Abstract
African trypanosomiasis is a severe parasitic disease that affects both humans and livestock. Several different species may cause animal trypanosomosis and although Trypanosoma vivax (sub-genus Duttonella) is currently responsible for the vast majority of debilitating cases causing great economic hardship in West Africa and South America, little is known about its biology and interaction with its hosts. Relatively speaking, T. vivax has been more than neglected despite an urgent need to develop efficient control strategies. Some pioneering rodent models were developed to circumvent the difficulties of working with livestock, but disappointedly were for the most part discontinued decades ago. To gain more insight into the biology of T. vivax, its interactions with the host and consequently its pathogenesis, we have developed a number of reproducible murine models using a parasite isolate that is infectious for rodents. Firstly, we analyzed the parasitical characteristics of the infection using inbred and outbred mouse strains to compare the impact of host genetic background on the infection and on survival rates. Hematological studies showed that the infection gave rise to severe anemia, and histopathological investigations in various organs showed multifocal inflammatory infiltrates associated with extramedullary hematopoiesis in the liver, and cerebral edema. The models developed are consistent with field observations and pave the way for subsequent in-depth studies into the pathogenesis of T. vivax - trypanosomosis.
Author Summary
While most research efforts have focused on T. b. brucei trypanosomosis, infections caused by T. vivax and T. congolense which predominate in livestock and small ruminants have been subject to little study. In order to circumvent the major constraints inherent to studying T. vivax/host interactions in the field, we developed in vivo murine models of T. vivax trypanosomosis. We show here that the mouse experimental model reproduce most features of the infection in cattle. More than reflecting only the main parasitological parameters of the animal infection, the mouse model can be used to elucidate the immunopathological mechanisms involved in parasite evasion and persistence, and the tissue damage seen during infection and disease. Studies planned for the future will allow us to further investigate T. vivax–induced immunopathology in an experimental context for which all the necessary tools are now available.
Introduction
African trypanosomiasis, one of the most neglected diseases, consists of a number of important human and animal pathologies caused by parasitic protists of the order Kinetoplastida. Human African Trypanosomiasis (HAT), or sleeping sickness, and animal trypanosomosis, or Nagana, are vector-borne diseases, that are primarily cyclically transmitted by tsetse flies. HAT is a major public health problem in 35 sub-Saharan countries. The related animal challenge, caused by several species, i.e. Trypanosoma vivax, Trypanosoma congolense and to a lesser extent to Trypanosoma brucei brucei causes about 3 million deaths annually in cattle and has a marked impact on African agriculture, causing annual livestock production losses of about US$ 1.2 billion. T. vivax accounts for up to half of total Trypanosoma prevalence in West Africa where it is considered the major pathogen for livestock and small ruminants [1],[2],[3]. Outside tsetse endemic areas, West African T. vivax isolates were introduced long ago into South American countries where it represents a real threat since it can be efficiently transmitted across vertebrate hosts by mechanical means and by various biting flies and tabanids [4], [5], [6].
The severity of the disease depends on parasite strain, endemicity and host species, but the key steps in the T. vivax - host interactions are still largely unknown. Several pieces of evidence point to the importance of host genetic factors in determining individual susceptibility and/or resistance to this infection [3], [7], [8], [9], [10], [11]. Trypanotolerance is defined as the ability demonstrated by cattle of different genetic backgrounds to control trypanosomosis [12], [13]. It has previously been reported that increased bovine resistance to trypanosomosis is associated with more control over parasitemia and related anemia, two of the main pathogenic effects of trypanosome infections [14], [15]. However, dissimilar courses of the infection may be due to genetic polymorphism and to the virulence of the parasite isolates, thus leading to moderate, progressive and/or lethal pathologies and therefore affecting mortality rates [5], [6], [7].
It is widely accepted that if trypanosomosis is to be successfully treated in the field, a number of parameters must be taken into account, including the seasonal trypanosome prevalence and vector abundance, the severity of the disease, the magnitude of the anemia, the stock nutritional state and the prescription of an appropriate trypanocidal drug [6], [16], [17], [18]. However, the antigenic complexity of trypanosomes, their ability to expose a variety of genetically-controlled surface coat antigens (VSG), and the diversity of the immune responses presented by unrelated hosts [19], [20], [21], call for the discovery of new parasite genetic markers and more in-depth knowledge of host trypanotolerance mechanisms.
Several early studies were conducted in more affordable mouse or rat experimental models of infection in attempts to throw light on trypanotolerance, antigenic variation, the pathogenesis of intravascular coagulation, and T. vivax immunobiology and dynamics [7], [11], [19], [22], [23], [24], [25]. However, these studies used a variety of more or less virulent isolates from cattle, goats, sheep, horses and donkeys to explore the ability of T. vivax stocks to infect several intact or immunosuppressed mouse strains. Although these studies had a huge impact on research into T. vivax, the diversity of the results they yielded and the difficulties encountered in establishing axenic parasite cultures or reliable in vivo infections that entirely resemble natural infections [26], constrained the work performed with these models. In consequence, more than 20 years ago, while biological investigations into VSG and the identification of serodemas were usual for more than a few trypanosomes of the Trypanozoon subgenus, studies on T. (Dutonella) vivax VSG molecules and structure of the coat were just been encouraged [26]. Research into T. vivax then focused on characterizing parasite surface proteins or comparing genetic diversity of Western to Eastern African parasite stocks and more recently on analyzing population clonality, [10], [27], [28], [29], [30], [31], [32], [33], but somehow neglected the further development of suitable rodent models.
Now, and in an attempt to circumvent the major constraints inherent to studying T. vivax/host interactions in the field and data inconsistencies arising from the difficulties encountered in the past, we have developed in vivo murine models of trypanosomosis using a T. vivax isolate known to maintain infectivity to rodents [23]. Here we show that this T. vivax isolate retains its original characteristics after several years of cryopreservation. The parasites can grow, multiply and be transmitted in vivo following predictable kinetics in the peripheral blood of different mouse strains selected for their susceptibility or resistance to different parasite inocula. Sustained and reproducible infections are obtained that successfully mimic the dynamics of the parasitological, histological and pathological features of the infection and closely resembling those observed for cattle trypanosomosis in the field. We have thus developed reliable mouse research models that can be used to elucidate the immunopathological mechanisms involved in T. vivax infection and associated disease. It is worth noting that T. vivax was recently shown to express a functional gene involved in the non specific polyclonal activation of host B cells and that this gene is absent in more widely studied T. brucei and T. congolense [34]. Furthermore, the work presented here is expected to be a useful and complementary tool for the further studies of T. vivax immunobiology and will thus provide valuable information about trypanotolerance, Trypanosoma evasion strategies from host immune system, and immunopathogenesis.
Materials and Methods
T. vivax parasites and oligonucleotides
Trypanosoma (Dutonella) vivax stabilates (STIB 731-A), cryopreserved on September 25, 1996 after 9 passages in mice, were kindly provided by R. Brun (Swiss Tropical Institute, Basel, Switzerland). STIB 731-A stabilates were originally prepared in November 1982 using bloodstream forms of IL 1392 T. vivax stock obtained from the blood of goat #M918, at ILRAD (ILRI), Nairobi, Kenya. This West African IL 1392 goat stock was derived from the Zaria Y486 Nigerian isolate of a naturally infected Zebu steer maintained by 62 serial passages in mice [23]. VSG ILDat 1.2 (ILRAD Duttonella antigen type 1.2) specific primers were deduced from the VSG ILDat 1.2 full length sequence (TvY486_0004810 variant surface glycoprotein putative, 1215 bp) obtained from the GeneDB of the Zaria Y486 Trypanosoma vivax nuclear genome (Sanger Institute Pathogen Sequencing Unit (PSU), http://www.sanger.ac.uk/Projects/T_vivax/): VSG-1.2F (5′ AATTTTGGTGAGTGTCGGTGT 3') and VSG-1.2R (5' ATTTCCTCCACCACGTAGCTC 3'). T. vivax- specific forward and reverse ribosomal promoter primers were also deduced from the Zaria Y486 chromosome 3: TvrDNAF (5' CTGATTTCGCCACTGCTATTATTTGC 3') and TvrDNAR (5' CGCTTCACTTGATGATCGTTTCG 3'), respectively. Parasites were maintained by weekly passages in mice and new stabilates were appropriately and regularly frozen in polysoma buffer/glycerol, as previously described [11]. Blood smears were prepared from infected mouse blood, air dried, fixed in methanol for 5 minutes and further stained with 5% Giemsa for 20 minutes.
Mice and infections
Seven to 10-week-old male BALB/c (H2d), C57BL/6 (H2b) or Swiss outbred (CD-1, RJOrl:SWISS) mice (Janvier, France) were used in all the studies. Mice were injected intraperitoneally with 101–105 bloodstream forms of T. vivax obtained at the peak of parasitemia (day 8 post infection). For parasite enumeration, five microliters of blood were harvested individually from the tail vein and appropriately diluted in buffered saline when necessary. Blood parasite counts were established under a light microscope and expressed as number of parasites per milliliter of blood. All animal work was conducted in accordance with relevant national and international guidelines (see here below).
Ethics statement
All mice were housed in our animal care facilities in compliance with European animal welfare regulations. The Institut Pasteur is member of the Committee #1 of the Comité Régional d'Ethique pour l'Expérimentation Animale (CREEA), Ile de France. The Animal housing conditions and protocols used in the present work were previously approved by the “Direction des Transports et de la Protection du Public, Sous-Direction de la Protection Sanitaire et de l'Environnement, Police Sanitaire des Animaux” under the number B 75-15-28 accordingly to the Ethics Chart of animal experimentation which includes appropriate procedures to minimize pain and animal suffering. PM has permission to perform experiments on vertebrate animals #75-846 issued by the Department of Veterinary Services of Paris, DDSV and is responsible for all the experiments and protocols carried out personally or under her direction in the framework of laws and regulations relating to the protection of animals.
Hematology
50 µl of retro-orbital blood were recovered onto 0.5 M EDTA. Samples were analyzed in a Scil Vet abc (Scil, Strasbourg, France) using pre-established and normalized parameters for the different mouse strains. Peripheral reticulocytes were counted as described [35], modified by S. Bagot (personal communication). Briefly, 5 µl of blood were fixed in 1 ml of 0.25% glutaraldehyde in PBS pH 7.4 and further stained with 1 µM Hoechst 33258/Thiazole orange 0.1 µg/ml in PBS pH 7.4 for 1 h at 37°C.
Histopathology
Twenty days after infection, mice were anesthetized with an i.p. injection of 0.1 ml per 10 g mouse body weight of a solution containing 1 mg/ml xylazine (Rompun 2%, Bayer, Leverkusen, Germany) and 10 mg/ml ketamine (Imalgène 1000, Merial, Lyon, France), and then sacrificed by cervical dislocation. After a complete post-mortem examination, the spleen, liver, kidneys, lung, heart and specimens of the central nervous system were removed and immediately fixed in 10% neutral-buffered formalin. Tissue samples from these organs were embedded in paraffin; five-micrometer sections were cut and stained with hematoxylin and eosin (HE).
Statistical analyses
All the experiments were performed two or three times using at least 5 mice per experimental group and per time point. Mice were analyzed individually and the differences between the groups used in this study were tested for statistical significance using Student's test or the Log-rank (Mantel-Cox) test whenever appropriate (Prism software, Graph Pad, San Diego, CA). Data are expressed as arithmetic means are presented as arithmetic means +/− the standard deviation (SD) of the means.
Results
Trypanosoma vivax molecular and phenotypic characterization
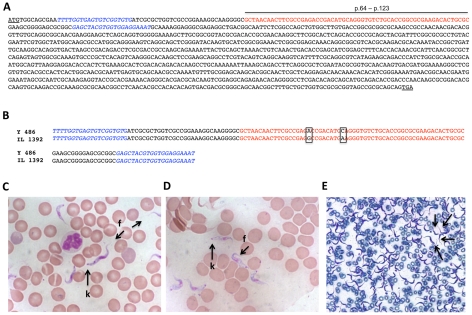
The IL 1392 West African stock of T. vivax is derived from the Nigerian isolate Zaria Y486 [23] which is infective for rodents and can be cyclically and/or mechanically transmitted [36], [37]. Rodent-infective derived clones of Y486 T. vivax, notably the IL 1392, have already been shown to express VSG ILDat 1.2 (ILRAD Duttonella antigen type 1.2) [19], [28], [38], [39] in a relatively stable fashion. This VSG can be readily recognized by its specific 20 amino acid N-terminal sequence (ANNFAETDMEGVCTGALTLR) [30], [31]. As can be seen in Figure 1A, VSG-1.2 forward and VSG-1.2 reverse oligonucleotide primers were deduced from the full length ILDat 1.2 gene sequence and flanking this 20 amino acid specific sequence. PCR reactions were then used to ascertain the identity of the initial IL 1392 T. vivax stabilate used in the present work, as previously shown [30], [31]. VSG-1.2F and VSG-1.2R primers amplified a 148 bp fragment of genomic DNA in IL 1392 bloodstream forms, and when sequenced, this showed more than 99% similarity with ILDat 1.2 and only 2 point mutations as compared to Zaria Y486 (See Fig. 1B), confirming the presence of ILDat 1.2 VSG from the rodent infective West African T. vivax 1392 isolate, not reactive with Eastern T. vivax strains or with DNA from T. brucei and T. congolense [27], [28], [40] It is also worth noting that a PCR reaction comprising TvDNAF (forward) and TvDNAR (reverse) oligonucleotides amplified a 1,8 kb DNA product whose sequence was flanked by the two primers and presented 95% homology to the highly specie-specific ribosomal promoter of the Y486 T. vivax reference strain (not shown). Furthermore, we recently showed that the IL 1392 T. vivax genome possesses a functional proline racemase gene (TvPRAC) that is absent in other trypanosomatid genomes [34]. Altogether these results established and confirmed the molecular identity of the IL 1392 T. vivax parasites used in the present work.
Figure 1. Molecular identity of T. vivax IL 1392.
Full lengh of ILDat1.2 VSG gene (A). Initiation and stop codons are underlined. The specific T. vivax 20-amino acids sequence at the N-terminal end of the gene is depicted in red (positions 64 to 123). Forward and reverse primers used in this experiment are in italics. DNA was extracted from T. vivax bloodstream forms and amplified by PCR using VSG-1.2F and VSG-1.2R primers. A fragment of 148 bp was obtained and the resulting sequence aligned with the Y486 reference strain (B). Two point mutations are squared. Blood smears of a mouse infected with T. vivax were fixed and stained with Giemsa (C and D); k = kinetoplast, f = flagellum. The high number of circulating parasites at the peak of parasitemia can be evaluated in the picture (E).
IL 1392 T. vivax bloodstream forms readily infected all mouse strains tested and were regularly maintained hereafter in the laboratory without losing infectivity through weekly passages in 7- to 8-week-old outbred Swiss (outbred) mice (CD-1, RJOrl:SWISS) (Janvier, France) by intra-peritoneal (i.p.) injection of 103 parasite forms. As can be seen in Figures 1C and 1D, the parasites showed a predominantly slender morphology, an anterior free flagellum and a narrow posterior end containing a large sub terminal kinetoplast, similar to stained trypanosomes from cattle, as previously described [10], [23]. Figure 1E shows large numbers of T. vivax in blood, at the peak of parasitemia in outbred mice.
Comparison of in vivo infections in mouse strains using T. vivax Y486-derived IL 1392 stock
Despite the high degree of gene synteny observed in kinetoplastids, genes coding for essential proteins associated with key metabolic reactions are not necessarily ubiquitous among members of the order. Accordingly, T. vivax but not Trypanosoma brucei, Trypanosoma congolense nor Leishmania spp possesses a TvPRAC enzyme responsible for the interconversion of L- and D-proline enantiomers [34]. This enzyme, earlier described in Trypanosoma cruzi parasites, was shown to be essential for parasite metabolism and triggers non-specific polyclonal B cell responses in the host thus contributing to mechanisms of parasite escape from the host immune system [41], [42]. Taking into account the fact that T. vivax multiplies extracellularly in the host bloodstream, unlike the intracellular and extracellular T. cruzi, it is conceivable that TvPRAC may also play a role in triggering non specific polyclonal B cell responses, contributing to antibody diversity, host immunosuppression, parasite evasion and persistence. In an attempt to further address these questions, we decided to develop a reliable and consistent mouse model and for this purpose studied several parasitological, hematological and immunological parameters of the infection using a parasite stock of defined antigenic identity.
The experimental murine infection was initially studied using 7 to 8-week-old intact BALB/c inbred mice infected with different inocula (101 to 105) of ILRAD 1392 T. vivax bloostream forms. The initial results showed that appearance of parasitemia was highly dependent upon the number of parasites injected as parasites could be detected as early as two days post-injection when a high inoculum (105) was used, while three to six days were necessary when lower parasite numbers were injected (101 to 104) (not shown). Death seemed to correlate with parasite load since average time to death was also dependent on the number of parasites in the inoculum (not shown). Thus, the more elevated the parasite inoculum, the lower the survival rate, corroborating published data based on the original parasite isolate [43].
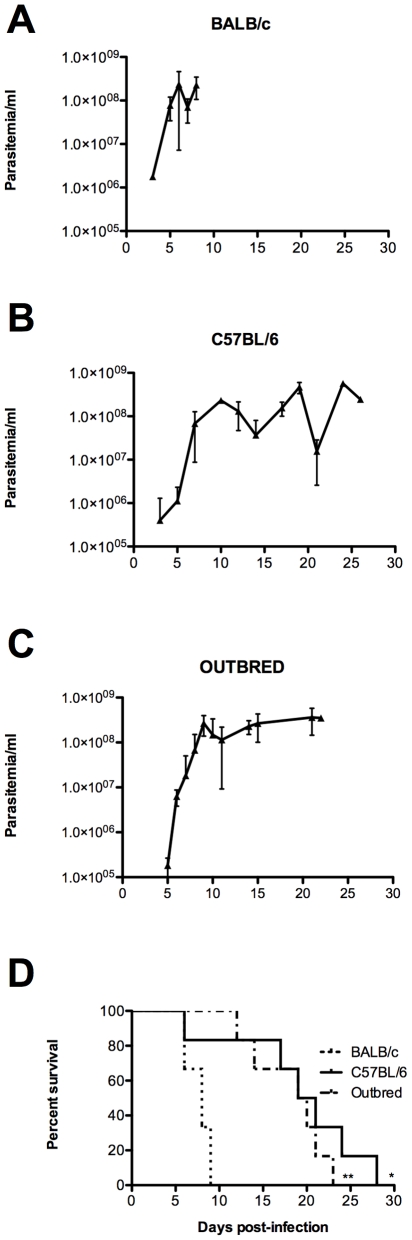
In order to compare the impact of host genetic background on the establishment of infection, we then conducted studies using BALB/c (H2d), another inbred mouse strain (C57BL/6) which bears a different haplotype (H2b), and an outbred mouse stock, all infected with an inoculum consisting of 102 bloodstream forms of T. vivax. BALB/c mice showed a rapid and pronounced increase in parasitemia that reached 4.108 parasites/ml, as recorded by daily monitoring (Fig. 2A). As compared to BALB/c and C57BL/6, detectable parasitemia (4–6 days post infection - d.p.i.-, ≥104 parasites/ml) was slightly delayed following infection of the outbred mice (Figures 2B and 2C). While parasitemia in all three mouse strains reached maximum levels 6 to 8 days post-infection, survival rates were significantly higher in the C57BL/6 and outbred mice than in the BALB/c mice which died in the first week of infection (Figure 2D). Moreover, while outbred mice showed a parasitemia plateau after 10 days of infection, recurrent parasitemia peaks were observed in the C57BL/6 mice over the same period, as also observed by De Gee et al. [7] and Mahan & Black [19], indicating that the C57BL/6 mice were partially controlling the parasite load.
Figure 2. Effect of host background on parasite load and fate.
BALB/c, C57BL/6 or Outbred mice were injected i.p. with 1×102 bloodstream forms of T. vivax and the mean parasitemia recorded individually during infection (A, B, C). Mean mortality (D) is depicted compared to BALB/c mice. Results are given as arithmetic means ± standard deviations of at least three independent experiments. Cumulative mortality was recorded over time for all groups and Kaplan-Meir survival curves plotted for the three mouse strains (D); Comparison between survival curves was performed using Log-rank Mantel-Cox test: * p<0.028, ** p<0.0018, when compared with BALB/c survival.
T. vivax experimental infection results in major changes in hematological parameters
Since BALB/c mice proved to be highly susceptible to the infection, we continued our studies using only C57BL/6 and outbred mice as these were able to endure the infection over a longer period of time. Microscopic examination of the peripheral blood of infected animals indicated an apparent loss of red blood cells, concomitant with high levels of parasitemia. To monitor this phenomenon, peripheral blood samples taken from individual mice were analyzed throughout the infection and subjected to hematological analysis. Complete blood counts showed similar and severe changes in both mouse strains (Figure 3). Firstly, hemoglobin concentrations were significantly decreased in both C57BL/6 (from 13.3±0.1 to 5.7±1.0 g/dl) and outbred mice (14.7±0.2 to 7.2±0.6 g/dl). This decrease was associated with a fall in the red blood cell counts (from 8.5±0.1 to 3.7±0.8 106 cells/mm3 and from 9.0±0.1 to 4.3±0.4 106 cells/mm3 in the C57BL/6 and outbred mice, respectively) and in hematocrit values (from 42.7±0.5 to 20.6±3.6% and from 49.6±0.9 to 25.4±2.4% in the C57BL/6 and outbred mice, respectively) (Fig. 3A, 3B and 3C). Taken together, these alterations indicated that the infection gave rise to severe anemia as reported for natural cases of bovine trypanosomosis caused by T. vivax [6], [44]. An evaluation made to measure immature red cell production in the blood showed a transient 5-fold increase in the number of reticulocytes 14 days post-infection (data not shown). Although only 20% of the injected animals were still alive 20 days post-infection, these results suggest that, at the time of death, the mice were suffering from regenerative, normocytic and normochromic anemia.
Figure 3. T. vivax induces major perturbations in hematological parameters and causes severe thrombocytopenia.
8-week-old Outbred (white symbols) or C57BL/6 (black symbols) mice were injected i.p. with 1×102 bloodstream forms of T. vivax. Blood samples were collected individually every 2–3 days and red blood cell counts (RBC, A), hematocrit (HCT, B), hemoglobin concentrations (HGB, C), leukocytes (WBC, D) and platelets (PLA, E), were determined. Results are given for days 5, 10, 15 and 20 as arithmetic means ± standard deviations of at least three different experiments with 3–5 mice per time point/experimental group. *** p<0.001, ** p<0.01, * p<0.05, when compared with samples from day 0. $ = not determined on day 10 for C57BL/6 mice.
Also, severe thrombocytopenia reported as an universal complication in the course of trypanosome infections [45] was observed in both the outbred and C57BL/6 mice, stemming from a dramatic fall in the platelet count as early as seven to ten days post-infection (Figure 3D). In addition, and except during the initial increase in white blood cell counts seen in the first days of the infection, a leucopenia was observed as the infection progressed and was more pronounced in the C57BL/6 mice (Figure 3E). The number of circulating lymphocytes fell significantly during the second week of infection, more precisely at around 20 d.p.i for the outbred mice and was accompanied by an increase in neutrophils and monocytes, as previously described with another Y-486 derived strain of T. vivax and albino mice [22] (see accompanying paper).
Marked to severe liver and spleen lesions
The extent of the tissue damage caused by T. vivax infection was assessed by means of anatomic pathological and histopathological examinations. Here, we chose to use the highly reproducible outbred model as it gave lower inter-individual differences within the mouse groups and sustained and elevated parasitemia. Outbred mice were infected with 1×102 parasites and a general anatomic pathological assessment of disturbances was conducted 20 days post-infection. At necropsy, gross lesions were observed only in the spleen and liver; the other organs were macroscopically normal. The spleens were uniformly enlarged, thereby characterizing marked splenomegaly, but did not show any congestion. They were firm and a little blood oozed from the cut surfaces. Randomly scattered white or red foci, ranging from 1 to 5 mm in diameter were observed on the capsules and the cut surfaces. Livers showed discrete, pale red or sometimes white foci that were sharply delineated from the adjacent parenchyma. These foci varied in size from 0.5 to 2 mm.
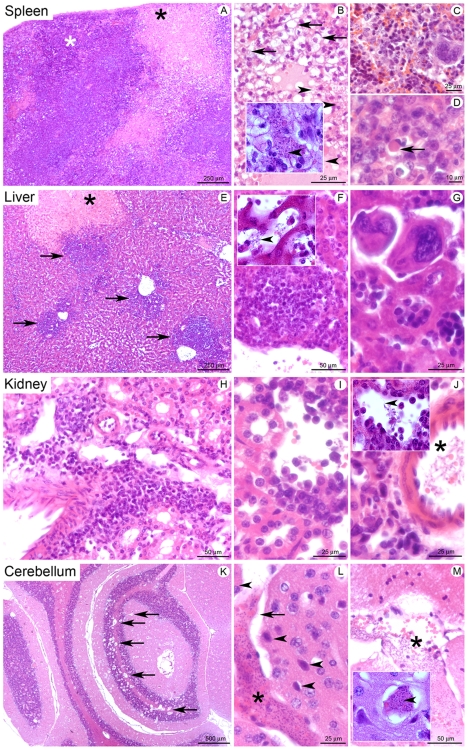
Histopathological analyses showed an elevated T. vivax load in the tissues observed along with multifocal inflammatory infiltrates in different organs, extramedullary hematopoiesis in the liver and cerebral edema
The tissues of outbred mice infected with T. vivax were also subjected to histopathological analysis 20 days post-infection. Lymphoid and non-lymphoid organs showed significant lesions (Figure 4). The spleens of infected animals (Figures 4A to 4D), showed diffuse lesions, more diffuse at the periphery of the organ, involving both the red and white pulps (Figure 4A). Lesions in the red pulp were characterized by necrosis with replacement of the normal tissue by an acidophilic and amorphous to fibrillar material containing cell debris, fibrin, extravasated erythrocytes and trypanosomes that were often clustered together in hemorrhagic foci (Figure 4B and inset arrowhead). Extramedullar hematopoiesis foci were reduced in number (Figure 4C). The white pulp showed disorganized lymphoid structure associated with marked infiltration by activated macrophages displaying vesiculous, euchromatic and nucleolated nuclei and abundant acidophilic cytoplasm. Infiltration by several lymphocytes and plasma cells was also noted (Figure 4D). Numerous plasma cells called ‘Mott cells’, characterized by their round shape and a polar cytoplasm containing stored immunoglobulins (Russel bodies), were observed in both the red and white pulps (Figure 4D, arrow). Collectively, these lesions were characteristic of diffuse, sub acute, necrotizing and hemorrhagic splenitis, associated with intralesional trypanosomes.
Figure 4. Histopathological study of mice infected with Trypanosoma vivax.
8-week-old Outbred mice were injected i.p. with 102 bloodstream forms of T. vivax and different lymphoid and non lymphoid organs were harvested for histopathological examination 20 days post-infection. Spleen (A–D): (A) Diffuse lesions characterized by large necrotic foci in the red pulp (black star), associated with lymphoid tissue disorganization in the white pulp (white star). (B) Infiltration of a necrotic focus by activated macrophages (top of the Fig., arrows) and trypanosomes (arrowhead shows very small basophilic points in the inset depicting a higher magnification). (C) Presence of lower density hematopoiesis compared to non-infected mice. (D) Infiltration of the white pulp by activated macrophages and presence of a Mott cell (arrow). Liver (E–G): (E) Multifocal inflammatory lesions centered on portal tracts/centrilobular veins (arrows), and focal necrotic focus (star). (F) Peri-venous inflammatory infiltrate composed of plasma cells (mostly), but also lymphocytes and macrophages. In the inset depicting a higher magnification, arrowhead points to trypanosomes in the vascular spaces. (G) Foci of extramedullary hematopoiesis. Kidney (H–J): (H) Interstitial inflammatory infiltrates (I) mostly composed of plasma cells. (J) Trypanosomes in an arcuate artery (star); in the inset depicting a higher magnification, arrowhead points to trypanosomes in the vascular spaces. Cerebellum (K–M): (K) Multifocal lesions centered on blood vessels (arrows). (L) Blood vessel lumen filled by trypanosomes, proteins and erythrocytes (star), with perivascular edema (arrow) and ischemic neurons (arrowheads). (M) Trypanosomes in a meningeal blood vessel. Hematoxylin-eosin staining, scale bars are indicated at the bottom of each photograph. In the inset depicting a higher magnification, the arrowhead points to trypanosomes.
A multifocal to coalescing lesion, primarily centered on the portal tracts but also involving centrilobular veins, was observed in the liver (Figure 4E). As can be seen, the lesion was characterized by marked infiltration of plasma cells, lymphocytes and macrophages (Figure 4F). Trypanosomes were frequently observed in the vascular spaces, i.e. sinusoids and the portal and terminal hepatic veins. Many necrotic foci were also observed, randomly distributed in the liver parenchyma and associated with hemorrhages and trypanosomes (Figure 4F, inset arrowhead). A very high density of extramedullar hematopoiesis foci was noted in the liver sinusoids (Figure 4G). Collectively, these lesions were characteristic of multifocal to coalescing necrotizing and hemorrhagic hepatitis, associated with extramedullary hematopoiesis and intralesional trypanosomes.
The infection also induced bilateral, multifocal and sub acute tubulointerstitial nephritis, as can be seen in Figures 4H to 4J. The kidneys showed bilateral multifocal lesions, mostly involving the renal cortex and characterized by interstitial perivascular and periglomerular infiltration of plasma cells, lymphocytes and macrophages (Figures 4H and 4I). Very few neutrophils were seen in this lesion. Some randomly distributed tubular epithelial cells were noted, showing acidophilic cytoplasm and a condensed hyper basophilic (pycnotic) and/or fragmented nucleus (necrotic cells). Trypanosomes were observed in the blood vessels, mostly in the arcuate arteries at the corticomedullary junction (Figure 4J, star and 4J, inset arrowhead).
The histopathological investigation of the central nervous system also discovered multifocal lesions centered primarily on small and medium-sized veins, and more severe in the cerebellum (Figure 4K). Evidence was often noted of dilatation and filling of the blood vessel lumen by erythrocytes, proteins and numerous trypanosomes. Vasogenic edema was observed, characterized by the presence of an amorphous and unstained material accumulated in perivascular spaces. Some angular and shrunken neurons close to these lesional blood vessels contained acidophilic cytoplasm and a condensed hyper basophilic nucleus, characteristic of ischemic necrosis (Figure 4L). Trypanosomes were also seen in the meningeal blood vessels (Figure 4M, star and inset, arrowhead).
Interestingly, and although observed in only a few animals, moderate lymphoid hyperplasia was noted in the lymph nodes, apparently associated with intravascular or intrasinusal trypanosomes, as previously described in ruminants [46] (not shown). In addition, histopathological examination of the heart, revealed the presence of numerous parasites in the ventricular cavities as well as in the blood vessels located in the periphery of the myocardium in some mice. Some of these lesions were accompanied by an infiltration of mononuclear cells (multifocal myocarditis), i.e. plasmocytes, lymphocytes and macrophages. These findings are suggestive of a myocardial commitment induced by the infection and are consistent with the congestive heart failure that has previously been reported for cattle trypanosomosis [26], [47], [48].
Discussion
While Human African Trypanosomiasis (HAT) has drawn the attention of many research groups over the last three decades, lesser consideration has been given to animal trypanosomosis (Nagana) despite its considerable impact on the development and fertility of livestock and the economical hardship it causes in several countries. Most studies, both in the distant past and more recently, have concentrated on analyzing the genetic factors involved in tolerance to trypanosomosis, or on describing the general deregulation of the immune response as expressed by a few individuals in different cattle species in the field [13], [49], [50], [51], [52], [53], [54], [55], [56]. For instance, T. brucei, which is of little clinical importance in livestock, has generally constituted the parasite of choice in experimentally and genetically controlled studies [57], [58], [59], [60]. But trypanosomosis, which is overwhelmingly the most prevalent cattle illness in Africa and South America, is mainly caused by T. vivax and T. congolense. The hallmark of their pathogenesis in the field is severe anemia accompanied by a general immunosuppressive condition [6], [21]. Since various types of tissue damage have been described for ruminants, horses, sheep and goats, distinct strategies are used to explain host resistance (“tolerance”?) or susceptibility to trypanosomes and/or the etiology of the lesions and tissue damage observed [20], [25], [61], [62], [63]. To overcome these difficulties, several experimental models were developed in rats and mice (see [21] for a review). Athough these studies showed that the mouse was potentially an important tool in understanding the pathogenesis of trypanosomosis and most particularly the immunobiology of host-parasite interactions, most subsequent studies focused on trypanosomes of the subgenus Trypanozoon (i.e. T. brucei) leaving T. (Duttonella) vivax infections poorly characterized. Thus, despite the fact that remarkable progress was made, the array of features shown by diverse stocks of T. vivax isolates has not painted a clear picture of the factors that could be central to the development of appropriate immuno(chemo)therapies [15], [64].
To better investigate the relationship between trypanosomosis and genetically-controlled rodents, we therefore undertook to develop new mouse models of Trypanosoma (Dutonnella) vivax infection. This parasite not only differs from other trypanosomes belonging to the Trypanozoon subgenus (i.e. T. brucei and T. equiperdum, but not T. evansi) with regard to its transmission and tissue distribution in the host, but also is generally recognized as possessing diverse isolates which may or not express the ability to infect laboratory rodents [10], [23], [36],[65]. For instance, East African isolates are known to induce mild infections and hemorhagic syndromes in cattle and only some stocks are adapted to rodents. Conversely, West African T. vivax isolates, obtained at different stages of natural infection, are responsible for the majority of trypanosomosis cases in cattle and other ruminants and may express mild, intermediate or high virulence to mice [7], [65]. The work presented here used a well characterized West African T. vivax isolate which is infective to rodents (IL 1392) [19], [23], [28], [31], [38], [39] and describes in detail the parasitological, hematological and histopathological parameters of the infection in different inbred and outbred mouse strains. IL 1392 was chosen for its stable expression of VSG ILDat 1.2, characteristic of rodent-adapted West African T. vivax isolates that together with closely related South American stocks pertain phylogenetically to the same clade [66]. Initially, our studies showed that the IL 1392 isolate, retained its infective characteristics and mouse infection profile after a long cryopreservation period (see Material and Methods) [11], [22]. In addition, the experimental mouse models used in this work proved easy to handle on infection and reflected the general characteristic features observed in livestock, namely the remodeling of secondary lymphoid organs, cardinal severe anemia, genetically-related differences in resistance to the parasite (but not to death) and the development of multifocal tissue hemorrhages, necrosis and consequent systemic pathologies.
Briefly, the work confirmed widespread observations that BALB/c mice are highly susceptible to T. vivax infection with the shortest survival time as compared to C57BL/6 or outbred mice. Furthermore, the BALB/c but also C57BL/6 and outbred experimental mouse models showed an early exponential increase in parasitemia, closely resembling acute trypanosomosis in the field [46]. Regardless of the fact that C57BL/6 and outbred mice proved to be more “tolerant” than BALB/c to T. vivax, limiting the pathological consequences of the infection and delaying mortality, all the mice presented common pathognomonic signs of the disease, such as anemia, cachexia, thrombocytopenia associated with high parasitemia and a tendency to leucopenia in the terminal stages [22], [45], [67]. As frequently observed in cattle and goats infected by T. vivax, the histopathological analysis of mouse tissues committed by the infection showed accumulation of trypanosomes nuclei and debris in the blood vessels of mouse spleen, liver and brain. Some extravascular foci associated with intense inflammatory and degenerative tissue disorders and cerebral edema were also observed [5], [22], [68]. It is noteworthy that both the red and white pulps of the spleen showed severe necrosis, with germinal centers depleted of lymphocytes, which could explain the lymphopenia observed at late stages in the infection. The marked splenitis, hepatitis and central nervous system involvement with vasogenic oedema and ischemia, reflect to what extent the model is of value in studies of T. vivax pathogenesis. The characteristic erythrocytopenia experienced at the peripheral level is suggestive of a decreased erythropoiesis. However, we cannot rule out possible extravascular haemolysis, or more specific apoptosis due to an autoimmune process triggered by the infection. A detailed study of bone-marrow cell populations before and during the infection will better address these questions (see accompanying paper).
The present systematic analysis described here using different mouse strains infected with a well characterized West African T. vivax isolate showed that these models are reliable and constitute new experimental tools for the study of trypanosomosis. The studies conducted aimed to develop models that could be used in the future to gain further insight into the genetic mechanisms involved in drug resistance and the discovery of new drug targets for purposes of parasite control. However, further studies using Eastern or other Western T. vivax stocks and the present mouse strains are encouraged to better approach the influence of genetic parasite divergences on disease outcome. These models of infection will be useful in the in vivo testing of new chemicals against T. vivax trypanosomosis since tests in the definitive hosts are prohibitively expensive. Finally, the mouse models given herein provide a description of the parasitological, hematological and histopathological features of T. vivax infection and pave the way to a more in-depth understanding of the immune responses involved in disease tolerance and susceptibility to T. vivax.
Acknowledgments
We wish to thank M-C Wagner, J. Mouries and A. Bandeira for their assistance with FlowJo analyses of reticulocyte counts. We are particularly indebted to R. Brun (Swiss Tropical Institute, Basel) for providing T. vivax (stock ILRAD 1392) and M. Jones from Transcriptum, for English revisions.
Footnotes
The authors have declared that no competing interests exist.
The work and position of NC were supported by Institut Pasteur and Fonds Dedies #17 (Sanofi/Aventis/Ministere de la Recherche). GJ was supported by a Roux Fellowship, Institut Pasteur. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gardiner PR, Wilson AJ. Trypanosoma (Duttonella) vivax. Parasitol Today. 1987;3:49–52. doi: 10.1016/0169-4758(87)90213-4. [DOI] [PubMed] [Google Scholar]
- 2.Kalu AU, Oboegbulem SI, Uzoukwu M. Trypanosomosis in small ruminants maintained by low riverine tsetse population in central Nigeria. Small Rumin Res. 2001;40:109–115. doi: 10.1016/s0921-4488(00)00215-7. [DOI] [PubMed] [Google Scholar]
- 3.Njiokou F, Simo G, Nkinin SW, Laveissiere C, Herder S. Infection rate of Trypanosoma brucei s.l., T. vivax, T. congolense “forest type”, and T. simiae in small wild vertebrates in south Cameroon. Acta Trop. 2004;92:139–146. doi: 10.1016/j.actatropica.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 4.Shaw JJ, Lainson R. Trypanosoma vivax in Brazil. Ann Trop Med Parasitol. 1972;66:25–32. doi: 10.1080/00034983.1972.11686794. [DOI] [PubMed] [Google Scholar]
- 5.Batista JS, Riet-Correa F, Teixeira MM, Madruga CR, Simoes SD, et al. Trypanosomiasis by Trypanosoma vivax in cattle in the Brazilian semiarid: Description of an outbreak and lesions in the nervous system. Vet Parasitol. 2007;143:174–181. doi: 10.1016/j.vetpar.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Osorio AL, Madruga CR, Desquesnes M, Soares CO, Ribeiro LR, et al. Trypanosoma (Duttonella) vivax: its biology, epidemiology, pathogenesis, and introduction in the New World—a review. Mem Inst Oswaldo Cruz. 2008;103:1–13. doi: 10.1590/s0074-02762008000100001. [DOI] [PubMed] [Google Scholar]
- 7.de Gee AL, Shah SD, Doyle JJ. Trypanosoma vivax: courses of infection with three stabilates in inbred mouse strains. Exp Parasitol. 1982;54:33–39. doi: 10.1016/0014-4894(82)90107-2. [DOI] [PubMed] [Google Scholar]
- 8.Moloo SK, Orinda GO, Sabwa CL, Minja SH, Masake RA. Study on the sequential tsetse-transmitted Trypanosoma congolense, T. brucei brucei and T. vivax infections to African buffalo, eland, waterbuck, N'Dama and Boran cattle. Vet Parasitol. 1999;80:197–213. doi: 10.1016/s0304-4017(98)00209-x. [DOI] [PubMed] [Google Scholar]
- 9.Moloo SK, Sabwa CL, Kabata JM. Vector competence of Glossina pallidipes and G. morsitans centralis for Trypanosoma vivax, T. congolense and T. b. brucei. Acta Trop. 1992;51:271–280. doi: 10.1016/0001-706x(92)90045-y. [DOI] [PubMed] [Google Scholar]
- 10.Gathuo HK, Nantulya VM, Gardiner PR. Trypanosoma vivax: adaptation of two East African stocks to laboratory rodents. J Protozool. 1987;34:48–53. doi: 10.1111/j.1550-7408.1987.tb03130.x. [DOI] [PubMed] [Google Scholar]
- 11.Ndao M, Magnus E, Buscher P, Geerts S. Trypanosoma vivax: a simplified protocol for in vivo growth, isolation and cryopreservation. Parasite. 2004;11:103–106. doi: 10.1051/parasite/2004111103. [DOI] [PubMed] [Google Scholar]
- 12.Paling RW, Dwinger RH. Potential of trypanotolerance as a contribution to sustainable livestock production in tsetse affected Africa. Vet Q. 1993;15:60–67. doi: 10.1080/01652176.1993.9694374. [DOI] [PubMed] [Google Scholar]
- 13.Hill EW, O'Gorman GM, Agaba M, Gibson JP, Hanotte O, et al. Understanding bovine trypanosomiasis and trypanotolerance: the promise of functional genomics. Vet Immunol Immunopathol. 2005;105:247–258. doi: 10.1016/j.vetimm.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Noyes HA, Alimohammadian MH, Agaba M, Brass A, Fuchs H, et al. Mechanisms controlling anaemia in Trypanosoma congolense infected mice. PLoS ONE. 2009;4:e5170. doi: 10.1371/journal.pone.0005170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stijlemans B, Guilliams M, Raes G, Beschin A, Magez S, et al. African trypanosomosis: from immune escape and immunopathology to immune intervention. Vet Parasitol. 2007;148:3–13. doi: 10.1016/j.vetpar.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Ikede BO, Losos GJ. Pathological changes in cattle infected with Trypanosoma brucei. Vet Pathol. 1972;9:272–277. doi: 10.1177/030098587200900407. [DOI] [PubMed] [Google Scholar]
- 17.Dwinger RH, Vos J, Nieuwenhuijs J, Zwart D, van Miert AS. Studies on the influence of non-steroidal anti-inflammatory drugs upon trypanosomiasis in goats and sheep. J Vet Pharmacol Ther. 1984;7:293–301. doi: 10.1111/j.1365-2885.1984.tb00914.x. [DOI] [PubMed] [Google Scholar]
- 18.Rawlings P, Dwinger RH, Snow WF. An analysis of survey measurements of tsetse challenge to trypanotolerant cattle in relation to aspects of analytical models of trypanosomiasis. Parasitology. 1991;102 Pt 3:371–377. doi: 10.1017/s0031182000064325. [DOI] [PubMed] [Google Scholar]
- 19.Mahan SM, Black SJ. Differentiation, multiplication and control of bloodstream form Trypanosoma (Duttonella) vivax in mice. J Protozool. 1989;36:424–428. doi: 10.1111/j.1550-7408.1989.tb05540.x. [DOI] [PubMed] [Google Scholar]
- 20.Lythgoe KA, Morrison LJ, Read AF, Barry JD. Parasite-intrinsic factors can explain ordered progression of trypanosome antigenic variation. Proc Natl Acad Sci U S A. 2007;104:8095–8100. doi: 10.1073/pnas.0606206104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antoine-Moussiaux N, Magez S, Desmecht D. Contributions of experimental mouse models to the understanding of African trypanosomiasis. Trends Parasitol. 2008;24:411–418. doi: 10.1016/j.pt.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Isoun TT. The histopathology of experimental disease produced in mice infected with Trypanosoma vivax. Acta Trop. 1975;32:267–272. [PubMed] [Google Scholar]
- 23.Leeflang P, Buys J, Blotkamp C. Studies on Trypanosoma vivax: infectivity and serial maintenance of natural bovine isolates in mice. Int J Parasitol. 1976;6:413–417. doi: 10.1016/0020-7519(76)90027-8. [DOI] [PubMed] [Google Scholar]
- 24.Arowolo RO, Ikede BO. Susceptibility of a rodent-adapted strain of Trypanosoma vivax to Berenil, Samorin and Novidium. Acta Trop. 1977;34:61–64. [PubMed] [Google Scholar]
- 25.Mahan SM, Hendershot L, Black SJ. Control of trypanodestructive antibody responses and parasitemia in mice infected with Trypanosoma (Duttonella) vivax. Infect Immun. 1986;54:213–221. doi: 10.1128/iai.54.1.213-221.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gardiner PR. Recent studies of the biology of Trypanosoma vivax. Adv Parasitol. 1989;28:229–317. doi: 10.1016/s0065-308x(08)60334-6. [DOI] [PubMed] [Google Scholar]
- 27.Allsopp BA, Newton SD. Characterization of Trypanosoma (Duttonella) vivax by isoenzyme analysis. Int J Parasitol. 1985;15:265–270. doi: 10.1016/0020-7519(85)90063-3. [DOI] [PubMed] [Google Scholar]
- 28.Gardiner PR, Pearson TW, Clarke MW, Mutharia LM. Identification and isolation of a variant surface glycoprotein from Trypanosoma vivax. Science. 1987;235:774–777. doi: 10.1126/science.3810164. [DOI] [PubMed] [Google Scholar]
- 29.Dirie MF, Murphy NB, Gardiner PR. DNA fingerprinting of Trypanosoma vivax isolates rapidly identifies intraspecific relationships. J Eukaryot Microbiol. 1993;40:132–134. doi: 10.1111/j.1550-7408.1993.tb04892.x. [DOI] [PubMed] [Google Scholar]
- 30.Burleigh BA, Wells CW, Clarke MW, Gardiner PR. An integral membrane glycoprotein associated with an endocytic compartment of Trypanosoma vivax: identification and partial characterization. J Cell Biol. 1993;120:339–352. doi: 10.1083/jcb.120.2.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gardiner PR, Nene V, Barry MM, Thatthi R, Burleigh B, et al. Characterization of a small variable surface glycoprotein from Trypanosoma vivax. Mol Biochem Parasitol. 1996;82:1–11. doi: 10.1016/0166-6851(96)02687-4. [DOI] [PubMed] [Google Scholar]
- 32.Buratai LB, Nok AJ, Ibrahim S, Umar IA, Esievo KA. Characterization of sialidase from bloodstream forms of Trypanosoma vivax. Cell Biochem Funct. 2006;24:71–77. doi: 10.1002/cbf.1189. [DOI] [PubMed] [Google Scholar]
- 33.Duffy CW, Morrison LJ, Black A, Pinchbeck GL, Christley RM, et al. Trypanosoma vivax displays a clonal population structure. Int J Parasitol. 2009;39:1475–1483. doi: 10.1016/j.ijpara.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 34.Chamond N, Cosson A, Coatnoan N, Minoprio P. Proline racemases are conserved mitogens: characterization of a Trypanosoma vivax proline racemase. Mol Biochem Parasitol. 2009;165:170–179. doi: 10.1016/j.molbiopara.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 35.Hansson GK, Andersson M, Jarl H, Stemme S. Flow cytometric analysis of reticulocytes using an RNA-binding fluorochrome. Scand J Clin Lab Invest. 1992;52:35–41. doi: 10.3109/00365519209085438. [DOI] [PubMed] [Google Scholar]
- 36.De Gee AL, Ige K, Leeflang P. Studies on Trypanosoma vivax: transmission of mouse infective T. vivax by tsetse flies. Int J Parasitol. 1976;6:419–421. doi: 10.1016/0020-7519(76)90028-x. [DOI] [PubMed] [Google Scholar]
- 37.Moloo SK, Kutuza SB, Desai J. Comparative study on the infection rates of different Glossina species for East and West African Trypanosoma vivax stocks. Parasitology. 1987;95 (Pt 3):537–542. doi: 10.1017/s0031182000057966. [DOI] [PubMed] [Google Scholar]
- 38.Gumm ID. The axenic cultivation of insect forms of Trypanosoma (Duttonella) vivax and development to the infective metacyclic stage. J Protozool. 1991;38:163–171. doi: 10.1111/j.1550-7408.1991.tb04424.x. [DOI] [PubMed] [Google Scholar]
- 39.Barry JD, Gathuo H. Antigenic variation in Trypanosoma vivax: isolation of a serodeme. Parasitology. 1984;89 (Pt 1):49–58. doi: 10.1017/s0031182000001128. [DOI] [PubMed] [Google Scholar]
- 40.Vos GJ, Gardiner PR. Antigenic relatedness of stocks and clones of Trypanosoma vivax from east and west Africa. Parasitology. 1990;100 Pt 1:101–106. doi: 10.1017/s0031182000060169. [DOI] [PubMed] [Google Scholar]
- 41.Reina-San-Martin B, Degrave W, Rougeot C, Cosson A, Chamond N, et al. A B-cell mitogen from a pathogenic trypanosome is a eukaryotic proline racemase. Nat Med. 2000;6:890–897. doi: 10.1038/78651. [DOI] [PubMed] [Google Scholar]
- 42.Chamond N, Goytia M, Coatnoan N, Barale JC, Cosson A, et al. Trypanosoma cruzi proline racemases are involved in parasite differentiation and infectivity. Mol Microbiol. 2005;58:46–60. doi: 10.1111/j.1365-2958.2005.04808.x. [DOI] [PubMed] [Google Scholar]
- 43.Joshua RA. Effect of strains of mice and challenge dose on the infectivity and virulence of Trypanosoma vivax. Vet Parasitol. 1986;19:39–45. doi: 10.1016/0304-4017(86)90030-0. [DOI] [PubMed] [Google Scholar]
- 44.Silva RA, Ramirez L, Souza SS, Ortiz AG, Pereira SR, et al. Hematology of natural bovine trypanosomosis in the Brazilian Pantanal and Bolivian wetlands. Vet Parasitol. 1999;85:87–93. doi: 10.1016/s0304-4017(99)00081-3. [DOI] [PubMed] [Google Scholar]
- 45.Davis CE. Thrombocytopenia: a uniform complication of African trypanosomiasis. Acta Trop. 1982;39:123–133. [PubMed] [Google Scholar]
- 46.Losos GJ, Ikede BO. Review of pathology of diseases in domestic and laboratory animals caused by Trypanosoma congolense, T. vivax, T. brucei, T. rhodesiense, and T. gambiense. Veterinary Pathology. 1972;9:1–71. [Google Scholar]
- 47.Kimeto BA, Mugera GM, Nyaga PN. Haemorrhagic pancarditis in cattle infected with Trypanosoma vivax. Vet Parasitol. 1990;34:295–301. doi: 10.1016/0304-4017(90)90076-n. [DOI] [PubMed] [Google Scholar]
- 48.Masake RA. The pathogenesis of infection with Trypanosoma vivax in goats and cattle. Vet Rec. 1980;107:551–557. doi: 10.1136/vr.107.24.551. [DOI] [PubMed] [Google Scholar]
- 49.Assoku RK, Hazlett CA, Tizard I. Immunosuppression in experimental African trypanosomiasis. Polyclonal B- cell activation and mitogenicity of trypanosome-derived saturated fatty acids. Int Arch Allergy Appl Immunol. 1979;59:298–307. [PubMed] [Google Scholar]
- 50.Maxie MG, Losos GJ, Tabel H. Experimental bovine trypanosomiasis (Trypanosoma vivax and T. congolense). I. Symptomatology and clinical pathology. Tropenmed Parasitol. 1979;30:274–282. [PubMed] [Google Scholar]
- 51.Rurangirwa FR, Tabel H, Losos GJ, Tizard IR. Immunosuppression in bovine trypanosomiasis. The establishment of “memory” in cattle infected with T. congolense and the effect of post infection serum on in vitro (3H)-thymidine uptake by lymphocytes and on leucocyte migration. Tropenmed Parasitol. 1980;31:105–110. [PubMed] [Google Scholar]
- 52.Tabel H, Losos GJ, Maxie MG, Minder CE. Experimental bovine trypanosomiasis (Trypanosoma vivax and T. congolense). III. Serum levels of immunoglobulins, heterophile antibodies, and antibodies to T. vivax. Tropenmed Parasitol. 1981;32:149–153. [PubMed] [Google Scholar]
- 53.Dwinger RH, Murray M, Moloo SK. Parasite kinetics and cellular responses in goats infected and superinfected with Trypanosoma congolense transmitted by Glossina morsitans centralis. Acta Trop. 1990;47:23–33. doi: 10.1016/0001-706x(90)90004-j. [DOI] [PubMed] [Google Scholar]
- 54.Masocha W, Robertson B, Rottenberg ME, Mhlanga J, Sorokin L, et al. Cerebral vessel laminins and IFN-gamma define Trypanosoma brucei brucei penetration of the blood-brain barrier. J Clin Invest. 2004;114:689–694. doi: 10.1172/JCI22104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vincendeau P, Bouteille B. Immunology and immunopathology of African trypanosomiasis. An Acad Bras Cienc. 2006;78:645–665. doi: 10.1590/s0001-37652006000400004. [DOI] [PubMed] [Google Scholar]
- 56.Guilliams M, Bosschaerts T, Herin M, Hunig T, Loi P, et al. Experimental expansion of the regulatory T cell population increases resistance to African trypanosomiasis. J Infect Dis. 2008;198:781–791. doi: 10.1086/590439. [DOI] [PubMed] [Google Scholar]
- 57.Ikede BO, Akpokodje JU, Hill DH, Ajidagba PO. Clinical, haematological and pathological studies in donkeys experimentally infected with Trypanosoma brucei. Trop Anim Health Prod. 1977;9:93–98. doi: 10.1007/BF02236387. [DOI] [PubMed] [Google Scholar]
- 58.Zwart D, Brun R, Dwinger RH, van Miert AS, Franssen FF, et al. Influence of fever and flurbiprofen on trypanosome growth. Acta Trop. 1990;47:115–123. doi: 10.1016/0001-706x(90)90073-9. [DOI] [PubMed] [Google Scholar]
- 59.Radwanska M, Guirnalda P, De Trez C, Ryffel B, Black S, et al. Trypanosomiasis-induced B cell apoptosis results in loss of protective anti-parasite antibody responses and abolishment of vaccine-induced memory responses. PLoS Pathog. 2008;4:e1000078. doi: 10.1371/journal.ppat.1000078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.de Gee AL. Host parasite relationships in Trypanosoma (Duttonella) vivax with special reference to the influence of antigenic variation. Vet Q. 1982;4:32–35. doi: 10.1080/01652176.1982.9693835. [DOI] [PubMed] [Google Scholar]
- 61.Desowitz RS, Watson HJ. Studies on Trypanosoma vivax. VI. The occurrence of antibodies in the sera of infected sheep and white rats, and their influence on the course of infection in white rats. Ann Trop Med Parasitol. 1953;47:247–257. [PubMed] [Google Scholar]
- 62.de Gee AL, Rovis L. Trypanosoma vivax: absence of host protein on the surface coat. Exp Parasitol. 1981;51:124–132. doi: 10.1016/0014-4894(81)90049-7. [DOI] [PubMed] [Google Scholar]
- 63.Anosa VO, Isoun TT. Pathology of experimental Trypanosoma vivax infection in sheep and goats. Zentralbl Veterinarmed B. 1983;30:685–700. doi: 10.1111/j.1439-0450.1983.tb01894.x. [DOI] [PubMed] [Google Scholar]
- 64.Courtin D, Berthier D, Thevenon S, Dayo GK, Garcia A, et al. Host genetics in African trypanosomiasis. Infect Genet Evol. 2008;8:229–238. doi: 10.1016/j.meegid.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 65.Joshua RA. Infectivity and virulence in a serodeme of Trypanosoma vivax. Comp Immunol Microbiol Infect Dis. 1988;11:99–104. doi: 10.1016/0147-9571(88)90024-0. [DOI] [PubMed] [Google Scholar]
- 66.Cortez AP, Ventura RM, Rodrigues AC, Batista JS, Paiva F, et al. The taxonomic and phylogenetic relationships of Trypanosoma vivax from South America and Africa. Parasitology. 2006;133:159–169. doi: 10.1017/S0031182006000254. [DOI] [PubMed] [Google Scholar]
- 67.Assoku RK, Gardiner PR. Detection of antibodies to platelets and erythrocytes during infection with haemorrhage-causing Trypanosoma vivax in Ayrshire cattle. Vet Parasitol. 1989;31:199–216. doi: 10.1016/0304-4017(89)90070-8. [DOI] [PubMed] [Google Scholar]
- 68.Whitelaw DD, Gardiner PR, Murray M. Extravascular foci of Trypanosoma vivax in goats: the central nervous system and aqueous humor of the eye as potential sources of relapse infections after chemotherapy. Parasitology. 1988;97 (Pt 1):51–61. doi: 10.1017/s0031182000066737. [DOI] [PubMed] [Google Scholar]