INTRODUCTION
Patients presenting with lumbosacral radicular pain due to lumbar disk herniation (LDH) often report specific events which they believe may have contributed to the onset of symptoms. Patient-identified inciting events may be physical activities, such as lifting events or sports activities, or they may be non-exertional occurrences, such as the act of coughing or sneezing. Although it is infeasible to prove a causative link between any specific inciting event and the occurrence of disk herniation, a patient’s belief in such a link alone may be sufficient to affect cognition about the risk of injury with activities and the success of a function-oriented therapeutic regimen[1].
A cumulative injury model of disk degeneration has traditionally been predominant in spine care[2]. This view of spinal degeneration suggests that disc structures are damaged through the cumulative effects of occasional excessive forces and repeated loading, often due to occupational exposures or leisure-time physical activities[3]. An injury model of disk degeneration might predict that a patient-identified inciting event was the final injury in a cascade of events culminating in annular rupture and displacement of disk material. Although some epidemiologic studies have found associations between occupational exposures and LDH or sciatica[4, 5], other studies have failed to find such an association[6-9]. Similarly, there is conflicting evidence for the possible association of leisure time physical activities with LDH or sciatica[4, 8, 10-12].
Recent investigations of disk degeneration in monozygotic twins have allowed the study of hereditary factors in addition to environmental factors[3, 13, 14]. When heredity is accounted for, leisure time physical activity and work exposures explain only a minor portion of the variance seen in disk degeneration[3]. A competing model of disk degeneration has emerged that portrays the process of degeneration as explained primarily by genetically programmed, age-activated processes. This alternative view of degeneration would suggest little relevance between patient-identified inciting events and the occurrence of LDH. However, no prior study has investigated the frequency of patient-identified inciting events in LDH.
The objectives of this study were to examine the clinical frequency of patient-identified inciting events in LDH, and to identify associations between the presence of these inciting events and the severity of the clinical presentation. Based on our clinical experience with the large variation in clinical presentations of LDH, and the results of recent genetic studies examining the role of heredity in LDH, we tested the null hypothesis that the presence of patient-identified inciting events is not associated with the severity of the clinical presentation.
METHODS
Study Participants
This study was an ancillary study to a prospective study of the outcomes of lumbar disk herniation. The study was approved by the Institutional Review Board of New England Baptist Hospital. Study participants were recruited from a hospital spine center between January 2008 and February 2009. All consecutive patients age 18 and older with lumbosacral radicular pain for < 12 weeks were evaluated for participation. Study participants received a comprehensive history and physical examination as per the standard of care in our clinic. Inclusion criteria were recent onset radicular pain (<12 weeks) in an L2, L3, L4, L5, or S1 dermatome, with or without neurologic changes, and available magnetic resonance imaging (MRI) demonstrating lumbar disk herniation corresponding with the neurologic level and side suggested by the clinical presentation. Exclusion criteria were known pregnancy; severe active medical or psychiatric comorbidities that would limit study participation; the presence of significant spinal or neuroforaminal stenosis from reasons other than lumbar disk herniation as the likely cause of radicular pain; infectious, inflammatory, or neoplastic cause of radiculopathy; significant degenerative or isthmic spondylolisthesis suspected of contributing to symptoms; and prior lumbar spine surgery at the affected level. After informed consent was obtained, the examining physician information used a standardized data sheet to record information on participant demographics, historical features, and physical examination findings.
Baseline Characteristics
We collected information on age, gender, race, comorbidity, duration of symptoms, prior history of low back pain, prior lumbar spine surgery, history of significant tobacco use, employment status, and workers compensation status. Race was categorized as ‘Asian’, ‘Black’, ‘Hispanic’, ‘Native American or Alaskan Native’, ‘Pacific Islander’, ‘White’, and ‘Other’. Comorbidities were measured using the Self-Administered Comorbidity Questionnaire (SACQ). The SACQ is widely used in orthopedic research, and has previously demonstrated reliability and validity[15]. Employment status was categorized as part-time employment, full-time employment, student, retired, disabled, and unemployed.
Patient-Identified Inciting Events
As standard practice in our clinic, we elicit and record information on inciting events that are identified by the patient as related to the onset of symptoms. An independent reviewer blinded to study design and hypotheses was trained in a systematic method of chart abstraction by a spine researcher, and information on the presence of patient-identified inciting events was obtained by retrospective chart review. An inciting event was defined as any occurrence, activity, or event that preceded or coincided with the onset of symptoms. There were no specific time restrictions as to how long before the onset of symptoms the inciting event could occur; for example, inciting events may have occurred days to weeks in advance of symptom onset, or at the precise moment of symptom onset. Inciting events were classified into one of five groups: heavy lifting, light lifting, non-lifting physical activities (sports, activities of daily living, household tasks, etc), physical trauma (motor vehicle accidents, falls, etc), and non-exertional occurrences (coughing, sneezing, bearing down, etc). Light lifting included weights of 35 lbs or less, while heavy lifting included weights >35 lbs. In situations where weights were not specified, the determination of light vs. heavy was made by the chart reviewer. In situations where no inciting event was identified, the herniation was classified as spontaneous.
In order to determine the reliability of our system of data abstraction, a retrospective chart review was repeated by a spine researcher using the same method of chart abstraction. The spine researcher was not blinded to study design and hypotheses. We then compared reliability between the two reviewers for the determination of spontaneous onset lumbar disk herniations, and lifting-associated lumbar disk herniations (heavy and light).
Outcomes measures
We prospectively recorded information on disability and pain intensity at the clinical presentation. Disability was measured by the Oswestry Disability Index (ODI). The ODI is a condition-specific measure of disability which has been used extensively in prior studies of low back pain and radiculopathy, and has demonstrated validity and reliability in these contexts[16]. Pain was measured by the visual analogue scale (VAS) for leg pain and the VAS for back pain[17].
Statistical Analysis
To characterize the study population, we calculated means and standard deviations for continuous variables, and frequencies and proportions for categorical variables. We determined the frequency of patient-identified inciting events in the categories of: ‘spontaneous onset’, ‘heavy lifting’, ‘light lifting’, ‘non-lifting physical activity’, ‘non-exertional occurrence’, and ‘physical trauma’.
To compare the baseline characteristics of the subgroups of patients with spontaneous LDH and an inciting event-associated LDH (not spontaneous), we used the chi-square test or Fisher’s exact test for dichotomous variables, and the Student’s T-test or Wilcoxon Signed-Rank test for continuous variables. For analytic purposes, race was dichotomized as ‘white’ vs. ‘non-white’ (Asian, Black, Hispanic, Native American or Alaskan Native, Pacific Islander, or Other). Due to small numbers in individual cells, the employment status categories of ‘unemployed’ and ‘student’ were combined as one category. We then examined associations between the presence of any patient-identified inciting event and the outcomes of ODI, VAS back pain, and VAS leg pain. For associations which demonstrated at least a trend towards statistical significance (p ≤ 0.20) in the univariate (between-subgroup) analyses, we created separate multivariate linear regression models including as covariates those baseline characteristics which 1) demonstrated a trend towards statistical difference between subgroups (p ≤ 0.20), or 2) were felt to have a possible conceptual basis for explaining the observed differences. Finally, we repeated this entire analytic process to compare the subgroups of patients with lifting-associated LDH and without lifting-associated LDH. All analyses were performed using SAS software, version 9.0 (SAS Institute., Cary, NC).
RESULTS
Baseline characteristics and outcome measures are presented in Table 1. 154 participants were recruited. Participants had a mean age ± standard deviation (SD) of 52.9 ± 13.4 years. The study population was 32% female and predominantly of white race (95.5%). Although the population demonstrated moderate disability (ODI=51 ± 21), 56% of participants were employed in either a full-time or part-time capacity, and only 8% had a worker’s compensation claim.
Table 1.
Characteristics of the Study Sample
| Baseline Characteristics (n=154) |
Mean (S.D.) or N (%) |
|---|---|
| Age (yrs.) | 52.9 (13.4) |
| Gender (% Female) | 49 (31.8%) |
| Race (% White) | 145(94.2%) |
| SACQ (0-45) | 2.8 (3.3) |
| Duration of symptoms (wks.) | 4.9 (3.0) |
| Prior low back pain history (%) | 116 (75.3%) |
| Current or past significant tobacco use (%) | 30 (19.9%) |
| Employment Status | |
| Current part-time employment (%) | 12 (7.9%) |
| Current full-time employment (%) | 73 (48.0%) |
| Unemployed± | 9 (5.9%) |
| Retired | 27 (17.8%) |
| Disabled | 31 (20.4%) |
| Worker’s compensation (%) | 10 (8.1%) |
| Oswestry Disability Index (0-100) | 51 (21) |
| Visual Analog Scale Leg Pain (0-10) | 7.0 (2.4) |
| Visual Analog Scale Back Pain (0-10) | 5.1 (3.3) |
includes ‘unemployed’ and ‘student’ status
SACQ – Self-administered Comorbidity Questionnaire
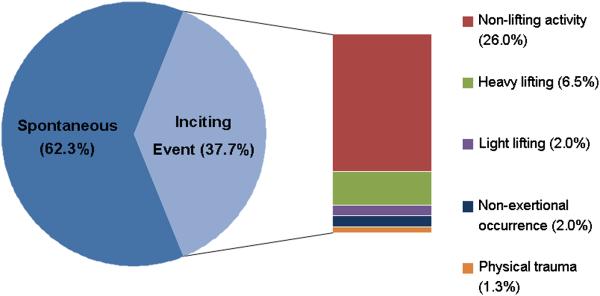
Figure 1 depicts the relative proportions of patient-identified inciting events associated with the onset of symptoms from acute LDH. 62% of LDH did not have a specific patient-identified event associated with onset of symptoms. Of the 38% of LDH where an inciting event was reported, non-lifting activities accounted for the largest proportion, comprising more than one-quarter (26%) of all LDH. Heavy lifting (6.5%), light lifting (2%), non-exertional occurrences (2%) and physical trauma (1.3%) accounted for relatively small proportions of all LDH.
Figure 1.
Patient-Identified Inciting Events
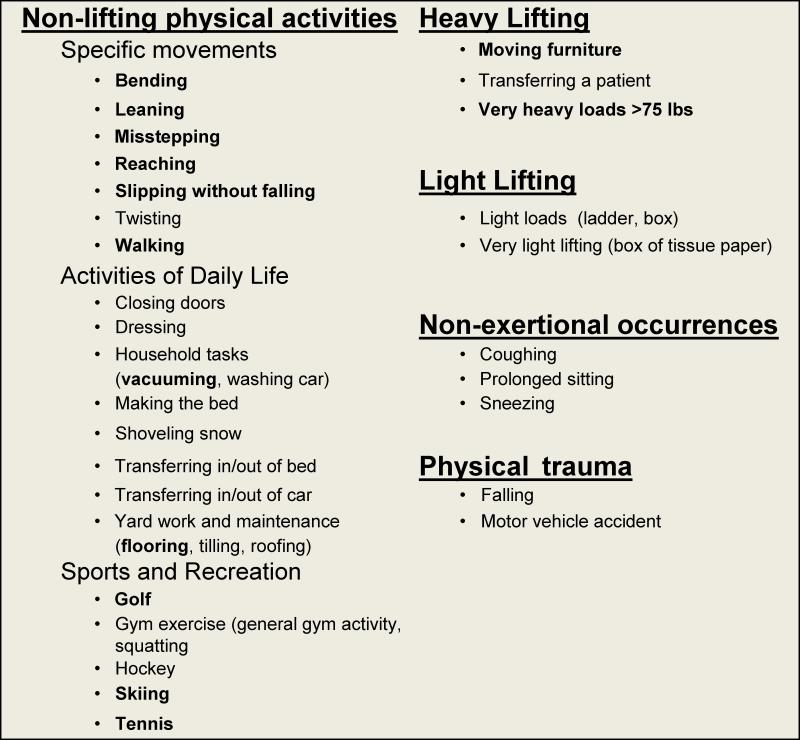
Figure 2 presents a table of all reported types of inciting events. Many activities or occurrences identified as inciting events were reported by more than one individual, and these are indicated in bold in Figure 2. The majority of patient-identified inciting events were either commonly performed movements or activities of daily living, which may in practical terms have been difficult for the patient to avoid, even if foreknowledge of impending herniation had been possible. A minority of inciting events involved strenuous activity or lifting, and are more representative of the possibly injurious activities commonly thought to be contributing factors to herniation. It was quite common for the association of inciting events to the onset of symptoms to be reported with uncertainty by the patient; for example, an event may have been reported as having a ‘possible’ connection to pain symptoms, or there may have been a large time lapse (> 1 week) between the event and the onset of symptoms. All occurrences reported by the patient were considered inciting events, regardless of the plausibility of the stated connection between the event and the onset of pain symptoms.
Figure 2.
Types of Specific Patient-Identified Inciting Events*
*Events identified by more than one patient are marked in bold
The baseline characteristics of the subgroups of patients with and without an inciting event are presented in Table 2. Patients with a spontaneous onset LDH were significantly older, less likely to have a history of tobacco use, and less likely to have a worker’s compensation claim (p ≤ 0.05). Employment status was significantly different in the group with spontaneous LDH (p=0.05). There was a trend towards a slightly shorter duration of symptoms in patients with spontaneous LDH (p ≤ 0.20). Table 3 demonstrates the results of univariate analyses of associations between the presence of an inciting event and the severity of the clinical presentation. Although there were no significant associations between the presence of an inciting event and ODI, leg pain, or back pain, there was a trend towards greater disability in the subgroup of patients with spontaneous LDH (p = 0.13). In multivariate linear regression analysis of the association between the presence of an inciting event and ODI, we included the covariates of age, gender, duration of symptoms, tobacco use history, employment status, and worker’s compensation claim status. When accounting for important adjustment variables, the association between spontaneous LDH and ODI was statistically significant, with an adjusted ODI of 49 in the inciting event-associated LDH group, as compared to an adjusted ODI of 57 in the spontaneous LDH group (p = 0.04).
Table 2.
Characteristics of Spontaneous vs. Inciting Event-Associated Lumbar Disk Herniation
| Baseline Characteristic | Spontaneous* (N=96) |
Inciting Events* (N=58) |
|
|---|---|---|---|
| Age (yrs.) | 55.1 (13.1) | 49.2 (13.2) | .008† |
| Female (%) | 28 (29.2%) | 21 (36.2%) | .36 |
| Race (% White) | 91 (94.8%) | 54 (93.1%) | .73 |
| SACQ (0-45) | 2.8 (3.4) | 2.9 (3.1) | .58 |
| Duration of symptoms (wks.) | 4.7 (3.2) | 5.2 (2.1) | .13 |
| Prior low back pain history (%) | 21 (21.9%) | 17 (29.3%) | .30 |
| Current or past significant tobacco use (%) | 13 (13.8%) | 17 (29.8%) | .02† |
| Employment Status | |||
| Current part-time employment (%) | 7 (7.4%) | 5 (8.8%) | |
| Current full-time employment (%) | 39 (41.1%) | 34 (60.0%) | |
| Unemployed± | 8 (8.4%) | 1(1.8%) | .05† |
| Retired | 22 (23.2%) | 5 (8.8%) | |
| Disabled | 19 (20.0%) | 12 (21.1%) | |
| Worker’s compensation (%) | 3 (4.0%) | 7 (14.6%) | .05† |
Mean (S.D.) or N (%)
statistically significant (p ≤ 0.05)
includes ‘unemployed’ and ‘student’ status
SACQ – Self-administered Comorbidity Questionnaire
Table 3.
Associations between a History of Patient-Identified Inciting Events and the Severity of the Clinical Presentation
| Outcome | Spontaneous LDH N=96 |
Inciting-Event Associated LDH N=57 |
|
|---|---|---|---|
| Oswestry Disability Index (0-100) | 53 ± 21 | 47 ± 21 | p=0.13 |
| Visual Analog Scale Leg Pain (0-10) | 7.1 ± 2.3 | 6.8± 2.5 | p=0.45 |
| Visual Analog Scale Back Pain (0-10) | 5.0 ± 3.2 | 5.3 ± 3.5 | p=0.61 |
The baseline characteristics of the subgroups of patients with and without a lifting-associated LDH are presented in Table 4. A history of tobacco use was significantly more common in the subgroup of patients with a lifting-associated LDH (p ≤ 0.05). There was a trend towards a lower percentage of female participants, and a higher percentage of patients with a worker’s compensation claim, in the subgroup of patients with a lifting-associated LDH (p ≤ 0.20). Employment status was significantly different in the group with a lifting-associated LDH (p ≤ 0.05)
Table 4.
Characteristics of Lifting- Associated vs. Non-Lifting Associated Lumbar Disk Herniation
| Baseline Characteristic | Non-Lifting- Associated* (N=141) |
Lifting- Associated* (N=13) |
|
|---|---|---|---|
| Age (yrs.) | 53.1 (13.6) | 50.9 (11.2) | .57 |
| Female (%) | 48 (34.0%) | 1 (7.7%) | .06 |
| Race (% White) | 133 (94.3%) | 12 (92.3%) | .56 |
| SACQ (0-45) | 2.7 (3.2) | 3.9 (4.4) | .39 |
| Duration of symptoms (wks.) | 4.9 (3.1) | 5.2 (2.9) | .57 |
| Prior low back pain history (%) | 106 (75.2%) | 10 (76.9%) | 1.00 |
| Current or past significant tobacco use (%) | 23 (16.7%) | 7 (53.9%) | .005† |
| Employment Status | |||
| Current part-time employment (%) | 8 (5.8%) | 4 (30.8%) | |
| Current full-time employment (%) | 70 (50.4%) | 3 (23.1%) | |
| Unemployed± | 8(5.8%) | 1 (7.7%) | 0.02† |
| Retired | 26 (18.7%) | 1 (7.7%) | |
| Disabled | 27 (19.4%) | 4 (30.8%) | |
| Worker’s compensation (%) | 7 (6.3%) | 3 (25.0%) | .06 |
Mean (S.D.) or N (%)
statistically significant (p ≤ 0.05)
includes ‘unemployed’ and ‘student’ status
SACQ – Self-administered Comorbidity Questionnaire
Table 5 demonstrates the results of simple univariate analyses of associations between the presence of a lifting-associated LDH and the severity of the clinical presentation. Although there were no significant associations (p ≤ 0.05) between the presence of a lifting-associated LDH and ODI, leg pain, or back pain, there was a trend towards greater disability and greater leg pain intensity in the subgroup of patients with a lifting-associated LDH (p ≤ 0.20). In multivariate linear regression analysis of the association between the presence of a lifting-associated LDH and ODI and leg pain, we included the covariates of age, gender, tobacco use history, employment status, and worker’s compensation claim status. When accounting for important adjustment variables, lifting-associated LDH was not significantly associated with disability, with an adjusted ODI of 51 in the lifting-associated LDH group, as compared to an adjusted ODI of 55 in the non-lifting-associated LDH group (p = 0.58). Similarly, when accounting for important adjustment variables, the trend towards greater leg pain in the subgroup of patients with a lifting-associated LDH was not seen, with an adjusted VAS of 7.6 in the lifting-associated LDH group, as compared to an adjusted VAS of 6.8 in the non-lifting-associated LDH group (p = 0.40).
Table 5.
Associations between a History of Lifting-Associated Inciting Events and the Severity of the Clinical Presentation
| Outcome | Non-Lifting- Associated LDH N=141 |
Lifting- Associated LDH N=13 |
|
|---|---|---|---|
| Oswestry Disability Index (0-100) | 50 ± 21 | 61 ± 17 | p=0.10 |
| Visual Analog Scale Leg Pain (0-10) | 6.9 ± 2.4 | 7.8± 2.3 | p=0.19 |
| Visual Analog Scale Back Pain (0-10) | 5.1 ± 3.3 | 5.6 ± 3.8 | p=0.54 |
Inter-rater reliability for the determination of spontaneous vs. non-spontaneous LDH was almost perfect (κ=0.81) using the classification of Landis and Koch[18]. There was substantial reliability for the determination of heavy lifting (κ=0.76), light lifting (κ=0.67), and any lifting (κ=0.72).
DISCUSSION
The primary finding of this study is that, although patient-identified inciting events were common in LDH, the majority of LDH occurred without specific inciting events. When inciting events were identified, non-lifting physical activities such as simple movements, activities of daily living, and sports activities were most common. A history of an inciting event was not significantly associated with a more severe clinical presentation in crude analyses. On the contrary, when adjusting for potential confounding, spontaneous LDH (without an inciting event) was significantly and independently associated with higher ODI scores at baseline (greater disability). However, the magnitude of this effect was small, and did not reach the threshold of 10 points on ODI commonly considered to be clinically important[19]. There was no significant association between the occurrence of a lifting-related event and increased severity of the clinical presentation. It should be noted that the finding of greater disability in the subgroup of patients who had a spontaneous LDH may be a consequence of the multiple statistical comparisons performed in our analysis. Further studies are warranted to investigate an association between spontaneous LDH and disability at clinical presentation.
Our findings suggest that a history of physical activities or other inciting events is not necessary to trigger the onset of symptoms secondary to LDH. These observations may be consistent with either a cumulative injury model or a genetic model of disk degeneration. From the perspective of the cumulative injury model, progressive injury may cause damage of disk structures to such an extent that even a small, transient increase in forces across the spine-insufficient to register as an inciting event by the patient- may lead to the final occurrence of herniation. From the competing perspective of the genetic model, a low frequency of inciting events is expected due to the fact that genetically encoded processes dependent on time and aging are the primary determinants of herniation. However, in the context of the onset of symptoms in acute LDH, neither model of degeneration strongly supports the notion that vigilant avoidance of activity may have staved off the final occurrence of herniation.
If a patient believes that a particular strenuous activity either triggered their disk herniation, or caused their injury to be more severe, they may be less inclined to comply with treatment recommendations when these involve increased activity[20]. This may be problematic for functional outcomes in light of the demonstrated improvements in disability and sick leave resulting from an early return to normal activities in patients with acute sciatica[21], and subacute LBP and/or lower extremity pain.[22, 23] In the absence of prior empirical data, the information that inciting events are not required for the onset of symptoms due to LDH, and that a history of inciting events appears to not be associated with greater symptom severity in LDH, may be useful in the counseling of patients experiencing lumbosacral radicular syndrome due to LDH. Indeed, prior work has shown that direct evidence-based education delivered by provider to patient can improve outcomes in spine care, including disability[24]. Nevertheless, firm conclusions on the role of inciting events in LDH ideally require confirmation by a prospective study, or replication in another sample.
It should be noted that the prevalence of spontaneous symptom onset in 62% of patients with radicular pain due to LDH in our study is strikingly similar to the results of the few prior studies of inciting events in low back pain. A prospective study of patients presenting to rehabilitation clinics found a spontaneous onset without identifiable cause in 67% of back pain episodes[25]. This work cited unpublished data by McKenzie, which noted a spontaneous onset without identifiable cause in 67% of back pain patients prior to the enactment of compensation legislation mandating the identification of a specific precipitating event[25]. Taken together, the existing literature on inciting events in spinal disorders therefore does not portray a strong link between the presence of specific inciting events and the onset of symptoms.
Our study has several limitations. First, the use of retrospective chart review may have contributed to inaccuracies in our determination of the presence and absence of inciting events. Although this may be the case, the documentation of the presence and absence of inciting events is a standard practice among our recruiting physicians, as a possible consequence of our previous experience with the importance of patient beliefs about activity in spine care[20]. The fact that our method of chart abstraction demonstrated near-perfect reliability for the analyzed dependent variables offers assurance of minimal random error. Second, our estimates of inciting event frequency may have been affected by recall bias. However, we believe that the tendency to underreport events due to lapses in memory was likely counterbalanced by the reporting of inciting events that were normal daily occurrences, only ‘possibly’ related to onset of pain according to the patient. Unfortunately, there exists no validated method of assessing the plausibility of patient-identified inciting events as the actual cause of symptom onset. Third, multiple statistical comparisons were made in our analysis. This limitation was unavoidable due to the absence of prior data on specific inciting events as the precipitant of acute LDH symptoms, and our resultant inability to target in advance those outcomes most likely to have associations with our independent variables. The practical consequence of this is that our use of a p-value cut-off of 0.05 overestimates the probability of an association occurring due to chance alone. Fourth, only 8% of individuals in our study reported worker’s compensation involvement. These findings may not be generalizable to individuals with worker’s compensation claims. Lastly, due to the cross-sectional nature of this study, firm conclusions about cause-and-effect relationships between the presence of an inciting event and either the occurrence of disk herniation, or the severity of the clinical presentation, cannot be made.
Despite these limitations, our study is the first to evaluate the presence or absence of inciting events in acute lumbar disk herniation. We found that the majority of LDH occurred without specific inciting events. A history of an inciting event was not significantly associated with a more severe clinical presentation in crude analyses. Rather, spontaneous LDH demonstrated an independent association with greater disability in multivariate analysis that was statistically significant, though likely not clinically meaningful. There was no significant association between the occurrence of a lifting-related event and the severity of the clinical presentation. Although these findings do not refute either the cumulative injury model or genetic model of disk degeneration, neither do they suggest that physical activity is associated with the occurrence or severity of disk herniation. This information may be helpful in the education of patients recovering from lumbar disk herniation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Rainville J, Pransky G, Gibson S, Suri P. The Physician as Disability Advisor for Back Pain Patients. In: Hasenbring MR,A, Turk D, editors. From Acute to Chronic Back Pain: Risk Factors, Mechanisms, and Clinical Implications. vol 1. Oxford University Press; Oxford: In Press. [Google Scholar]
- 2.Videman T, Gibbons LE, Kaprio J, Battie MC. Challenging the cumulative injury model: positive effects of greater body mass on disc degeneration. Spine J. 2009 doi: 10.1016/j.spinee.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Videman T, Levalahti E, Battie MC. The effects of anthropometrics, lifting strength, and physical activities in disc degeneration. Spine. 2007;32(13):1406–13. doi: 10.1097/BRS.0b013e31806011fa. [DOI] [PubMed] [Google Scholar]
- 4.Miranda H, Viikari-Juntura E, Martikainen R, Takala EP, Riihimaki H. Individual factors, occupational loading, and physical exercise as predictors of sciatic pain. Spine. 2002;27(10):1102–9. doi: 10.1097/00007632-200205150-00017. [DOI] [PubMed] [Google Scholar]
- 5.Seidler A, Bergmann A, Jaeger M, et al. Cumulative occupational lumbar load and lumbar disc disease - results of a German multi-center case-control study (EPILIFT) BMC Musculoskelet Disord. 2009;10(1):48. doi: 10.1186/1471-2474-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schenk P, Laubli T, Hodler J, Klipstein A. Magnetic resonance imaging of the lumbar spine: findings in female subjects from administrative and nursing professions. Spine. 2006;31(23):2701–6. doi: 10.1097/01.brs.0000244570.36954.17. [DOI] [PubMed] [Google Scholar]
- 7.Kelsey JL. An epidemiological study of the relationship between occupations and acute herniated lumbar intervertebral discs. Int J Epidemiol. 1975;4(3):197–205. doi: 10.1093/ije/4.3.197. [DOI] [PubMed] [Google Scholar]
- 8.Kelsey JL. An epidemiological study of acute herniated lumbar intervertebral discs. Rheumatol Rehabil. 1975;14(3):144–59. doi: 10.1093/rheumatology/14.3.144. [DOI] [PubMed] [Google Scholar]
- 9.Battie MC, Videman T, Gibbons LE, et al. Occupational driving and lumbar disc degeneration: a case-control study. Lancet. 2002;360(9343):1369–74. doi: 10.1016/S0140-6736(02)11399-7. [DOI] [PubMed] [Google Scholar]
- 10.Alaranta H, Hurme M, Karppi SL. Leisure time physical activities and the results of surgery of lumbar disc herniation. Scand J Rehabil Med. 1987;19(3):105–8. [PubMed] [Google Scholar]
- 11.Karvonen MJ, Viitasalo JT, Komi PV, Nummi J, Jarvinen T. Back and leg complaints in relation to muscle strength in young men. Scand J Rehabil Med. 1980;12(2):53–9. [PubMed] [Google Scholar]
- 12.Riihimaki H, Viikari-Juntura E, Moneta G, Kuha J, Videman T, Tola S. Incidence of sciatic pain among men in machine operating, dynamic physical work, and sedentary work. A three-year follow-up. Spine. 1994;19(2):138–42. doi: 10.1097/00007632-199401001-00003. [DOI] [PubMed] [Google Scholar]
- 13.Videman T, Battie MC, Gibbons LE, et al. Lifetime exercise and disk degeneration: an MRI study of monozygotic twins. Med Sci Sports Exerc. 1997;29(10):1350–6. doi: 10.1097/00005768-199710000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Videman TG,LE, Kapprio J, Battie MC. Challenging the Cumulative Injury Model-Positive Effects of Greater Body Mass on Disc Degeneration. 36th Annual Meeting of the International Society for the Study of the Lumbar Spine; Miami, FL. May 5, 2009; 2009. [Google Scholar]
- 15.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–52. doi: 10.1097/00007632-200011150-00017. discussion 2952. [DOI] [PubMed] [Google Scholar]
- 17.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72(1-2):95–7. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 18.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. [PubMed] [Google Scholar]
- 19.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 2008;33(1):90–4. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 20.Rainville J, Pransky G, Indahl A, Mayer EK. The physician as disability advisor for patients with musculoskeletal complaints. Spine. 2005;30(22):2579–84. doi: 10.1097/01.brs.0000186589.69382.1d. [DOI] [PubMed] [Google Scholar]
- 21.Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Lack of effectiveness of bed rest for sciatica. N Engl J Med. 1999;340(6):418–23. doi: 10.1056/NEJM199902113400602. [DOI] [PubMed] [Google Scholar]
- 22.Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain? Spine. 2000;25(15):1973–6. doi: 10.1097/00007632-200008010-00017. [DOI] [PubMed] [Google Scholar]
- 23.Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine. 1995;20(4):473–7. doi: 10.1097/00007632-199502001-00011. [DOI] [PubMed] [Google Scholar]
- 24.Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–30. doi: 10.1097/00002508-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Hall H, McIntosh G, Wilson L, Melles T. Spontaneous onset of back pain. Clin J Pain. 1998;14(2):129–33. doi: 10.1097/00002508-199806000-00007. [DOI] [PubMed] [Google Scholar]