Abstract
Study Objectives:
To evaluate the effect of body position on REM-related obstructive sleep apnea (OSA) patients.
Design:
Retrospective analysis.
Patients:
100 consecutive adult OSA patients (apnea-hypopnea index [AHI] ≥ 5) who had ≥ 10 min of REM sleep in both supine and lateral postures. REM-related OSA was defined by previously used criteria (REM AHI/Non-REM (NREM) AHI ≥ 2) and was compared with data from Not–REM-related OSA (REM AHI / NREM AHI < 2).
Measurements and Results:
Most (93%) of the REM-related OSA patients (n = 45) had a mild–moderate syndrome, compared to 50.9% in the Not–REM-related OSA patients (n = 55). REM-related OSA patients had a lower apnea index (AI), AHI, supine and lateral AHI, and NREM AHI, but similar REM AHI compared to the Not–REM-related OSA group. For the entire group, the following sequence was observed: AHI REM supine > AHI NREM supine > AHI REM lateral > AHI NREM lateral. Also, for the REM-related and Not–REM-related OSA patients, the interaction between supine posture and REM sleep led to the highest AHI. However, the average length of apnea and hypopneas during REM sleep was similar in the supine and lateral postures.
Conclusions:
During REM sleep, the supine position is associated with increased frequency but not increased duration of apneas and hypopneas. These body position effects prevail over the differences between REM-related and Not–REM-related OSA patients.
Citation:
Oksenberg A; Arons E; Nasser K; Vander T; Radwan H. REM-related obstructive sleep apnea: the effect of body position. J Clin Sleep Med 2010;6(4):343-348.
Keywords: Obstructive sleep apnea, REM sleep, body position
REM sleep related obstructive sleep apnea (OSA), i.e., the sleep breathing abnormality in which apneas and hypopneas are confined mainly to REM sleep periods, has lately attracted several investigations in order to find out if this is a specific clinical entity or just part of the spectrum of sleep disordered breathing. Haba-Rubio et al.1 showed that neither clinical history nor daytime sleepiness differentiated patients with REM sleep disordered breathing (SDB) and NREM SDB. They found a high occurrence of REM SDB in mild and moderate cases, and the incidence of REM SDB was similar in men and women. In another study2 aimed to evaluate the effect of gender on polysomnographic features of OSA, REM-related OSA was found in 34% of the OSA population (similar to the previous study), and was much more common in women than men (62% and 24%, respectively). This entity has recently been found to be more prevalent in women than men, and more prevalent in younger patients than older patients of both sexes.3,4 In a Spanish study of 419 OSA cases, the prevalence of REM-related OSA was similar to that seen in previous studies (32.9%) and was seen primarily in obese women with mild disease.5
BRIEF SUMMARY
Current Knowledge/Study Rationale: REM-related OSA is a sleep breathing abnormality in which apneas and hypopneas are confined mainly to REM sleep periods. It is already known that body posture has a major effect on breathing abnormalities during sleep but the effect of body posture on REM-related OSA has not been evaluated previously.
Study Impact: This study showed that body position has an important effect on breathing abnormalities during REM sleep. During this sleep stage, the supine posture has a worsening effect, facilitating the occurrence of breathing abnormalities, but the duration of these events is similar to duration of events occurring in the lateral posture. These body position effects are similar for REM-related and Not–REM-related OSA patients.
Body position has a major influence on sleep related breathing disorders.6,7 The deleterious effect of the supine posture and the helpful effect of the lateral position on sleep related breathing abnormalities have been reported consistently.8–11 However, the effect of body position on REM-related OSA has not been investigated. Thus, the aim of this study was to assess the effect of body posture in REM-related OSA patients.
MATERIALS AND METHODS
Patient Population
Data were obtained from 100 consecutive adult ( ≥ 18 years old) newly diagnosed OSA patients (AHI ≥ 5), who underwent complete polysomnographic evaluation at our sleep disorders unit from February until August 2005 and had ≥ 10 min of REM sleep in both supine and lateral postures. Unfortunately, head/neck position was not controlled for.
Of these 100 OSA patients, 21% were women. The average AHI was 25.3 ± 17.9; average body mass index (BMI) was 29.3 ± 4.6; and average age was 52.2 ± 12.3 years. Twenty-seven percent had hypertension. REM-related OSA was defined by previously used criteria1 (REM AHI / NREM AHI ≥ 2) and was compared with Not–REM-related OSA (REM AHI/NREM AHI < 2). Forty-five percent of these patients had REM-related OSA. Demographic and polysomnographic data of the entire group and the subgroups of REM-related and Not–REM-related OSA patients are summarized in Table 1.
Table 1.
Demographic and polysomnographic data of the entire group, REM-related and Not–REM-related OSA patients
| Entire group | REM-related OSA | Not–REM-related OSA | |
|---|---|---|---|
| Number of patients, n | 100 | 45 | 55 |
| Age, y | 52.2 ± 12.3 | 49.7 ± 13.7 | 54.2 ± 10.8 |
| Hypertensive, n (%) | 27 (27%) | 12 (27%) | 15 (27%) |
| Males, n (%) | 79 (79%) | 29 (64%) | 50 (91%)* |
| BMI, kg/m2 | 29.3 ± 4.6 | 29.5 ± 5.2 | 29.2 ± 4.1 |
| Sleep efficiency, (%) | 86.7 ± 11.1 | 84.3 ± 9.8 | 88.7 ± 7.3‡ |
| TST, min | 349.8 ± 44.5 | 334.1 ± 48.6 | 362.7 ± 36.4* |
| TST REM, min | 75.6 ± 20.9 | 73.5 ± 24.2 | 77.3 ± 17.9 |
| TST NREM, min | 274.2 ± 38.8 | 260.6 ± 38.7 | 285.4 ± 35.5§§ |
| TST supine, min | 164.0 ± 76.3 | 153.3 ± 81.2 | 172.7 ± 71.6 |
| TST lateral, min | 179.9 ± 73.8 | 176.5 ± 73.9 | 182.7 ± 74.3 |
| TST REM supine, min | 32.7 ± 18.1 | 35.2 ± 20.0 | 30.6 ± 16.2 |
| TST REM lateral, min | 42.9 ± 20.7 | 38.3 ± 19.7 | 46.7 ± 20.8 |
| REM sleep, % | 21.0 ± 5.1 | 21.2 ± 5.8 | 20.8 ± 4.6 |
| SWS sleep, % | 23.5 ± 9.8 | 26.6 ± 8.4 | 20.9 ± 10.1¤¤ |
| ESS, units (0-24) | 10.8 ± 5.1 | 10.1 ± 4.9 | 11.4 ± 5.3 |
| AI, events / sleep hour | 9.1 ± 15.9 | 3.4 ± 4.3 | 13.8 ± 19.9** |
| AHI, events / sleep hour | 25.3 ± 17.9 | 16.3 ± 8.7 | 32.6 ± 20.2** |
| AHI–REM | 35.7 ± 19.1 | 36.0 ± 16.3 | 35.5 ± 21.2 |
| AHI–NREM | 22.5 ± 19.1 | 11.1 ± 7.5 | 31.8 ± 20.6** |
| AHI REM / AHI NREM | 2.7 ± 2.9 | 4.5 ± 3.6 | 1.2 ± 0.4** |
| Supine AHI, events / sleep hour | 40.9 ± 24.4 | 28.2 ± 17.4 | 51.3 ± 24.4** |
| Lateral AHI, events / sleep hour | 15.2 ± 19.5 | 10.8 ± 10.4 | 18.8 ± 24.1¤ |
| Awake SpO2, % | 96.3 ± 1.2 | 96.4 ± 1.3 | 96.3 ± 1.1 |
| Min SpO2 REM, % | 80.3 ± 10.7 | 82.4 ± 9.5 | 78.6 ± 11.3 |
| Min SpO2 NREM, % | 85.5 ± 6.1 | 87.3 ± 4.5 | 83.9 ± 6.8§ |
AHI refers to apnea hypopnea index; AI, apnea index; BMI, body mass index; ESS, Epworth Sleepiness Scale; SWS, slow wave sleep; TST, total sleep time. All p-values are for differences between REM-related and Not–REM-related OSA patients:
p = 0.002,
p < 0.0001,
p = 0.004,
p = 0.001,
p = 0.03,
p = 0.003,
p = 0.016.
Overnight Polysomnographic Evaluation
Polysomnography (PSG) was performed in all cases with the Rembrandt Manager System (Medcare, Amsterdam, Netherlands) and included conventional parameters.7 Sleep stages were scored manually according to standard criteria12 by the same polysomnographic technicians during the entire study period. Apnea was defined as an episode of complete breathing cessation ≥ 10 sec (thermistor signal), and hypopnea as a reduction in oral/nasal airflow amplitude lasting ≥ 10 sec, accompanied with arousal or by a drop ≥ 3% in SpO2. The number of apnea + hypopnea events/sleep hour (AHI) was calculated, and severity of OSA was defined as mild for AHI 5-15, moderate for AHI > 15 to 30, and severe for AHI ≥ 30.13 The Epworth Sleepiness Scale (ESS)14 was used for the subjective estimation of daytime sleepiness. EEG arousals were scored according to published guidelines.15 The apnea hypopnea duration index (AHDI) was calculated for REM sleep in the supine and lateral posture and was defined as the average duration (min) of apnea + hypopnea / h of REM sleep in the defined posture.
The ethics committee of the Loewenstein Hospital-Rehabilitation Center approved the study.
Statistical analysis
For the comparison of demographic characteristics, sleep related respiratory parameters, and sleep architecture variables of REM-related and Not–REM-related groups, data were analyzed using the χ2 test for categorical variables and the 2-sample Student t-test for continuous variables (Tables 1, 2, 4). The effects on AHI indexes were analyzed using analysis of variance (ANOVA) with main factor of Group (REM-related vs. Not–REM-related) and repeated-measures factors of body posture (supine vs. lateral) and sleep stage (REM vs. NREM). The significance level was set at p < 0.05. Data analysis was performed with the SAS software package (Version 9.1; SAS Institute; Cary, NC). Results are expressed as mean ± SD.
Table 2.
Effect of body posture on AHI, AHI–REM, and Min SpO2 REM for the entire group, REM–related, and Not–REM-related OSA patients
| Supine | Lateral | |
|---|---|---|
| Entire group AHI | 40.9 ± 24.4 | 15.2 ± 19.5* |
| REM-related OSA AHI | 28.2 ± 17.4 | 10.8 ± 10.4* |
| Not–REM-related OSA AHI | 51.3 ± 24.4 | 18.8 ± 24.1* |
| Entire group AHI–REM | 54.2 ± 20.7 | 22.8 ± 23.2* |
| REM-related OSA AHI–REM | 50.0 ± 20.7 | 23.1 ± 20.6* |
| Not–REM-related OSA AHI–REM | 57.6 ± 20.2 | 22.4 ± 25.3* |
| Entire group Min SpO2REM, % | 80.9 ± 10.3 | 87.8 ± 9.1* |
| REM-related OSA Min SpO2 REM, % | 83.2 ± 9.0 | 88.1 ± 8.1** |
| Not–REM-related OSA Min SpO2 REM, % | 79.0 ± 11.0 | 87.5 ± 9.9* |
AHI refers to apnea hypopnea index; Min SpO2 REM, minimum oxygen saturation in REM sleep;
p < 0.001;
p = 0.008.
Table 4.
Effect of body posture on apnea and hypopnea duration and related parameters during REM sleep for the entire group, REM–related, and Not–REM-related OSA patients
| Entire group | Supine | Lateral | p |
|---|---|---|---|
| Av. REM sleep time, min | 32.7 ± 18.1 | 42.9 ± 20.7 | 0.0002 |
| Av. apnea duration, sec | 32.3 ± 8.7 | 36.7 ± 18.6 | ns |
| Av. hypopnea duration, sec | 30.3 ± 8.1 | 32.1 ± 10.1 | ns |
| Av. number of apnea + hypopnea events (range) | 27.2 ± 15.4 (4–87) | 15.5 ± 17.5 (0–77) | 0.0000 |
| Apnea hypopnea duration index, min / h of REM sleep | 27.9 ± 9.8 | 13.0 ± 14.2 | 0.0000 |
| REM-related OSA group | |||
| Av. REM sleep time, min | 35.2 ± 20.0 | 38.3 ± 19.7 | ns |
| Av. apnea duration, sec | 30.5 ± 7.5 | 32.3 ± 14.1 | ns |
| Av. hypopnea duration, sec | 29.7 ± 6.6 | 31.9 ± 7.7 | ns |
| Av. number of apnea + hypopnea events (range) | 25.9 ± 15.2 (4–64) | 15.6 ± 16.8 (0–77) | 0.0015 |
| Apnea hypopnea duration index, min / hour of REM sleep | 24.7 ± 9.2 | 13.0 ± 12.1 | 0.0000 |
| Not–REM-related OSA group | |||
| Av. REM sleep time, min | 30.6 ± 16.2 | 46.7 ± 20.8 | 0.0000 |
| Av. apnea duration, sec | 33.4 ± 9.4 | 40.0 ± 21.1 | ns |
| Av. hypopnea duration, sec | 30.8 ± 9.1 | 32.3 ± 12.0 | ns |
| Av. number of apnea + hypopnea events (range) | 28.3 ± 17.4 (6–87) | 15.3 ± 18.2 (0–60) | 0.0002 |
| Apnea hypopnea duration index, min / hour of REM sleep | 30.6 ± 9.5 | 13.1 ± 15.7 | 0.0000 |
RESULTS
Table 1 shows the main demographic and polysomnographic characteristics of our entire group of OSA patients as well as the REM-related and Not–REM-related OSA groups.
Demographic Data
Of 100 OSA patients, 45 fulfilled the definition for REM-related OSA; 55 had Not–REM-related OSA. The number of females was significantly higher (p < 0.001) in the REM-related OSA group. Of 45 patients with REM-related OSA, 16 (36%) were female; only 5 (9%) of 55 patients in the Not–REM-related OSA group were female. In the REM-related OSA group, the number of males decreased as the severity of the syndrome increased. There were 15 males with mild disease, 13 with moderate disease, and 1 male with severe disease. In the Not–REM-related OSA group, however, the number of men increased as the severity of disease increased: there were 8 males with mild disease, 17 with moderate disease, and 25 with severe disease.
The BMI of females in the REM-related group was significantly higher than males (33.3. ± 5.0 vs. 27.4 ± 4.0, p < 0.04). In the Not–REM-related group, the 5 females had a BMI not significantly different from males (31.7 ± 9.0 vs. 29.0 ± 3.3, respectively)
REM-related patients were younger than Not–REM-related patients, but difference did not reach statistical significance.
Polysomnographic Data
Total sleep time (TST) was higher in the Not–REM-related group, but this was due to differences in TST in NREM sleep rather than TST in REM sleep. TST in supine and lateral did not differ between the groups. The percentage of REM sleep did not differ between groups, but SWS was higher in the REM-related group, reflecting perhaps the milder form of the syndrome in these patients.
Most sleep related breathing parameters were significantly worse in the Not-REM-related group than in the REM-related group, including AHI, supine and lateral AHI, AI, AHI in NREM, and minimum SpO2 in NREM. However, subjective sleepiness as measured by the ESS did not reveal a significant difference between REM-related and Not–REM-related OSA patients.
Table 2 shows the effect of body posture on REM sleep related breathing parameters for the entire group, as well as for the REM-related and Not-REM - related patients. All REM-related breathing parameters were significantly worse in the supine posture than the lateral position for the entire group and both subgroups.
Table 3 shows the effect of body posture and REM vs. NREM sleep on AHI for the entire group as well as for the REM-related and Not–REM-related groups. Supine posture was the dominant factor influencing the AHI values. In all 3 groups, supine indexes were significantly higher than lateral indexes for both REM and NREM sleep. For the entire group of 100 OSA patients, the following sequence was observed: AHI REM supine > AHI NREM supine > AHI REM lateral > AHI NREM lateral. In addition, for the entire group, as well as for the REM-related and Not–REM-related OSA groups, interaction between supine posture and REM sleep led to the highest AHI. Supine REM indexes were significantly higher than the supine NREM indexes, except for patients in the Not–REM-related group.
Table 3.
AHI values for the supine and lateral postures during REM and NREM sleep in the three groups*
| Entire group, N = 100 | REM | NREM |
|---|---|---|
| Supine | 54.2 ± 20.7 | 37.6 ± 27.3 |
| Lateral | 22.8 ± 23.2 | 13.2 ± 21.4 |
| REM-related, N = 45 | ||
| Supine | 50.0 ± 20.7 | 22.0 ± 18.6 |
| Lateral | 23.1 ± 20.6 | 8.0 ± 9.8 |
| Not–REM-related, N = 55 | ||
| Supine | 57.6 ± 20.2 | 50.4 ± 26.8 |
| Lateral | 22.4 ± 25.3 | 17.4 ± 26.8 |
ANOVA with main factor of Group (REM-related vs. Not–REM-related) and repeated-measures factors of body posture (supine vs. lateral) and sleep stages (REM vs. NREM) yielded significant effects of sleep stage (F1,98 = 100.771, p < 0.001) and posture (F1,98 = 194.899, p < 0.001). It also revealed significant interactions of sleep stage × Group (F1,98 = 31.321, p < 0.001), posture × Group (F1,98 = 12.139, p < 0.005), and sleep stage × posture (F1,98 = 6.533, p < 0.05). A significant main effect of the Group factor was demonstrated as well (F1,98 = 333.937, p < 0.005).
Table 4 shows the effect of body posture on apnea and hypopnea duration during REM sleep for the entire group and both subgroups. In the 3 groups of patients, no differences were observed for the length of apneas and hypopneas between the supine and lateral posture. However, the numbers of apnea and hypopnea events (and consequently the apnea hypopnea duration index [AHDI], which expressed the average time spent in apnea and hypopnea/hour of REM sleep for each position), were significantly higher in supine. These data showed that, during REM sleep, the supine position is associated with increased frequency but not increased duration of apneas and hypopneas.
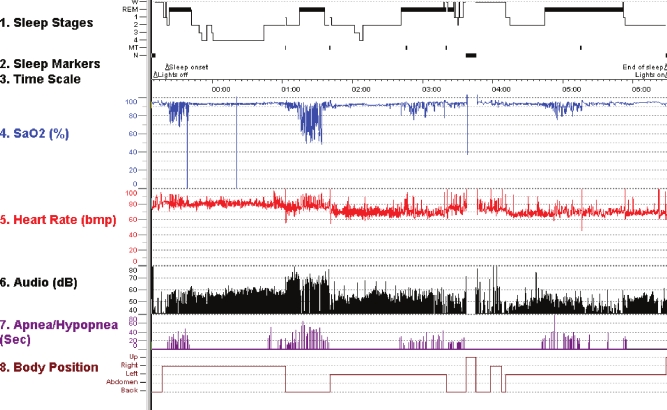
Figure 1 shows an example of body position effect on breathing abnormalities during REM sleep.
Figure 1.
The effect of body posture on a REM-related OSA patient
The figure shows: sleep stages, SaO2 (SpO2) (%), heart rate (bpm), audio (dB), apnea/hypopnea events and duration (sec), and body position changes. Note the distinct pattern of desaturation events during REM sleep in the different body postures. In this case the supine position has a worsening effect; the left side is the best sleep position for this patient. After the third REM period, the patient woke up, went to bathroom, and had difficulty resuming sleep.
DISCUSSION
There are two major findings of this study. REM-related OSA patients had a disorder significantly less severe than patients with Not–REM-related OSA. Secondly, the supine posture during sleep had a detrimental effect on both REM-related OSA patients and Not–REM-related OSA patients.
The first finding of our study is not new. Others1–5 have already found that a REM-related OSA appears to be a common finding in mild-moderate OSA, mainly in women. Accordingly, a characteristic of REM-related OSA patients is the mild-moderate form of the disease. This was clearly observed in our patients: in the REM-related OSA patients group, only 6.6% had a severe syndrome, compared to 49.1% in the NREM-related OSA.
In our population of OSA patients, the average AHI of REM-related patients was half of the average AHI in Not–REM-related patients. The differences between these groups in relation to AI were even bigger. These are not surprising results; most breathing abnormalities of these patients were concentrated in REM sleep, which represents only about 20% of TST. Accordingly, the NREM AHI of Not–REM-related OSA patients was significantly higher than the NREM AHI in REM-related OSA patients (31.8 ± 20.6 vs.11.1 ± 7.5 respectively), but REM AHI was similar in both groups (35.5 ± 21.2 vs. 36.0 ± 16.3, respectively).
A higher prevalence of women among REM-related OSA patients was also found in the present study, confirming results of others.1–5 Although 79% of our OSA patients were men (men have a higher prevalence in a treatment-seeking population of OSA patients); only 64% of REM-related OSA patients were men, compared to 93% of the Not–REM-related group.
REM-related OSA patients were also younger than Not–REM-related OSA patients (49.7 ± 13.7 vs. 54.2 ± 10.8 years), as has been previously been found by others,3–5 but this age difference did not reach statistical significance.
We did not find BMI differences between groups of OSA patients. However, in the REM-related OSA group, women were significantly heavier than men. These findings confirm the results of others5 who found, like us, that the percentage of OSA patients with hypertension was similar in both groups.
The harmful effect of the supine posture during in sleep related breathing abnormalities has been shown consistently.6–8 Sleeping in the supine posture significantly increases not only the frequency but also the severity of the abnormal breathing events.9 Accordingly, adoption of the lateral posture and avoiding the supine position during sleep could represent an effective behavioral maneuver to decrease the number of apneas and hypopneas, improve sleep quality, and reduce daytime sleepiness in many positional OSA patients.10,11
In this study we showed that the detrimental effect of the supine posture during sleep overcame the differences between REM-related and Not–REM-related OSA. The supine AHI was significantly higher than the lateral AHI for the entire group and for both the REM-related and Not–REM-related groups. However, the difference for AHI between the two postures was much higher in the Not–REM-related group. The AHI was lower, and the AHI difference between the supine and lateral posture was also smaller in the REM-related OSA group. Interestingly, supine REM AHI was significantly higher than lateral REM AHI for the whole group and for both the REM-related and Not–REM-related groups, but supine and lateral indexes for REM AHI were similar for the groups.
Since we consistently found a significant interaction between REM sleep and supine posture, and since REM-related OSA is a condition found mainly in mild- moderate OSA, our findings also suggest that night-to-night variability in mild-moderate OSA depends not just on the amount of REM and the amount of supine sleep, but the amount of supine REM sleep.
The worsening effect of the supine posture during REM sleep was observed also by comparing the minimum SpO2 levels. Minimum SpO2 levels were lower in supine than in lateral for all patients and for both REM- related and Not–REM-related groups.
The effect of body posture on the duration of the apnea /hypopnea episodes is of interest. The number of apnea and hypopnea episodes, and consequently the apnea and hypopnea time per hour of REM sleep in the defined posture (expressed by the AHDI), was higher in the supine than the lateral posture. However the average length of apneas and hypopneas events was similar for the entire group and for both the REM-related and Not–REM-related groups. During REM sleep, the supine posture facilitates the occurrence of apnea and hypopnea events; but when they occur; their lengths are not different from those in the lateral posture.
It is known that, compared to NREM sleep, during REM sleep there is an increase in the duration of apnea episodes, which causes a worsening in the desaturation events.16 Our study shows that during REM sleep, the supine posture had an additive effect on the frequency but not on the duration of apnea episodes. We previously demonstrated that the supine posture worsens apnea episodes during sleep stage 2.9 The results of the present study expand the context of the worsening effect of the supine posture to apnea events occurring during REM sleep.
The effect of body posture on breathing abnormalities during sleep has been described by many authors, searching mainly the effect of the classical positions, namely; supine, prone, and lateral postures.6 It is now clear that most of these studies oversimplified the effect of body position effect on breathing abnormalities during sleep. Not taking into consideration the effect of head/neck position on the occurrence and severity of breathing abnormalities during sleep is clearly a limitation, and this is also a limitation in the present study. Recent studies have nicely addressed this issue,17 as well as important aspects related to upper airway morphology,18–20 showing that this area is much more complex and requires further investigation.
In summary, this study showed that body position has an important effect on breathing abnormalities during REM sleep. During this sleep stage, the supine posture has a worsening effect, facilitating the occurrence of breathing abnormalities, but the duration of these events is similar to duration of events occurring in the lateral posture. These body position effects are similar for REM-related and Not–REM-related OSA patients.
DISCLOSURE STATEMENT
This was not an industry support study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Haba-Rubio J, Janssens JP, Rochat T, et al. Rapid eye movement related disordered breathing: clinical and polysomnographic features. Chest. 2005;128:3350–7. doi: 10.1378/chest.128.5.3350. [DOI] [PubMed] [Google Scholar]
- 2.O'Connor C, Thornley KS, Hanly PJ. Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med. 2000;161:1465–72. doi: 10.1164/ajrccm.161.5.9904121. [DOI] [PubMed] [Google Scholar]
- 3.Koo B, Patel S, Strohl K, et al. Rapid eye movement–related sleep disordered breathing: influence of age and gender. Chest. 2008;134:1156–61. doi: 10.1378/chest.08-1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koo B, Dostal J, Ioachimescu O, et al. The effects of gender and age on REM-related sleep-disordered breathing. Sleep Breath. 2008;12:257–64. doi: 10.1007/s11325-007-0161-7. [DOI] [PubMed] [Google Scholar]
- 5.Campos-Rodriguez F, Fernandez-Palacin A, Reyes Nunes N, et al. Caracteristicas clinicas y polisomnograficas del syndrome de apneas durante el sueno localizado en la fase REM. Arch Bronconeumol. 2009;45:330–4. doi: 10.1016/j.arbres.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Oksenberg A, Silverberg DS. The effect of body posture on sleep-related breathing disorders: facts and clinical implications. Sleep Med Rev. 1998;2:139–62. doi: 10.1016/s1087-0792(98)90018-1. [DOI] [PubMed] [Google Scholar]
- 7.Oksenberg A, Silverberg DS, Arons E, et al. Positional vs nonpositional obstructive sleep apnea patients. Anthropomorphic, nocturnal polysomnographic and multiple sleep latency test data. Chest. 1997;112:629–39. doi: 10.1378/chest.112.3.629. [DOI] [PubMed] [Google Scholar]
- 8.Richard W, Kox D, den Herder C. The role of sleep position in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2006;263:946–50. doi: 10.1007/s00405-006-0090-2. [DOI] [PubMed] [Google Scholar]
- 9.Oksenberg A, Khamaysi Y, Silverberg DS, et al. Association of body position with severity of apneic events in patients with severe nonpositional obstructive sleep apnea. Chest. 2000;118:1018–24. doi: 10.1378/chest.118.4.1018. [DOI] [PubMed] [Google Scholar]
- 10.Oksenberg A, Silverberg DS, Offenbach D, et al. Positional therapy for obstructive sleep apnea patients: A six-month follow up study. Laryngoscope. 2006;116:1995–2000. doi: 10.1097/01.mlg.0000237674.66716.a7. [DOI] [PubMed] [Google Scholar]
- 11.Oksenberg A, Silverberg DS. Avoiding the supine posture during sleep for patients with mild obstructive sleep apnea. Am J Respir Crit Care Med. 2009;180:101. doi: 10.1164/ajrccm.180.1.101. [DOI] [PubMed] [Google Scholar]
- 12.Rechtschaffen A, Kales A, editors. A manual of standardized terminology techniques and scoring system for sleep stages of human subjects. Los Angeles: Brain Information Service/Brain Research Institute, University of California at Los Angeles; 1968. [Google Scholar]
- 13.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 14.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 15.American Sleep Disorders Association. EEG arousals: Scoring rules and examples. Sleep. 1992;15:173–84. [PubMed] [Google Scholar]
- 16.Findley LJ, Wilhoit SC, Suratt PM. Apnea duration and hypoxemia during rem sleep in patients with obstructive sleep apnea. Chest. 1985;87:432–36. doi: 10.1378/chest.87.4.432. [DOI] [PubMed] [Google Scholar]
- 17.Lee JB, Park JH, Hong JH, et al. Determining optimal sleep position in patients with positional sleep-disordered breathing using response surface analysis. J Sleep Res. 2009;18:26–35. doi: 10.1111/j.1365-2869.2008.00703.x. [DOI] [PubMed] [Google Scholar]
- 18.Walsh JF, Leigh MS, Paduch A, et al. Effect of body posture on pharyngeal shape and size in adults with and without obstructive sleep apnea. Sleep. 2008;31:1543–9. doi: 10.1093/sleep/31.11.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saigusa H, Suzuki M, Higurashi N, et al. Three-dimensional morphological analyses of positional dependence in patients with obstructive sleep apnea syndrome Anesthesiology. 2009;110:885–90. doi: 10.1097/ALN.0b013e31819b5d57. [DOI] [PubMed] [Google Scholar]
- 20.Soga T, Nakata S, Yasuma F, et al. Upper airway morphology in patients with obstructive sleep apnea syndrome: effects of lateral positioning. Auris Nasus Larynx. 2009;36:305–9. doi: 10.1016/j.anl.2008.04.007. [DOI] [PubMed] [Google Scholar]