Abstract
Objective
To study the relationship between parent concerns about development in the first year and a half of life and later autism diagnostic outcomes.
Method
Parent concerns about development were collected for infants at high and low risk for autism, using a prospective, longitudinal design. Parents were asked about developmental concerns at study intake and when their infant was 6, 12, and 18 months. Infants were then followed up until 36 months, when diagnostic status was determined.
Results
By the time their child was 12 months, parents who have an older child with autism reported significantly more concerns in autism spectrum disorders-related areas than parents of children with typical outcomes. These concerns were significantly related to independent measures of developmental status and autism symptoms and helped predict which infants would later be diagnosed with autism or autism spectrum disorders. At 6 months, however, the concerns of parents who have an older child with autism do not predict outcome well.
Conclusion
Explicitly probing for parent concerns about development is useful for identifying children in need of closer monitoring and surveillance, as recommended by the American Academy of Pediatrics.
A fundamental component of pediatric practice is parent appraisal of child development.1 Developmental history taking, including elicitation of parental concerns, is standard in most routine pediatric visits and is used to alert physicians to the possibility of conditions requiring further evaluation. As the incidence of and media attention to autism spectrum disorders (ASD) increase, concerns about the possibility of these conditions are increasingly being raised by parents.2 Recently published guidelines from the American Academy of Pediatrics recommend that pediatricians ask parents about developmental concerns at each well-child visit and screen all children for autism twice by the second birthday.3 If concerns are identified by parents, the American Academy of Pediatrics' surveillance and screening algorithm3 recommends that an autism-specific screener should be administered and/or the child should be referred for a diagnostic evaluation, depending on the level of concern. Thus, parent report alone can trigger a referral for further evaluation.
Retrospective studies indicate that parents recognize signs of autism far earlier than it is diagnosed. Although symptoms are typically present by the second birthday and one third of parents cite concerns before the first birthday,4 diagnoses are often not made until the fourth year of life or later.5 Early concerns are sometimes dismissed,2 resulting in a several month to several year delay of diagnosis.6–8 Thus, early detection methods need improvement, in the hope that earlier diagnosis will lead to earlier initiation of treatment and reduced disability. As reviewed below, there is a robust literature on the accuracy of parent reports in general and for predicting developmental delays specifically; little, however, is known about their utility in predicting later autism diagnoses.
Several studies have examined how well parent information corresponds with developmental tests and/or expert clinical judgment. Correlations are moderately high (0.45– 0.65) between parent report of vocabulary and concurrent expressive language scores9 and very strong (0.80) between parent estimation of their child's developmental age and actual developmental quotients obtained through standardized testing.10 Parent concerns in high-risk infants were confirmed by formal assessment 95% of the time.11 Glascoe and colleagues12 have standardized the measurement of parent concerns through an instrument, the Parents' Evaluation of Developmental Status (PEDS). It is designed for children birth to 8 years and asks both general questions about concerns (please list any concerns about your child's learning, behavior, or development) and specific questions about concerns in 10 individuals domains (i.e., cognitive, language, motor, self-help). The Parents' Evaluation of Developmental Status demonstrates high accuracy in predicting disability (sensitivity 0.79 and specificity 0.72 in a sample aged 21 to 84 months).13 Although the Parents' Evaluation of Developmental Status was developed as a broadband screening instrument, a recent investigation found that parent concerns recorded between 18 and 59 months were correlated with concurrent scores on the Modified Checklist for Autism in Toddlers,14 suggesting that it might be useful to screen for ASD as well. This finding was not replicated in a study screening 18- to 30-month old infants in primary care settings,15 however, leading these authors to suggest that ASD-specific tools will be needed in the universal screening process.
However, the importance of assessing the accuracy of parent reports of early development and their predictive validity for identifying autism is complicated in several ways. Several studies suggest that signs of autism emerge gradually over time and that the earliest symptoms are subtle and not easy to detect, particularly by untrained observers.16 A few retrospective studies suggest that symptoms can be detected before the first birthday in some children,17,18 but these early differences appear to be nonspecific (e.g., sleeping, eating, temperament patterns) and do not differentiate children with developmental delays from those with autism.19 Group differences are more reliably present and consistently found across studies in the second year of life.20 Several prospective investigations of infants at higher risk for autism (because of family history) have failed to find differences at 6 months between children who are later diagnosed with autism and those who develop typically.21–24 Bryson et al,25 in a consecutive case series of infant siblings who developed autism, followed prospectively from 6 months, describe several children whose symptoms are not present at their 6- and 12-month visits but emerge slowly during the second year of life. Not a single child who developed autism (n = 9) displayed marked limitations in social reciprocity at 6 months. All 9 infants were described as interested in social interactions, responsive to others, demonstrating sustained eye contact and social smiles. This pattern of slow emergence of symptoms during the first year and a half of life may complicate efforts to use parent reports to identify autism symptoms earlier.
A second complication is the influence of risk status on parent reporting. Several studies have demonstrated that parents' perceptions of child development are impacted by their child's health status. For example, low birth weight children were rated as in poor health significantly more commonly by parents than by professionals.26 In prospective studies that follow high-risk families who already have a child with autism, as in this investigation, it is possible that parents may have heightened vigilance to developmental variations and over-report concerns. Conversely, it is equally possible that such parents will be more astute observers of child development who notice subtle manifestations of early developmental problems that may not yet be apparent on standardized assessments. Studies have shown that typically developing children whose parents reported concerns but who passed developmental screens (apparent false positives) performed significantly lower on tests of cognitive functioning and had significantly more behavioral problems than children whose parents raised no concerns.27 It was concluded that parents who appeared to be excessively worried were in fact “… vigilant observers who noticed behavioral and developmental problems that fall in the gray zone between disabled and average.”27(p. 6) Parent concerns have also been found to correlate with developmental test scores in toddlers at risk for autism.28
This study collected parent concerns about development for infants at high and low risk for autism, using a prospective, longitudinal design. Parents were asked about developmental concerns at study intake and when their infant was 6, 12, and 18 months. Infants were then followed up until 36 months, when diagnostic status was determined. We examined whether the number and type of parent concerns differed over time as a function of outcome status. Although previous studies have examined the ability of parent concerns to predict concurrent test scores in children at risk for autism,14,28 this study is the first to examine the relationship between longitudinal parent report and later diagnostic outcome.
METHOD
Participants
Participants were enrolled in a longitudinal study of development from infancy to 3 years, recruited at 2 sites (UC Davis, n = 149; UCLA, n = 125). The sample included 174 infants with an older sibling with ASD (high-risk group), whose diagnosis was confirmed by meeting at least the ASD cutoffs on both the Autism Diagnostic Observation Schedule (ADOS) and the Social Communication Questionnaire (SCQ), and 100 infants with an older sibling with typical development (low-risk group), confirmed by an intake screening questionnaire and scores below the ASD range on the SCQ. The gender ratio was balanced, with 56% of the total sample being male infants. Ninety-two infants (36%) were from an ethnic or racial minority group. There were no differences between the risk groups in gender ratio, family income, ethnicity, or racial background (all p values >.30).
Thirty-one participants (11%) withdrew from the study before 36 months. There were no significant differences in gender or site between those who withdrew versus those who continued; there was a nonsignificant trend for subjects who withdrew to be in the high-risk group (χ2 = 2.90, df = 1, p = .09). For all analyses of parent concerns detailed later, preliminary analytic models that included attrition as a 2-level fixed factor (withdrew vs. continued to outcome) revealed no significant differences at any age (6, 12, or 18 months) and no significant differences in change in parent concerns over time. As such, attrition does not appear to have biased the results in a particular fashion. After accounting for attrition, the final sample described in this study consisted of 243 infants (n = 151 high risk, n = 92 low risk).
At the final study visit at 36 months, participants were classified into 1 of 4 outcome groups, using the following definitions:
Autism/ASD (n = 26): scored over the ASD cutoff on the ADOS and DSM-IV clinical best estimate judgment of an expert clinician was consistent with these scores. Outcomes of autism and ASD were grouped together because of the small size of the subgroups and because their distinction is tentative early in development.
Other delays (n = 57): scored >1.5 standard deviations below the mean on one or more scales of the Mullen or clinical best estimate judgment of an expert clinician was of a behavior problem or developmental delay and did not meet autism/ASD criteria. This group included children with global developmental delay, speech-language delay, marked hyperactivity, or marked anxiety.
High-risk typical (n = 86): did not meet criteria for other outcome classifications and had an older sibling with autism.
Low-risk typical (n = 74): did not meet criteria for the other outcome classifications and had an older sibling with typical development.
Measures
Parent Concerns Questionnaire
A trained examiner interviewed parents at the end of each visit, asking “Do you have any concerns about [your child's] development or behavior at this time?” and recording the verbatim response. Examiners were research assistants with autism treatment experience, graduate students in clinical psychology, postdoctoral fellows with clinical degrees, and a pediatrician. All parent responses were recorded, without judgment about whether a concern was legitimate, reasonable, or age appropriate. If a response indicated that the concern was no longer current (e.g., “we used to be worried about his speech, but now he's talking a lot”), it was not coded, as the form was meant to be a window into current concerns at the time of the test visit. If a response indicated concern but was minimized (“his language seems a little slower than his sister, but I'm not really worried—it is probably because she talks for him”), it was still coded as a concern because previous investigations have found that such equivocal comments are often associated with developmental difficulties.27 Responses were coded into 1 of 8 concern categories (Table 1) or as “no concerns” by raters unaware of group membership. Coders were initially trained to 90% agreement on all codes. Fifteen percent of responses were then double coded to maintain ongoing reliability. Intraclass correlation coefficients were in the acceptable range for all codes, ranging from 0.64 for general developmental concerns to 0.97 for motor concerns (mean intraclass correlation coefficients across the 9 codes was 0.86).
Table 1.
Categories of Parent Concerns Coded
| Code | Description | Example |
|---|---|---|
| No concerns | Response indicating no concerns or highlighting positive attributes of the child. Mutually exclusive with all other codes | “He's talking so much.” “Seems like she's doing fine to us.” |
| Speech/language/communication | Concerns related to the production of speech (expressive language, vocabulary, articulation), nonverbal vocalizations (babbling), and gestures (pointing); language comprehension; reciprocity or intentionality of communication | “She still has very few words.” “Shouldn't he be waving bye and hi by now?” |
| Social | Concerns about social engagement, interest in other people, social or emotional reciprocity, and social attention | “He seems oblivious to other people.” “He doesn't look at us very much.” |
| Stereotyped behavior | Rigid, repetitive, or otherwise odd behavior in the sensory, motor (odd hand/arm/body posturing), or object-use domains | “She always needs to be holding a matchbox car in each hand.” “He covers his ears a lot, even when it doesn't seem too loud.” |
| Motor | Concern refers to delays in achieving motor milestones and/or general clumsiness | “My pediatrician told me that a lot of kids don't walk by 12 months but now he's 17 months and still not walking.” |
| Medical/regulatory | Concern refers to a specific medical issue/condition, general health problem, or physiological functions (eating, sleeping, elimination) | “He seems to get sick more than other kids.” “She seems small for her age.” “He still isn't sleeping through the night.” “She only eats a few bites, then stops.” |
| Behavior/temperament | Any concerns related to behavior or temperament, including activity level, attention, behavioral regulation (intensity of response, aggression, impulsivity, compliance); mood/general disposition (happy, cranky, anxious; poorly modulated affect) | “She won't sit still for even a minute. I can't get her to listen to a story.” “He can be so stubborn.” “They've officially warned us at school that if he bites again he's out.” “He won't let me put him down when we go somewhere new.” |
| Unspecified autism | Concern refers explicitly or implicitly to autism but does not focus on any specific symptom | “He acts like my other son did at this age and he has autism.” |
| General developmental | Concerns about development that are general, as well as cognitive and self-help concerns | “He's just hitting his milestones later than my other kids.” “She seems to be off-track developmentally.” |
The 8 concern categories were collapsed into 2 dependent measures for analysis: ASD concerns (the sum of concerns falling in the speech/language/communication, social, stereotyped behavior, and unspecified autism categories), and general concerns (the sum of concerns falling into the motor, medical/regulatory, behavior/temperament, and general development categories).
Autism Diagnostic Observation Schedule29
This is a semistructured standardized interaction and observation that measures symptoms of autism. It has 2 empirically derived cutoffs, one for ASD and one for autistic disorder. Psychometric studies report very high inter-rater reliability and agreement in diagnostic classification (autism vs. nonspectrum) for individuals aged 24 months and older.29 The ADOS was administered in this study at 18 and 24 months as a quantitative measure of autism symptoms and at 36 months for diagnostic classification purposes. It was also used to verify diagnosis in older siblings of high-risk infants.
Social Communication Questionnaire30
This parent-report questionnaire is composed of 40 yes/no questions about behaviors characteristic of autism. Previous studies have shown good to excellent internal consistency reliability and discriminative validity of the SCQ across a wide age range,30 including children younger than 4 years.31 The SCQ was used in this study to verify diagnosis in older siblings of high-risk infants.
Mullen Scales of Early Learning32
This is a standardized developmental test for children birth to 68 months. Four subscales were administered: Fine Motor, Visual Reception, Expressive Language, and Receptive Language. An overall score, the Early Learning Composite (ELC), is also obtained. The Mullen subscales and composite have excellent internal consistency (median, 0.91) and test-retest reliability (median, 0.84).
Modified Checklist for Autism in Toddlers33
This is a 23-item parent-report questionnaire that is used as a screening tool for autism in toddlers between 18 and 30 months. The positive predictive value of the Modified Checklist for Autism in Toddlers in primary care settings has been reported to be 0.57.
Procedure
This study was conducted under the approval of the UC Davis and UCLA Institutional Review Boards. Infants were assessed at 6, 12, 18, 24, and 36 months by examiners unaware of the child's group membership. The test protocol included the Mullen Scales of Early Learning, the ADOS, and other experimental tests reported elsewhere.16,22,34 Parent concerns were collected at intake, 6, 12, and 18 months, at the end of each visit, so that responses would not bias collection of the rest of the data.
RESULTS
Sample Characteristics
Parent concerns were collected on 243 infants (216 at both intake and at least 1 study visit, 5 at intake only, and 22 at a study visit only). The average age at intake was 7.3 months (SD = 5.4). There was a significant difference between the high- and low-risk groups in age at intake (high risk: M = 8.5, SD = 5.6; low risk: M = 5.4, SD = 4.4; t(240) = 4.45, p < .001).
Table 2 displays the percent of the autism/ASD outcome group with parent concerns at each age. Consistent with previous reports,4,6,35 concerns about communication were the most common concern at most ages.
Table 2.
Frequencies and Percentages of Autism/ASD Outcome Group With Parent Concerns at Each Age
| 6 mo (n = 14) | 12 mo (n = 22) | 18 mo (n = 26) | |
|---|---|---|---|
| Speech/language/communication, n (%) | 3 (21.4) | 15 (68.2) | 18 (69.2) |
| Social, n (%) | 4 (28.6) | 5 (22.7) | 11 (42.3) |
| Stereotyped behavior, n (%) | 3 (21.4) | 4 (18.2) | 8 (30.8) |
| Motor, n (%) | 3 (21.4) | 6 (27.3) | 3 (11.5) |
| Medical/regulatory, n (%) | 3 (21.4) | 4 (18.2) | 5 (19.2) |
| Behavior/temperament, n (%) | 1 (7.1) | 2 (9.1) | 7 (26.9) |
| Unspecified autism, n (%) | 0 (0) | 4 (18.2) | 2 (7.7) |
| General developmental, n (%) | 0 (0) | 2 (9.1) | 2 (14.3) |
ASD, autism spectrum disorders.
Table 3 displays characteristics of the sample by outcome group. Significant differences were found on all measures. Post-hoc comparisons using Bonferroni corrections revealed that the autism/ASD group scored significantly higher on the ADOS and the SCQ and significantly lower on the Mullen than all other groups. There were no differences between the high- and low-risk typical groups on any measure.
Table 3.
Characteristics of Outcome Groups at 36 Months
| Measure | Autism/ASD | Other Delays | High-risk Typical | Low-risk Typical |
|---|---|---|---|---|
| ADOS communication + social score, M (SD) | 13.12a (3.42) | 4.47b (3.00) | 1.94c(1.36) | 1.64c (1.41) |
| SCQ total, M (SD) | 12.70a (5.89) | 5.08b (4.27) | 3.6lb(4.13) | 3.94b (2.77) |
| Mullen visual reception, M (SD) | 39.75a (20.02) | 48.76b (12.08) | 64.01c (10.53) | 62.76c (11.37) |
| Mullen fine motor, M (SD) | 34.30a (11.91) | 45.60b (10.23) | 56.60c (12.38) | 57.47c (13.54) |
| Mullen receptive language, M (SD) | 35.81a (14.25) | 45.40b (10.59) | 54.27c (8.84) | 55.09c (9.31) |
| Mullen expressive language, M (SD) | 39.38a (14.38) | 47.52b (9.74) | 56.14c(7.70) | 57.82c (6.64) |
| Mullen ELC, M (SD) | 74.09a (22.70) | 93.91b (16.17) | 115.25c (15.31) | 116.43c (14.32) |
ADOS, Autism Diagnostic Observation Schedule; SCQ, Social Communication Questionnaire; ELC, early learning composite.
Groups with different superscripts are significantly different at p < .05 after Bonferroni correction.
Groups with different superscripts are significantly different at p < .05 after Bonferroni correction.
Groups with different superscripts are significantly different at p < .05 after Bonferroni correction.
There were no significant differences between sites in age at intake or number of concerns at any visit. There was a significant site difference in outcome classification (χ2 = 12.26, df = 3, p < .01), reflecting significantly more children with other delays outcomes at UC Davis than UCLA and significantly more with high-risk typical outcomes at UCLA than UC Davis.
Parent Concerns at Intake
The presence of concerns at intake was analyzed using binary logistic regression in a generalized linear model with a logit linka and outcome group (autism/ASD, other delays, high-risk typical, or low-risk typical) as a between-subjects factor. Given the significant difference in age at intake between the high- and low-risk groups, this was included as a covariate. There were significant group differences in ASD concerns (χ2 = 11.67, df = 3, p < .01) but not in general concerns. Specifically, the autism/ASD group had significantly more ASD concerns at intake (32%) than the high-risk typical (12%; χ2 = 4.77, df = 1, p < .05) and low-risk typical groups (1%; χ2 = 10.17, df = 1, p < .001), and marginally more concerns than the other delays group (14%; χ2 = 3.12, df = 1, p = .08). The low-risk typical group had significantly fewer ASD concerns than all of the other groups.
Parent Concerns Over Time
Parent concerns from 6 to 18 months were analyzed using generalized estimating equations to model the data as a negative binomial distribution with a log link function.b Repeated measures were modeled during the 3-time points, with age at visit used as the time variable centered at 12 months. Nonlinear time effects were examined using the square of age (i.e., to examine quadratic effects); however, given that such curvilinear time effects were never significant in any of the models, only the linear effect for time was retained. Model diagnostics involved examining scatter plots of residuals plotted against age and against predicted scores. These revealed no violations of model assumptions.
For ASD concerns, there were significant main effects for outcome group (Wald χ2 = 62.36, df = 3, p < .001) and age (Wald χ2 = 22.31, df = 1, p < .001) and a significant outcome by age interaction (Wald χ2 = 15.04, df = 3, p < .01). Figure 1 displays growth trajectories for ASD concerns for each outcome group. Examination of parameter estimates for outcome by age interaction terms revealed that the autism/ASD group had a significantly greater increase in ASD concerns over time compared with both the high-risk typical (Wald χ2 = 4.13, df = 1, p < .05) and low-risk typical groups (Wald χ2 = 3.94, df = 1, p < .05), but not compared with the other delays group (p = .50). Follow-up simple comparisons revealed that the autism/ASD group had significantly more ASD concerns than all other groups by 12 and 18 months, whereas the low-risk typical group had significantly fewer ASD concerns than all other groups at all ages.
Figure 1.
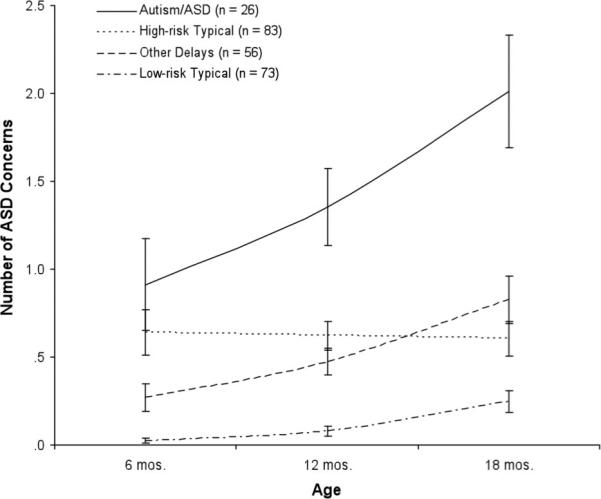
Growth trajectories for ASD concerns. ASD, autism spectrum disorders.
Results of the same analytic models for general concerns revealed only a significant main effect for outcome group (Wald χ2 = 11.95, df = 3, p < .01), with the autism/ASD group showing significantly more general concerns than the low-risk typical group (Wald χ2 = 9.46, df = 1, p < .01), marginally more than the other delays group (Wald χ2 = 3.61, df = 1, p = .06), but a similar number as the high-risk typical group (p = .46).
Parent Concerns and Independent Measures of Functioning
An additional question concerned the degree to which independent measurement of developmental change over time correlated with parent-reported concerns. To this end, we again examined parent concerns using the same predictive models above, but with the addition of measures of ASD symptoms and developmental functioning as time-varying covariates. This strategy allowed us to examine the extent to which parent concerns did (or did not) mirror independent, contemporaneous measures of functioning.
Measures of Autism Symptoms
First, we examined the degree to which parent concerns were related to continuous measures of autism symptoms at 18 months, as measured by the Modified Checklist for Autism in Toddlers (M-CHAT) total and ADOS algorithm scores. The same longitudinal negative binomial models described earlier were used, except that outcome group was not included because it would be redundant with autism symptoms. Analyses of ASD concerns revealed significant main effects for M-CHAT total score (Wald χ2 = 30.47, df = 1, p < .001) and for age (Wald χ2 = 8.18, df = 1, p < .01). The interaction was not significant. Higher scores on the M-CHAT at 18 months were associated with more parent-reported ASD concerns across all ages. Analyses of general concerns revealed no relationship with M-CHAT scores.
Given that the relationship between parent concerns and M-CHAT scores may reflect shared method variance (i.e., parent report), we also used 18-month ADOS scores, which were rated by expert examiners, as an independent, continuous measure of autism symptoms. Using the same longitudinal negative binomial models, again collapsed across outcome groups, we found a significant main effect for 18-month ADOS scores (Wald χ2 = 33.50, df = 1, p < .001), such that children with higher ADOS scores had more ASD concerns reported by parents across all time points than those with lower ADOS scores.
Measures of Development
The predictive model for ASD concerns with the addition of the Mullen ELC as a time-varying covariate across all ages revealed a significant main effect for the ELC (χ2 = 7.98, df = 1, p < .01) and a significant age by ELC interaction (χ2 = 7.77, df = 1, p < .01). The ELC and ASD concerns were significantly correlated at 18 months (Spearman's rho = −0.50, p < .001), indicating that higher ASD concerns were related to lower scores on the Mullen. The same correlation at 12 months was marginally significant (rho = −0.14, p = .053) but was negligible at 6 months (rho = 0.03, p = .77). No other higher-order effects with ELC, group, and age were observed. For general concerns, the main effect of ELC was significant (χ2 = 4.28, df = 1, p < .05), with a decrease of 2 standard deviations on the ELC associated with an increase of 0.2 parent-reported concerns.
We also examined the degree to which ratings of proband (older sibling) ASD symptoms, as measured by the Social Communication Questionnaire, might predict parent concerns and we added this variable as a predictor to the same initial models as earlier. There were no significant effects of proband autism symptoms on parent concerns about the infant sibling at any age.
Receiver Operating Characteristic (ROC) Curve Analyses
We next examined number of parent concerns at each age using ROC analyses to find optimal cutoff values for number of concerns at each age in predicting later outcome status. ROC analysis is a technique commonly used to identify optimal thresholds in diagnostic decision making. It yields a range of decision-making accuracy across all possible cutoff values, with the optimal value defined as the highest point on the curve. Separate analyses were conducted for ASD concerns at 6, 12, and 18 months, comparing (1) the autism/ASD outcome group to the other delays outcome group and (2) the low-risk typical outcome group to the combined ASD and other delays outcome groups. Optimal thresholds were identified using Youden's36 index, which corresponds to the highest point on the ROC curve furthest from the diagonal (where the diagonal represents a sensitivity and specificity no better than chance). Figure 2 displays one of the resulting ROC curve analyses for the autism/ASD versus the other delays outcome groups in number of ASD concerns at 12 months.
Figure 2.
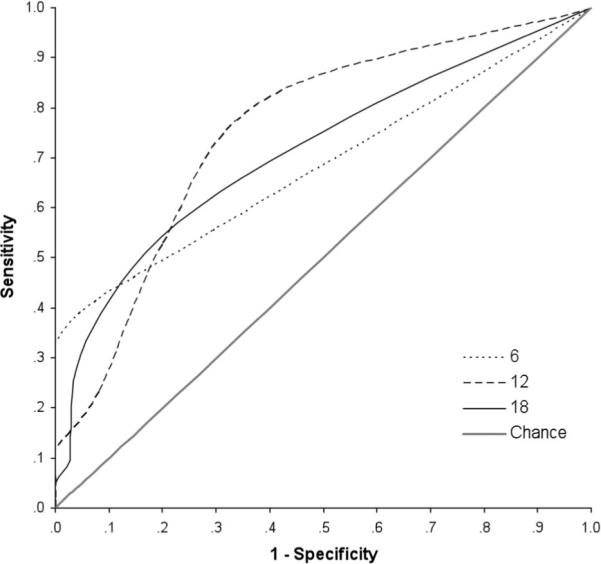
ROC curves at each age for number of ASD concerns (autism/ASD vs. other delays outcome groups). ASD, autism spectrum disorders.
As shown in Table 4, the diagnostic utility of parent concerns was poor at 6 months, as evidenced by the nonsignificant area under the curve (i.e., the overall diagnostic utility did not differ from chance). In contrast, there was evidence of moderate group discrimination based on ASD concerns at 12 months, comparing autism/ASD outcomes to other delays outcomes, as evidenced by significant tests of the area under the curve. At 18 months, tests of the area under the curve were significant for all group comparisons; however, the values for the area under the curve are considered only moderate in terms of decision making,37 ranging from 0.66 to 0.71, suggesting limited diagnostic utility despite significant differences from chance.37
Table 4.
ROC Analyses
| Age (in months) | Area Under Curve | Standard Error | Optimal Thresholda | Youden Index | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | Risk Ratio | |
|---|---|---|---|---|---|---|---|---|---|---|
| Autism/ASD vs. other delays | 6 | .68 | 0.12 | 2 | 0.33 | 0.33 | 1.00 | 1.00 | 0.74 | 3.83 |
| 12 | .74** | 0.08 | 1 | 0.42 | 0.82 | 0.60 | 0.58 | 0.83 | 3.50 | |
| 18 | .71* | 0.08 | 2 | 0.34 | 0.57 | 0.77 | 0.60 | 0.75 | 2.40 | |
| (Autism/ASD + other delays) vs. low-risk typical | 6 | .47 | 0.08 | 2 | 0.01 | 0.12 | 0.89 | 0.43 | 0.58 | 1.02 |
| 12 | .61 | 0.06 | 1 | 0.21 | 0.57 | 0.64 | 0.51 | 0.69 | 1.65 | |
| 18 | .67*** | 0.05 | 2 | 0.27 | 0.36 | 0.92 | 0.77 | 0.64 | 2.16 |
ASD, autism spectrum disorders.
Threshold based on Youden's index36 (max [sensitivityI + Specificityi − 1]).
p < .05.
p < .01.
p < .001.
As also shown in Table 4, optimal thresholds ranged from 1 to 2 for the number of ASD concerns that provided the best diagnostic utility. In general, although the specificity of such cutoffs were high, the sensitivity was low at most ages, suggesting a relatively high rate of false negatives in using such cutoffs, despite the relatively low rate of false positives. Best discrimination between autism/ASD outcomes and other delays outcomes was achieved at 12 months, using a threshold of 1 ASD concern (sensitivity = 0.82, specificity = 0.60).
DISCUSSION
This study found that, by the time their child was 12 months, parents who have an older child with autism reported significantly more concerns in ASD-related areas than parents of children with typical outcomes. These concerns were significantly related to independent measures of developmental status and autism symptoms and helped predict which infants would later be diagnosed with autism or ASD.
At 6 months, however, the concerns of parents who have an older child with autism do not predict outcome well. There were significantly more concerns in both the autism/ASD outcome group and the high-risk typical outcome group than the other groups at this age. In addition, parent concerns at 6 months were not related to independent measures of developmental functioning. Together, these results suggest that parent concerns about their 6-month-old infants were driven more by their status as a younger sibling of a child on the spectrum than by actual developmental differences. One interpretation is that, early in their child's development, some parents who have an older child on the spectrum are anxious and hypervigilant about development, likely due to their awareness of higher recurrence risks in siblings. By 12 months, however, their concerns appear to reflect observed developmental differences and do in fact help predict which children will go on to have atypical outcomes; this is consistent with previous studies.13,27
The failure to discriminate outcomes based on 6-month parent concerns is not surprising, given the emerging nature of behavioral signs of autism.16 Because previous studies have found few developmental differences at 6 months in infant siblings who go on to develop autism,21–24 we expected that parent concerns would increase over time and we found this. With both standardized testing and parent reports finding few group differences at 6 months, this adds to a growing body of literature suggesting that overt behavioral signs of autism are not present in many children at this age.
The significant differences between outcome groups at the time of intake suggest that there were clear selection biases operating in this sample. Many parents already had concerns about development before the first test visit, confirming what has long been suspected by researchers conducting high-risk infant sibling studies: parents often enroll in a study because they are already worried about their child's development. If such ascertainment biases are operating in other samples, it means that outcome rates from these kinds of studies cannot be used to estimate recurrence risk because the rates will be elevated relative to the population of all parents who have an older child with autism. Thus, it is critically important that future studies of recurrence rate use epidemiologic samples with community-based ascertainment, rather than the self-selection that is typical in most infant sibling studies.
This study also helped us examine the specificity of first concerns. Both prospective and retrospective studies17–19,24 find early differences that are nonspecific (e.g., sleeping, eating, temperament patterns) and do not differentiate children with autism from those with developmental delays. Consistent with this, we found that at 6 months parents had both more ASD and more general concerns about children with autism/ASD outcomes, but neither type of concern differentiated them from children in the high-risk group who had typical outcomes. By 12 months and after, however, parent concerns were specific to ASD-related domains and general concerns were unable to differentiate the groups. Sensitivity and specificity were better for ASD than general concerns at 12 months and later. Both the American Academy of Pediatrics and recent studies15 suggest that universal screening for autism use ASD-specific instruments rather than broadband developmental tools. Although the measure used in this study was not an ASD-specific instrument, our findings generally support this suggestion. The specific types of first concerns found in this study are consistent with those reported in retrospective investigations,4,35 which have found that concerns about communication predominate, with social and medical issues also commonly reported.
Finally, we examined classification accuracy and whether there were numbers and/or types of concerns at specific ages that could be used as cutoffs to predict later autism outcomes. Others have suggested that 2 or more concerns in ASD-related domains7 or 3 or more general concerns14 might help identify children in need of further evaluation. We found that the sensitivity and specificity of one or more ASD concern at 12 months were moderately good in predicting outcome, but the positive predictive value was not high enough to recommend this practice yet as an early identification screening tool. In addition, it is likely that the prediction of outcome through parent concerns will be more accurate within a high-risk framework (e.g., with parents who have already experienced a child with autism) than within community-based samples. Different methodologies for eliciting parent concerns may need to be developed for use in community screening. Therefore, it is critical that the results of this study are replicated in an epidemiologic sample.
Nevertheless, the results of this study demonstrate the utility of explicitly probing for parent concerns about development as an aid to identifying children in need of closer monitoring and surveillance, as recommended by the American Academy of Pediatrics.3 When concerns are reported by parents at the 12-month well-child visit or later, providers should listen to and act on this information, applying an autism-specific screener (as recommended by the AAP3), rather than reassuring parents. At the least, if a period of waiting is determined to be the best course of action, practitioners should institute “watchful waiting”2 in which parents are given a definite timeline and specific behaviors to monitor, with close guidance from the provider. If, after this period, improvement in development is not apparent, it is critical to refer such children for comprehensive evaluation. Given the public health emergency that autism presents and the lengthy period between first parent concerns and autism diagnosis,5 it is an imperative of the field to improve our methods of early identification.
ACKNOWLEDGMENTS
We are grateful to Diane Larzelere for preparation of the article. A special thanks to the children and families who participated in this longitudinal study. The work in this article was supported by grants R01 MH068398 (to S.O.) and U54 MH068172 (to M.S.) from the National Institute of Mental Health.
Footnotes
For binomial data, the logit link function is used to model the linear relationship between the dependent variable and predictor variables.
Negative binomial distributions are used for data characterized by significant positive skew and a variance much greater than the mean. Generalized estimating equations allow for modeling data with such non-normal distributions. The link function permits independently specifying the association between predictors [e.g., group or age] and the dependent variable [in this case, number of parent concerns]. Repeated measures were modeled using an autoregressive error covariance matrix because homogeneity of variance assumptions made by traditional repeated-measures analysis of variance was not met.
REFERENCES
- 1.Majnemer A, Rosenblatt B. Reliability of parental recall of developmental milestones. Pediatr Neurol. 1994;10:304–308. doi: 10.1016/0887-8994(94)90126-0. [DOI] [PubMed] [Google Scholar]
- 2.Caronna EB, Augustyn M, Zuckerman B. Revisiting parental concerns in the age of autism spectrum disorders: the need to help parents in the face of uncertainty. Arch Pediatr Adolesc Med. 2007;161:406–408. doi: 10.1001/archpedi.161.4.406. [DOI] [PubMed] [Google Scholar]
- 3.Johnson CP, Myers SM, Council on Children with Disabilities Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120:1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- 4.DeGiacomo A, Fombonne E. Parental recognition of developmental abnormalities in autism. Eur Child Adolesc Psychiatr. 1998;7:131–136. doi: 10.1007/s007870050058. [DOI] [PubMed] [Google Scholar]
- 5.Mandell DS, Novake MM, Zubritsky CD. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116:1480–1486. doi: 10.1542/peds.2005-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howlin P, Moore A. Diagnosis of autism. Autism. 1997;1:135–162. [Google Scholar]
- 7.Siegel B, Pliner C, Eschler J, Elliott GR. How children with autism are diagnosed: difficulties in identification of children with multiple developmental delays. J Dev Behav Pediatr. 1988;9:199–204. [PubMed] [Google Scholar]
- 8.Young RL, Brewer N, Pattison C. Parental identification of early behavioral abnormalities in children with autistic disorder. Autism. 2003;7:125–143. doi: 10.1177/1362361303007002002. [DOI] [PubMed] [Google Scholar]
- 9.Dale PS, Bates E, Reznick JS, Morisset C. The validity of a parent report instrument of child language at twenty months. J Child Lang. 1989;16:239–249. doi: 10.1017/s0305000900010394. [DOI] [PubMed] [Google Scholar]
- 10.Pulsifer MB, Hoon AH, Palmer FB, Gopalan R, Capute AJ. Maternal estimates of developmental age in preschool children. J Pediatr. 1994;125:S18–S24. doi: 10.1016/s0022-3476(94)70171-7. [DOI] [PubMed] [Google Scholar]
- 11.Rogers BT, Booth LJ, Duffy LC, et al. Parent's developmental perceptions and expectations for their high-risk infants. J Dev Behav Pediatr. 1992;13:102–107. doi: 10.1097/00004703-199204000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Glascoe FP. Collaborating With Parents: Using Parents' Evaluation of Developmental Status to Detect and Address Developmental and Behavioral Problems. Ellsworth & Vandermeer Press Ltd; Nashville, TN: 1998. [Google Scholar]
- 13.Glascoe FP. Parents' concerns about children's development: prescreening technique or screening test? Pediatrics. 1997;99:522–528. doi: 10.1542/peds.99.4.522. [DOI] [PubMed] [Google Scholar]
- 14.Glascoe FP, Macias MM, Wegner LM, Robertshaw NS. Can a broadband developmental-behavioral screening test identify children likely to have autism spectrum disorder? Clin Pediatr. 2007;46:801–805. doi: 10.1177/0009922807303928. [DOI] [PubMed] [Google Scholar]
- 15.Pinto-Martin JA, Young LM, Mandell DS, Poghosyan L, Giarelli E, Levy SE. Screening strategies for autism spectrum disorders in pediatric primary care. J Dev Behav Pediatr. 2008;29:345–350. doi: 10.1097/DBP.0b013e31818914cf. [DOI] [PubMed] [Google Scholar]
- 16.Ozonoff S, Heung K, Byrd R, Hansen R, Hertz-Picciotto I. The onset of autism: patterns of symptom emergence in the first years of life. Autism Res. 2008;1:320–328. doi: 10.1002/aur.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baranek GT. Autism during infancy: a retrospective video analysis of sensory-motor and social behaviors at 9–12 months of age. J Autism Dev Disord. 1999;29:213–224. doi: 10.1023/a:1023080005650. [DOI] [PubMed] [Google Scholar]
- 18.Werner E, Dawson G, Osterling J, Dinno N. Recognition of autism spectrum disorder before one year of age: a retrospective study based on home videotapes. J Autism Dev Disord. 2000;30:157–162. doi: 10.1023/a:1005463707029. [DOI] [PubMed] [Google Scholar]
- 19.Werner E, Dawson G, Munson J, Osterling J. Variation in early developmental course in autism and its relation with behavioral outcome at 3–4 years of age. J Autism Dev Disord. 2005;35:337–350. doi: 10.1007/s10803-005-3301-6. [DOI] [PubMed] [Google Scholar]
- 20.Palomo R, Belinchon M, Ozonoff S. Autism and family home movies: a comprehensive review. J Dev Behav Pediatr. 2006;27:S59–S68. doi: 10.1097/00004703-200604002-00003. [DOI] [PubMed] [Google Scholar]
- 21.Landa R, Garrett-Mayer E. Development in infants with autism spectrum disorders: a prospective study. J Child Psychol Psychiatry. 2006;47:629–638. doi: 10.1111/j.1469-7610.2006.01531.x. [DOI] [PubMed] [Google Scholar]
- 22.Nadig A, Ozonoff S, Young GS, Rozga A, Sigman M, Rogers SJ. A prospective study of response-to-name in infants at risk for autism. Arch Pediatr Adolesc Med. 2007;161:378–383. doi: 10.1001/archpedi.161.4.378. [DOI] [PubMed] [Google Scholar]
- 23.Yirmiya N, Ozonoff S. The very early phenotype of autism. J Autism Dev Disord. 2007;37:1–11. [Google Scholar]
- 24.Zwaigenbaum L, Bryson S, Rogers T, Roberts W, Brian J, Szatmari P. Behavioral manifestations of autism in the first year of life. Int J Dev Neurosci. 2005;23:143–152. doi: 10.1016/j.ijdevneu.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Bryson SE, Zwaigenbaum L, Brian J, et al. A prospective case series of high-risk infants who developed autism. J Autism Dev Disord. 2007;37:12–24. doi: 10.1007/s10803-006-0328-2. [DOI] [PubMed] [Google Scholar]
- 26.Scholle SH, Whiteside L, Kelleher K, Bradley R, Casey P. Health status of preterm low-birth-weight infants. Arch Ped Adolesc Med. 1995;149:1351–1328. doi: 10.1001/archpedi.1995.02170250057010. [DOI] [PubMed] [Google Scholar]
- 27.Glascoe FP. The value of parents' concerns to detect and address developmental and behavioral problems. J Paediatr Child Health. 1999;35:1–8. doi: 10.1111/j.1744-6155.1999.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 28.McMahon CR, Malesa EE, Yoder PJ, Stone WL. Parents of children with autism spectrum disorders have merited concerns about their later-born infants. Res Pract Pers Sev D. 2007;32:154–160. [Google Scholar]
- 29.Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30:205–223. [PubMed] [Google Scholar]
- 30.Berument SK, Rutter M, Lord C, Pickles A, Bailey A. Autism screening questionnaire: Diagnostic validity. Br J Psychiatry. 1999;175:444–451. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- 31.Corsello C, Hus V, Pickles A, et al. Between a ROC and a hard place: decision making and making decisions about using the SCQ. J Child Psychol Psychiatry. 2007;48:932–940. doi: 10.1111/j.1469-7610.2007.01762.x. [DOI] [PubMed] [Google Scholar]
- 32.Mullen EM. Mullen Scales of Early Learning. AGS; Circle Pines, MN: 1995. [Google Scholar]
- 33.Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. 2001;31:131–144. doi: 10.1023/a:1010738829569. [DOI] [PubMed] [Google Scholar]
- 34.Merin NM, Young GS, Ozonoff S, Rogers SJ. Visual fixation patterns during reciprocal social interaction distinguish a subgroup of 6-month-old infants at risk for autism from comparison infants. J Autism Dev Disord. 2007;37:108–121. doi: 10.1007/s10803-006-0342-4. [DOI] [PubMed] [Google Scholar]
- 35.Coonrod EE, Stone WL. Early concerns of parents of children with autistic and nonautistic disorders. Inf Young Child. 2004;17:258–268. [Google Scholar]
- 36.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 37.Akobeng AK. Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr. 2007;96:644–647. doi: 10.1111/j.1651-2227.2006.00178.x. [DOI] [PubMed] [Google Scholar]


