Abstract
Purpose
To determine the 4-year incidence of visual impairment (VI) and blindness and worsening of visual acuity in adult Latinos/Hispanics aged 40 years and older.
Design
Population-based, longitudinal study.
Methods
Participants underwent a detailed ophthalmologic examination including assessing both presenting binocular (PVA) and best-corrected distance visual acuity (BCVA) in both eyes using a standard ETDRS protocol. The main outcome measures are 4-year incidence of visual impairment and blindness based on PVA or BCVA in the better seeing eye and defined as 1) baseline visual acuity (PVA or BCVA)≥20/40 and a follow-up PVA or BCVA<20/40 but better than 20/200, and 2) baseline PVA>20/200 and a follow-up PVA≤20/200 respectively. Monocular worsening was defined as a decrease of ≥5, 10, and 15 letters in either eye.
Results
Four thousand six hundred and fifty eight participants were examined at baseline and the 4-year follow-up. The 4-year incidence of presenting binocular VI and blindness was 2.9% and 0.3%. The 4-year incidence of best corrected VI and blindness was 1.2% and 0.3%. The 4-year incidence of monocular worsening by ≥5, 10, and 15 letters was 24.8%, 8.5% and 3.1% respectively. The incidence of VI and blindness increased with age at baseline (P<0.01). The incidence of VI in the second eye (12.2%) was significantly higher than incidence of VI in the first eye (2.9%)(P<0.001).
Conclusion
Overall, the annual incidence of VI in Latinos/Hispanics was higher than that reported in non-Hispanic white persons and the highest reported in a population-based study in the U.S. Screening and intervention programs to reduce visual impairment and blindness should focus on the older Latino population.
Latinos/Hispanics, the largest US minority and the fastest growing segment of the US population, are a racial/ethnic population with unique demographic, socioeconomic, mortality, morbidity, and ocular disease characteristics. According to the 2000 US Census, 12.5% of US residents, or 35 million people, are Latino/Hispanic.1 This number is expected to nearly double to 61.4 million by the year 2025.1 Given this growth in the Latino population, the burden of eye disease in Latinos are increasingly becoming a public health concern.
There are few population-based epidemiologic studies focusing on visual impairment rates in Latinos. Previous studies2–12 have estimated prevalence and incidence rates of visual impairment on persons of European ancestry,2–4 and African ancestry5,6,12. However, a majority of studies published on visual impairment have focused on obtaining prevalence estimates,5–11 and only a select few have gathered follow-up data from their original cohort to obtain incidence estimates of visual impairment.2,4,12 No previous study has examined the incidence of visual impairment and eye disease in a Latino/Hispanic population. Both the Proyecto Ver study7 and the Los Angeles Latino Eye Study (LALES)11 have provided prevalence estimates of visual impairment in population-based samples of adult Latinos. In the LALES it was noted that the age-specific prevalence of visual impairment in the better-seeing eye in Latinos was higher than that noted in studies on persons of European ancestry. The age-specific prevalence also showed a significant trend with older persons having higher rates of visual impairment. However, while suggestive, these data did not provide clear evidence that older Latinos were more likely to become visually impaired and blind compared to younger Latinos. This emphasized the importance of obtaining incidence rates in an aging Latino cohort.
Furthermore, most incidence studies provide estimates of visual impairment in one eye, typically the “worse” eye. However, as we have shown previously, persons with bilateral visual impairment have worse health-related quality of life than those with unilateral visual impairment13. Thus, to gain an accurate assessment of the burden of visual impairment particularly from a quality of life perspective, it is important to obtain incidence rates of unilateral and bilateral visual impairment particularly in persons with existing unilateral visual impairment. No previous epidemiological study has reported these results.2,3,12
Finally, while the prevalence of both visual impairment and blindness (severe visual impairment) in Latinos is higher than non-Hispanic whites in both the Beaver Dam Eye Study (BDES)8 and Blue Mountains Eye Study (BMES),9 and similar to that of Afro-Carribeans in Barbados, no comparison data are present on the incidence rates of visual impairment and blindness. 5 LALES provides the first opportunity to compare the incidence of visual impairment in Latinos and persons of African and European ancestry.
METHODS
Population
Details of the baseline LALES study design have been reported elsewhere.14 In summary, the data collection for the baseline population-based prevalence study was conducted from 2000 to 2003. Of the 7789 eligible residents (aged 40 years and older and self-identified Latinos) in six census tracts in La Puente, California who were invited to participate, 6357 (82%) completed an in-home questionnaire and a clinical examination. All living eligible individuals from the baseline LALES were invited to participate in the 4-year follow-up incidence study. Data collection for the incidence study began in 2004 and was completed in 2008.
Incidence Study Procedures
An in-home interview was conducted (including sociodemographic, medical and ocular history and utilization of health care). Details of the interview are available elsewhere.14 Participants were scheduled for a detailed eye examination conducted at the LALES local eye examination center. The visit included a visual field evaluation and a slit-lamp and dilated fundus examination performed by an ophthalmologist. Visual acuity (VA) was determined for each eye with the presenting correction, if any, using the revised ETDRS charts 1, 2, and 3; Lea symbol charts for illiterate participants.14 Visual acuity was measured at 1 meter for those who read <20 letters at 4 meters. Automated refraction with a Humphrey Automatic Refractor (model 599, Carl Zeiss Meditec, Dublin, CA) was performed if the participant could not read ≥55 letters at 4 meters in either eye; this was followed by a subjective refraction using standard protocols.11 These protocols were identical to the ones in the baseline assessment. As in the baseline study, individuals who did not complete a clinical examination at the examination center were asked to undergo an in-home examination by an ophthalmologist and a trained technician using the ETDRS protocol. Visual acuity was scored as the total number of letters read correctly and converted to a logarithm of the minimal angle of resolution (LogMAR) score. The 4-year incidence of visual impairment and blindness was calculated, and estimates were made of percentages of individuals with worsening improvement of vision from baseline to follow-up.
Multiple quality control measures were implemented throughout the study. 14 These measures included validation of at least 5% of each interviewer’s work, validation of 10% of inclinic questionnaires, and repeat measurement of several variables during the clinic examination by more than one technician. In addition, data checks were incorporated into the data management program, and the supervising technician reviewed participant information in the database for completeness and accuracy.
Definitions
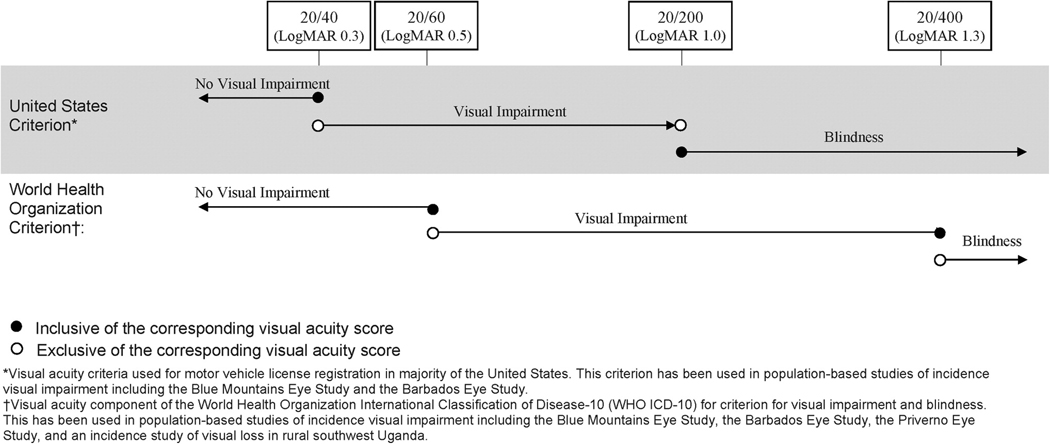
There are no universally accepted criteria for visual impairment, blindness (severe visual impairment), or changes in visual impairment. The criteria that we have used in this study are summarized in Figure 1.
Figure 1.
Criteria for Visual Impairment and Blindness in the Los Angeles Latino Eye Study *Visual acuity criteria used for motor vehicle license registration in a majority of the states in the United States of America.
†Visual acuity component of the World Health Organization International Classification of Disease-10 (WHO ICD-10) for criteria for visual impairment and blindness.
For a majority of the analysis, we use a United States (US) and World Health Organization (WHO) criteria for visual impairment and blindness. Based on previous convention, the criterion for incidence of visual impairment and blindness using standard US and WHO criteria include in their baseline at-risk cohort only those persons with no visual impairment or blindness in their better-seeing eye (no bilateral visual impairment at baseline). Modifications to the US and WHO criteria were made to redefine the at-risk cohort to include those who at baseline had no unilateral or bilateral visual impairment to provide data on the incidence of visual impairment and blindness in the first and second eye.
Presenting Binocular Visual Impairment and Blindness
A novel aspect of our incidence study was the assessment of binocular VA (with both eyes open), a better measure of functional vision than monocular visual acuity in the better seeing eye. Using the US criterion, persons at risk for binocular visual impairment had a baseline presenting binocular VA (PVA) better than or equal to 20/40; visual impairment at follow-up was PVA worse than 20/40 but better than 20/200. Those at risk for binocular blindness had a baseline PVA better than 20/200; blindness at follow-up was PVA 20/200 or worse. Using the WHO criterion, persons at risk for binocular visual impairment had a baseline presenting VA (PVA) better than or equal to 20/60; visual impairment at follow-up was PVA worse than 20/60 but no worse than 20/400. Those at risk for binocular blindness had a baseline PVA better than or equal to 20/400; blindness at follow-up was PVA worse than 20/400.
Visual Impairment and Blindness in the Best corrected Better Seeing Eye
The standard criterion for visual impairment and blindness in the US and the WHO criteria refer to the best corrected visual acuity in the better seeing eye.
US Criterion: For this incidence analyses persons at risk for visual impairment had a baseline presenting VA (BCVA) of 20/40 or better in their better seeing eye. Persons were identified as having incident visual impairment if at follow-up they had a BCVA worse than 20/40 but better than 20/200 in the better seeing eye. Those at risk for blindness had a baseline BCVA better than 20/200 in their better seeing eye. Persons were identified as having incident blindness if at follow-up they had a BCVA of 20/200 or worse in their better seeing eye.
WHO Criterion: For these analyses persons at risk for visual impairment had a baseline presenting VA (BCVA) of 20/60 or better in their better seeing eye. Persons were identified as having incident visual impairment if at follow-up they had a BCVA worse than 20/60 but no worse than 20/400 in their better seeing eye. Those at risk for blindness had a baseline BCVA better than or equal to 20/400 in their better seeing eye. Persons were identified as having incident blindness if at follow-up they had a BCVA of worse than 20/400.
Monocular Visual Impairment and Blindness
Both US and WHO criteria were used. According to US criterion, those at risk for visual impairment in a specific eye had a baseline best-corrected VA (BCVA) of 20/40 or better; visual impairment at follow-up was BCVA worse than 20/40 but better than 20/200 (not including 20/40 or 20/200) in the same eye. By these same criteria, persons at risk for blindness in a specific eye had baseline BCVA better than 20/200; blindness at follow-up was BCVA 20/200 or worse (including 20/200) in the same eye. Using WHO criteria, individuals at risk for visual impairment in a specific eye had a baseline BCVA 20/60 or better; visual impairment at follow-up was BCVA worse than 20/60 but better than or equal to 20/400 (not including 20/60 but including 20/400) in the same eye. WHO criteria defined those at risk for blindness in a specific eye as having a baseline BCVA 20/400 or better; blindness at follow-up was BCVA worse than 20/400 (not including 20/400) in the same eye.
Worsening and improvement in Binocular Presenting Visual Acuity
Persons at risk for binocular worsening had baseline PVA better than no light perception; worsening at follow-up was loss of ≥5, 10, or 15 letters read correctly. Those capable of binocular improvement read ≥5, 10, or 15 letters correctly at baseline; improvement at follow-up was an increase of ≥5, 10, or 15 letters read correctly.
Worsening and Improvement in Monocular Best Corrected Visual Acuity
Monocular worsening was defined as decrease from baseline to follow-up of ≥5, 10, and 15 letters read correctly evaluated in either eye (at risk, BCVA of light perception or better in both eyes at baseline) and in the better-seeing eye (at risk, BCVA of light perception of better in one or both eyes at baseline). Monocular improvement was gain from baseline to follow-up of ≥5, 10, and 15 letters read correctly evaluated in either eye and in the worse-seeing eye (at risk, capable of improving from baseline by ≥5, 10, and 15 letters read correctly in the eye of interest).
Statistical Methods
To examine possible impact of non-participation at the 4-year follow-up examination, socio-demographic and clinical characteristics were compared between participants who completed the follow-up examination and nonparticipants using the chi-square test for categorical variables and Student’s t-test for continuous variables. Overall and age-standardized (to the LALES population) 4-year incidence rates of binocular or monocular visual impairment and blindness were calculated for each of the categories of visual impairment and blindness (described above) as the proportion of the number of new cases (participants or eyes) with visual impairment or blindness to the number of participants (or eyes) that had no visual impairment or blindness at the time of the baseline examination. Analyses were stratified by age at baseline examination and gender. Because there were no gender differences in any of the incidence rates, results of these analyses are not presented. The statistical significance of associations between incidence and age subgroups was assessed with the test of trend.
Overall and age-specific progression rates for binocular (per participant) and monocular (either eye, better-seeing eye, worse-seeing eye) worsening or improvement in vision was calculated for each criterion for change (5, 10, 15 letters, described above) as the ratio of the number of cases (participants or eyes) that worsened or improved to the number of participants with visual impairment at baseline examination. LOWESS (locally weighted polynomial regression) plots for the US and WHO criteria for visual impairment and blindness allowed an assessment of the relationship between age at baseline and the incidence of visual impairment and blindness..
To compare the incidence of visual impairment across population-based studies, the annual incidence of visual impairment, blindness, and change in visual impairment was estimated from the 4-year incidence in the LALES and the 5-year incidence in the BDES and the BMES using criteria from the BDES. In addition, the 4-year incidence rates of visual impairment and blindness were annualized to compare the results to the BISED using US and WHO criteria.
All analyses were conducted using SAS version 9.1 (SAS Institute, Cary, North Carolina). STATA version 9.0 (STATA Corp LP, College Station, Texas) was used to create LOWESS (locally weighted regression) plots.
RESULTS
Study Cohort
Of the 6357 participants examined at baseline, 6100 living participants were eligible for this follow-up study. Of the 6100 living eligibles, 4658 (76%) completed a clinical examination and 4640 (76%) had complete visual acuity data (Figure 2). Participants were followed for a mean of 4.2±0.52 years. Socio-demographic and historical characteristics of participants who completed the interview and clinical examination at the 4-year follow-up (n=4658) and nonparticipants (n=1442) are summarized in Table 1. The majority of participants were female (60%); <60 years of age (69%), and were born outside the US (77%). Specifically, the country of birth was identified as Mexico in 64%, US in 23%, El Salvador in 5%, Guatemala in 2.5%, Nicaragua in 1% and other countries in 4.5% of participants. Only 19% reported their health to be excellent or very good, and 41% had at least 2 co-morbidities. Participants and non-participants differed significantly with regard to gender, age, marital status, health insurance, history of hypertension, co-morbidities, self-reported vision, in-home binocular near vision, history of ocular disease and history of cataract (p<0.05).
Figure 2.
Participation Flowchart for assessing 4-year Incidence and Progression of Visual Impairment in the Los Angeles Latino Eye Study.
Table 1.
Comparison of Los Angeles Latino Eye Study Participants and Nonparticipants in the 4-year Incidence Study
| Participants* N = 4658 |
Nonparticipants† N = 1442 |
P‡ | ||||
|---|---|---|---|---|---|---|
| Characteristics | n | % | n | % | ||
| Gender (female) | 2801 | 60% | 802 | 56% | <0.003 | |
| Age group | ||||||
| Mean (± SD) | 54.7 | 10.5 | 53.1 | 10.7 | < 0.001 | |
| 40–49 | 1763 | 38% | 660 | 46% | < 0.001 | |
| 50–59 | 1462 | 31% | 427 | 30% | ||
| 60–69 | 938 | 20% | 220 | 15% | ||
| 70–79 | 409 | 9% | 107 | 7% | ||
| 80+ | 86 | 2% | 28 | 2% | ||
| Country of birth (United States) | 1094 | 24% | 315 | 22% | 0.20 | |
| Acculturation (low |<1.9|) | 1537 | 33% | 447 | 31% | 0.17 | |
| Working status (employed) | 2323 | 50% | 746 | 52% | 0.19 | |
| Education level ≥ 12 years | 1576 | 34% | 467 | 32% | 0.33 | |
| Marital status (married) | 3279 | 71% | 959 | 67% | 0.01 | |
| Income level > $40,000 | 582 | 13% | 183 | 13% | 0.83 | |
| Health insurance | 3119 | 67% | 773 | 54% | <0.001 | |
| ≥ 2 comorbidities§ | 1903 | 41% | 492 | 34% | <0.001 | |
| Self-reported health excellent/very good |
884 | 19% | 288 | 20% | 0.38 | |
| History of hypertension | 1392 | 30% | 368 | 26% | 0.002 | |
| History of diabetes | 868 | 19% | 235 | 16% | 0.05 | |
| Self-reported vision excellent/good | 1940 | 42% | 594 | 38% | 0.02 | |
| In-home binocular near vision better than 20/40 |
214 | 5% | 89 | 6% | 0.02 | |
| History of any ocular disease | 616 | 13% | 152 | 11% | 0.01 | |
| History of cataract | 472 | 10% | 109 | 8% | 0.004 | |
| History of glaucoma | 118 | 3% | 41 | 3% | 0.51 | |
| History of macular degeneration | 33 | 1% | 10 | 1% | 0.96 | |
| History of diabetic retinopathy | 99 | 2% | 21 | 2% | 0.11 | |
Participants completing the clinical examination at follow-up.
Nonparticipants of the follow-up examination who had participated in the baseline examination (Include persons who refused the follow-up examination).
Chi-square test for categorical variables, t test for continuous variables.
Co-morbidities refer to the summation of the following medical conditions: arthritis, diabetes, back pain, hypertension, deafness, asthma, angina, skin cancer, other cancers, heart disease, stroke, and heart failure.
Incidence of Binocular Visual Impairment and Blindness
The 4-year incidence of presenting binocular visual impairment (US Criterion) in the overall cohort at risk was 2.9% (95% CI: 2.4%, 3.4%).(Table 2) The four year incidence of presenting binocular blindness (US Criterion) was 0.3% (95% CI: 0.2%, 0.5%). The incidence of both conditions increased significantly (P<0.001) with age of the participant at the time of the baseline examination. For example, over the 4-year period, the incidence of presenting binocular visual impairment (US criterion) in those age 80 years and older (19.4%) was thirteen fold higher than those aged 40–49 years at baseline (1.4%). Similarly, the incidence of presenting binocular blindness (US Criterion) in those age 80 years and older (3.8%) was seven fold higher than those aged 50–59 years at baseline (0.5%).
Table 2.
Four-year Incidence of Presenting Binocular Visual Impairment stratified by Age at Baseline in Participants in the Los Angeles Latino Eye Study
| Age at baseline (years) |
Incidence of Visual Impairment | Incidence of Blindness | ||||
|---|---|---|---|---|---|---|
| N | n | % (CI) | N | n | % (CI) | |
| United States Criterion* | ||||||
| 40–49 | 1739 | 25 | 1.4 (0.9, 2.0) | 1753 | 0 | NA |
| 50–59 | 1422 | 27 | 1.9 (1.2, 2.6) | 1453 | 7 | 0.5 (0.1, 0.8) |
| 60–69 | 888 | 31 | 3.5 (2.3, 4.7) | 934 | 5 | 0.5 (0.1, 1.0) |
| 70–79 | 371 | 34 | 9.2 (6.2, 12.1) | 398 | 1 | 0.3 (0.0, 0.7) |
| 80+ | 62 | 12 | 19.4 (9.5, 29.2) | 78 | 3 | 3.8 (0.0, 8.1) |
| P < 0.001 | P < 0.001 | |||||
| Crude Overall | 4482 | 129 | 2.9 (2.4, 3.4) | 4616 | 16 | 0.3 (0.2, 0.5) |
| Age standardized# | 3.0 (2.5, 3.5) | 0.4 (0.2, 0.6) | ||||
| World Health Organization Criterion† | ||||||
| 40–49 | 1747 | 14 | 0.8 (0.4, 1.2) | 1754 | 0 | NA |
| 50–59 | 1438 | 17 | 1.2 (0.6, 1.7) | 1453 | 5 | 0.3 (0.0, 0.6) |
| 60–69 | 912 | 24 | 2.6 (1.6, 3.7) | 937 | 0 | 0,NA |
| 70–79 | 386 | 19 | 4.9 (2.8, 7.1) | 402 | 2 | 0.5 (0.0, 1.2) |
| 80+ | 71 | 10 | 14.1 (6.0, 22.2) | 81 | 3 | 3.7 (0.0, 7.8) |
| P < 0.001 | P < 0.001 | |||||
| Crude Overall | 4554 | 84 | 1.8 (1.5, 2.2) | 4627 | 10 | 0.2 (0.1, 0.3) |
| Age-standardized# | 1.9 (1.5, 2.3) | 0.2 (0.1, 0.3) | ||||
N= number at risk at baseline; n= incident cases; % (CI)= prevalence and 95 percent confidence interval. P = Test of trend.
U.S. Criterion 1. Incidence of visual impairment: Persons with Baseline presenting binocular visual acuity (PVA) of 20/40 or better and follow-up PVA worse than 20/40 but better than 20/200 (not including 20/40 or 20/200). Incidence of Blindness: Persons with Baseline PVA better than 20/200 and follow-up PVA 20/200 or worse (including 20/200).
W.H.O. Criterion. Incidence of visual impairment: Persons with Baseline PVA 20/60 or better and follow-up PVA worse than 20/60 but better than or equal to 20/400 (not including 20/60 but including 20/400). Incidence of Blindness: Persons with Baseline PVA 20/400 or better and follow-up PVA worse 20/400 (not including 20/400).
NA: No incident cases.
Age-standardized to the LALES population.
Incidence of Visual Impairment and Blindness in the Best Corrected Better Seeing Eye
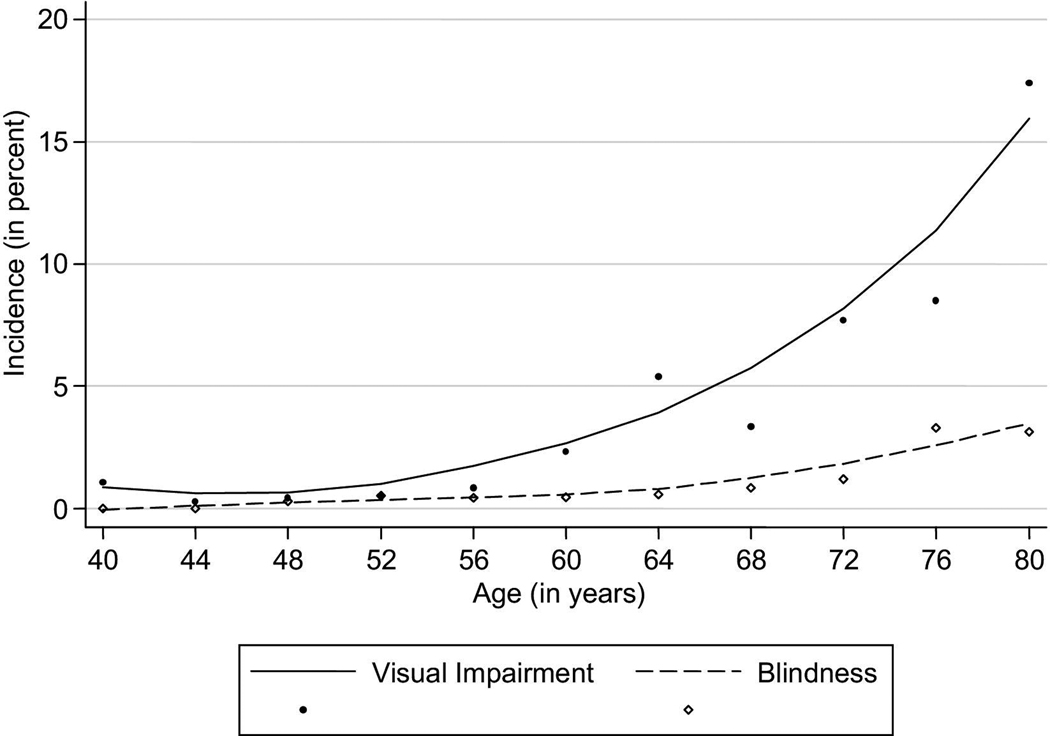
The 4-year incidence of visual impairment using the US and WHO criteria were 1.2% and 0.7% respectively.(Table 3) The four year incidence of blindness using the US and WHO criteria were 0.3% and 0.2% respectively. The incidence of both conditions increased significantly (P<0.001) with age at baseline. For example, over the 4-year period, the incidence of visual impairment in the best corrected better seeing eye (US criterion) in those age 80 years and older (14.1%) was twenty eight-fold higher than those aged 40–49 years at baseline (0.5%). Similarly, the incidence of blindness in the best corrected better seeing eye (US Criterion) in those age 80 years and older (2.5%) was six-fold higher than those aged 50–59 years at baseline (0.3%). LOWESS plots of the combined 4-year incidence of visual impairment and blindness using United States criterion (Figure 3) demonstrated strong associations with older age. Incidence of visual impairment and blindness both showed gradual increase across all age-groups.
Table 3.
Four-year Incidence of Best corrected Visual Impairment and Blindness Stratified by Age at Baseline in Participants in the Los Angeles Latino Eye Study
| Age at baseline (years) |
Incidence of Visual Impairment | Incidence of Blindness | ||||
|---|---|---|---|---|---|---|
| N | n | % (CI) | N | n | % (CI) | |
| United States Criterion* | ||||||
| 40–49 | 1751 | 8 | 0.5 (0.1, 0.8) | 1754 | 0 | NA |
| 50–59 | 1444 | 6 | 0.4 (0.1, 0.7) | 1446 | 5 | 0.3 (0.0, 0.6) |
| 60–69 | 913 | 15 | 1.6 (0.8, 2.5) | 931 | 3 | 0.3 (0.0, 0.7) |
| 70–79 | 383 | 16 | 4.2 (2.2, 6.2) | 397 | 2 | 0.5 (0.0, 1.2) |
| 80+ | 71 | 10 | 14.1 (6.0, 22.2) | 79 | 2 | 2.5 (0.0, 6.0) |
| P < 0.001 | P < 0.001 | |||||
| Crude Overall | 4562 | 55 | 1.2 (0.9, 1.5) | 4607 | 12 | 0.3 (0.1, 0.4) |
| Age-standardized# | 1.3 (1.0, 1.6) | 0.3 (0.1, 0.5) | ||||
| World Health Organization Criterion† | ||||||
| 40–49 | 1751 | 2 | 0.1 (0.0, 0.3) | 1755 | 0 | NA |
| 50–59 | 1444 | 4 | 0.3 (0.0, 0.5) | 1446 | 4 | 0.3 (0.0, 0.5) |
| 60–69 | 922 | 12 | 1.3 (0.6, 2.0) | 932 | 0 | NA |
| 70–79 | 394 | 9 | 2.3 (0.8, 3.8) | 400 | 1 | 0.3 (0.0, 0.7) |
| 80+ | 74 | 7 | 9.5 (2.8, 16.1) | 81 | 2 | 2.5 (0.0, 5.8) |
| P < 0.001 | P = 0.005 | |||||
| Crude Overall | 4585 | 34 | 0.7 (0.5, 1.0) | 4614 | 7 | 0.2 (0.0, 0.3) |
| Age-standardized# | 0.8 (0.5, 1.1) | 0.2 (0.1, 0.3) | ||||
N= number at risk at baseline; n= incident cases; % (CI)= prevalence and 95 percent confidence interval; P = Test of trend.
U.S. Criterion. Incidence of visual impairment: Person with Baseline best corrected visual acuity (BCVA) of 20/40 or better in better seeing-eye, and follow-up BCVA worse than 20/40 but better than 20/200 (not including 20/40 or 20/200) in better seeing-eye. Incidence of Blindness: Persons with Baseline BCVA better than 20/200 in the better seeing eye and follow-up BCVA 20/200 or worse (including 20/200).
W.H.O. Criterion.Incidence of visual impairment: Persons with Baseline BCVA 20/60 or better in better seeing-eye and follow-up BCVA worse than 20/60 but better than or equal to 20/400 (not including 20/60 but including 20/400) in the better seeing-eye. Incidence of Blindness: Persons with Baseline BCVA 20/400 or better in better seeing-eye and follow-up BCVA worse 20/400 (not including 20/400) in better seeing-eye.
NA: No incident cases.
Age-standardized to the LALES population.
Figure 3.
Age-specific Four-year Incidence of Visual Impairment and Blindness in the Los Angeles Latino Eye Study*
*United States Criteria: Visual Impairment: Baseline = BCVA 20/40 or better in one or both eyes. Follow-up = BCVA worse than 20/40 but better than 20/200 in the better-seeing eye (not including 20/40 or 20/200).
Incidence of Monocular Visual Impairment and Blindness - First Eye, Second Eye and Either Eye
The 4-year incidence of monocular visual impairment and blindness using modified US and WHO criteria is presented in Tables 4 and 5, respectively. More than 95% of participants were bilaterally unimpaired at baseline (had no visual impairment or blindness in either eye). In general, as expected based on the criteria, the incidence of monocular visual impairment and blindness was lower using the modified WHO criterion compared to the US criterion. As with binocular visual impairment, the incidence of monocular impairment increased significantly with age. For example, using modified US criteria, the incidence of monocular visual impairment in those bilaterally unimpaired at baseline (developing visual impairment in the first eye) was 20-fold higher in persons aged 80 years and older (14.6%) compared to those aged 40–49 years (0.7%) at baseline. Similarly using modified US criteria, the incidence of monocular blindness in those not blind in either eye baseline (becoming blind in the first eye) was 28-fold higher in persons aged 80 years and older (5.6%) compared to those aged 40–49 years (0.2%) at baseline.
Table 4.
Four-year Incidence of Monocular Best Corrected Visual Impairment in the Los Angeles Latino Eye Study
| Age at baseline (years) |
Incidence in 1st Eye | Incidence in 2nd Eye | Incidence in Either Eye ∥ | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | n | % (CI) | N | n | % (CI) | N | n | % (CI) | |
| United States Criterion* | |||||||||
| 40–49 | 1704 | 12 | 0.7 (0.3, 1.1) | 44 | 2 | 4.5 (0.0, 10.7) | 1748 | 14 | 0.8 (0.4, 1.2) |
| 50–59 | 1393 | 18 | 1.3 (0.7, 1.9) | 50 | 1 | 2.0 (0.0, 5.9) | 1443 | 19 | 1.3 (0.7, 1.9) |
| 60–69 | 845 | 45 | 5.3 (3.8, 6.8) | 64 | 7 | 10.9 (3.3, 18.6) | 909 | 52 | 5.7 (4.2, 7.2) |
| 70–79 | 329 | 44 | 13.4 (9.7, 17.1) | 44 | 10 | 22.7 (10.3, 35.1) | 373 | 54 | 14.5 (10.9, 18.0) |
| 80+ | 48 | 7 | 14.6 (4.6, 24.6) | 19 | 7 | 36.8 (15.2, 58.5) | 67 | 14 | 20.9 (11.2, 30.6) |
| P < 0.001 | P < 0.001 | P < 0.001 | |||||||
| Crude Overall | 4319 | 126 | 2.9 (2.4, 3.4) | 221 | 27 | 12.2 (7.9, 16.5) | 4540 | 153 | 3.4 (2.8, 3.9) |
| Age-standardized# | 3.2 (2.6, 3.8) | 7.3 (4.5, 10.1) | 3.6 (3.0, 4.1) | ||||||
| World Health Organization Criterion† | |||||||||
| 40–49 | 1719 | 10 | 0.6 (0.2, 0.9) | 30 | 0 | NA | 1749 | 10 | 0.6 (0.2, 0.9) |
| 50–59 | 1409 | 13 | 0.9 (0.4, 1.4) | 35 | 1 | 2.9 (0.0, 8.4) | 1444 | 14 | 1.0 (0.5, 1.5) |
| 60–69 | 862 | 24 | 2.8 (1.7, 3.9) | 56 | 6 | 10.7 (2.6, 18.8) | 918 | 30 | 3.3 (2.1, 4.4) |
| 70–79 | 355 | 38 | 10.7 (7.5, 13.9) | 33 | 4 | 12.1 (1.0, 23.3) | 388 | 42 | 10.8 (7.7, 13.9) |
| 80+ | 60 | 8 | 13.3 (4.7, 21.9) | 12 | 6 | 20.0 (21.7, 78.3) | 72 | 14 | 19.4 (10.3, 28.6) |
| P < 0.001 | P < 0.001 | P < 0.001 | |||||||
| Crude Overall | 4405 | 93 | 2.1 (1.7, 2.5) | 166 | 17 | 10.2 (2.6, 14.9) | 4571 | 110 | 2.4 (2.0, 2.9) |
| Age-standardized# | 2.3 (1.8, 2.8) | 5.1 (2.7, 7.5) | 2.5 (2.0, 3.0) | ||||||
N= number at risk at baseline; n= incident cases; % (CI)= prevalence and 95 percent confidence interval; P = Test of trend.
US modified Criterion. Incidence of visual impairment: Persons with Baseline best-corrected visual acuity (BCVA) 20/40 or better in the 1st or 2nd eye and follow-up BCVA worse than 20/40 but better than 20/200 (not including 20/40 or 20/200) in the 1st or 2nd eye.
W.H.O. modified Criterion. Incidence of visual impairment: Persons with Baseline BCVA 20/60 or better in the 1st or 2nd eye and follow-up BCVA worse than 20/60 but better than or equal to 20/400 (not including 20/60 but including 20/400) in the 1st or 2nd eye.
This column combines the at-risk cohorts for incidence in the first eye and incidence in the second eye.
NA: No incident cases.
Age-standardized to the LALES population.
Table 5.
Four-year Incidence of Monocular Blindness in the Los Angeles Latino Eye Study
| Age at baseline (years) |
Incidence in 1st Eye | Incidence in 2nd Eye | Incidence in Either Eye ∥ | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | n | % (CI) | N | n | % (CI) | N | n | % (CI) | |
| United States Criterion* | |||||||||
| 40–49 | 1733 | 4 | 0.2 (0.0, 0.5) | 22 | 0 | NA | 1755 | 4 | 0.2 (0.0, 0.5) |
| 50–59 | 1431 | 10 | 0.7 (0.3, 1.1) | 22 | 4 | 18.7 (2.1, 34.3) | 1453 | 14 | 1.0 (0.5, 1.5) |
| 60–69 | 911 | 21 | 2.3 (1.3, 3.3) | 24 | 0 | NA | 935 | 21 | 2.2 (1.3, 3.2) |
| 70–79 | 383 | 15 | 3.9 (2.0, 5.9) | 16 | 2 | 12.5 (0.0, 28.7) | 399 | 17 | 4.3 (2.3, 6.2) |
| 80+ | 71 | 4 | 5.6 (0.3, 11.0) | 8 | 1 | 12.5 (0.0, 35.4) | 79 | 5 | 6.3 (1.0, 11.7) |
| P < 0.001 | P = 0.418 | P < 0.001 | |||||||
| Crude Overall | 4529 | 54 | 1.2 (0.9, 1.5) | 92 | 7 | 7.6 (2.2, 13.0) | 4621 | 61 | 1.3 (1.0, 1.6) |
| Age-standardized# | 1.2 (0.9, 1.5) | 7.0 (1.8, 12.2) | 1.3 (1.0, 1.7) | ||||||
| World Health Organization Criterion† | |||||||||
| 40–49 | 1745 | 8 | 0.5 (0.1, 0.8) | 11 | 0 | NA | 1756 | 8 | 0.5 (0.1, 0.8) |
| 50–59 | 1437 | 6 | 0.4 (0.1, 0.8) | 16 | 3 | 18.8 (0.0, 37.9) | 1453 | 9 | 0.6 (0.2, 1.0) |
| 60–69 | 919 | 14 | 1.5 (0.7, 2.3) | 17 | 0 | NA | 936 | 14 | 1.5 (0.7, 2.3) |
| 70–79 | 391 | 9 | 2.3 (0.8, 3.8) | 11 | 1 | 9.1 (0.0, 26.1) | 402 | 10 | 2.5 (1.0, 4.0) |
| 80+ | 76 | 5 | 6.6 (1.0, 12.2) | 5 | 1 | 20.0 (0.0, 55.1) | 81 | 6 | 7.4 (1.7, 13.1) |
| P < 0.001 | P = 0.581 | P < 0.001 | |||||||
| Crude Overall | 4568 | 42 | 0.9 (0.6, 1.2) | 60 | 5 | 8.3 (1.3, 15.3) | 4628 | 47 | 1.0 (0.7, 1.3) |
| Age-standardized# | 0.9 (0.6, 1.2) | 7.0 (0.9, 13.1) | 1.0 (0.7, 1.3) | ||||||
N=number at risk at baseline; n= incident cases; % (CI)= prevalence and 95 percent confidence interval; P = Test of trend.
US Modified Criterion. Incidence of Monocular Blindness (1st or 2nd eye): Persons with Baseline BCVA better than 20/200 in the 1st or 2nd eye and follow-up BCVA 20/200 or worse (including 20/200) in the 1st or 2nd eye.
W.H.O. modified Criterion. Incidence of Monocular Blindness (1st or 2nd eye): Persons with Baseline BCVA 20/400 or better in the 1st or 2nd eye and follow-up BCVA worse than 20/400 (not including 20/400) in the 1st or 2nd eye.
This column combines the incidence in the first eye and incidence in the second eye.
NA: No incident cases.
Age-standardized to the LALES population.
The 4-year risk of developing visual impairment or blindness in the second eye was higher than the risk of developing visual impairment or blindness in the first eye (Tables 4 and 5). Thus, persons who have pre-existing visual impairment or blindness in one eye are more likely to develop visual impairment or blindness in the second eye compared to those who have no visual impairment in either eye (Tables 4 and 5). For example, using modified US criteria and age-standardization, the incidence of monocular visual impairment in those visually impaired in one eye at baseline (developing visual impairment in the second eye) was twice as high (7.3%) compared to those who had no visual impairment in both eye at baseline (3.2%). Similar to the rates seen for incidence in the first eye, there also appears to be an age-related trend for developing visual impairment in the second eye. The age-specific rates for visual impairment (based on best corrected visual acuity using US criterion) in the second eye were 8 fold higher in persons 80 years and older (36.8%) compared to those aged 40–49 years (4.5%) at baseline, No age–related trend was present for the incidence of blindness in the second eye, probably due to a limited number of persons developing blindness. The overall incidence for blindness in the second eye is 7.6% and 8.3% for the modified US and WHO criteria, respectively.
Table 4 and 5 also show the combined incidence rates from the first eye and the second eye – incidence in either eye. Using the modified US criterion, 3.4% of persons developed visual impairment in either eye and 1.3% became monocularly blind in either eye. Similar to the increases in the incidence of visual impairment in the first and second eyes in older persons compared to younger persons older Latinos had higher incidences of visual impairment and blindness in either eye.
Worsening and Improvement in Binocular Presenting Visual Acuity
Over 4 years, loss of ≥5, 10, and 15 letters of binocular presenting visual acuity occurred in 24.8%, 8.5%, and 3.1% of participants at risk, respectively (Table 6). Persons who were older at the baseline examination were more likely to have a worsening in their presenting binocular visual acuity compared to those who were younger. (P<0.001) Improvements of ≥5, 10, and 15 letters of binocular presenting visual acuity occurred in 12.7%, 4.6% and 3.9% of individuals at risk, respectively. Persons who were older at the baseline examination were also more likely to have an improvement (of ≥5 and 10 letters but not 15 letters) in their presenting binocular visual acuity compared to those who were younger. (P<0.03)
Table 6.
Severity of Worsening and Improvement of Presenting Binocular Visual Acuity over a 4-year Period Stratified by Age at Baseline in Participants of the Los Angeles Latino Eye Study
| Binocular Worsening* | Binocular Improvement† | |||||||
|---|---|---|---|---|---|---|---|---|
| Age at baseline (years) | N | n | % (CI) | P | N | n | % (CI) | P |
| ≥ 15 letters change | ||||||||
| 40–49 | 1756 | 35 | 2.0 (1.3, 2.6) | <0.001 | 315 | 14 | 4.4 (2.2, 6.7) | 0.379 |
| 50–59 | 1451 | 40 | 2.8 (1.9, 3.6) | 419 | 19 | 4.5 (2.5, 6.5) | ||
| 60–69 | 938 | 34 | 3.6 (2.4, 4.8) | 438 | 14 | 3.2 (1.5, 4.8) | ||
| 70–79 | 403 | 28 | 6.9 (4.5, 9.4) | 282 | 9 | 3.2 (1.1, 5.2) | ||
| 80+ | 82 | 8 | 9.8 (3.3, 16.2) | 68 | 3 | 4.4 (0.0, 9.3) | ||
| Total | 4630 | 145 | 3.1 (2.6, 3.6) | 1522 | 59 | 3.9 (2.9, 4.8) | ||
| ≥ 10 letters change | ||||||||
| 40–49 | 1756 | 105 | 6.0 (4.9, 7.1) | <0.001 | 1251 | 44 | 3.5 (2.5, 4.5) | 0.021 |
| 50–59 | 1451 | 106 | 7.3 (6.0, 8.6) | 1247 | 59 | 4.7 (3.6, 5.9) | ||
| 60–69 | 938 | 99 | 10.6 (8.6, 12.5) | 872 | 46 | 5.3 (3.8, 6.8) | ||
| 70–79 | 403 | 67 | 16.6 (13.0, 20.3) | 395 | 21 | 5.3 (3.1, 7.5) | ||
| 80+ | 82 | 18 | 22.0 (13.0, 30.9) | 83 | 6 | 7.2 (1.7, 12.8) | ||
| Total | 4630 | 395 | 8.5 (7.7, 9.3) | 3848 | 176 | 4.6 (3.9, 5.2) | ||
| ≥ 5 letters change | ||||||||
| 40–49 | 1756 | 388 | 22.1 (20.2, 24.0) | <0.001 | 1636 | 166 | 10.1 (8.7, 11.6) | < 0.001 |
| 50–59 | 1451 | 344 | 23.7 (21.5, 25.9) | 1429 | 185 | 12.9 (11.2, 14.7) | ||
| 60–69 | 938 | 252 | 26.9 (24.0, 29.7) | 935 | 141 | 15.1 (12.8, 17.4) | ||
| 70–79 | 403 | 135 | 33.5 (28.9, 38.1) | 405 | 64 | 15.8 (12.2, 19.4) | ||
| 80+ | 82 | 31 | 37.8 (27.3, 48.3) | 83 | 13 | 15.7 (7.8, 23.5) | ||
| Total | 4630 | 1150 | 24.8 (23.6, 26.1) | 4488 | 569 | 12.7 (11.7, 13.7) | ||
N= number at risk at baseline; n= incident cases; % (CI)= prevalence and 95 percent confidence interval; P = Test of trend.
Binocular worsening: Persons at Baseline with Presenting visual acuity (PVA) better than no light perception and at follow-up with Loss of 15 or more, 10 or more, or 5 or more letters read correctly.
Binocular improvement: Persons at Baseline capable of improving by 5 or more, 10 or more, or 15 or more letters read correctly at presenting, and at follow-up had an increase of 5 or more, 10 or more, or 15 or more letters read correctly.
Monocular Worsening and Improvement in Best Corrected Visual Acuity
Four-year monocular worsening of ≥5, 10, and 15 letters in either eye occurred in 30%, 8.8% and 4.3% of persons at risk, respectively (Table 7). In each vision loss stratum, participants at risk who were older at baseline were significantly (P<0.001) more likely to experience worsening. The four-year monocular improvement of ≥5, 10, and 15 letters in either eye occurred in 16.6%, 3.3% and 2.9% of persons at risk, respectively (Table 8). The proportions of persons with improvement in either eye generally increased with increasing age.
Table 7.
Severity of Worsening of Monocular Best Corrected Visual Acuity over a 4 year period Stratified by Age at Baseline in Participants of the Los Angeles Latino Eye Study
| Worsening in either eye* | Worsening in the better-seeing eye† | |||||||
|---|---|---|---|---|---|---|---|---|
| Age at baseline (years) | N | n | % (CI) | P | N | n | % (CI) | P |
| ≥ 15 letters worsening | ||||||||
| 40–49 | 1754 | 23 | 1.3 (0.8, 1.8) | <0.001 | 1754 | 14 | 0.8 (0.4, 1.2) | <0.001 |
| 50–59 | 1442 | 39 | 2.7 (1.9, 3.5) | 1442 | 26 | 1.8 (1.1, 2.5) | ||
| 60–69 | 932 | 63 | 6.8 (5.1, 8.4) | 932 | 32 | 3.4 (2.3, 4.6) | ||
| 70–79 | 400 | 56 | 14.0 (10.6, 17.4) | 400 | 28 | 7.0 (4.5, 9.5) | ||
| 80+ | 81 | 18 | 22.2 (13.2, 31.3) | 81 | 13 | 16.0 (8.1, 24.0) | ||
| Total | 4609 | 199 | 4.3 (3.7, 4.9) | 4609 | 113 | 2.5 (2.0, 2.9) | ||
| ≥ 10 letters worsening | ||||||||
| 40–49 | 1754 | 67 | 3.8 (2.9, 4.7) | <0.001 | 1754 | 45 | 2.6 (1.8, 3.3) | <0.001 |
| 50–59 | 1442 | 79 | 5.5 (4.3, 6.7) | 1442 | 47 | 3.3 (2.3, 4.2) | ||
| 60–69 | 932 | 134 | 14.4 (12.1, 16.6) | 932 | 85 | 9.1 (7.3, 11.0) | ||
| 70–79 | 400 | 99 | 24.8 (20.5, 29.0) | 400 | 58 | 14.5 (11.0, 18.0) | ||
| 80+ | 81 | 25 | 30.9 (20.8, 40.9) | 81 | 19 | 23.5 (14.2, 32.7) | ||
| Total | 4609 | 404 | 8.8 (7.9, 9.6) | 4609 | 25 | 5.5 (4.9, 6.2) | ||
| ≥ 5 letters worsening | ||||||||
| 40–49 | 1754 | 417 | 23.8 (21.8, 25.8) | <0.001 | 1754 | 326 | 18.6 (16.8, 20.4) | <0.001 |
| 50–59 | 1442 | 362 | 25.1 (22.9, 27.3) | 1442 | 278 | 19.3 (17.2, 21.3) | ||
| 60–69 | 932 | 342 | 36.7 (33.6, 39.8) | 932 | 255 | 27.4 (24.5, 30.2) | ||
| 70–79 | 400 | 220 | 55.0 (50.1, 59.9) | 400 | 166 | 41.5 (36.7, 46.3) | ||
| 80+ | 81 | 44 | 54.3 (43.5, 65.2) | 81 | 34 | 42.0 (31.2, 52.7) | ||
| Total | 4609 | 1385 | 30.0 (28.7, 31.4) | 4609 | 1059 | 23.0 (21.8, 24.2) | ||
N= number at risk at baseline; n= incident cases; % (CI)= prevalence and 95 percent confidence interval; P = Test of trend.
Criterion for Worsening in either eye (one eye only): Persons with incident worsening were those with a baseline best-corrected visual acuity (BCVA) of light perception or better in both eyes and a loss of 15 or more, 10 or more, or 5 or more letters read correctly at follow-up compared to baseline in the eye which was the worse-seeing eye at baseline.
Criterion for Worsening in the better-seeing eye: Persons with incident worsening were those with a baseline BCVA of light perception or better in one or both eyes and with a loss of 15 or more, 10 or more, or 5 or more letters read correctly at follow-up compared to baseline in the eye which was the better-seeing eye at baseline.
Table 8.
Level of Improvement of Monocular Best Corrected Visual Acuity over a 4 year Period Stratified by Age at Baseline in Participants of the Los Angeles Latino Eye Study
| Improvement in either eye* | Improvement in the worse-seeing eye† | |||||||
|---|---|---|---|---|---|---|---|---|
| Age at baseline (years) | N | n | % (CI) | P | N | n | % (CI) | P |
| ≥ 15 letters improvement | ||||||||
| 40–49 | 687 | 4 | 0.6 (0.0, 1.2) | <0.001 | 687 | 4 | 0.6 (0.0, 1.2) | <0.001 |
| 50–59 | 711 | 12 | 1.7 (0.7, 2.6) | 711 | 11 | 1.5 (0.6, 2.5) | ||
| 60–69 | 596 | 25 | 4.2 (2.6, 5.8) | 596 | 24 | 4.0 (2.4, 5.6) | ||
| 70–79 | 333 | 23 | 6.9 (4.2, 9.6) | 333 | 22 | 6.6 (3.9, 9.3) | ||
| 80+ | 77 | 6 | 7.8 (1.8, 13.8) | 77 | 5 | 6.5 (1.0, 12.0) | ||
| Total | 2404 | 70 | 2.9 (2.2, 3.6) | 2404 | 66 | 2.7 (2.1, 3.4) | ||
| ≥ 10 letters improvement | ||||||||
| 40–49 | 1644 | 29 | 1.8 (1.1, 2.4) | <0.001 | 1644 | 21 | 1.3 (0.7, 1.8) | <0.001 |
| 50–59 | 1405 | 26 | 1.9 (1.1, 2.6) | 1405 | 24 | 1.7 (1.0, 2.4) | ||
| 60–69 | 919 | 45 | 4.9 (3.5, 6.3) | 919 | 42 | 4.6 (3.2, 5.9) | ||
| 70–79 | 401 | 35 | 8.7 (6.0, 11.5) | 401 | 30 | 7.5 (4.9, 10.1) | ||
| 80+ | 83 | 11 | 13.3 (6.0, 20.5) | 83 | 11 | 13.3 (6.0, 20.5) | ||
| Total | 4452 | 146 | 3.3 (2.8, 3.8) | 4452 | 128 | 2.9 (2.4, 3.4) | ||
| ≥ 5 letters improvement | ||||||||
| 40–49 | 1752 | 198 | 17.0 (15.2, 18.8) | 0.618 | 1752 | 192 | 11.0 (9.5, 12.4) | 0.002 |
| 50–59 | 1444 | 231 | 16.0 (14.1, 17.9) | 1444 | 158 | 10.9 (9.3, 12.6) | ||
| 60–69 | 933 | 142 | 15.2 (12.9, 17.5) | 933 | 104 | 11.1 (9.1, 13.2) | ||
| 70–79 | 402 | 77 | 19.2 (15.3, 23.0) | 402 | 66 | 16.4 (12.8, 20.0) | ||
| 80+ | 83 | 18 | 21.7 (12.8, 30.6) | 83 | 18 | 21.7 (12.8. 30.6) | ||
| Total | 4614 | 766 | 16.6 (15.5, 17.7) | 4614 | 538 | 11.7 (10.7, 12.6) | ||
N= number at risk at baseline; n= incident cases; % (CI)= prevalence and 95 percent confidence interval; P = Test of trend.
Criterion for Improvement in either eye (one eye only): Persons capable of improving from Baseline by 5 or more, 10 or more, or 15 or more letters read correctly and at follow-up had an increase of 5 or more, 10 or more, or 15 or more letters read correctly in the better-seeing eye.
Criterion for Improvement in the worse-seeing eye: Persons capable of improving from Baseline by 5 or more, 10 or more, or 15 or more letters read correctly and at follow-up had an increase of 5 or more, 10 or more, or 15 or more letters read correctly in the worse-seeing eye.
DISCUSSION
LALES data provide the first observed incidence estimates of visual impairment and blindness in a large population of Latinos of primarily Mexican ancestry in the U.S. The results demonstrate a high incidence of both visual impairment and blindness and high rates of worsening of visual acuity. The 4-year incidence of binocular visual impairment was 2.9% and of blindness was 0.3%. Based on US and WHO criteria, the overall 4-year incidence of monocular visual impairment in the first eye was 2.9% and 1.6%, respectively, while the incidence of blindness was 1.2% and 0.9%, respectively. Furthermore, worsening of binocular vision by ≥5 letters over 4 years was experienced by nearly one quarter of persons at risk, and a similar worsening in monocular vision was demonstrated in nearly 30% of participants.
As has been previously noted 2, 3, 12, 15–19 the incidence of visual impairment and progression increased with age. Based on binocular measures and using the US criterion, the 4-year incidence of visual impairment was 19.4% in persons 80 or older and of blindness was 3.8%. Similarly the 4-year incidence rates for monocular visual impairment and blindness in the first eye were 14.6% and 5.6%, respectively. These high rates of incidence underscore the importance of targeting older Latinos in screening programs and public health messages. Improvement in both binocular and monocular vision by ≥5 letters occurred in over 10% of persons. Such improvements presumably were related to cataract removal, correction of refractive error, or other ophthalmic interventions.
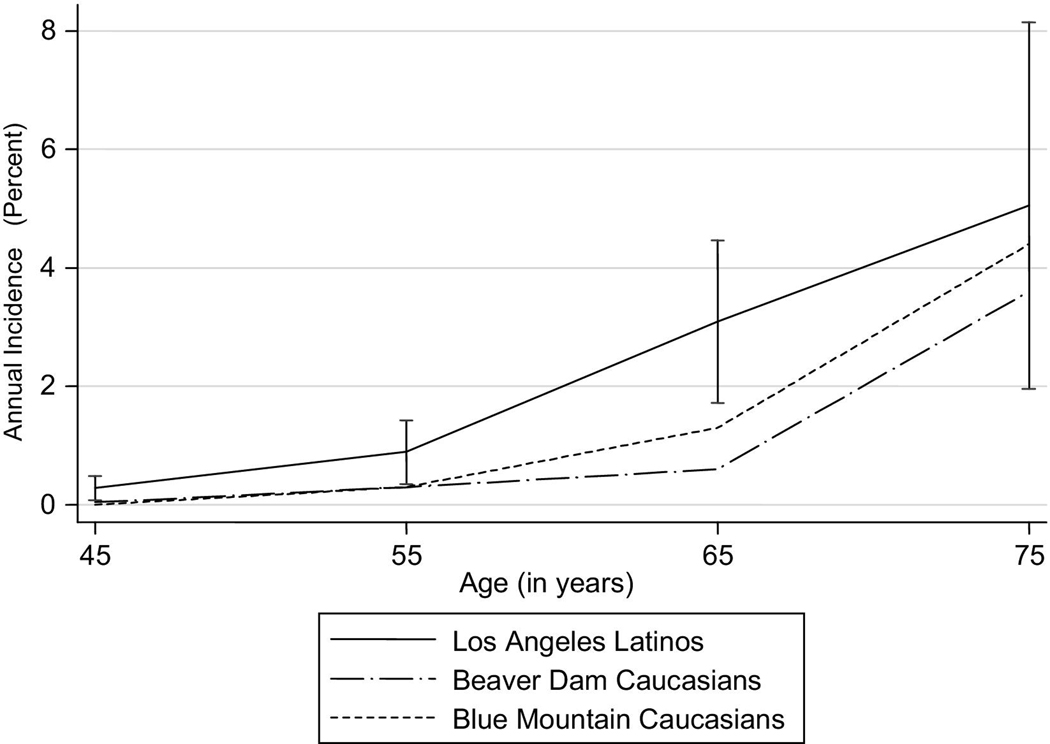
Despite differences among LALES, BMES, BDES, and BISED with regard to study designs, populations, and data collection methods, it is of interest to compare estimates of the incidence of visual impairment. Overall, the estimated annual incidence of visual impairment and blindness (severe visual impairment) in the better-seeing eye at baseline in the LALES population was greater to the incidence reported in BDES and BMES (Table 9 and Figure 4). Furthermore, the estimated annual rates of worsening and improvement in the better-seeing eye at baseline were also higher in LALES compared to BMES, and BDES (Table 10). However, these differences were not significantly different due to small numbers of persons developing visual impairment and blindness. In all three populations, persons who were older at baseline were more likely to experience worsening and improvement than younger individuals. A comparison of the 4-year incidence of visual impairment and blindness in BISED, which included an Afro-Caribbean population, and LALES (using United States criteria), illustrates that the incidence of visual impairment in BISED was approximately 2.6 times higher than that reported in LALES (1.3% vs. 0.5%, respectively), while that of blindness was two times higher in BISED (0.4% vs. 0.2%, respectively). Irrespective of the criteria used, older age was associated with increased incidence of visual impairment and blindness all populations.
Table 9.
Comparison of Estimated Annual Incidence§ of Visual Impairment and Blindness Stratified by Age in non-Hispanic Whites in Beaver Dam, Wisconsin Blue Mountains, Australia and Los Angeles Latinos.
| LALES |
BDES |
BMES |
||||
|---|---|---|---|---|---|---|
| Age at baseline (years) | N | % (CI) | N | % (CI) | N | % (CI) |
| Any Visual Impairment* | ||||||
| <55 | 2578 | 0.3 (0.1, 0.5) | 1230 | 0.04 (0.0, 0.2) | 331 | ‡ |
| 55–64 | 1150 | 0.9 (0.4, 1.4) | 1022 | 0.3 (0.00, 0.6) | 844 | 0.3 (0.0, 0.7) |
| 65–74 | 614 | 3.1 (1.7, 4.5) | 894 | 0.6 (0.1, 1.2) | 806 | 1.3 (0.6, 2.1) |
| 75+ | 193 | 5.1 (2.0, 8.1) | 318 | 3.6 (1.5, 5.6) | 307 | 4.4 (2.1, 6.7) |
| Blindness (Severe visual impairment)† | ||||||
| <55 | 2592 | 0.07 (0.0, 0.2) | 1238 | ‡ | 333 | ‡ |
| 55–64 | 1164 | 0.1 (0.0, 0.3) | 1027 | 0.02 (0.0, 0.1) | 846 | ‡ |
| 65–74 | 644 | 0.4 (0.0, 0.8) | 926 | ‡ | 816 | 0.1 (0.1, 0.4) |
| 75+ | 223 | 1.0 (0.0, 2.3) | 368 | 0.5 (0.0, 1.2) | 329 | 1.1 (0.0, 2.2) |
LALES = Los Angeles Latino Eye Study, BDES = Beaver Dam Eye Study, BMES = Blue Mountains Eye Study.
N= number at risk for incidence of visual impairment at baseline; % (CI)=prevalence and 95% confidence interval;
The annualized incidence rates are derived from 4-year incidence data for LALES and 5-year incidence data for BDES and BMES.
Criterion for Any visual impairment (BDES criterion): Persons with Baseline BCVA better than 20/40 in one or both eyes at baseline and follow-up BCVA 20/40 or worse in the better-seeing eye (including 20/40). Persons with incident blindness are included in the criterion for any visual impairment.
Criterion for Blindness (Severe visual impairment) (BDES criterion): Persons with a BCVA better than 20/200 in one or both eyes at baseline and follow-up BCVA 20/200 or worse in the better-seeing eye (including 20/200).
No incident cases.
Figure 4.
Comparison of Estimated Annual Incidence of Visual Impairment Stratified by Age in three Population-Based Studies – the Beaver Dam Eye Study, the Blue Mountains Eye Study and the Los Angeles Latino Eye Study.
Table 10.
Comparison of Estimated Annual Worsening and Improvement of Best Corrected Visual Acuity Stratified by Age in non-Hispanic Whites in Beaver Dam, Wisconsin, Blue Mountains, Australia and Los Angeles Latinos.
| LALES |
BDES |
BMES |
||||
|---|---|---|---|---|---|---|
| Age at baseline (years) | N | % (CI) | N | % (CI) | N | % (CI) |
| Worsening in better seeing eye (≥ 15 letters worse)* | ||||||
| <55 | 2583 | 0.3 (0.1, 0.5) | 1239 | 0.02 (0.0, 0.1) | 333 | ‡ |
| 55–64 | 1159 | 0.5 (0.1, 0.9) | 1027 | 0.2 (0.0, 0.5) | 846 | 0.04 (0.0, 0.2) |
| 65–74 | 644 | 1.4 (0.5, 2.3) | 926 | 0.34 (0.0, 0.7) | 817 | 0.2 (0.0, 0.6) |
| 75+ | 223 | 3.0 (0.8, 5.3) | 375 | 1.7 (0.4, 3.0) | 331 | 1.1 (0.0, 2.3) |
| Improvement in worse seeing eye (≥ 15 letters better)† | ||||||
| <55 | 1077 | 0.3 (0.0, 0.6) | 531 | 0.3 (0.0, 0.7) | 159 | 0.3 (0.0, 1.1) |
| 55–64 | 646 | 0.6 (0.0, 1.2) | 614 | 0.2 (0.0, 0.6) | 508 | 0.1 (0.0, 0.4) |
| 65–74 | 473 | 1.3 (0.3, 2.3) | 718 | 0.7 (0.1, 1.3) | 632 | 0.4 (0.0, 0.9) |
| 75+ | 208 | 1.8 (0.0, 3.6) | 353 | 0.9 (0.0, 1.8) | 318 | 0.8 (0.0, 1.8) |
LALES = Los Angeles Latino Eye Study, BDES = Beaver Dam Eye Study, BMES = Blue Mountains Eye Study.
N= number at risk for incidence of visual impairment at baseline. % (CI)=prevalence and 95% confidence interval; Annual worsening and improvement rates are estimated from 4-year incidence data for LALES and 5-year incidence data for BDES and BMES.
Criterion for Worsening (≥ 15 letters worse) in the better seeing eye: Persons with incident worsening had a baseline BCVA of light perception or better in one or both eyes and at follow-up had BCVA loss of 15 or more letters read correctly in the better-seeing eye.
Criterion for Improvement (≥ 15 letters better) in the worse seeing eye: Persons capable of improving from Baseline by 15 or more letters read correctly in one or both eyes at best correction (BCVA 20/20 or worse) and at follow-up had an increase of 15 or more letters read correctly in the worse-seeing eye.
No incident cases.
In general, the incidence of visual impairment among Latinos appears to be intermediate between that in non-Hispanic white and Afro-Caribbean populations. These results parallel those of prevalence studies which have noted age-specific rates of visual impairment and blindness in Latinos to be higher than those of non-Hispanic whites in the United States, Australia, and the Netherlands but lower than those of Barbadian Afro-Caribbeans.11 These differences in the incidence may reflect differences in - the biological risk for developing eye diseases, socioeconomic status and access to ophthalmic care. Latinos are a relatively young population compared with African-Americans and non-Hispanic whites in the US, and the incidence of visual impairment and blindness can be expected to rise as the Latino population ages.
Our study has several strengths. First, it is a population-based study with a large sample size and a high participation rate (76%). Second, the use of standard methods allows comparisons with other incidence studies. Third, the quality control procedures implemented in LALES minimized measurement error. Fourth, it is the first study to look at incidence rates of visual impairment and blindness in a Latino population. An additional strength of LALES was the use of binocular vision measurements that provide insight into the functional burden of visual impairment. While BCVA may be most appropriate measure for non-refractive ocular pathology, functional impairment is likely best assessed utilizing PVA. Finally, we have provided an assessment of the incidence of visual impairment and blindness in the first and second eyes which illuminate the greater likelihood of developing visual impairment in the second eye and significantly reducing vision-specific function. In previous studies, incidence of visual impairment in the second eye is not presented. However, as noted in Table 4 and Table 5, the incidence of visual impairment in the second eye is significantly higher than the incidence of visual impairment in the first eye. Given that individuals who transition from monocular impairment to binocular impairment are likely to have significant reductions in their vision-specific function13 it is critical to present this data to provide a comprehensive assessment of the burden of incident visual impairment and blindness in the population.
This study has several limitations. First, despite the high participation rate, participants and nonparticipants differed statistically with regard to several factors that may have led us to underestimate the true incidence of visual impairment. For example, at baseline, nonparticipants were statistically less likely to have excellent or good self-reported vision or to have in-home binocular near vision better than 20/40. Nonparticipants also were statistically less likely to have health insurance, a potential barrier to on-going ophthalmic care. However, a careful analysis suggests that the difference between participants and nonparticipants while statistically significant, is small. An imputed incidence rate of presenting binocular visual impairment for nonparticipants (utilizing baseline data) was 5.6% (CI: 4.2%, 7.1%), whereas the actual observed incidence for participants was 4.6% (95% CI: 4.0%, 5.2%). These results suggest that although expected incidence for nonparticipants is higher than the observed incidence for participants, the difference is small, indicating that the two groups do not differ in a meaningful manner.
Second, exclusion of institutionalized persons (nursing homes, group homes) also may have led to underestimation of the incidence of visual impairment and blindness. Klein and associates noted a significantly higher incidence of vision loss in those residing in nursing homes than in non-institutionalized individuals. However, since Latinos are less likely to institutionalize their parents,20 the small number of those Latinos residing in nursing homes or group homes are likely to have a minimal impact on the overall incidence rates reported here. Third, the LALES population is primarily of Mexican ancestry and may not be representative of all Latino subgroups. Thus, our findings should not be generalized to other Latino subgroups. However, because our group was primarily of Mexican ancestry, our results can be generalized to Latinos from Mexico. Finally, there was the possibility of a design effect as the analysis assumed independence between participants. However, we could not previously demonstrate evidence of a family clustering effect11 in the prevalence study and thus it is likely that any design effect present in this study is negligible.
In summary, LALES is the largest population-based study of the incidence of eye disease in the United States. Its age-specific incidence rates of visual impairment and blindness are the highest of any racial/ethnic group reported in the US. These high rates emphasize the importance of focusing efforts on Latinos - the fastest growing segment in the United States. In particular, older Latinos are likely to be significantly impacted by interventions directed at screening and management of treatable visual impairment. However, while there is an increasing public health concern of disease rates in Latinos, evidence regarding the impact of intervention needs to be obtained.
Table 11.
Comparison of Estimated Annual Incidence of Visual Impairment and Blindness by United States and World Health Organization Criteria Stratified by Age in Barbadian Afro-Caribbeans and Los Angeles Latinos
| Age at baseline (years) |
Visual impairment |
Blindness |
||||||
|---|---|---|---|---|---|---|---|---|
| LALES |
BISED |
LALES |
BISED |
|||||
| N | % (CI) | N | % (CI) | N | % (CI) | N | % (CI) | |
| United States Criterion* | ||||||||
| 40–49 | 1751 | 0.1 (0.0, 0.3) | 978 | 0.1 (0.0, 0.4) | 1754 | ‡ | 989 | ‡ |
| 50–59 | 1444 | 0.1 (0.0, 0.3) | 825 | 0.5 (0.0, 0.9) | 1446 | 0.1 (0.0, 0.2) | 847 | 0.1 (0.0, 0.2) |
| 60–69 | 913 | 0.4 (0.0, 0.8) | 658 | 1.7 (0.7, 2.7) | 931 | 0.1 (0.0, 0.3) | 721 | 0.3 (0.0, 0.7) |
| 70+ | 454 | 1.4 (0.3, 2.5) | 409 | 5.4 (3.2, 7.6) | 476 | 0.2 (0.0, 0.6) | 533 | 1.8 (0.7, 3.0) |
| World Health Organization Criterion† | ||||||||
| 40–49 | 1751 | 0.03 (0.0, 0.1) | 986 | 0.1 (0.0, 0.2) | 1755 | ‡ | 989 | ‡ |
| 50–59 | 1444 | 0.1 (0.0, 0.2) | 832 | 0.3 (0.0, 0.7) | 1446 | 0.1 (0.0, 0.2) | 848 | ‡ |
| 60–69 | 922 | 0.3 (0.1, 0.7) | 703 | 1.0 (0.3, 1.8) | 932 | ‡ | 726 | 0.2 (0.0, 0.4) |
| 70+ | 468 | 0.9 (0.0, 1.7) | 472 | 3.6 (1.9, 5.2) | 481 | 0.2 (0.0, 0.5) | 549 | 0.7 (0.0, 1.4) |
LALES = Los Angeles Latino Eye Study, BISED = Barbados Incidence Study of Eye Diseases, WHO = World Health Organization.
N= number at risk for incidence of visual Impairment/blindness at baseline. % (CI)=prevalence and 95% confidence interval; estimated from overall 4-year incidence data for LALES and BISED studies.
US Criterion Incidence of Visual Impairment: Persons with Baseline BCVA 20/40 or better and follow-up BCVA worse than 20/40 but better than 20/200 (not including 20/40 or 20/200). Incidence of Blindness: Persons with Baseline BCVA better than 20/200 and follow-up BCVA 20/200 or worse (including 20/200).
W.H.O. Criterion. Incidence of Visual Impairment: Persons with Baseline BCVA 20/60 or better and follow-up BCVA worse than 20/60 but better than or equal to 20/400 (not including 20/60 but including 20/400). Incidence of Blindness: Persons with Baseline BCVA 20/400 or better and follow-up BCVA worse 20/400 (not including 20/400).
No incident cases.
ACKNOWLEDGEMENTS/DISCLOSURE
Support: National Institutes of Health Grants: NEI U10-EY-11753 and EY-03040 and an unrestricted grant from Research to Prevent Blindness, New York, NY. Rohit Varma is a Research to Prevent Blindness Sybil B. Harrington Scholar.
Financial Disclosure: The authors have no proprietary or commercial interest in any materials discussed in the manuscript.
Statement about Conformity: The study protocol was approved by the Institutional Review Board (IRB)/Ethics Committee at the University of Southern California and all study procedures adhered to the recommendations of the Declaration of Helsinki. Written consent was obtained from all participants.
Contributions: design and conduct of the study (RV, SPA); collection, management, analysis, and interpretation of the data (JC, AWPG, MT, SPA, & RV); and preparation, review, or approval of the manuscript (JC, AWPG, MT, SPA, & RV).
Other Acknowledgements:
The Los Angeles Latino Eye Study Group (LALES I)
University of Southern California, Los Angeles, CA.-Rohit Varma, MD, MPH; Sylvia H. Paz, MS; Stanley P. Azen, PhD; Lupe Cisneros, COA; Elizabeth Corona; Carolina Cuestas, OD; Denise R. Globe, PhD; Sora Hahn, MD; Mei-Ying Lai, MS; George Martinez; Susan Preston-Martin, PhD; Ronald E. Smith, MD; LaVina Tetrow, Mina Torres, MS; Natalia Uribe, OD; Jennifer Wong, MPH; Joanne Wu, MPH; Myrna Zuniga.
Battelle Survey Research Center, St. Louis, MO- Sonia Chico, BS; Lisa John, MSW; Michael Preciado, BA; Karen Tucker, MA.
Ocular Epidemiology Grading Center, University of Wisconsin, Madison, WI Ronald Klein, MD, MPH.
The Los Angeles Latino Eye Study Group (LALES II)
University of Southern California, Los Angeles, CA: Rohit Varma, MD, MPH (Principal Investigator); Stanley P. Azen, PhD (Co–Principal Investigator); Mina Torres, MS (Project Director); Jaime Barrera; Farzana Choudhury, MBBS, MPH; Lupe Cisneros, COA; Jessica Chung, MPH, PhD; Elizabeth Corona; Carolina Cuestas, OD; Anne DiLauro, MPH (2005–2007); Jeanne Dzekov; Ana Evans (2004–2007); Athena W.P. Foong; Carlos Lastra, MD; Mei-Ying Lai, MS; George Martinez; Roberta McKean-Cowdin, PhD; Carlos Moya; Sylvia H. Paz, MS (2004–2005); Fernando Pena, MD (2004–2005); Corina Shtir, MS; Ronald E. Smith, MD; LaVina Tetrow (2004–2005); Heather Volk, PhD; Ying Wang, MS (2006–2007); Joanne Wu, MPH (2004–2006).
Battelle Survey Research Center, St. Louis, MO: Lisa John, MSW; Karen Tucker, MA; Natasha Van Leeuwen.
Ocular Epidemiology Grading Center, University of Wisconsin, Madison, WI:
Ronald Klein, MD, MPH; Tiffany Jan; Michael D. Knudtson, MA; Stacy E. Meuer; Michael Neider.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.United States Census 2000. [cited 2007 July 5];U.S. Census Bureau projections of the resident population by race, Hispanic origin, and nativity: middle series 2050 to 2070. 2000 NP-T5-G:[Available from: http://www.census.gov/population/projections/nation/summary/np-t5-g.txt.
- 2.Foran S, Mitchell P, Wang JJ. Five-year change in visual acuity and incidence of visual impairment: the Blue Mountains Eye Study. Ophthalmology. 2003;110:41–50. doi: 10.1016/s0161-6420(02)01295-2. [DOI] [PubMed] [Google Scholar]
- 3.Klein R, Klein BE, Lee KE. Changes in visual acuity in a population. The Beaver Dam Eye Study. Ophthalmology. 1996;103(8):1169–1178. doi: 10.1016/s0161-6420(96)30526-5. [DOI] [PubMed] [Google Scholar]
- 4.McCarty DJ, Fu CL, Harper CA, Taylor HR, McCarty CA. Five-year incidence of diabetic retinopathy in the Melbourne Visual Impairment Project. Clin Experiment Ophthalmol. 2003;31:397–402. doi: 10.1046/j.1442-9071.2003.00685.x. [DOI] [PubMed] [Google Scholar]
- 5.Hyman L, Wu SY, Connell AM, et al. Prevalence and causes of visual impairment in The Barbados Eye Study. Ophthalmology. 2001;108:1751–1756. doi: 10.1016/s0161-6420(01)00590-5. [DOI] [PubMed] [Google Scholar]
- 6.Tielsch JM, Sommer A, Witt K, Katz J, Royall RM. Blindness and visual impairment in an American urban population. The Baltimore Eye Survey. Arch Ophthalmol. 1990;108:286–290. doi: 10.1001/archopht.1990.01070040138048. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez J, Sanchez R, Munoz B, et al. Causes of blindness and visual impairment in a population-based sample of U.S Hispanics. Ophthalmology. 2002;109:737–743. doi: 10.1016/s0161-6420(01)01008-9. [DOI] [PubMed] [Google Scholar]
- 8.Klein R, Klein BE, Linton KL, De Mets DL. The Beaver Dam Eye Study: visual acuity. Ophthalmology. 1991;98:1310–1315. doi: 10.1016/s0161-6420(91)32137-7. [DOI] [PubMed] [Google Scholar]
- 9.Attebo K, Mitchell P, Smith W. Visual acuity and the causes of visual loss in Australia. The Blue Mountains Eye Study. Ophthalmology. 1996;103:357–364. doi: 10.1016/s0161-6420(96)30684-2. [DOI] [PubMed] [Google Scholar]
- 10.Klaver CC, Wolfs RC, Vingerling JR, Hoffman A, de Jong PT. Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol. 1998;116:653–658. doi: 10.1001/archopht.116.5.653. [DOI] [PubMed] [Google Scholar]
- 11.Varma R, Ying-Lai M, Klein R, Azen SP. Prevalence and risk indicators of visual impairment and blindness in Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2004;111:1132–1140. doi: 10.1016/j.ophtha.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Leske MC, Wu SY, Hyman L, et al. Four-year incidence of visual impairment: Barbados Incidence Study of Eye Diseases. Ophthalmology. 2004;111:118–124. doi: 10.1016/j.ophtha.2003.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Varma R, Wu J, Chong K, Azen SP, Hays RD. Los Angeles Latino Eye Study Group. Impact of severity and bilaterality of visual impairment on health-related quality of life. Ophthalmology. 2006;113:1846–1853. doi: 10.1016/j.ophtha.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 14.Varma R, Paz SH, Azen SP, et al. The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004;111:1121–1131. doi: 10.1016/j.ophtha.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Guzowski M, Wang JJ, Rochtchina E, Rose KA, Mitchell P. Five-year refractive changes in an older population: the Blue Mountains Eye Study. Ophthalmology. 2003;110:1364–1370. doi: 10.1016/S0161-6420(03)00465-2. [DOI] [PubMed] [Google Scholar]
- 16.Klein R, Klein BE, Lee KE, Cruickshanks KJ, Gangon RE. Changes in visual acuity in a population over a 10-year period: The Beaver Dam Eye Study. Ophthalmology. 2001;108:1757–1766. doi: 10.1016/s0161-6420(01)00769-2. [DOI] [PubMed] [Google Scholar]
- 17.Klein R, Klein BE, Lee KE, et al. Changes in visual acuity in a population over a 15-year period: the Beaver Dam Eye Study. Am J Ophthalmol. 2006;142:539–549. doi: 10.1016/j.ajo.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 18.Lee KE, Klein BE, Klein R. Changes in refractive error over a 5-year interval in the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1999;40:1645–1649. [PubMed] [Google Scholar]
- 19.Lee KE, Klein BE, Klein R, Wong TY. Changes in refraction over 10 years in an adult population: the Beaver Dam Eye study. Invest Ophthalmol Vis Sci. 2002;43:2566–2571. [PubMed] [Google Scholar]
- 20.Klein R, Wang Q, Klein BE, Moss SE, Meuer SM. The relationship of age-related maculopathy, cataract, and glaucoma to visual acuity. Invest Ophthalmol Vis Sci. 1995;36:182–191. [PubMed] [Google Scholar]
- 21.Mausbach BT, Coon DW, Depp C, et al. Ethnicity and time to institutionalization of dementia patients: a comparison of Latina and Caucasian female family caregivers. J Am Geriatr Soc. 2004;52:1077–1084. doi: 10.1111/j.1532-5415.2004.52306.x. [DOI] [PubMed] [Google Scholar]