Abstract
Evaluation of the function of heterotopic cardiac transplants has traditionally been accomplished by either manual palpation or serial biopsies. Both methods have drawbacks. Palpation can be difficult to differentiate a pulse from the graft versus a transmitted pulse from the native aorta. Serial biopsies, though accurate, require multiple laparotomies, leading to increased morbidity and possibly mortality rates. In this study we used an advanced telemetry system, consisting of an intra-abdominal implant, that was capable of continuously monitoring simultaneously several parameters of the transplanted heart and the status of the recipient. In a large animal model of heterotopic cardiac xenotransplantation (pig donor to baboon recipient), we implanted the device in 12 animals: 8 with and 4 without immunosuppression. We monitored and continuously recorded the left ventricular pressure (both peak-systolic and end-diastolic [LVEDP]), heart rate, and the electrocardiogram pattern of the transplanted heart as well as the temperature of the recipient. The left ventricular pressure proved to be the most valuable parameter to assess graft heart function. In the 4 nonimmunosuppressed cases, grafts were rejected acutely. In these cases, the end-diastolic pressure increased sharply and the heart stopped contracting when the difference between the systolic and the diastolic pressure decreased to <10 mm Hg. The earliest reproducible sign of rejection was an increased LVEDP. Among long-term survivors, the increase in diastolic pressure was gradual, indicating progressive thickening of the myocardium and decreased compliance of the ventricle. Six of 8 immunosuppressed animals died of other complications before rejecting the transplanted heart. The telemetry was also helpful to indicate early onset of fever in the recipients, thus allowing us to intervene early and prevent potentially lethal septic complications. Continuous monitoring of several parameters via telemetry allowed detection of changes associated with rejection as well as other complications at an early stage, allowing prompt intervention, treatment, and possibly reversal of rejection.
Accurate determination of transplanted heart function in a pig-to-baboon xenotransplantation model is difficult and time consuming. The traditional means to evaluate heart function include palpation, ultrasound, biopsy, and laparotomy. These methods require frequent administration of anesthesia to the baboon, increasing the risk of complications such as bleeding, infection, and adhesion formation, sometimes compromising the experiment. The monitoring of heterotopic transplantation by telemetry has been described.1–4 Herein we have described a new telemetry unit that relies mostly on left ventricular pressure versus echocardiography as described before. We have used this system for continuous monitoring of transplanted heart function.
MATERIALS AND METHODS
Animals
Twelve healthy baboons weighing 6–15 kg were used as recipients. Twelve piglets weighing 4–10 kg were used as heart donors. Using a National Institutes of Health Animal Care and Use Committee–approved protocol, we performed heterotopic heart transplantation surgery, as described elsewhere.5 Briefly, the donor pig heart aorta was anastomosed to the baboon’s abdominal aorta and the pig heart pulmonary artery to the baboon’s inferior vena cava. All baboons received immunosuppression to avoid graft rejection.
Telemetry Implant and the System
The telemetry implant consisted of a left ventricular probe, 2 electrocardiogram (ECG) leads, temperature probe, a battery unit, and a base module (Konigsberg Instruments, Pasadena, CA). The cages were modified to accommodate a receiver connected to the base station that monitored and recorded the functions (RMISS, Wilmington, DE). The software enabled continuous remote monitoring of 4 subjects at one time (DISS, Dexter, MI). The parameters included left ventricular pressure (LVP), heart rate based on LVP (LVPHR), peak-systolic pressure (PEAK), and end-diastolic pressure (END), ECG, Heart rate based on ECG (ECGHR), and recipient body temperature (TEMP). All data for these parameters were recorded on a daily basis using vendor-provided software that enabled detailed analysis of the data.
RESULTS
All hearts in the group receiving immunosuppression survived for extended periods (range 20–179 d; mean 40 d), whereas all grafts in baboons without immunosuppression were rejected within 2 days. The telemetry system provided an accurate evaluation of graft function.
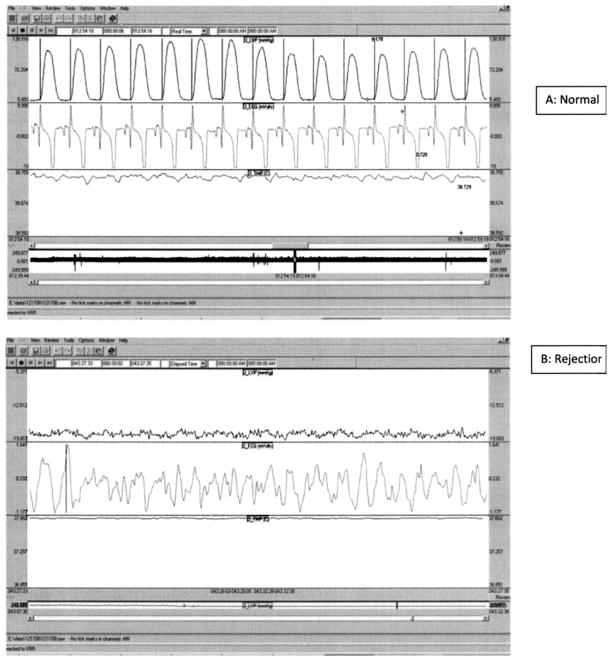
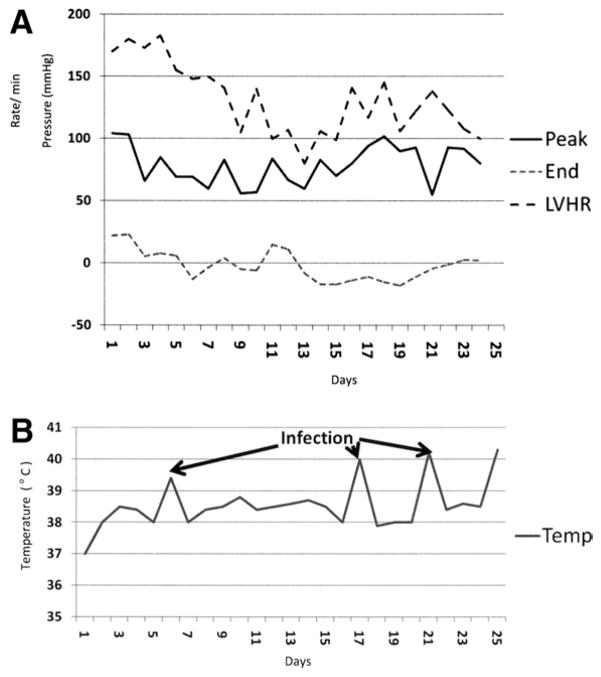
Figure 1 shows the live monitoring of 2 transplants at one time. Figure 2A shows a typical reading from a graft that was fully functional and Fig 2B a reading from a rejected graft. LVP changes and LVPHR were the most reliable measures for heart function, as seen in these figures. A slow decrease in PEAK and increased END indicated the onset of rejection, allowing proper intervention. Figure 3A shows the LVPHR and both the PEAK and the END for graft survival for the longest period, 179 days. As shown, the LVPHR was maintained throughout the length of survival except on 2 occasions when the rate dropped, which was suspected to be the onset of rejection. Investigation revealed an inability to receive immunosuppressive drugs owing to blockage of the central line by thrombus. When the line was cleared and immunosuppressive medications resumed, the heart regained function. Similarly, as shown in Fig 3B, an increase in recipient temperature properly alerted us of a possible infection; intervention with proper antibiotics averted this complication. Thus, this system provided early clues of complications which we were able to effectively prevent from progression which potentially could have led to graft and recipient loss.
Fig 1.
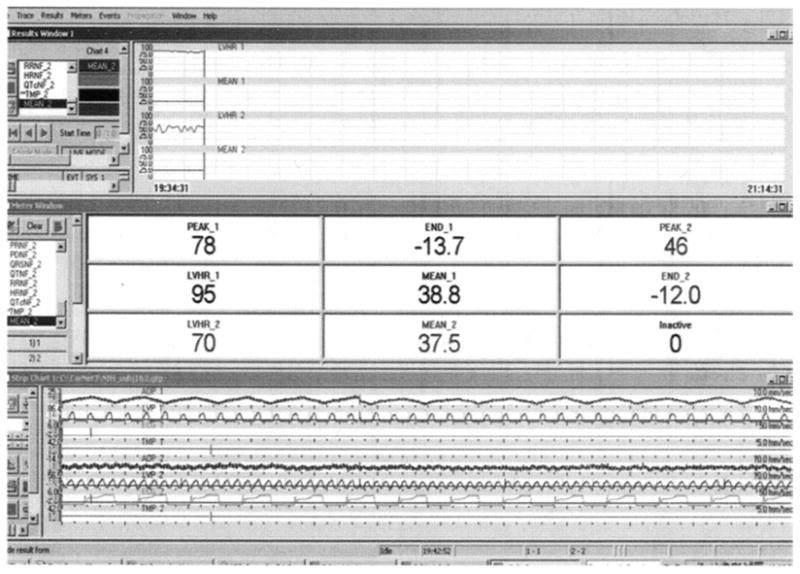
Direct view of the monitor, displaying continuous measurement of graft function by telemetry. Readings from 2 transplanted pig cardiac xenografts and recipient baboons are shown. The parameters include left ventricular peak-systolic pressure (PEAK_1, PEAK_2), end-diastolic pressure (END_1, END_2), heart rate (LVHR_1, LVHR_2), and recipient temperature (MEAN_1, MEAN_2).
Fig 2.
Telemetry interpretations of normal and rejected cardiac xenografts: A. Normal LVP and ECG readings. B. Loss of graft function indicated by abnormal LVP and ECG readings.
Fig 3.
Representative telemetry recordings from 1 baboon with long-term surviving cardiac xenograft. A. LVHR, PEAK, and END recordings of the graft function over 6 months. B. Temperature recording over 6 months.
DISCUSSION
There were several advantages to using this implantable telemetry system, including the ability to continuously monitor transplanted heart function and recipient temperature remotely, providing accurate measurements of graft survival and management of immunosuppression. We found the measurement of LVPHR to be a superior method over ECGHR, because we were able to reliably detect a loss of graft function by this method.
Although there were several advantages, we also encountered some disadvantages with this system, such as bleeding from the LVP probe insertion site, a complication that was overcome by securing the probe using 2 purse-string sutures with pladgets. Left ventricular cavity thrombus formation was also seen, owing to the probe, which was corrected by maintaining a higher heparin level. The system did not allow the use of electrical cardioversion in cases of fibrillation and needed to be removed when cardioversion was necessary.
In conclusion, this system, although complex to establish, provided reliable measurement of graft function and advanced clues in cases of infection, rejection, or loss of graft function. This system also avoided repeated anesthesia of recipient baboons to evaluate heart function by traditional means. The ability to evaluate several parameters retrospectively was an added advantage of this system.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chen RH, Kadner A, Adams DH. Monitoring pig-to-primate cardiac xenografts with live internet images of recipients and xenograft telemetric signals: histologic and immunohistochemical correlations. J Heart Lung Transplant. 2000;19:591. doi: 10.1016/s1053-2498(00)00101-7. [DOI] [PubMed] [Google Scholar]
- 2.Pirolo JS, Shuman TS, Brunt EM, et al. Noninvasive detection of cardiac allograft rejection by prospective telemetric monitoring. J Thorac Cardiovasc Surg. 1992;103:969. [PubMed] [Google Scholar]
- 3.Groeneveld WH, Kort WJ. Endpoint detection of heterotopic grafted rat hearts using an implanted transmitter. J Surg Res. 1981;31:82. doi: 10.1016/0022-4804(81)90033-0. [DOI] [PubMed] [Google Scholar]
- 4.Koike K, Hesslein PS, Dasmahapatra HK, et al. Telemetric detection of cardiac allograft rejection. Correlation of electrophysiological, histological, and biochemical changes during unmodified rejection. Circulation. 1988;78:I106. [PubMed] [Google Scholar]
- 5.Adams DH, Chen RH, Kadner A, Naficy S. Technique for heterotopic pig heart xenotransplantation in primates. Ann Thorac Surg. 1999;68:265. doi: 10.1016/s0003-4975(99)00488-9. [DOI] [PubMed] [Google Scholar]