Abstract
Background
Preclerkship clinical-skills training has received increasing attention as a foundational preparation for clerkships. Expectations among medical students and faculty regarding the clinical skills and level of skill mastery needed for starting clerkships are unknown. Medical students, faculty teaching in the preclinical setting, and clinical clerkship faculty may have differing expectations of students entering clerkships. If students’ expectations differ from faculty expectations, students may experience anxiety. Alternately, congruent expectations among students and faculty may facilitate integrated and seamless student transitions to clerkships.
Aims
To assess the congruence of expectations among preclerkship faculty, clerkship faculty, and medical students for the clinical skills and appropriate level of clinical-skills preparation needed to begin clerkships.
Methods
Investigators surveyed preclinical faculty, clerkship faculty, and medical students early in their basic clerkships at a North American medical school that focuses on preclerkship clinical-skills development. Survey questions assessed expectations for the appropriate level of preparation in basic and advanced clinical skills for students entering clerkships.
Results
Preclinical faculty and students had higher expectations than clerkship faculty for degree of preparation in most basic skills. Students had higher expectations than both faculty groups for advanced skills preparation.
Conclusions
Preclinical faculty, clerkship faculty, and medical students appear to have different expectations of clinical-skills training needed for clerkships. As American medical schools increasingly introduce clinical-skills training prior to clerkships, more attention to alignment, communication, and integration between preclinical and clerkship faculty will be important to establish common curricular agendas and increase integration of student learning. Clarification of skills expectations may also alleviate student anxiety about clerkships and enhance their learning.
Keywords: preclinical medical education, clerkships, curriculum, clinical skills, bedside teaching
Mastering clinical skills is fundamental to becoming a physician. While many medical schools continue to follow the Flexner model of teaching basic sciences in the first 2 years of medical school, the preclinical period is also a critical time for providing students with a solid introduction to and foundation in core clinical skills (1). In recent years, early clinical-skills training has received increased attention, partially due to clerkship directors’ concerns about the clinical skills of students entering clerkships (2, 3). Despite the widespread importance cited for preclerkship skills preparation and increased calls for integration between the preclinical and clerkship stages of training, few schools vertically integrate their clinical-skills curricula by establishing, coordinating, and communicating expectations for breadth and depth of skills training across the preclerkship and clerkship periods (4).
While transparent statements in educational settings about expected competencies are important, there is little formal guidance about which competencies early clinical-skills training should focus on and to what extent (5–7). Since learning occurs by the construction of new knowledge and skills on prior knowledge and skills (8, 9), the objectives of preclinical skills development are optimally correlated and aligned developmentally with basic clerkship goals. The more curricula are aligned or mapped, with clearly delineated scope and sequence, the more students will relate new learning to prior learning and build advanced understanding (10). Harden outlined the integration ladder that defines the various levels of integration, from polarization to fully integrated teaching (11). Temporal coordination – parallel teaching or concurrent teaching – defines timing for teaching topics within a subject; equally important is temporal coordination of competencies across training levels, which requires full understanding of the curriculum by teachers at different levels.
While no dominant methods have emerged for preclerkship clinical-skills training, a successful clinical-skills curriculum may use a variety of formats and settings, with clearly defined learning objectives for each activity and learning opportunities based on the ability to help students achieve objectives (12). Preclerkship contact with real patients enhances integration of theory and practice, knowledge construction and clinical reasoning, increases student motivation, and provides acclimation to clinical environments (13–15). Ideally, early patient contact occurs in the context of a series of educational experiences that build on one another (16).
‘Guided bedside learning’ uses learning communities to deliver a preclerkship clinical-skills curriculum (17–19). Under the guidance of a consistent faculty mentor, preclerkship medical students learn clinical skills at the bedside in the context of real patients through a year-long, progressive, developmental process. During training, students receive a mix of clinical-skills laboratory preparation, bedside guidance from their faculty mentor, and limited independence with the patient, using explicit competency standards. Guided bedside learning has been associated with improved student performance in basic clerkships and increased comfort starting clinical clerkships (20, 21).
As early clinical-skills training programs emerge nationally and internationally, it is important to assess the extent to which preclinical and clerkship faculty share common expectations and understanding about the ideal breadth and depth of clinical skills appropriate for the start of clinical clerkships. Alignment between preclinical and clerkship faculty should make the transition to clerkships smooth and enhance students’ clerkship experience and learning. As medical schools grow and faculty who are already spread thin with clinical, research, and teaching responsibilities are asked to assume more teaching, maintaining clarity and coordination of objectives for clinical skills at each level of medical education becomes imperative.
Prince and colleagues described medical student anxiety as they transition to clerkships (22). Some of this may result from unclear understanding of skills expected of students in clerkships. O'Brien and colleagues (23) highlighted the complex and multifaceted struggles students face as they start clerkships and called for improved communication between students and teachers early in clerkships, especially in helping students develop standards and skills for self-assessment. Development of common expectations for clinical-skills preparation between students and faculty is one pathway to reduce student anxiety, ease the transition, and maximize efficient skill improvement.
In our study, we asked three questions: What are teacher and learner expectations of clinical-skills training in preparation for clerkships? Are preclinical faculty expectations similar to those of clerkship faculty for clinical-skills preparation? What are the expectations of medical students compared with preclinical and clerkship faculty?
Methods
Context
This study was conducted at the University of Washington School of Medicine, a large, North American medical school with a preclinical curriculum that incorporates clinical-skills preparation in the preclinical setting through its colleges program (17). Thirty-seven faculty mentors work in a learning community setting to establish and implement a dynamic curriculum, teach clinical skills to second-year students, and provide ongoing mentoring. Students receive clinical-skills preparation in the inpatient setting in the context of real patients and using the curricular approach of guided bedside learning in preparation for clerkships. The core components of the guided bedside learning in the colleges program are shown in Table 1. The curriculum focuses most strongly on history taking, physical examination, communication skills, oral case presentation, and write-ups, with some focus as the year progresses to an introduction to clinical reasoning.
Table 1.
Characteristics of the preclinical ‘Guided Bedside Learning’ approach to clinical-skills training
|
Overview of research
We conducted one-time, online, anonymous surveys of: (1) preclinical faculty responsible for teaching clinical skills to second-year students through the guided bedside teaching approach; (2) basic clerkship site directors who assume overall responsibility for all medical students within a clerkship at one geographic location; and (3) medical students approximately 3 months into the start of their clerkships. By surveying students who had recently started clerkships, we hoped to capture students at a point at which they had insight into what skills are necessary and appropriate for starting their clinical years, while minimizing recall bias regarding the specifics of their preclinical training.
Instruments
Investigators (MDW, MBJ, EAG) developed three similar instruments for online administration. For each participant group, we asked what level of preparation they expected for medical students for the start of clerkships in a variety of clinical skills related to competencies, from basic (i.e., take a comprehensive history) to advanced (i.e., developing a differential diagnosis). The Likert rating scale for all three surveys was 1 = none to 5 = considerable preparation. The question wording was modified slightly to reflect the composition of each group (see Appendix 1). For the purposes of this paper, all of these will be referred to as ‘expectations for student preparation.’
Clinical skills were based on the primary topics relevant to developing basic clinical skills. They were reviewed and modified by two clinician-investigators (MBJ, EAG) as well as by several medical educators and clinician-educators, including physician and non-physician members of the medical school's basic required clerkship curriculum committee.
Demographic questions concerning teaching experience and settings were developed for the teaching faculty in order to assess whether clinical teaching experience or years teaching might explain any findings in primary analyses. In addition, basic demographic information (such as gender) was collected for all participants.
Recruitment and subjects
All recruitment was conducted by e-mail. For each subject group, we requested participation in an anonymous, online research survey with the intention of promoting quality improvement and common understanding of expectations of clinical skills for the start of clerkships. Student participants received a US$5 coffee card for completing the survey. A blinded method was employed to distribute coffee cards to students in order to ensure anonymity. The faculty received no compensation. All surveys and methods were approved as exempt by the University of Washington Human Subjects Division.
For each group, we sent an initial e-mail and two follow-up requests approximately two weeks apart. In April 2008, we requested participation of all 33 college faculty members – the preclinical faculty – who taught second-year medical students at that time. To recruit clerkship faculty, we identified required clerkship directors at each clerkship location. Initial mailings went to 97 clerkship site directors within six clerkships (internal medicine, family medicine, surgery, psychiatry and behavioral sciences, pediatrics, and obstetrics and gynecology). To recruit medical students, we e-mailed all 185 third-year medical students in their basic clerkship year in October 2008, approximately 3 months into clerkships.
Data analysis
Anonymous surveys were prepared using Catalyst, a Web-based application for course and research surveys created at the University of Washington. Completed survey results were converted to SPSS files, and analyses were performed using SPSS Version 16 for Windows. Comparisons of ratings by clerkship faculty, preclinical faculty, and medical students were performed using one-way analysis of variance; post-hoc comparisons were performed using the Bonferroni correction. A standard alpha of .05 was used for statistical significance.
Results
Participants and non-respondents
Fifty-six of 97 (58%) clerkship faculty completed surveys. Among 33 preclinical faculty serving as college mentors at the time of the study, 30 (91%) completed surveys. Of 185 medical students, 115 (62%) completed surveys.
Among the faculty, 50% of preclinical and 35.2% of clerkship faculty were women. Among medical students, 59.1% were women.
Review of the teaching experience of preclinical and clerkship faculty revealed that in both groups, 90% (n=27) of preclinical faculty and 82.1% (n=46) of clerkship faculty had 5+ years of experience teaching in a clinical setting with medical students at any level and/or residents at any level. Most (83.3%, n=25) preclinical faculty also taught students in basic clerkships. These demographic variables were therefore not used to further examine possible relationships to ratings.
Because 14 of the clerkship faculty (25%) did not teach preclinical students in addition to students in basic clerkships, we compared ratings of the expectations of students’ training by these faculty members with ratings by the clerkship faculty members who also taught preclinical students. Results were similar between the two subgroups, suggesting that the teaching setting did not contaminate groups in primary analyses.
For medical students and clerkship faculty, the demographic and teaching characteristics of respondents were compared to those of the entire groups to which surveys were mailed. Medical student respondents were compared with the entire class by gender and preclinical first-year education site (Seattle vs. non-Seattle). Clerkship faculty respondents were compared with the entire group of clerkship faculty by gender and number of years teaching clinical medicine (less than 5 years compared with 5+ years). Characteristics were similar, suggesting that respondents are representative of the groups as a whole. Because of the high response rate, we did not perform this comparison for preclinical faculty.
Expectations for clinical-skills preparation
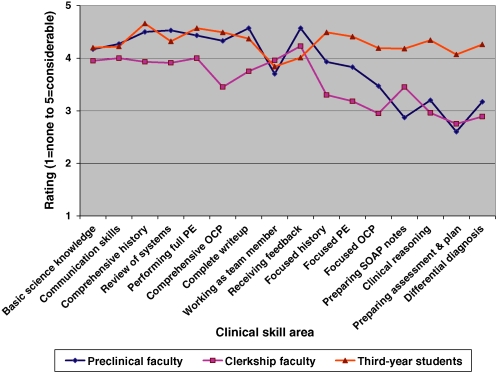
As shown in Table 2, statistically significant differences were found in all but three clinical skills areas in expectations of clinical-skills preparation for students starting clerkship. A visual representation of comparative data is shown in Fig. 1. Both preclinical faculty and medical students had higher expectations than clerkship faculty for preparation in all basic clinical skills except communication skills, working as a team member, and receiving feedback. No significant differences were found between the groups in expectations for communication skills or working as a team member. For receiving feedback, preclinical faculty had higher expectations than students.
Table 2.
Perceptions of extent of clinical-skills preparation appropriate for students beginning clerkships in basic and advanced clinical skills and in basic science knowledgea
| Preclinical Faculty | Clerkship Faculty | Third-Year Students | ||
|---|---|---|---|---|
| n=30 | n=56 | n=115 | ||
| Skill Area | Mean (SD) | Mean (SD) | Mean (SD) | Alpha |
| Basic clinical skills | ||||
| Communication skills | 4.27 (0.83) | 4.0 (0.86) | 4.22 (0.9) | ns |
| Taking a comprehensive history | 4.5 (0.57) | 3.93 (1) | 4.66 (0.56) | 0.000c,d |
| Complete review of systems | 4.53 (0.57) | 3.91 (0.98) | 4.32 (0.82) | 0.002c,d |
| Performing a full physical exam | 4.43 (0.57) | 4 (0.97) | 4.57 (0.66) | 0.000c,d |
| Comprehensive oral case presentation | 4.33 (0.55) | 3.45 (0.89) | 4.49 (0.71) | 0.000c,d |
| Complete write-up | 4.57 (0.63) | 3.75 (0.93) | 4.37 (0.72) | 0.000c,d |
| Working as a team member | 3.7 (1) | 3.96 (1) | 3.84 (1) | ns |
| Receiving feedback | 4.57 (0.57) | 4.23 (0.87) | 4.01 (1.1) | 0.017e |
| Advanced clinical skills | ||||
| Focused history | 3.93 (0.79) | 3.3 (1) | 4.49 (0.9) | 0.000b,c,d |
| Focused physical exam | 3.83 (0.83) | 3.18 (1.1) | 4.41 (0.91) | 0.000b,c,d |
| Focused oral case presentation | 3.47 (0.9) | 2.95 (0.9) | 4.19 (1) | 0.000b,c |
| Preparing SOAP notes | 2.87 (0.97) | 3.45 (1) | 4.18 (1) | 0.000 b,c,f |
| Clinical reasoning | 3.2 (0.66) | 2.96 (0.81) | 4.34 (0.8) | 0.000b,c |
| Preparing assessment and plan | 2.6 (0.62) | 2.75 (0.79) | 4.07 (1.1) | 0.000b,c |
| Differential diagnosis | 3.17 (0.65) | 2.89 (0.85) | 4.26 (0.96) | 0.000b,c |
| Knowledge-related | ||||
| Basic science knowledge | 4.17 (0.8) | 3.95 (0.8) | 4.2 (0.86) | ns |
aMean ratings on the Likert scale: 1 = none to 5 = considerable in response to questions about expectations concerning students’ preparation in skill areas and basic science knowledge for beginning third-year clerkships. Alpha < 0.05. All post-hoc tests used Bonferroni correction for multiple comparisons.
bStudents higher than preclinical faculty.
cStudents higher than clerkship faculty.
dPreclinical faculty higher than clerkship faculty.
ePreclinical faculty higher than students.
fClerkship faculty higher than preclinical faculty.
Fig. 1.
Extent of clinical skills preparation perceived as appropriate for students for the start of clerkships.
In assessing expectations for training in advanced clinical skills for the start of clerkships, there were significant differences in all seven clinical-skills areas. In all areas, students had significantly higher expectations than either preclinical faculty or clerkship faculty. In two areas (focused history and focused physical exam), the preclinical faculty had significantly higher expectations than the clerkship faculty. In one area (preparing SOAP notes), the clerkship faculty had significantly higher expectations than the preclinical faculty.
For basic science knowledge, there were no significant differences between the three groups in the extent of preparation perceived as appropriate for a student beginning clerkships.
Discussion
In a curriculum in which preclerkship clinical-skills training has been shown to improve students' early comfort with and performance in clerkships (20, 21), we found substantial differences in the expectations for clinical-skills preparation for clerkships between preclinical faculty, clerkship faculty, and medical students. Preclinical faculty and medical students had significantly higher expectations than clerkship faculty for preparation in most basic clinical skills. Students had significantly higher expectations than both faculty groups for advanced clinical skills.
The small number of differences between preclinical and clinical faculty for expectations of training in advanced clinical-skills suggests that preclinical and clerkship faculty commonly perceive that teaching advanced skills is most appropriate for the clerkship setting.
The lack of congruence between preclerkship and clerkship faculty for preparation in basic clinical skills suggests a curriculum in transition. A developmental, spiral curriculum, as posited by Harden and colleagues, requires congruence between different training settings, whether preclinical to clinical, or undergraduate to postgraduate (17, 24, 25). Communication across different levels is important, but in this case, may not have sufficiently occurred. This has important implications for the many medical schools currently, or considering, undertaking curriculum reviews and reform. Curricular reforms have the potential to initiate change in either portion of a curriculum or comprehensively. For example, in today's dominant ‘2 + 2’ Flexnerian curriculum, reform may be limited to either the first 2 years or the second 2 years. The colleges curricular innovation most strongly focuses on skills training in the preclerkship period. Data from this study indicate the need to consider curricular reforms holistically and in the case of early clinical-skills training, integrate efforts, and communicate closely with clerkship faculty. Processes, such as curriculum mapping, may be used when curricular changes occur so that innovations are fully aligned and integrated with other parts of the curriculum (10).
Students had higher expectations for advanced skill preparation than both faculty groups. Providing sustained guided bedside learning did not reduce students’ expectations of advanced preparation. This may emanate from transition anxiety or ‘shock of practice’ of students as they enter clerkships and the perception of being unprepared for and inadequate in skills they are exposed to in clerkships (26). Because students were surveyed partway into their first year of clerkships rather than at the start of the first year of clerkships, this is unlikely. Finally, students may have had insufficient communication by preclinical and clerkship faculty concerning skills and skills level expected for the start of clerkships, leading to high expectations for preparation in both basic and advanced clinical skills.
Overall, data suggest that even when clinical skills are taught within the preclinical curriculum in a curriculum with clear competency standards, there may be discrepancies between expectations of students and faculty concerning skills that should be addressed and the extent to which students should receive preparation. This highlights the need to consider and coordinate the full range of activities and curricula related to clinical-skills development, from first-year training to the final year of medical school. While this point has been highlighted in relationship to basic science education, it needs to be considered more fully for clinical-skills development.
Our data also support the findings of O'Brien et al. (23) that improved communication between students and faculty would benefit students in knowing the standards expected of them. In our setting, both preclinical and clerkship faculty need to discuss with and explain expectations to students. As more medical schools strengthen and refine early clinical-skills programs, communicating expectations at each point of training, including for the start of clerkships, will assume greater importance.
Before these communications occur, preclinical and clerkship faculty must agree on expectations. Discussions between preclinical and clerkship faculty could establish common expectations for student skills for the start of clerkships. One approach might be to have preclinical and clerkship faculty jointly develop and review competencies. This would require initial consensus on a philosophical foundation that accepts an integrated approach, works toward a seamless transition between preclerkship education and clerkships, and agrees on skills and levels appropriate at each developmental stage.
This study has several limitations. The response rate varied by group: from an excellent response rate (91%) from preclinical faculty to moderate response rates from students (62%) and clerkship faculty (58%). However, demographic and teaching characteristics of respondents were similar to the same characteristics for the entire groups to which surveys were mailed, suggesting that respondents and non-respondents were comparable. The data collected from students carry the possibility of recall bias. Students were asked to reflect back on their preclinical skills training, and to report their perception of the extent of clinical skills preparation appropriate for starting clerkships. This choice was deliberate; students who have not yet experienced clerkships are typically not yet in a position to report on which skills (and what level of skills) are needed in those settings. Further, students 3 months into clerkships may have had variable experiences in different clerkships, and thus variable perceptions on skills needed for starting basic clerkships. The survey instruments were designed using a simple Likert scale, with end anchors to help better clarify each clinical objective for students or faculty; this introduces the possibility of variable interpretations of each skill area.
The data presented here are for one medical school; studies are needed to confirm these findings in other settings with strong preclerkship focus on clinical-skills development and to ascertain whether increased communication about expectations across training levels results in increased congruence in expectations for student performance.
Curriculum reviews and reforms will benefit from holistic and vertically integrated approaches that consider all portions of the curriculum in relationship to one another. Students would benefit from improved communication with and from preclinical and clerkship faculty about expectations for clinical skills and proficiency at the start of clerkships. Both sets of faculty should reinforce this information. It is important for preclinical and clerkship faculty to develop a common philosophical understanding about the process and timing of clinical-skills development and delineation of responsibility. In a fully integrated, developmental model, clerkship faculty would have a strong sense of the preclinical curriculum for clinical-skills development and could help students to build upon and advance the skills taught by preclinical faculty. An intentional, ongoing dialogue between preclinical and clerkship faculty will optimize this process and enhance medical student education.
Appendix 1.
Question posed to each group of raters to assess clinical skill areas.
Raters: Students early in third year
Based on your experiences as an early third year student, what level of preclinical preparation for clerkships should occur in each of the following? (Rating scale: 1 = none to 5 = considerable preparation.)
Raters: Preclinical faculty
For medical students at the completion of their second year, what level of preparation do you believe is appropriate for each of the following? (Rating scale: 1 = none to 5 = considerable preparation.)
Raters: Clerkship faculty
For third-year medical students at the beginning of their clinical year (i.e., in their first or second clerkship), what level of preparation do you expect in each of the following? (Rating scale: 1 = none to 5 = considerable preparation.)
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.Omori DM, Wong RY, Aontonelli MA, Hemmer PA. Introduction to clinical medicine: a time for consensus and integration. Am J Med. 2006;118:189–94. doi: 10.1016/j.amjmed.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 2.Windish DM, Paulman PM, Goroll AH, Bass EB. Do clerkship directors think medical students are prepared for the clerkship years? Acad Med. 2004;79:56–61. doi: 10.1097/00001888-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Alexander EK. Perspective: moving students beyond an organ-based approach when teaching medical interviewing and physical examination skills. Acad Med. 2008;83:906–9. doi: 10.1097/ACM.0b013e318184f2e5. [DOI] [PubMed] [Google Scholar]
- 4.Cooke M, Irby DM, O'Brien BC. Educating physicians: a call for reform of medical school and residency. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- 5.Armstrong EG, Mackey M, Spear SJ. Medical education as a process management problem. Acad Med. 2004;79:721–8. doi: 10.1097/00001888-200408000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Matson CC, Stearns J, Defer T, Greenberg L, Ullian JA. Prerequisite competencies for third-year clerkships: an interdisciplinary approach. Fam Med. 2007;39:38–42. [PubMed] [Google Scholar]
- 7.Corbett EC, Jr, Elnicki DM, Conaway MR. When should students learn essential physical examination skills? Views of internal medicine clerkship directors in North America. Acad Med. 2008;83:96–9. doi: 10.1097/ACM.0b013e31815c68c3. [DOI] [PubMed] [Google Scholar]
- 8.Kaufman DM. ABC of learning and teaching in medicine: applying educational theory in practice. BMJ. 2003;326:213–6. doi: 10.1136/bmj.326.7382.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prince KJAH, Boshuizen HP. From theory to practice in medical education: effect on knowledge application, clinical reasoning and learning. In: Boshuizen HPA, Bromme R, Gruber H, editors. Professional learning: gaps and transitions on the way from novice to expert. Dordrecht, The Netherlands: Kluwer Academic Publishers; 2004. pp. 121–39. [Google Scholar]
- 10.Harden RM. AMEE guide no. 21: curriculum mapping: a tool for transparent and authentic teaching and learning. Med Teach. 2001;23:123–37. doi: 10.1080/01421590120036547. [DOI] [PubMed] [Google Scholar]
- 11.Harden RM. The integration ladder: a tool for curriculum planning and evaluation. Med Educ. 2000;34:551–7. doi: 10.1046/j.1365-2923.2000.00697.x. [DOI] [PubMed] [Google Scholar]
- 12.Task Force on the Clinical Skills Education of Medical Students. Recommendations for clinical skills curricula for undergraduate medical education: recommendations for preclerkship clinical skills education for undergraduate medical education. Washington, DC: Association of American Medical Colleges; 2008. [Google Scholar]
- 13.Diemers AD, Dolmans DH, Verwijnen MG, Heineman E, Scherpbier AJ. Students' opinions about the effects of preclinical patient contacts on their learning. Adv Health Sciences Educ Theory Prac. 2008;13:633–47. doi: 10.1007/s10459-007-9070-6. [DOI] [PubMed] [Google Scholar]
- 14.Diemers AD, Dolmans DH, Van Santen M, Van Luijk SJ, Janssen-Noordman AM, Scherpbier AJ. Students' perceptions of early patient encounters in a PBL curriculum: a first evaluation of the Maastricht experience. Med Teach. 2007;29:135–42. doi: 10.1080/01421590601177990. [DOI] [PubMed] [Google Scholar]
- 15.Dornan T, Littlewood S, Margolis SA, Scherpbier A, Spencer J, Ypinazar V. How can experience in clinical and community settings contribute to early medical education? A BEME systematic review. Med Teach. 2006;28:3–18. doi: 10.1080/01421590500410971. [DOI] [PubMed] [Google Scholar]
- 16.Kachur E. Observations during early clinical exposure – an effective tool or a bore? Med Educ. 2003;37:88–9. doi: 10.1046/j.1365-2923.2003.01421.x. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein EA, Maclaren CF, Smith S, Mengert TJ, Maestas RR, Foy HM, Wenrich MD, Ramsey PG. Promoting fundamental clinical skills: a competency-based college approach at the University of Washington. Acad Med. 2005;80:423–33. doi: 10.1097/00001888-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Ferguson KJ, Wolter EM, Yarbrough DB, Carline JD, Krupat E. Defining and describing medical learning communities: results of a national survey. Acad Med. 2009;84:1549–56. doi: 10.1097/ACM.0b013e3181bf5183. [DOI] [PubMed] [Google Scholar]
- 19.Irby DM, Wilkerson L. Educational innovations in academic medicine and environmental trends. J Gen Intern Med. 2003;18:370–6. doi: 10.1046/j.1525-1497.2003.21049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whipple ME, Barlow CB, Smith S, Goldstein EA. Early introduction of clinical skills improves medical student comfort at the start of third-year clerkships. Acad Med. 2006;8:S40–3. doi: 10.1097/00001888-200610001-00011. [DOI] [PubMed] [Google Scholar]
- 21.Jackson MB, Keen M, Wenrich MD, Schaad DC, Robins L, Goldstein EA. Impact of a pre-clinical clinical skills curriculam on student performance in third-year clerkships. J Gen Intern Med. 2009;26:929–33. doi: 10.1007/s11606-009-1032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prince KJ, Boshuizen HP, van der Vleuten CP, Scherpbier AJ. Students' opinions about their preparation for clinical practice. Med Educ. 2005;39:704–12. doi: 10.1111/j.1365-2929.2005.02207.x. [DOI] [PubMed] [Google Scholar]
- 23.O'Brien B, Cooke M, Irby DM. Perceptions and attributions of third-year student struggles in clerkships: do students and clerkship directors agree? Acad Med. 2007;82:970–8. doi: 10.1097/ACM.0b013e31814a4fd5. [DOI] [PubMed] [Google Scholar]
- 24.Harden RM, Davis MH, Crosby JR. The new Dundee medical curriculum: a whole that is greater than the sum of the parts. Med Educ. 1997;31:264–71. doi: 10.1111/j.1365-2923.1997.tb02923.x. [DOI] [PubMed] [Google Scholar]
- 25.Davis MH, Harden RM. Planning and implementing an undergraduate medical curriculum: the lessons learned. Med Teach. 2003;25:596–608. doi: 10.1080/0142159032000144383. [DOI] [PubMed] [Google Scholar]
- 26.Prince KJAH, Van de Wiel MWJ, Scherpbier AJJA, Van der Vleuten CPM, Boshuizen HPA. A qualitative analysis of the transition from theory to practice in undergraduate training in a PBL medical school. Adv Health Sci Educ Theory Prac. 2000;5:105–16. doi: 10.1023/A:1009873003677. [DOI] [PubMed] [Google Scholar]