizations of patients with atrial fibrillation in the United States during the time period, of which 133,003 underwent ablation. The proportion of patients with atrial fibrillation who had ablation increased significantly over time, from 0.06% in year 1990 to 0.79% in 2005 (p<0.001 for trend, Figure 1).
Figure 1.
Overall Rate of Catheter Ablation Procedures in 269,471 Hospitalizations of Patients With Atrial Fibrillation From Years 1990 to 2005.
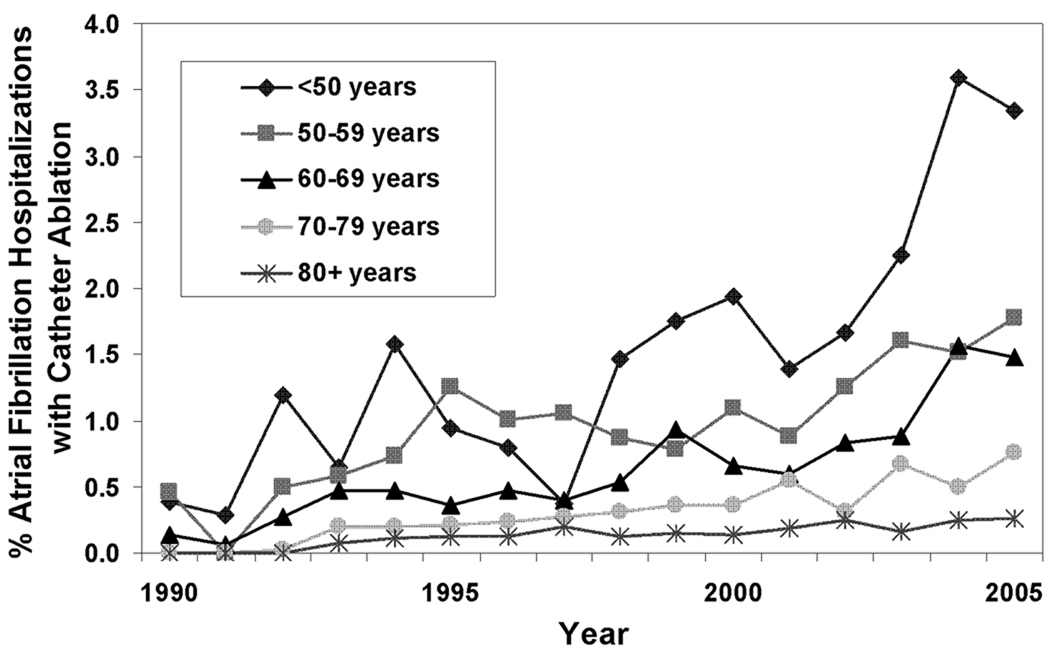
On univariate analysis, people with atrial fibrillation undergoing ablation were on average younger and more likely to be male than those who did not have ablation (Table 1). The rate of catheter ablation was higher in patients younger than 50 years (1.75%) compared to 0.55% in patients aged 50 to 79 years, and 0.16% in patients aged 80 or older. However, ablation rates increased significantly in all age groups over time, with no one age group increasing at a significantly faster rate than the others (p value for interaction between age categories and hospitalization year = 0.7, Figure 2). People undergoing ablation tended to have lower CHADS2 stroke risk scores and fewer risk factors for stroke, including heart failure, coronary artery disease, and diabetes mellitus (Table 1).
Table 1.
Characteristics of 269,471 Hospitalizations with Atrial Fibrillation, Stratified by Catheter Ablation Procedure During Hospitalization.
| Characteristic | Ablation N=1144 |
No Ablation N=268,327 |
P Value |
|---|---|---|---|
| Age, mean yrs and 95% CI* | 66.0 [65.2–66.8] | 75.9 [75.8–75.9] | <0.001 |
| Male (%) | 56.6 | 46.6 | <0.001 |
| Insurance (%) | <0.001 | ||
| Private | 22.1 | 10.9 | |
| Medicare | 56.5 | 78.2 | |
| Medicaid | 2.2 | 2.5 | |
| Self-pay | 0.7 | 1.2 | |
| Other/unknown | 18.5 | 7.2 | |
| Region (%) | <0.001 | ||
| West | 14.5 | 11.8 | |
| Midwest | 23.4 | 31.6 | |
| Northeast | 23.7 | 25.4 | |
| South | 39.3 | 31.2 | |
| Hospital bed size (%) | <0.001 | ||
| 6–99 | 1.2 | 12.7 | |
| 100–199 | 6.6 | 22.3 | |
| 200–299 | 17.4 | 23.8 | |
| 300–499 | 35.5 | 29.3 | |
| 500+ | 39.3 | 12.0 | |
| CHADS2 score, mean and 95% CI | 1.0 [0.9–1.0] | 1.5 [1.5–1.5] | <0.001 |
| CHADS2 = 0 (%) | 36.5 | 15.7 | <0.001 |
| Comorbid conditions | |||
| Heart failure (%) | 26.8 | 38.2 | <0.001 |
| Coronary artery disease (%) | 25.4 | 32.7 | <0.001 |
| Hypertension (%) | 30.8 | 29.2 | 0.24 |
| Diabetes mellitus (%) | 11.4 | 14.5 | 0.003 |
| Length of stay, mean days and 95% CI | 5.1 [4.7–5.5] | 7.4 [7.3–7.4] | <0.001 |
| Discharge Status (%) | <0.001 | ||
| Home | 88.8 | 58.7 | |
| Short term skilled facility | 0.8 | 4.06 | |
| Long term skilled facility | 4.0 | 18.3 | |
| Inpatient death | 1.0 | 6.7 | |
| Alive but status unknown | 5.0 | 10.9 |
CI=Confidence Interval
Figure 2.
The Rate of Catheter Ablation Procedures in 269,471 Hospitalizations of Patients With Atrial Fibrillation From Years 1990 to 2005, stratified By Patient Age.
People who underwent ablation were more likely to have private insurance as their primary source of payment and less likely to have Medicare (Table 1). Ablation rates were higher among patients with atrial fibrillation hospitalized in the Western and Southern regions of the United States (0.52% and 0.53%, respectively), compared to rates in the Midwest (0.30%) and Northeast (0.40%). Hospital bed size was significantly related to the frequency of ablation, with the overall rate of ablation in patients with atrial fibrillation being 0.04% in hospitals with 6 to 99 beds compared to 1.37% in hospitals with at least 500 beds (p<0.001). Length of stay was shorter in patients with ablations compared to patients without ablation therapy, and patients with ablation were more likely to be discharged home (Table 1). The inpatient mortality rate in patients undergoing ablation was quite low (0.96%).
In multivariate analysis, the likelihood of ablation therapy in a hospitalized patient with atrial fibrillation increased by 15% per year (95% confidence interval [CI] 13% to 16%) over the time period, adjusted for clinical and hospital characteristics. The likelihood of ablation decreased with older age (adjusted odds ratio [aOR] 0.7 [95% CI 0.6–0.7] for each decade of age over 50 years) and for each one point increase in CHADS2 score (aOR 0.7 [95% CI 0.7–0.8]). Ablation was significantly more likely to be performed in hospitals with larger bed-sizes (aOR 27.4 [95% CI 16.1–46.6] comparing bed-size of 500+ to bed-size of 6 to 99) and in patients with private insurance (aOR 1.4 [95% CI 1.2–1.6], Table 2). The goodness-of-fit of the model was appropriate, with a non-significant Hosmer-Lemeshow test p-value of 0.13.
Table 2.
Multivariable Adjusted Predictors of Catheter Ablation in Hospitalized Patients With Atrial Fibrillation
| Characteristic | All Patients N=269,471 |
Subset* N=246,402 |
|---|---|---|
| Adjusted Odds Ratio and 95 % Confidence Interval | ||
| Age (per decade over 50 yrs) | 0.67 [0.64–0.71] | 0.69 [0.64–0.74] |
| Male | 1.0 [0.91–1.2] | 0.88 [0.75–1.0] |
| Insurance | ||
| Private | Ref | Ref |
| Not private | 0.73 [0.63–0.85] | 0.70 [0.58–0.86] |
| Other/unknown | 0.71 [0.38–1.4] | 0.93 [0.45–1.9] |
| Region | ||
| Northeast | Ref | Ref |
| West | 1.4 [1.2–1.8] | 1.2 [0.95–1.6] |
| Midwest | 0.84 [0.71–1.0] | 0.81 [0.65–1.0] |
| South | 1.3 [1.1–1.5] | 1.1 [0.94–1.4] |
| Hospital bed size | ||
| 6–99 | Ref | Ref |
| 100–199 | 2.8 [1.6–4.9] | 5.0 [2.1–11.5] |
| 200–299 | 6.8 [4.0–11.7] | 10.2 [4.5–21.1] |
| 300–499 | 11.1 [6.5–19.0] | 16.6 [7.4–37.3] |
| 500+ | 26.1 [15.3–44.5] | 40.2 [17.9–90.4] |
| CHADS2 score (per point increase) |
0.74 [0.69–0.79] | 0.77 [0.71–0.85] |
Subset of patients who had no other code for cardiac arrhythmias
To account for the possibility that the ablation procedure was not specifically for atrial fibrillation, we performed a subgroup analysis that excluded all patients who also had diagnostic codes for supraventricular or ventricular tachycardias (427.0, 427.1, 427.2, and 427.4), or atrial flutter (427.32). Of the 269,471 hospitalizations with atrial fibrillation, 23,069 (8.6%) had a code for an arrhythmia in addition to atrial fibrillation. When we excluded patients with other arrhythmias, we identified 691 patients who underwent ablation and who only had a diagnosis of atrial fibrillation. An analysis of this subset yielded results similar to the full analysis (Table 2). The likelihood of ablation therapy in this subset of patients with only atrial fibrillation increased by 14% per year (95% CI 11%–16%], adjusting for patient age, sex, insurance status, CHADS2 score, and hospital region and bed-size.
Discussion
The proportion of hospitalized patients with atrial fibrillation who undergo ablation therapy in the United States has been increasing by approximately 15% per year over the last fifteen years. Patients receiving ablation therapy are more likely to be younger, have private insurance, and have fewer stroke risk factors. These demographics likely reflect the fact that these ablations are elective procedures that are preferentially performed in healthier, lower-risk patients. Despite these preferences, the rate of ablation therapy has been increasing significantly across all age groups, even in the oldest patients.
Though limited by relatively short follow-up data, published studies of ablation therapies for atrial fibrillation show promising results (17, 26), and initial cost analyses suggest possible fiscal benefits of ablation for atrial fibrillation (20). Despite a paucity of randomized clinical trials comparing ablation to pharmacologic rhythm and rate control, studies suggest that quality of life may be significantly improved with ablation as compared to antiarrhythmic drugs (21). This may be because ablation may reduce atrial fibrillation related symptoms (12). As ablation becomes more widespread and recommended, physicians, including hospitalists, may be increasingly likely to refer their patients for ablation, even for patient sub-groups who were not well-represented in clinical trial settings.
The inpatient mortality rate in patients undergoing ablation therapy was quite low in our study, although ablation is not without some risk of procedure-related stroke and other complications (19). An analysis of the compiled studies on ablation for atrial fibrillation estimates that major complication such as cardiac tamponade or thromboembolism occur in as many as 7% of patients (26). Patients are at highest risk for embolic events, such as transient ischemic attacks or ischemic strokes, in the immediate hours to weeks after ablation. An estimated 5%–25% of patients will develop a new arrhythmia at some point in the post-ablation period and other complications including esophageal injury, phrenic nerve injury, groin hematoma, and retroperitoneal bleed, have been observed (26). Increasing co-management of post-ablation patients will necessitate that hospitalists understand the potential complications of ablation as well as current strategies for bridging anticoagulation therapy.
Few data are available about the safety and efficacy of catheter ablation for patients over the age of 65 years. In fact, the mean age of patients enrolled in most clinical trials of catheter ablation was younger than 60 years (26,29). There are also limited data about the long-term efficacy of ablation therapy in patients with structural heart disease (30); despite this, our study shows that a quarter of patients with atrial fibrillation undergoing ablation therapy in the United States have diagnosed heart failure. As always, the optimistic introduction of new technologies to unstudied patient populations carries the risk of unintended harm. Hospitalists are well situated to collect and analyze outcome data for older patients with multiple comorbidities and to provide real-time monitoring of potential complications.
Few studies have focused on the demographic and comorbid characteristics of patients undergoing ablation for atrial fibrillation on a national level. One study examined characteristics of patients referred to a single academic center for atrial fibrillation ablation from 1999 to 2005 and found that referred patients have, over time, been older (mean age 47 years in 1999 and 56 years in 2005), have more persistent atrial fibrillation, larger atria, and were more likely to have had a history of cardiomyopathy (0% in 1999 to 16% in 2006) (16). This study also reported that men were consistently more likely to be referred for ablation than women. These results are generally consistent with our findings.
Our study has several limitations. The exact indication and specific type of ablation were not available in the NHDS, and it is possible that the ablation procedure was for an arrhythmia other than atrial fibrillation. However, our analysis of the subset of patients who only had atrial fibrillation as a diagnosis yielded results similar to the full analysis. We were unable to assess specific efficacy or complication data, but mortality was low and patients tended to have short hospital stays. Because the NHDS samples random hospitalizations, it is possible that some patients were over-represented in the database if they were repeatedly hospitalized in a single year. This could potentially bias our results towards an overestimate of the number of patients who receive ablation.
It remains unclear what proportion of atrial fibrillation ablation procedures occur in the outpatient versus inpatient setting. Inpatient versus outpatient status is not specified in the few single center ablation experiences reported in the literature (16), and the few trials reported are not reliable for determining practice in a non-study setting. The most recent (2006) HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation recommends aggressive anticoagulation in the peri-procedure period with either heparin or low molecular weight heparins, followed by a bridge to warfarin (17). It makes intuitive sense that patients undergoing ablation for atrial fibrillation would be admitted at least overnight to bridge anticoagulation therapy and monitor for complications, but widespread use of low molecular weight heparin may make hospitalization less necessary. The observation that patients undergoing ablation had shorter hospital stays does not necessarily imply that ablation procedures shorten hospital stays. Rather, the data almost certainly reflect the fact that ablations are mostly elective procedures performed in the setting of planned short-term admissions.
Our study provides important epidemiologic data about national trends in the use of ablation therapy in hospitalized patients with atrial fibrillation. We find that the rate of catheter ablation in patients with atrial fibrillation has been increasing significantly over time and across all age groups, including the oldest patients. As the proportion of patients with atrial fibrillation who receive ablation therapy continues to increase over time, comprehensive long-term outcome data and cost-effectiveness analyses will be important.
Acknowledgments
This work was supported by a Paul B. Beeson Career Development Award (1 K23 AG28978) from the National Institute on Aging.
Footnotes
Neither of the authors have conflicts of interest pertaining to the manuscript.
References
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Atrial Fibrillation Investigators. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154(13):1449–1457. [PubMed] [Google Scholar]
- 3.Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113(5):359–364. doi: 10.1016/s0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 4.Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am J Med. 1995;98(5):476–484. doi: 10.1016/S0002-9343(99)80348-9. [DOI] [PubMed] [Google Scholar]
- 5.Poole-Wilson PA, Swedberg K, Cleland JG, et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomized controlled trial. Lancet. 2003;362(9377):7–13. doi: 10.1016/S0140-6736(03)13800-7. [DOI] [PubMed] [Google Scholar]
- 6.Maggioni AP, Latini R, Carson PE, et al. Valsartan reduces the incidence of atrial fibrillation in patients with heart failure: results from the Valsartan Heart Failure Trial (Val-HeFT) Am Heart J. 2005;149(3):548–557. doi: 10.1016/j.ahj.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 7.Wolf PA, Mitchell JB, Baker CS, Kannel WB, D'Agostino RB. Impact of atrial fibrillation on mortality, stroke, and medical costs. Arch Intern Med. 1998;158(3):229–234. doi: 10.1001/archinte.158.3.229. [DOI] [PubMed] [Google Scholar]
- 8.Le Heuzey JY, Paziaud O, Piot O, et al. Cost of care distribution in atrial fibrillation patients: the COCAF study. Am Heart J. 2004;147(1):121–126. doi: 10.1016/s0002-8703(03)00524-6. [DOI] [PubMed] [Google Scholar]
- 9.Crijns HJ, Van Gelder IC, Van Gilst WH, Hillege H, Gosselink AM, Lie KI. Serial antiarrhythmic drug treatment to maintain sinus rhythm after electrical cardioversion for chronic atrial fibrillation or atrial flutter. Am J Cardiol. 1991;68(4):335–341. doi: 10.1016/0002-9149(91)90828-9. [DOI] [PubMed] [Google Scholar]
- 10.Roy D, Talajic M, Dorian P, et al. Amiodarone to prevent recurrence of atrial fibrillation. Canadian Trial of Atrial Fibrillation Investigators. N Engl J Med. 2000;342(13):913–920. doi: 10.1056/NEJM200003303421302. [DOI] [PubMed] [Google Scholar]
- 11.Van Gelder IC, Crijns HJ, Tieleman RG, et al. Chronic atrial fibrillation. Success of serial cardioversion therapy and safety of oral anticoagulation. Arch Intern Med. 1996;156(22):2585–2592. doi: 10.1001/archinte.156.22.2585. [DOI] [PubMed] [Google Scholar]
- 12.Oral H, Pappone C, Chugh A, Good E, et al. Circumferential pulmonary-vein ablation for chronic atrial fibrillation. N Engl J Med. 2006;354(9):934–941. doi: 10.1056/NEJMoa050955. [DOI] [PubMed] [Google Scholar]
- 13.Chugh A, Morady F. Atrial fibrillation: catheter ablation. J Interv Card Electrophysiol. 2006;16(1):15–26. doi: 10.1007/s10840-006-9018-4. [DOI] [PubMed] [Google Scholar]
- 14.Packer DL, Asirvatham S, Munger TM. Progress in nonpharmacologic therapy of atrial fibrillation. J Cardiovasc Electrophysiol. 2003;14(12 Suppl):S296–S309. doi: 10.1046/j.1540-8167.2003.90403.x. [DOI] [PubMed] [Google Scholar]
- 15.Mickelsen S, Dudley B, Treat E, Barela J, Omdahl J, Kusumoto F. Survey of physician experience, trends and outcomes with atrial fibrillation ablation. J Interv Card Electrophysiol. 2005;12(3):213–220. doi: 10.1007/s10840-005-0621-6. [DOI] [PubMed] [Google Scholar]
- 16.Gerstenfeld EP, Callans D, Dixit S, et al. Characteristics of patients undergoing atrial fibrillation ablation: trends over a seven-year period 1999–2005. J Cardiovasc Electrophysiol. 2007;18(1):23–28. doi: 10.1111/j.1540-8167.2006.00662.x. [DOI] [PubMed] [Google Scholar]
- 17.Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114(7):e257–e354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 18.Lakkireddy D, Patel D, Ryschon K, et al. Safety and efficacy of radiofrequency energy catheter ablation of atrial fibrillation in patients with pacemakers and implantable cardiac defibrillators. Heart Rhythm. 2005;2(12):1309–1316. doi: 10.1016/j.hrthm.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 19.Cappato R, Calkins H, Chen SA, et al. Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. 2005;111(9):1100–1105. doi: 10.1161/01.CIR.0000157153.30978.67. [DOI] [PubMed] [Google Scholar]
- 20.Khaykin Y, Morillo CA, Skanes AC, McCracken A, Humphries K, Kerr CR. Cost comparison of catheter ablation and medical therapy in atrial fibrillation. J Cardiovasc Electrophysiol. 2007;18(9):907–913. doi: 10.1111/j.1540-8167.2007.00902.x. [DOI] [PubMed] [Google Scholar]
- 21.Wazni OM, Marrouche NF, Martin DO, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA. 2005;293(21):2634–2640. doi: 10.1001/jama.293.21.2634. [DOI] [PubMed] [Google Scholar]
- 22.Pappone C, Augello G, Sala S, et al. A randomized trial of circumferential pulmonary vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation: the APAF Study. J Am Coll Cardiol. 2006;48(11):2340–2347. doi: 10.1016/j.jacc.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 23.Fang MC, Chen J, Rich MW. Atrial fibrillation in the elderly. Am J Med. 2007;120(6):481–487. doi: 10.1016/j.amjmed.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 24.O'Neill MD, Jaïs P, Hocini M, Sacher F, Klein GJ, Clémenty J, Haïssaguerre M. Catheter ablation for atrial fibrillation. Circulation. 2007;116(13):1515–1523. doi: 10.1161/CIRCULATIONAHA.106.655738. [DOI] [PubMed] [Google Scholar]
- 25.Furberg CD, Psaty BM, Manolio TA, Gardin JM, Smith VE, Rautaharju PM. Prevalence of atrial fibrillation in elderly subjects (the Cardiovascular Health Study) Am J Cardiol. 1994;74(3):236–241. doi: 10.1016/0002-9149(94)90363-8. [DOI] [PubMed] [Google Scholar]
- 26.Calkins H, Brugada J, Packer DL, et al. HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2007;4(6):816–861. doi: 10.1016/j.hrthm.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 27.US Department of Health and Human Services, Public Health Service, National Center for Health Statistics National Hospital Discharge Survey 1990–2005. [Accessed July 15, 2007];Multi-Year Public-Use Data File Documentation. Available at: http://www.cdc.gov/nchs/about/major/hdasd/nhds.htm.
- 28.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–2870. doi: 10.1001/jama.285.22.2864. [DOI] [PubMed] [Google Scholar]
- 29.Wood MA, Brown-Mhoney C, Kay GN, Ellenbogen KA. Clinical outcomes after ablation and pacing therapy for atrial fibrillation: a meta-analysis. Circulation. 2000;101(10):1138–1144. doi: 10.1161/01.cir.101.10.1138. [DOI] [PubMed] [Google Scholar]
- 30.Hsu LF, Jaïs P, Sanders P, et al. Catheter ablation for atrial fibrillation in congestive heart failure. N Engl J Med. 2004;351(23):2373–2383. doi: 10.1056/NEJMoa041018. [DOI] [PubMed] [Google Scholar]