Abstract
Background
Groin pain after total hip arthroplasty (THA) or total hip resurfacing arthroplasty can be troubling for patients and surgeons. Potential sources of pain include infection, loosening, metal hypersensitivity, or impingement of bony structures or the iliopsoas tendon.
Questions/purposes
We compared the rate of groin pain after THA or hip resurfacing using metal-on-metal to those of other bearing surfaces.
Methods
We identified 347 (334 patients) primary total hip (n = 301) or resurfacing (n = 46) arthroplasties. Complete preoperative, operative, and postoperative data were available for 282 hips. We retrospectively reviewed the charts for the presence or absence of groin pain at a minimum of 1 year after surgery with a specific focus on etiologic factors. The minimum followup was 12 months (mean, 14 months; range 12 to 24 months).
Results
The rate of groin pain was 7% (15 of 217 patients) after THA with conventional bearing surfaces, 15% (4 of 26 patients) with metal-on-metal THA and 18% (7 of 39 patients) with total hip resurfacing. Younger patients were more likely to report groin pain postoperatively and more likely to have metal-on-metal bearing surfaces.
Conclusions
Our data at short-term followup suggest increased rates of groin pain after metal-on-metal THA or resurfacing arthroplasty versus THA using polyethylene or ceramic bearing surfaces. The reasons are not clear but they appear to be associated with younger age. Potential factors include impingement, activity level and possibly higher expectations for patients receiving metal-on-metal bearing surfaces that may make those patients more likely to report postoperative pain.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Metal-on-metal bearing surfaces used in both THA and total hip resurfacing have increased in popularity in recent years in an effort to eliminate polyethylene wear-induced osteolysis. A large metal-on-metal bearing surface has improved wear rates as compared with smaller head sizes and has the added advantage of decreased risk of dislocation [3, 10, 16, 19, 22]. However, hip resurfacings appear to be associated with a higher risk of groin pain. One recent study indicated 18% of patients reported continued groin pain after hip resurfacing [17], a higher rate than previously reported (0.37–4.3%) after conventional THA [1, 20]. In practice we noted patients with metal-on-metal bearing surfaces had a higher incidence of groin pain than patients undergoing standard THA, but the reasons for the increased rate of groin pain were unclear.
Groin pain after THA can be troubling for patients and surgeons. Potential sources of pain include infection and loosening, and these can occur independently of the type of arthroplasty or bearing surface. The mechanisms of pain after metal-on-metal total hip resurfacing are presumably similar to those of THA, although there are several unique to the procedure. These include impingement of the anterior native femoral neck against the metal socket or soft tissues and occult femoral neck fracture and these must be considered when evaluating these patients [15, 18]. Other potential causes of groin pain are related to the metal-on-metal bearing surface itself and include hypersensitivity to metal components leading to pain and joint effusion [6, 14, 21, 27]. Impingement of the iliopsoas tendon can occur with standard THA but has also been recently reported as occurring with total hip resurfacing or metal-on-metal hip arthroplasty [1, 5, 8, 11, 12, 20, 23, 25, 26].
We therefore: (1) determined whether the rate of groin pain after total hip resurfacing and metal-on-metal THA is greater than conventional THA; and (2) described possible factors leading to the increased risk of groin pain.
Patients and Methods
We used a computerized database to identify all patients undergoing total joint arthroplasty and identified 334 patients (347 hips) having primary THAs or total hip resurfacings between December 1, 2006, and November 31, 2007 at our institution. Of these, 61 were excluded as a result of clinical followup of less than 1 year and three patients had died before their 1-year followup visit. One patient was excluded as a result of severe radiation-induced necrosis of the acetabulum before his index arthroplasty. This left 269 patients (282 hips or 81%) who had complete preoperative, postoperative, and intraoperative records and pre- and postoperative radiographs. Patients were grouped by their bearing surface into two categories: 58 patients with 65 metal-on-metal arthroplasties and 211 patients with 217 conventional arthroplasties (including both polyethylene and ceramic acetabular liners). Preoperative diagnoses included osteoarthritis (198 of 282 [70%]), developmental dysplasia (39 of 282 [14%]), and other diagnoses (45 of 282 [16%]). The gender ratio was 150 female (53%) and 132 male (47%). Among the 65 hips with metal-on-metal arthroplasties the preoperative diagnoses were primary osteoarthritis in 45 hips, developmental dysplasia of the hip in nine, posttraumatic arthritis in six, osteonecrosis in two, synovial chondromatosis in two, and deformity after slipped capital femoral epiphysis in one hip. We obtained Institutional Review Board approval prior to the study.
All surgery was performed by two experienced surgeons (RTT, RJS). Thirty-nine of the 65 hips with metal-on-metal implants had resurfacing and 26 had THA. The implants used for THA were 19 ASR and seven Pinnacle acetabular shells, 25 Summit femoral stems, and one AML femoral stem (DePuy, Warsaw, IN). Implants used for total hip resurfacing were 33 Conserve Plus (Wright Medical, Arlington, TN) and six ASR (DePuy). All implants were uncemented except for the resurfacing heads, which were all cemented. No bone graft was used. The mean age of patients was 49 years (range, 22–65 years). The surgical approach was posterior in 64 hips and transtrochanteric in one hip.
Two hundred eleven patients (217 hips) underwent THA using metal-on-polyethylene or ceramic-on-ceramic bearing surfaces. Of these, 12 had ceramic liners and 205 received highly crosslinked polyethylene. All acetabular components were uncemented. The acetabular implants used were 204 Pinnacle acetabular shells, eight Duraloc option (DePuy), four Trident (Howmedica, Mahway, NJ), and one Trabecular Metal (Zimmer, Warsaw, IN). Sixty-one femoral components were cemented and the remainder uncemented. Femoral components included 143 Summit stems, five AML, three Bantam, and one S-ROM (DePuy); 47 Exeter cemented stems, 13 Omnifit EON cemented stems, and four Secur-fit (Stryker, Mahway, NJ); and one CDH stem (Zimmer). Autologous bone graft was used in eight acetabuli and four femurs. The mean age of patients was 61 years (range, 13-94 years). The surgical approach was posterior in 211 and anterolateral in six hips. Preoperative diagnoses were primary osteoarthritis in 153 hips, developmental dysplasia of the hip in 30, osteonecrosis in 19, posttraumatic arthritis in nine, residual arthritis from slipped capital femoral epiphysis in two hips, and one patient each with diagnoses of hemophilic arthropathy, post-Perthes arthritis, postseptic arthritis, and rheumatoid arthritis.
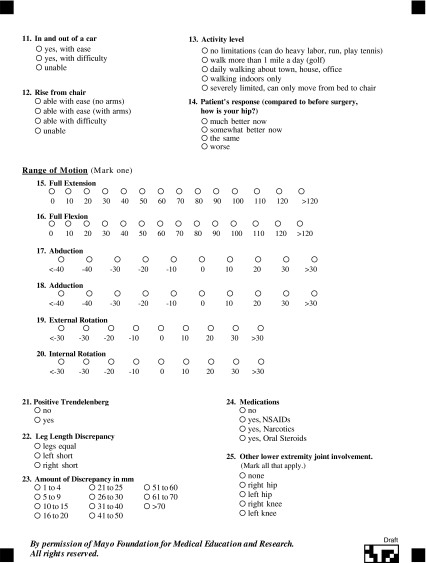
Patients were asked to return for an examination, interview, and radiographic evaluation at regular followup intervals (2, 12 and 24 months postoperatively). Clinical assessment of all patients who underwent hip arthroplasty was performed by the surgeon using a standardized hip analysis sheet (Appendix 1) during these visits. All patients were asked if they had any hip pain and, if so, the grade (slight, moderate, severe) and location (trochanter, groin, buttock, or thigh) of pain were noted. Gait, leg length, and ROM were assessed as were provocative tests for pain, including resisted straight leg raise and psoas stretch test. The psoas stretch test is performed by extending the patient’s leg and externally rotating it, which could reproduce the patient’s groin pain [11, 25].
Radiographs were obtained at all followup visits with three projections used for radiographic analysis: AP pelvis and AP and cross-table lateral radiographs of the operative hip. One of us (RBB) reviewed these radiographs for periprosthetic lucency or loosening according to the systems of DeLee and Charnley [7] for acetabular lucency and Gruen et al. [9] for femoral periprosthetic lucency, uncovered anterior components that may lead to iliopsoas tendonitis [25] or evidence of impingement (insufficient head neck offset ratio) of the residual femoral neck after total hip resurfacing [2, 18]. It should be noted that substantial interobserver variability exists in assessment of periprosthetic lucency. Prior studies have indicated kappa = 0.37 or a rate of consensus of 46% for acetabular components and 87% consensus for femoral components [4, 24]. Additional tests were obtained as needed, eg, CT scan to evaluate for occult periprosthetic fracture or laboratory studies and aspiration to evaluate possible infectious etiology.
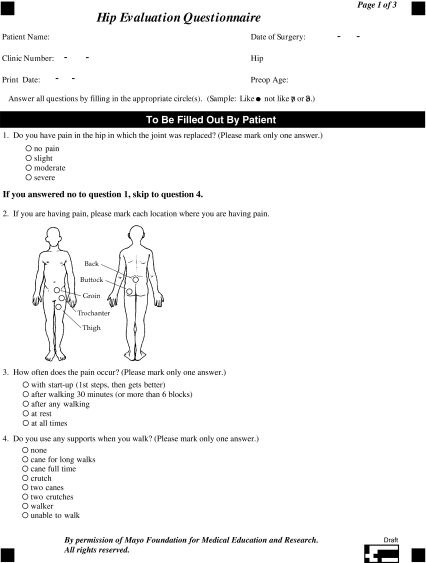
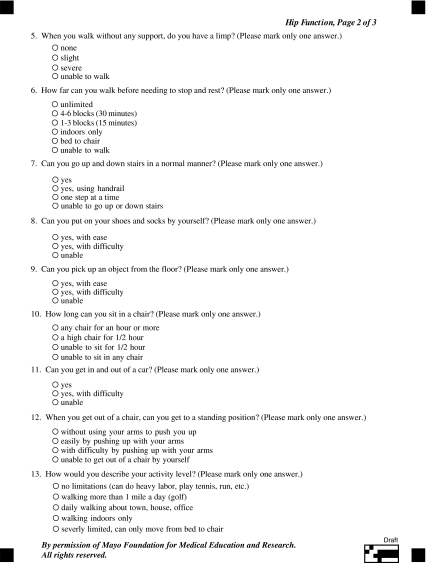
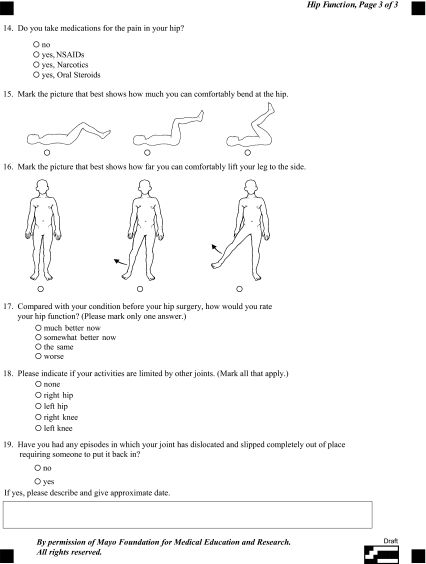
Patients who were unable to return for evaluation were sent a standardized questionnaire (Appendix 2) to evaluate their function and satisfaction. Additionally, these patients were asked to have a local orthopaedic surgeon send the results of a clinical examination and recent radiographs. Of the 269 patients included in the study, 245 (91%) returned to clinic for followup at the one year mark and the remainder sent in the questionnaire. All patients returning to clinic for examination had complete radiographs available. No patients following up via questionnaire had 1 year radiographs available but all had immediate postoperative radiographs for review. It should be mentioned that all patients noting groin pain at the 12 month visit in the current study were evaluated in clinic by the treating surgeon and had complete radiographic examinations.
Results are reported as mean (SD) or count (percentage) unless otherwise specified. The analysis focused primarily on the outcome of groin pain at 1 year postoperatively. Potential risk factors evaluated included age, gender, body mass index (BMI), preoperative diagnosis, surgical approach, and prosthetic bearing surface (polyethylene, ceramic, metal [THA], and metal [resurfacing]). The association of these factors with the outcome of groin pain was evaluated using logistic regression with univariate analyses performed. Because a subset of the patients had both right and left hips included in the analysis, the logistic regression was performed in a generalized linear models framework using generalized estimating equations to properly account for the within-patient correlation. Odds ratios are reported with 95% confidence intervals. All statistical tests were two-sided. A power analysis was performed and showed the present data set had 80% power to detect a rate of groin pain of at least 23% in the hip resurfacing group and 27% in the metal-on-metal THA group as being different from the observed rate of 7% in the conventional THA group.
Results
The rate of groin pain was higher for patients who underwent hip resurfacing or metal-on-metal THA versus conventional THA with polyethylene or ceramic acetabular liners (Table 1).
Table 1.
Rate of groin pain at one year postoperatively
| Surgery type | Rate of groin pain | Statistical comparison to conventional THA |
|---|---|---|
| Conventional THA | 15/217 (7%) | |
| Metal-on-metal THA | 4/26 (15%) | Odds ratio, 2.45; 95% CI, 0.73–8.19, p = 0.146 |
| Resurfacing | 7/39 (18%) | Odds ratio, 2.95; 95% CI, 1.10–7.91, p = 0.032 |
Younger patients were more likely to report pain (Table 2) and were also more likely (p < 0.001) to have received a metal-on-metal bearing surface. Because the mean ages for the implant type groups differed (mean age, 49 versus 61 years for metal-on-metal and conventional bearing surfaces, respectively), we performed further analysis to control for the confounding effect of age on the effect of surgery type. The 26 patients with groin pain were matched on age (± 3 years) and gender to 26 patients without pain. A comparison of the rates of pain among this small subset of age- and gender-matched patients revealed similar outcomes regardless of bearing surface (p = 0.19 for resurfacing versus conventional THA, p = 0.32 for metal-on-metal versus conventional THA). No other variables studied predicted pain (Table 2).
Table 2.
Risk factors for groin pain at one year status post arthroplasty
| Variable | p value | Odds ratio (95% confidence interval) |
|---|---|---|
| Age | 0.017 | 1.38 (1.05–1.81) for 10 year decrease in age |
| Preoperative diagnosis | ||
| DDH versus OA | 0.051 | 2.67 (1.00–1.74) |
| OA versus other diagnoses | 0.768 | 1.19 (0.37–3.78) |
| Gender | 0.734 | 1.15 (0.51–2.59) for male |
| BMI (> 25 versus < 25) | 0.627 | 0.80 (0.32–2.00) |
Patients who received resurfacing were more likely to have moderate or severe pain (Table 3). Of these, two underwent revision to THA for apparent femoral neck impingement resulting in mild pain, with excellent pain relief after revision (Fig. 1A–B). An additional patient obtained satisfactory pain relief with an ultrasound-guided injection into the iliopsoas sheath tendon (Fig. 2A–B). One patient in the conventional THA group also received an ultrasound guided injection for iliopsoas impingement with good outcome (Fig. 3A–B). Patients identified as indeterminate all had mild pain that was not easily categorized by history, examination, or radiographic findings, and they felt no need for further diagnostic studies.
Table 3.
Severity and etiology of groin pain
| Resurfacing | Metal-on-metal THA | Conventional THA | |||||
|---|---|---|---|---|---|---|---|
| Severity | |||||||
| Mild | 4 | 3 | 13 | ||||
| Moderate | 2 | 1 | 2 | ||||
| Severe | 1 | ||||||
| Etiology | |||||||
| Iliopsoas impingement | 1 | 6 | |||||
| Femoral neck impingement | 5 | ||||||
| Periprosthetic fracture | 1 | 2 | |||||
| Recurrent dislocation | 1 | ||||||
| Indeterminate | 1 | 3 | 6 | ||||
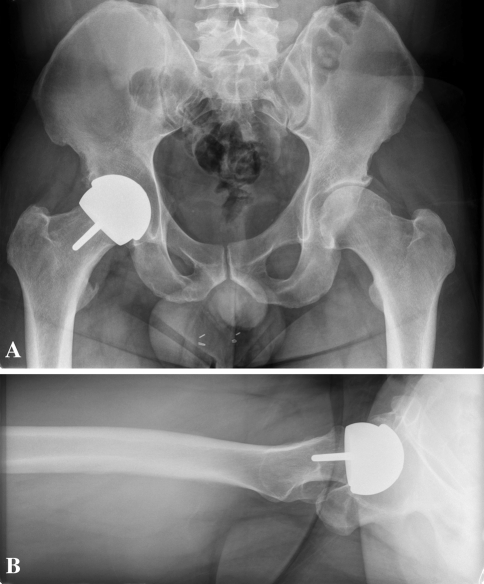
Fig. 1A–B.
The radiographs of a 35-year-old patient with residual groin pain with high flexion activities after total hip resurfacing performed for osteoarthritis are shown. (A) There is an apparent CAM lesion remaining on the anterior surface of the femoral neck. Postoperative pain was mild and no further treatment was recommended. (B) Calcification at the lesser trochanter can also be seen; however, pain was only present at high degrees of flexion where the osteophyte may contact the acetabular component.
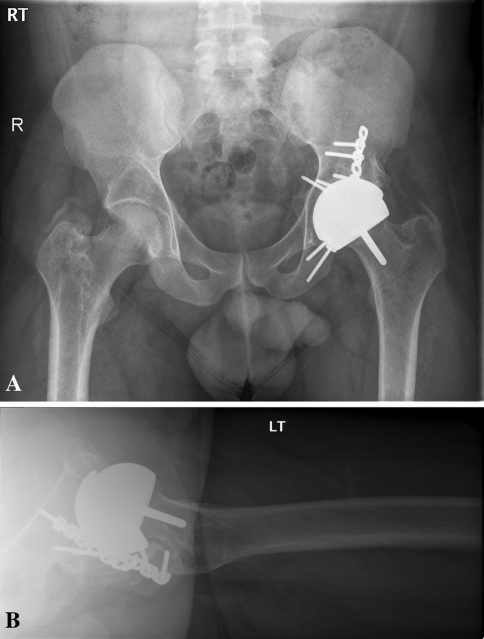
Fig. 2A–B.
The radiographs of a 24-year-old patient with groin pain consistent with iliopsoas impingement after total hip resurfacing performed for posttraumatic arthritis are shown. (A) The cup is not prominent anteriorly; however, the large femoral head is prominent and somewhat medialized on the femoral neck. (B) Also, a screw tip projects into the pelvis that may irritate the iliacus muscle. The patient experienced moderate groin pain that was relieved with an ultrasound-guided iliopsoas tendon sheath injection.
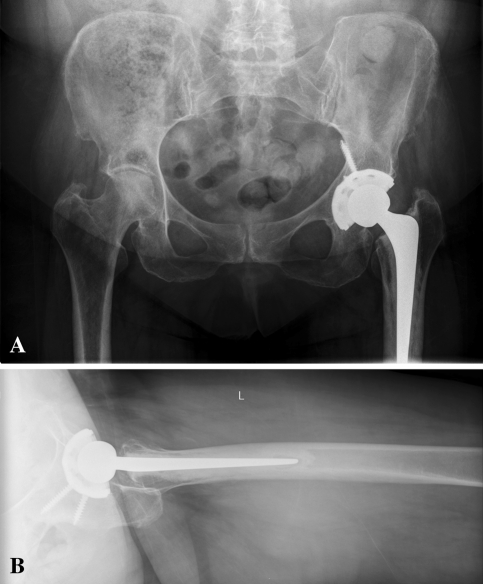
Fig. 3A–B.
The radiographs of a 76-year-old patient with groin pain consistent with iliopsoas impingement after metal-on-polyethylene THA performed for osteoarthritis are shown. (A) The cup is prominent anteriorly as a result of relative lack of anteversion and possible oversizing. (B) Pain was relieved after ultrasound-guided iliopsoas tendon sheath injection.
Discussion
Metal-on-metal bearing surfaces in hip arthroplasty have advantages such as decreased wear and dislocation rates [4, 10, 16, 19, 22] compared to conventional THA. However, their use may be associated with an increased rate of postoperative groin pain when compared to conventional THA [1, 17, 20]. We performed the present retrospective study to assess (1) whether the rate of groin pain after total hip resurfacing and metal-on-metal THA is greater than conventional THA; and (2) the possible factors leading to the increased risk of groin pain.
Our study is limited by several factors. First, the effects of patient activity and expectations are impossible to measure in a retrospective study. Second, the patient populations were heterogeneous among the type of hip arthroplasty, with younger patients much more likely to receive a metal-on-metal bearing surface. Both young age and metal-on-metal bearing surfaces were risk factors for groin pain in the present study, suggesting the possibility of statistical interaction between these variables. Third, the relatively small number of patients reporting pain at 1 year limited our ability to separate these and other potentially confounding variables. Fourth, our analysis is limited by the fact that many patients reporting groin pain at 1 year were pleased with the outcome of their surgery and only had mild pain; therefore, no additional studies were obtained beyond the standard radiographs and physical examination that would yield clues to the etiology of their pain. Further investigation into various causes of their pain was not clinically indicated. Exclusion of these patients with mild indeterminate causes of groin pain, which may not be attributable to the hip arthroplasty, may lead to different results. However, it should be noted that non-arthroplasty causes of pain would be expected to be similar among the study groups.
We found a higher rate of groin pain for patients receiving THA or resurfacing with metal-on-metal bearing surfaces than for conventional bearing surfaces. This is in agreement with prior work (Table 4). Most patients had only mild pain, and examination and radiographic analysis did not lead to a diagnosis in many cases. However, bone and soft tissue impingement were common (Table 3) and seem to be more prevalent with hip resurfacing versus conventional THA. In addition, we separately analyzed metal-on-metal THA and found a similar rate of groin pain to the resurfacing group (Table 1). We are not aware of any studies that have reported on these data. Possible causes for the increased rates of pain include hypersensitivity to metal-on-metal bearing surfaces [7, 14, 21, 27] (although this was not diagnosed in any of our patients) or greater impingement of the psoas tendon across the larger femoral heads used for resurfacing or metal-on-metal THA compared to conventional THA [1, 5, 8, 11, 12, 20, 23, 25, 26].
Table 4.
Groin pain after hip arthroplasty-reported values
| Study | Duration of followup* | Rate of groin pain |
|---|---|---|
| Nasser et al. [17] | 12 (26) | 18% resurfacing |
| O’Sullivan et al. [20] | 2 (20) | 0.37% conventional THA (requiring surgery) |
| Ala Eddine et al. [1] | 1 (7) | 4.3% THA |
| Bartelt et al. [current study] | 12 (14) | 18% resurfacing 15% metal on metal THA 7% conventional THA |
* Duration of followup is reported as minimum and mean values in months.
Risk factors for groin pain after THA and resurfacing were analyzed and we found that younger age at the time of surgery was an important predictor of groin pain at 1 year in this study. Notably, patients receiving metal-on-metal bearing surfaces in the present study were younger on average compared with conventional THA. Activity after THA is related to patient age with patients between the ages of 50 and 59 the most active [13]. Anticipated activity level after surgery is part of our preoperative selection criteria for metal-on-metal bearings, creating potential bias. Younger patients, with ostensibly higher activity levels and expectations, were more likely to receive metal-on-metal bearing surfaces and therefore could potentially report more pain postoperatively. Unfortunately, we lacked sufficient statistical power in the current study to adequately address this possibly confounding variable. Recent work examining groin pain after hip resurfacing suggests there is no effect of age on the rate of pain [17]. While female gender has been associated with postoperative groin pain in two studies [17, 20], we found no such association. Most hip resurfacings in the present study were performed in men (32 of 39, 82%), limiting our ability to analyze gender as a risk factor.
Our data suggest patients who undergo metal-on-metal THA or hip resurfacing with metal-on-metal bearing surfaces may be more likely to experience groin pain at 1 year after surgery and these patients tend to be younger. Many potential causes of pain are preventable with proper surgical technique and/or patient selection. Further study is required to confirm whether patient age, expectations and activity level contribute to groin pain.
Acknowledgments
We thank Dirk Larson, MS for assistance with statistical analysis.
Appendix 1
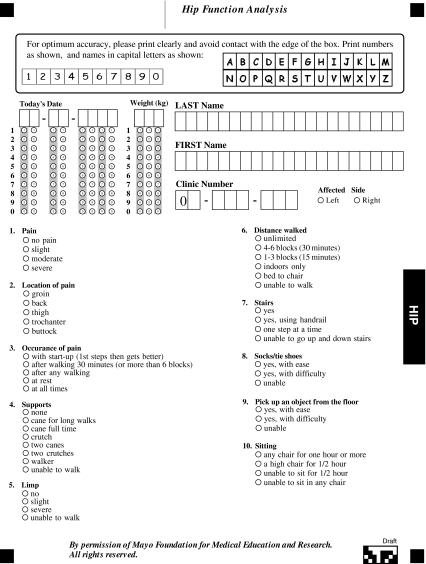
Appendix 2
Footnotes
One or more of the authors (RTT, RJS) has received funding from DePuy, Wright Medical Technologies, or Biomet. The institution of the authors has received funding from DePuy, Zimmer and Stryker. Each author certifies that he or she has or may receive payments or benefits from a commercial entity related to this work.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ala Eddine T, Remy F, Chantelot C, Giraud F, Migaud H, Duquennoy A. Anterior iliopsoas impingement after total hip arthroplasty: diagnosis and conservative treatment in 9 cases [in French] Rev Chir Orthop Reparatrice Mot. 2001;87:815–819. [PubMed] [Google Scholar]
- 2.Beaulé PE, Harvey N, Zaragoza E, Le Duff MJ, Dorey FJ. The femoral head/neck offset and hip resurfacing. J Bone Joint Surg Br. 2007;89:9–15. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 3.Bozic KJ, Kurtz S, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:1614–1620. doi: 10.2106/JBJS.H.01220. [DOI] [PubMed] [Google Scholar]
- 4.Brand RA, Yoder SA, Pedersen DR. Interobserver variability in interpreting radiographic lucencies about total hip reconstructions. Clin Orthop Relat Res. 1985;192:237–239. [PubMed] [Google Scholar]
- 5.Cyteval C, Sarrabère MP, Cottin A, Assi C, Morcos L, Maury P, Taourel P. Iliopsoas impingement on the acetabular component: radiological and computed tomography findings of a rare hip prosthesis complication in eight patients. J Comput Assist Tomogr. 2003;27:183–188. doi: 10.1097/00004728-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Davies AP, Willert HG, Campbell PA, Learmouth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am. 2005;87:18–27. doi: 10.2106/JBJS.C.00949. [DOI] [PubMed] [Google Scholar]
- 7.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 8.Dora C, Houweling M, Koch P, Sierra RJ. Iliopsoas impingement after total hip replacement: the results of non-operative management, tenotomy or acetabular revision. J Bone Joint Surg Br. 2007;89:1031–1035. doi: 10.1302/0301-620X.89B8.19208. [DOI] [PubMed] [Google Scholar]
- 9.Gruen TA, McNeice GM, Amstutz HC. Modes of failure of cemented stem-type femoral components: a radiologic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 10.Harris WH. Wear and periprosthetic osteolysis. Clin Orthop Relat Res. 2001;393:66–70. doi: 10.1097/00003086-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Heaton K, Dorr LD. Surgical release of iliopsoas tendon for groin pain after total hip arthroplasty. J Arthroplasty. 2002;17:779–781. doi: 10.1054/arth.2002.33570. [DOI] [PubMed] [Google Scholar]
- 12.Jasani V, Richards P, Wynn-Jones C. Pain related to the psoas muscle after total hip replacement. J Bone Joint Surg Br. 2002;84:991–993. doi: 10.1302/0301-620X.84B7.13194. [DOI] [PubMed] [Google Scholar]
- 13.Kinkel S, Wollmerstedt N, Kleinhans JA, Hendrich C, Heisel C. Patient activity after total hip arthroplasty declines with advancing age. Clin Orthop Relat Res. 2009;467:2053–2058. doi: 10.1007/s11999-009-0756-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis after contemporary metal-on-metal total hip arthroplasty. Five to nine-year follow-up. J Bone Joint Surg Am. 2006;88:1183–1191. doi: 10.2106/JBJS.D.02916. [DOI] [PubMed] [Google Scholar]
- 15.Lavigne M, Rama KR, Roy A, Vendittoli PA. Painful impingement of the hip joint after total hip resurfacing: a report of two cases. J Arthroplasty. 2008;23:1074–1079. doi: 10.1016/j.arth.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84(Suppl 2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 17.Nasser AB, O’Neill Beaule PE, ME Kim PR, Fazekas A. Incidence of groin pain after metal on metal hip resurfacing. Clin Orthop Relat Res. 2010;468:392–399. doi: 10.1007/s11999-009-1133-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nikolaou V, Bergeron SG, Huk OL, Zukor DJ, Antoniou J. Evaluation of persistent pain after hip resurfacing. Bull NYU Hosp Jt Dis. 2009;67:168–172. [PubMed] [Google Scholar]
- 19.Oparaugo PC, Clarke IC, Malchau H, Herberts P. Correlation of wear debris-induced osteolysis and revision with volumetric wear-rates of polyethylene—a survey of 8 reports in the literature. Acta Orthop Scand. 2001;72:22–28. doi: 10.1080/000164701753606644. [DOI] [PubMed] [Google Scholar]
- 20.O’Sullivan M, Tai CC, Richards S, Skyrme AD, Walter WL, Walter WK. Iliopsoas Tendonitis. A complication after total hip arthroplasty. J Arthroplasty. 2007;22:166–170. doi: 10.1016/j.arth.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 21.Pandit H, Vlychou M, Whitwell D, Crook D, Luqmani R, Ostlere S, Murray DW, Athanasou NA. Necrotic granulomatous pseudotumors in bilateral resurfacing hip arthroplasties: evidence for a type IV immune response. Virchows Arch. 2008;453:529–534. doi: 10.1007/s00428-008-0659-9. [DOI] [PubMed] [Google Scholar]
- 22.Sochard DH. Relationship of acetabular wear to osteolysis and loosening in total hip arthroplasty. Clin Orthop Relat Res. 1999;363:135–150. [PubMed] [Google Scholar]
- 23.Taher RT, Power RA. Iliopsoas tendon dysfunction as a cause of pain after total hip arthroplasty relieved by surgical release. J Arthroplasty. 2003;18:387–388. doi: 10.1054/arth.2003.50047. [DOI] [PubMed] [Google Scholar]
- 24.Temmerman OPP, Raijmakers PGHM, David EFL, Pijpers R, Molenaar MA, Hoekstra OS, Berkhof J, Manoliu RA, Teule GJJ, Heyligers IC. A comparison of radiographic and scintigraphic techniques to assess aseptic loosening of the acetabular component in a total hip replacement. J Bone Joint Surg Am. 2004;86:2456–2463. doi: 10.2106/00004623-200411000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Trousdale RT, Cabanela ME, Berry DJ. Anterior iliopsoas impingement after total hip arthroplasty. J Arthroplasty. 1995;10:546–549. doi: 10.1016/S0883-5403(05)80160-3. [DOI] [PubMed] [Google Scholar]
- 26.Valle CJD, Rafii M, Jaffe WL. Iliopsoas tendinitis after total hip arthroplasty. J Arthroplasty. 2001;16:923–926. doi: 10.1054/arth.2001.26597. [DOI] [PubMed] [Google Scholar]
- 27.Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Koster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical histomorphological study. J Bone Joint Surg Am. 2005;87:28–36. doi: 10.2106/JBJS.A.02039pp. [DOI] [PubMed] [Google Scholar]