Abstract
Per capita Medicare spending is more than twice as high in New York City and Miami than in places like Salem, Oregon. How much of these differences can be explained by Medicare's paying more to compensate for the higher cost of goods and services in such areas? To answer this question, we analyzed Medicare spending after adjusting for local price differences in 306 Hospital Referral Regions. The price-adjustment analysis resulted in less variation in what Medicare pays regionally, but not much. The findings suggest that utilization—not local price differences—drives Medicare regional payment variations, along with special payments for medical education and care for the poor.
Average per capita Medicare spending varies almost threefold across regions in the United States. Part of the differences could derive from the fact that Medicare pays health care providers in rural areas at lower rates than in large cities because the cost of living in Des Moines, for example, is lower than in New York City. In addition, other Medicare payment mechanisms boost payments for specific regions and hospitals, such as direct and indirect supplements for graduate medical education programs or federal payments for disproportionate numbers of low-income patients.
The Dartmouth Atlas of Health Care has demonstrated large regional variations in Medicare spending.1 We extend those findings by deconstructing Medicare spending into variations owing to prices and those owing to utilization rates. By inpatient utilization, we mean average diagnosis-related group (DRG) weights (a Medicare payment classification system) as set by the Centers for Medicare and Medicaid Services (CMS) to represent the amount of effort necessary for specific procedures or hospitalizations. By physician utilization we mean the sum of relative value units (RVUs), Medicare's geographically adjusted payment schedule for physicians.
Along with other measures of utilization, we approximated quantities of health care services that are aggregated using a common set of national prices. Note that we did not directly measure inputs such as doctor visits and hospital days—a distinction to which we return below.
Our approach builds on previous analyses by the Dartmouth Institute for Health Policy and Clinical Practice and the pioneering work of the Medicare Payment Advisory Commission (MedPAC),2–4 which also examined differences in spending and utilization across states. Our approach differs in that we focused on Hospital Referral Regions (306 distinct hospital service areas in the United States) and provided a simpler analytic approach designed for use with multiyear measures of health spending.
Using Medicare claims from 2006, we present per capita non-price-adjusted (actual) expenditures and price-adjusted expenditures aggregated by Hospital Referral Region. (By price-adjusted expenditures we mean what expenditures would be if Medicare reimbursed all services at exactly the same national prices whether the patient were treated in Enid, Oklahoma, or San Francisco, California.) Both actual and price-adjusted expenditures were further adjusted for regional differences in age, sex, and race. Each component of Medicare payment, such as inpatient and outpatient services, is reimbursed using somewhat different price adjustments. As a result, we adjusted each component separately, and then we aggregated them to create a final measure of price-adjusted Medicare expenditures.
There has been considerable debate about the importance of Medicare spending variations across U.S. regions, particularly for high-expenditure areas such as McAllen, Texas, the subject of a widely read health policy narrative published in the New Yorker in 2009.5 Some analysts have suggested that spending differences are driven by factors such as higher prices, rates of illness, or poverty, rather than systemwide differences in how patients are treated. For example, a recent MedPAC study found weaker regional variations after adjusting for price and illness across regions.6
Although we have considered the potential importance of illness and poverty elsewhere,7 in this paper we focus solely on whether adjustments for prices “explain” regional variations in health care spending, particularly in areas with high Medicare spending such as New York, Miami, and Los Angeles. The specifics of price adjustment for each category are available in a technical report.8
Study Data and Methods
Unit of Measurement
The geographic measurement unit for this analysis is the Hospital Referral Region. This unit was created to define discrete geographical regions of health care, as described by John Wennberg and Megan McAndrew Cooper.9 These standardized geographic units make it possible to analyze price-adjusted Medicare spending data over time.
Past studies of spending at the regional level have relied on the 5 percent Continuous Medicare History Sample created by the CMS. However, this data set does not provide sufficient clinical detail for price adjustment. Therefore, we used the 20 percent random sample of all Medicare files.
Measuring Use and Spending
For measuring hospital inpatient utilization, we used DRG-based quantity measures that are designed to reflect “true” medical inputs. (DRG prices are set to reflect the average of patients' hospital-borne costs within a large sample of hospitals.) We included outlier payments, which constitute 3.7 percent of total payments to short-stay hospitals, in our measure of utilization because they represent real resources spent for patients with unusually high health care costs.
For payments to physicians under the Medicare Part B (physician services) program, we relied primarily on relative value units, which Medicare uses as a measure of the amount of time spent on an office visit, for example. In practice, Medicare reimburses physicians in New York more for an office visit than for an identical office visit in Wisconsin by paying more per relative value unit. Our method “undoes” this differential by recreating Part B spending using the same dollar payment per relative value unit whether the doctor is in Wisconsin or New York. Thus, if Part B spending is higher in New York, it's because more services are provided, and not because prices are higher.
Other Medicare spending categories were calculated to measure, indirectly, the actual service provided to the patient. These adjustments relied in turn on the CMS regional wage index as the primary mechanism to adjust Medicare expenditures. The wage index is particularly useful when the price-adjustment mechanism used by Medicare to reimburse providers is too complex to unravel or requires additional data sets (such as nursing home risk-adjustment assessments). This index is the primary means to adjust expenditures for the variety of Medicare spending components exclusive of Part A inpatient and Part B physician payments.
For Medicare outpatient payments, only 60 percent of the base payment is eligible for adjustment by the local wage index. Medicare assumes that 60 percent of expenses represent local purchases (and hence local prices) for employees, rents, and other input costs. The remaining 40 percent of Medicare outpatient payments are assumed to not require local price adjustment because they are bought on a national market.10
A similar logic was used for other categories of Medicare expenditures, although we assumed a 75/25 mix—a rough average among the different categories of expenditures such as nursing homes—rather than the 60/40 mix described above.11–13 The adjustment factors for these smaller components of overall Medicare spending may be imperfect. But these imperfections have little impact on our overall estimates of Medicare spending because they are small relative to inpatient and physician charges that rely on DRGs and RVUs, respectively.
Analyses
We constrained (or “normalized”) the sum of U.S. price-adjusted expenditures to be equal to the sum of actual expenditures. This additional proportional adjustment ensures that the national average of per capita price-adjusted spending is equal to the national average of actual per capita Medicare spending.14 Similar to the methods employed for analyzing Medicare spending data in the Dartmouth Atlas,1 price-adjusted Medicare spending was also adjusted for age, sex, and race.
The comparison data were the age-sex-race adjusted Medicare expenditures. The results are presented on a per capita basis, where the population includes all Medicare Part A and B beneficiaries age sixty-five and older who are not enrolled in a health maintenance organization (HMO).
Study Results
Measures of Spending
We combined all Medicare spending components to create an aggregated measure, adjusted for price, age, sex, and race, of expenditures for each Hospital Referral Region (detailed data are presented in an Online Appendix).15 Exhibit 1 lists the ten Hospital Referral Regions with the highest per capita spending; the ten regions with the lowest spending; and the five highest and lowest proportional differences between actual (age-sex-race adjusted) spending and price-adjusted spending in 2006.
EXHIBIT 1. Per Capita Medicare Spending By Hospital Referral Region (HRR), Adjusted And Not Adjusted For Price, 2006.
source Data are from the authors' analyses of 2006 Medicare data and represent annual per capita expenditures and price-adjusted expenditures, reflecting regional differences in age, sex, and race. note For details on the adjustment methods, see text.
| HRR number | HRR name | Per capita spending | Price-adjusted per capita spending | Percentage difference |
|---|---|---|---|---|
| 10 HRRs with highest price-adjusted per capita Medicare spending | ||||
| 127 | FL—Miami | $15,909 | $14,966 | 6% |
| 402 | TX—McAllen | 13,633 | 13,881 | −2 |
| 297 | NY—Bronx | 12,004 | 8,653 | 39 |
| 303 | NY—Manhattan | 11,744 | 8,861 | 33 |
| 396 | TX—Harlingen | 11,489 | 11,324 | 1 |
| 56 | CA—Los Angeles | 10,674 | 9,325 | 14 |
| 301 | NY—East Long Island | 10,608 | 8,740 | 21 |
| 233 | MI—Dearborn | 10,460 | 9,791 | 7 |
| 217 | LA—Monroe | 10,226 | 11,385 | −10 |
| 234 | MI—Detroit | 9,954 | 9,541 | 4 |
| 10 HRRs with lowest price-adjusted per capita spending | ||||
| 324 | ND—Minot | 6,033 | 6,711 | −10 |
| 428 | VA—Lynchburg | 6,022 | 6,524 | −8 |
| 105 | CO—Grand Junction | 5,983 | 6,075 | −2 |
| 342 | OR—Eugene | 5,968 | 5,798 | 3 |
| 194 | IA—Iowa City | 5,902 | 6,254 | −6 |
| 370 | SD—Rapid City | 5,854 | 6,176 | −5 |
| 345 | OR—Salem | 5,810 | 5,642 | 3 |
| 193 | IA—Dubuque | 5,799 | 6,219 | −7 |
| 448 | WI—La Crosse | 5,715 | 5,757 | −1 |
| 150 | HI—Honolulu | 5,293 | 5,212 | 2 |
| 5 HRRs with highest percentage difference between price-adjusted and non-price-unadjusted spending | ||||
| 297 | NY—Bronx | 12,004 | 8,653 | 39 |
| 303 | NY—Manhattan | 11,744 | 8,861 | 33 |
| 65 | CA—Alameda County | 9,251 | 7,094 | 30 |
| 81 | CA—San Francisco | 8,140 | 6,278 | 30 |
| 85 | CA—San Mateo County | 7,878 | 6,104 | 29 |
| 5 HRRs with lowest percentage difference between price-adjusted and non-price-unadjusted spending | ||||
| 208 | KY—Paducah | 7,626 | 8,680 | −12 |
| 260 | MS—Meridian | 8,208 | 9,371 | −12 |
| 321 | ND—Bismarck | 6,152 | 7,053 | −13 |
| 2 | AL—Dothan | 7,543 | 8,703 | −13 |
| 6 | AL—Mobile | 7,759 | 8,990 | −14 |
Note that the benchmark estimates of non-price-adjusted expenditures differ somewhat from those on the Dartmouth Atlas Web site.1 As we noted above, the numbers we present were calculated directly from all available individual 20 percent Parts A and B Medicare claims files, instead of the 5 percent Medicare Continuous Medicare History Sample created by the CMS. These discrepancies are a topic for future research.
Regions Displaying Most Variation
As the first two panels of Exhibit 1 demonstrate, price adjustment does not erase the phenomenon of regional spending variation. Miami remains the highest-spending U.S. region, followed by McAllen, Texas. The nearly threefold gap between Miami and Salem, Oregon (unadjusted differences, $15,909 versus $5,810), is largely unaffected by price adjustment ($14,966 versus $5,642).
Other regions dropped in the rankings as a result of price adjustments. For example, San Francisco, with price-adjusted spending of $6,278, dropped in its ranking from 109th (unadjusted) to 291st (price-adjusted) of 306 regions in terms of overall expenditures.
The correlation coefficient is 0.84 (p < 0:01) between the price-adjusted and non-price-adjusted expenditure measure, while the standard deviation of expenditures across regions is $1,125 for price-adjusted and $1,376 for non-price-adjusted expenditures, when weighted by the fee-for-service population. (Weighting by population gives more importance to big regions than smaller ones.) When unweighted, the standard deviation is $1,200 for price-adjusted and $1,264 for non-price-adjusted expenditures. That is, adjusting for prices reduces the extent of regional variation, but not by much.
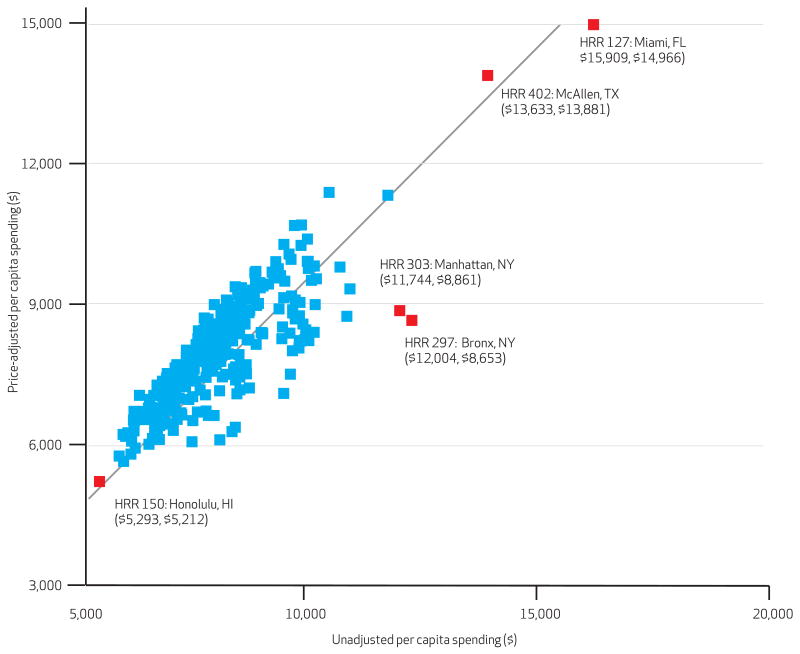
Exhibit 2 shows a graphical representation of these patterns, with age-sex-race adjusted expenditures on the horizontal axis and expenditures including price adjustment on the vertical axis. This exhibit, along with the third and fourth panels of Exhibit 1, demonstrates that price adjustment matters a great deal in some but not all areas (in Exhibit 2, the points farthest from the diagonal are those most affected). Per capita actual expenditures in southern Hospital Referral Regions tend to be somewhat less than the price-adjusted expenditures. For example, per capita actual Medicare expenditures in Mobile, Alabama, were $7,759, while per capita price-adjusted expenditures were $8,990. In other words, unadjusted Medicare spending in Mobile appeared to be so low largely because of modest cost of living in the region, but in fact price-adjusted expenditures were above average.
EXHIBIT 2. Total Per Capita Medicare Reimbursements At The Hospital Referral Region (HRR) Level, Adjusted And Not Adjusted For Price, 2006.
source Data are from the authors' analyses of 2006 Medicare data and represent annual per capita expenditures and price-adjusted expenditures, reflecting regional differences in age, sex, and race. note For details on the adjustment methods, see text.
Conversely, the New York and Northern California regions experienced the largest downward price adjustment. Bronx, New York (per capita spending, $12,004), accounted for many more Medicare dollars per capita than Montgomery, Alabama ($7,902). But after adjusting for differences in what Medicare pays per procedure or office visit, the two regions were nearly identical ($8,653 versus $8,761).
Much of the reason why the New York metropolitan area is so costly is not because of the wage index per se (what we usually think of as “cost-of-living” adjustments), but because the CMS pays hospitals in the New York area so much to reimburse them for graduate medical education and caring for disproportionate shares of low-income patients.
For example, in the Bronx, unadjusted hospital expenditures were $7,513 (see Exhibit 3); after price adjustment, per capita expenditures dropped to just $4,814. In other words, Bronx hospitals receive a 56 percent upward adjustment above the national average per DRG. Manhattan hospitals receive an upward adjustment of 49 percent. These adjustments are far greater than what would result from simple adjustments for cost of living.
EXHIBIT 3. Hospital Referral Regions (HRRs) With The Highest And Lowest Percentage Differences Between Adjusted And Non-Adjusted Per Capita Medicare Part A Spending, 2006.
source Data are from the authors' analyses of 2006 Medicare data and represent annual per capita expenditures and price-adjusted expenditures, reflecting regional differences in age, sex, and race. note For details on the adjustment methods, see text.
| HRR number | HRR name | Per capita spending | Price-adjusted per capita spending | Percentage difference |
|---|---|---|---|---|
| 5 HRRs with highest percentage difference between price-adjusted and non-price-adjusted Part A spending | ||||
| 297 | NY—Bronx | $7,513 | $4,814 | 56% |
| 303 | NY—Manhattan | 6,589 | 4,424 | 49 |
| 65 | CA—Alameda County | 5,362 | 3,906 | 37 |
| 81 | CA—San Francisco | 4,373 | 3,187 | 37 |
| 82 | CA—San Jose | 4,382 | 3,254 | 35 |
| 5 HRRs with lowest percentage difference between price-adjusted and non-price-adjusted Part A spending | ||||
| 146 | GA—Columbus | 2,832 | 3,342 | −15 |
| 214 | LA—Lake Charles | 4,214 | 4,979 | −15 |
| 321 | ND—Bismarck | 3,032 | 3,620 | −16 |
| 2 | AL—Dothan | 3,453 | 4,224 | −18 |
| 6 | AL—Mobile | 3,448 | 4,257 | −19 |
Discussion
We have presented a price-adjustment method designed to adjust the dollar amounts that the CMS pays for price differences across regions. We have also removed the additional payments that Medicare provides for graduate medical programs, disproportionate-share programs, and other items. Reversing these adjustments provides us with a greater ability to compare utilization differences across regions.
Price Adjustments and Variation
Our results suggest that although price adjustments do tend to decrease the overall variance in geographical spending patterns, they cannot account for more than a small fraction of the variation we observe in the national data. Furthermore, not all high-cost regions are high-cost for the same reasons. Bronx and Manhattan are high-spending areas primarily because they get paid more per hospitalization than do hospitals anywhere else in the country.
Physician payments constitute the second-largest component of Medicare expenditures after hospital expenditures. For example, the twentieth percentile of price-adjusted per capita Part B expenditures is $1,797, and the eightieth percentile is $2,461. Despite variation in Medicare payment amounts, there is still plenty of difference in physician utilization between regions.
Meanwhile, Miami was the Hospital Referral Region with the highest per capita utilization in the country in 2006, whether price-adjusted or not (Exhibit 1). Miami may be something of a special case, however. Its price-adjusted average per capita hospitalization expenditure of $4,800 was high, but not higher than several other regions. Where Miami stands out is in its spending for outpatient, device, and home health care (complete data are available in the Online Appendix).15 Some part of this may be the consequence of fraud, rather than actual utilization.16,17
Policy efforts to reduce the extent of regional variations in Medicare spending have been criticized, in part because of a concern that Medicare spending in cities with high cost of living would be unduly harmed by reforms. The price-adjusted measure therefore provides a more reliable basis for comparing the use of health care services not biased by CMS price-adjustment mechanisms, many of which are quite complex. For example, observed associations between Medicare (or overall) spending and quality at the regional level could be affected by adjustments for prices. Much less, however, is known about the distribution of prices paid for services in private insurance markets.
Other Price Indices
As we noted earlier, our results follow the efforts by MedPAC to create a comprehensive price index. Recently, MedPAC issued a report showing that although regional variations existed even after price and illness were adjusted for, the variations were considerably smaller than what had been previously found.6 The differences between our study and MedPAC's are unlikely to be the result of price-adjustment methodologies.18 Although we make it easier to apply our methods to multiple years and focus on Hospital Referral Regions rather than states or Metropolitan Statistical Areas, neither is likely to lead to different conclusions.
The most important explanation is that MedPAC also adjusted for illness using Hierarchical Condition Category measures. Illness adjustment is beyond the scope of this paper, but it is considerably more complex than price adjustment. The difficulty with illness adjustments arise because regions where health care is practiced more intensively tend to diagnose and label more disease, a factor that could bias results.19,20
Study Limitations
One limitation of the study is that it is impossible to exactly reverse all of the complex methods used by the CMS, which means that our adjustments are approximate. Nonetheless, particularly for the “big-ticket” items such as inpatient short-stay hospital care and physician reimbursements, we are confident that these approximations of adjusted expenditures provide a good summary of real differences in per capita health care use by DRGs and RVUs.
But there are also limitations in using DRGs and RVUs to measure hospital intensity. Recall that New York City hospitals might appear to be relatively parsimonious in terms of these two measures, at least compared to Los Angeles or Miami. However, direct measures of utilization suggest a different story.
Measuring hospital days per decedent in the last two years of life for chronically ill patients implies that the Manhattan Hospital Referral Region is 78 percent above the national average—far exceeding the rates in Los Angeles (43 percent above average) and Miami (48 percent). The Hospital Referral Region–level measures of end-of-life utilization are based on the decedent's ZIP code of residence and thus include everyone in the Medicare sample with a chronic illness as determine by Iezzoni risk adjustment, including those without a hospital admission.21
The price-adjustment methods and results presented can be extended to other measures of utilization; for example, the methods can be equally applied to Medicare expenditures that include the total amount paid to providers, and not simply the amount the CMS pays.
Concluding Comments
This study has demonstrated that there are substantial variations in price-adjusted Medicare spending across regions. But it has also demonstrated that there are also substantial variations in what Medicare pays for the same medical services across regions —particularly for Part A hospital services. We believe that greater transparency in documenting regional differences in utilization, and regional differences in what the CMS pays providers, can help improve the efficiency and equity of the Medicare program.
Contributor Information
Daniel J. Gottlieb, is a research associate at the Dartmouth Institute for Health Policy and Clinical Practice in Lebanon, New Hampshire. (dan.gottlieb@tdi.dartmouth.edu)
Weiping Zhou, is a research associate at the Dartmouth Institute.
Yunjie Song, is a statistical research analyst at the Dartmouth Institute.
Kathryn Gilman Andrews, is a Post-Bachelor Fellow at the Institute for Health Metrics and Evaluation in Seattle, Washington.
Jonathan S. Skinner, is a professor at the Department of Economics, Dartmouth College, in Hanover, New Hampshire
Jason M. Sutherland, is an assistant professor at the School of Population and Public Health, University of British Columbia, in Vancouver
Notes
- 1.Dartmouth Institute for Health Policy and Clinical Practice. Hanover (NH): Dartmouth Institute; Dartmouth atlas of health care [Internet] [cited 2010 Jan 18]. Available from: http://www.dartmouthatlas.org. [Google Scholar]
- 2.Internal documents from the Medicare Payment Advisory Commission (MedPAC).
- 3.Washington (DC): MedPAC; 2003. Jun, For a published discussion of MedPAC methods and results, see Medicare Payment Advisory Commission. Report to the Congress: variation and innovation in Medicare [Internet] [cited 2010 Jan 18]. Available from: http://www.medpac.gov/publications/congressional_reports/June03_Titlepg_Insidecov_Acknow.pdf. [Google Scholar]
- 4.Hackbarth GM. Washington (DC): MedPAC; 2002. Jul 23, Adjusting Medicare payments for local market input prices. Testimony before the Subcommittee on Health of the House Ways and Means Committee, 23 July2002 [Internet] [cited 2010 Jan 18]. Available from: http://www.medpac.gov/publications/congressional_testimony/072302(WM)local_input_prices.pdf. [Google Scholar]
- 5.Gawande A. The cost conundrum: what a Texas town can teach us about health care. New Yorker. 2009 Jun 1; [Google Scholar]
- 6.Medicare Payment Advisory Commission. Washington (DC): MedPAC; 2009. Dec, Measuring regional variation in service use [Internet] [cited 2010 Jan 18]. Available from: http://medpac.gov/documents/Dec09_RegionalVariation_report.pdf. [Google Scholar]
- 7.Sutherland JM, Fisher ES, Skinner JS. Getting past denial—the high cost of health care in the United States. N Engl J Med. 2009;361:1227. doi: 10.1056/NEJMp0907172. [DOI] [PubMed] [Google Scholar]
- 8.Gottlieb D, Zhou W, Song Y, Andrews K, Skinner J, Sutherland JM. A standardized method for adjusting Medicare expenditures for regional differences in prices. Hanover (NH): Dartmouth College; 2009. [Google Scholar]
- 9.Wennberg J, Cooper M, editors. Dartmouth atlas of health care. Chicago (IL): American Hospital Association; 1996. [Google Scholar]
- 10.Medicare Payment Advisory Commission. Washington (DC): MedPAC; 2008. Oct, Outpatient hospital services payment system [Internet] [cited 2010 Jan 18]. Available from: http://www.medpac.gov/documents/MedPAC_Payment_Basics_07_OPD.pdf. [Google Scholar]
- 11.Washington (DC): MedPAC; 2008. For example, psychiatric hospital adjustments were 76 percent and home health care, 77 percent, while inpatient hospital weights were just under 70 percent. See Medicare Payment Advisory Commission. Psychiatric hospital services payment system[Internet] [cited 2010 Jan 18]. Available from: http://www.medpac.gov/documents/MedPAC_Payment_Basics_08_psych.pdf. [Google Scholar]
- 12.Medicare Payment Advisory Commission. Washington (DC): MedPAC; 2008. Oct, Home health care services payment system[Internet] [cited 2010 Jan 18]. Available from: http://www.medpac.gov/documents/MedPAC_Payment_Basics_08_HHA.pdf. [Google Scholar]
- 13.Medicare Payment Advisory Commission. Washington (DC): MedPAC; 2008. Oct, Hospital acute inpatient services payment system [Internet] [cited 2010 Jan 18]. Available from: http://www.medpac.gov/documents/MedPAC_Payment_Basics_08_hospital.pdf. [Google Scholar]
- 14.This adjustment factor was calculated for the entire Medicare program, including the population under age sixty-five.
- 15.The Online Appendix is available by clicking the Online Appendix link in the box to the right of the article online.
- 16.A recent Sixty Minutes television report focused on fraud in South Florida. Medicare fraud: a $60 billion crime [Internet] Sixty Minutes (CBS) 2009 Oct 25; [cited 2010 Jan 18]. Available from: http://www.cbsnews.com/stories/2009/10/23/60minutes/main5414390.shtml.
- 17.Morris L. Combating fraud in health care: an essential component of any cost containment strategy. Health Aff (Millwood) 2009;28(5):1351–6. doi: 10.1377/hlthaff.28.5.1351. [DOI] [PubMed] [Google Scholar]
- 18.We are grateful to Jeff Stensland and Mark Miller of MedPAC for helpful discussions of their price adjustment methods.
- 19.Gilden D. McAllen: a tale of three counties. The Health Care Blog [blog on the Internet] 2009 Jun 25; [cited 2010 Jan 18]. Available from: http://www.thehealthcareblog.com/the_health_care_blog/2009/06/mcallen-is-now-a-tale-of-three-counties.html Gilden's risk adjusters—based like the Hierarchical Condition Codes index on Medicare claims data—suggested that McAllen, Texas, was much sicker than El Paso.
- 20.Gawande A. Atul Gawande: the cost conundrum redux. News Desk [blog on the Internet] 2009 Jun 23; [cited 2010 Jan 18]. Available from: http://www.newyorker.com/online/blogs/newsdesk/2009/06/atul-gawande-the-cost-conundrum-redux.html Gawande did not find evidence that McAllen, Texas, differed from El Paso, Texas, with regard to objective health measures of the population.
- 21.Wennberg JE, et al. Lebanon (NH): Dartmouth Institute; 2008. Tracking the care of patients with severe chronic illness; the Dartmouth atlas of health care 2008 [Internet] [cited 2010 Jan 18]. Available from: http://dartmouthatlas.org/atlases/2008_Chronic_Care_Atlas.pdf. [PubMed] [Google Scholar]