Abstract
Background
A number of recent reports have described novel failure mechanisms of metal-on-metal bearings in total and resurfacing hip arthroplasty. Hip arthroplasties with metal-on-metal articulations are also subject to the traditional methods of failure seen with different bearing couples. There is currently little information in the literature to help guide timely clinical evaluation and management of these patients.
Questions/purposes
We therefore describe the (1) clinical presentations; (2) reasons for failure; (3) operative findings; and (4) histologic findings in patients with failed metal-on-metal hip arthroplasties.
Methods
We retrospectively identified all 37 patients (37 hips) with metal on metal total hip or resurfacing arthroplasties who underwent revision over the past 3 years at our institution. Relevant clinical, radiographic, laboratory, intraoperative, and histopathologic findings were analyzed for all patients.
Results
Of the 37 patients, 10 were revised for presumed hypersensitivity specific to the metal-on-metal articulation. This group included eight patients with tissue histology confirming chronic inflammation with lymphocytic infiltration, eight with aseptic loosening of a monoblock screwless uncemented acetabular component, two with iliopsoas impingement associated with a large-diameter femoral head, and three with femoral neck fracture after resurfacing arthroplasty; the remainder of the patients were revised for infection, instability, component malposition, and periprosthetic fracture.
Conclusions
Increased awareness of the modes of failure will bring to light the potential complications particular to metal-on-metal articulations while placing these complications into the context of failures associated with all hip arthroplasties. This novel clinical information should be valuable for the practicing surgeon faced with this patient population.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
In recent years, there has been renewed interest in metal-on-metal bearing surfaces for THA. Decreased wear rates, absence of polyethylene debris, and improved stability are favorable aspects of large head metal-on-metal articulations [11]. Metal-on-metal technology is now used in over one-third of all hip arthroplasties performed in the United States [4].
At the same time, there is increasing awareness of potential biologic consequences unique to the metal-on-metal bearing couple. Adverse local tissue reactions specific to metal particulate debris have been described [5, 21]. The incidence of metal-on-metal-induced hypersensitivity tissue reactions remains uncertain, although recent reports suggest an incidence of 1% or less [5, 11]. The proposed mechanism, still incompletely understood, is believed to have an inflammatory component with delayed-type hypersensitivity-like reactions termed aseptic lymphocytic vasculitis-associated lesions (ALVAL) [5, 10, 21]. Necrotic changes have also been observed with cobalt-chrome wear particles in periprosthetic tissues [15]. There appears to be a spectrum of reactivity and soft tissue changes, with a number of potential factors (ie, female gender, implant design and size, acetabular component position, and obesity) having been described that predispose to this response [13, 17].
Some additional modes of failure exist that are unique to modern metal-on-metal implants. Femoral neck fracture after resurfacing has been well-described [1, 20]. Early mechanical failure of the solid monoblock acetabular component with larger-diameter metal-on-metal THA has also been reported and is believed to be the result of particular aspects of implant design or technique [12, 14]. The difficulty in evaluating and treating these patients has been described, and delay in diagnosis is likely common [7]. A painful metal-on-metal total hip may be difficult to diagnose given our limited experience with these inflammatory synovial reactions and lack of awareness of clinical presentation along with the uncertainty regarding the appropriate treatment.
We therefore describe the (1) clinical presentations; (2) reasons for failure; (3) operative findings; and (4) histologic findings in patients with failed metal-on-metal hip arthroplasties. The purpose of this report is to focus on this critical and controversial clinical issue and detail our observational findings in patients who appear to have failed from adverse reactions to metal debris. The descriptive account of these relatively novel findings can be added to the emerging understanding of this poorly understood problem. Greater awareness of the presentation and findings in these patients should reduce the delays in diagnosis and help guide appropriate treatment.
Patients and Methods
We retrospectively identified from our institutional total joint registry 37 patients who had a revision of a failed metal-on-metal articulation over the past 3 years (September 1, 2006 through August 31, 2009). Twenty four of the 37 patients (65%) were female; the mean age at the time of surgery was 56 years (range, 34–83 years). During this time period, 1032 revision THAs were performed in patients with bearings other than metal-on-metal. Thus, patients with metal-on-metal bearings comprised a small minority (3.5%) of our total revision hip population. Six of the index procedures (16%) were performed at our institution; the majority of the index procedures were performed elsewhere and the patient subsequently referred to our center. Twenty-nine of the patients (77%) had a metal-on-metal articulation placed at the time of their primary hip surgery, whereas the remainder had the bearing couple placed at the time of a revision procedure. Three patients presented with failed hip resurfacings and the remainder had THAs.
Preoperative demographic and clinical data, encompassing symptoms and physical exam findings, were collected prospectively on a routine basis for all total joint patients and recorded in our institutional registry. We further retrospectively reviewed the medical records of all patients identified in the registry as having had a metal-on-metal bearing at the time of revision during the time interval of this study; no patients were recalled in followup specifically for this study. There was no standard approach to the laboratory and imaging workup of these patients prior to revision surgery, and the diagnostic evaluation varied by surgeon and clinical presentation. Laboratory markers of inflammation were obtained on all patients. Skin patch testing, ion levels, and lymphocyte proliferation assays were not routinely performed. The results of any hip aspirations were recorded if available. Preoperative anteroposterior and cross-table lateral hip radiographs were retrospectively analyzed in blinded fashion by a single reviewer using digital templating software to determine acetabular component abduction and anteversion angles, respectively; plain radiographs have been reported to give good, but not excellent, reproducibility and acceptable interobserver reliability for radiographic measurement of cup position but are less exact than CT measurement [8]. Additional imaging studies (CT or MRI) were not routinely obtained, although they were reviewed for this study if they had been performed.
Nine different surgeons performed the revision procedures. The surgical approach was through either an anterolateral or posterior approach depending on surgeon preference. Intraoperatively, tissue and fluid were sent for culture and histopathology routinely in all patients. Intraoperative findings were obtained through review of the operative note dictated by the surgeon and photographs when available.
Tissue was obtained for pathologic and microbial analysis in all patients. At least one sample was routinely obtained from the periprosthetic pseudocapsule. Cancellous bone was not routinely sampled. The degree of inflammation was assessed qualitatively by a board-certified pathologist familiar with revision total joint arthroplasty. The diagnosis of ALVAL was made when an inflammatory infiltrate of lymphocytes and macrophages was seen in a perivascular distribution [2, 13, 15]. Areas of necrosis were also noted if present. Retrieval analysis was not performed on any of the prostheses.
Postoperative clinical outcomes were determined solely through chart review. At our institution, patients are routinely seen at two months, one year, and yearly thereafter, although the followup intervals may be individualized by the surgeon depending upon patient circumstances. The minimum followup after revision surgery for patients diagnosed with an adverse reaction to the metal-on-metal articulation was two months (mean, 12 months; range, 2 to 28 months).
The study protocol was approved by our local Institutional Review Board, and informed consent to participate in medical research was obtained from all patients.
Results
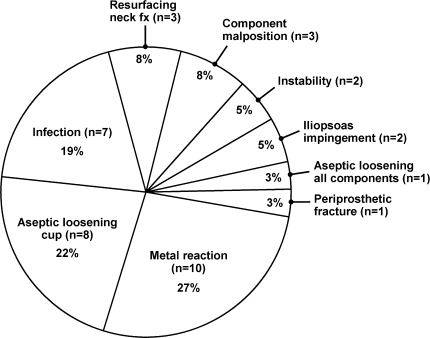
The reasons for revision were varied. The majority of revisions were performed for reasons that are not unique to metal-on-metal articulations (Fig. 1). The clinical presentations, reasons for revision, operative findings, and histologic findings in those patients with conventional methods of failure were typical and have been well described previously in the literature (Table 1).
Fig. 1.
The etiology of revision in patients with a metal-on-metal bearing couple at our institution over the past 3 years is depicted.
Table 1.
Patients revised with a metal-on-metal bearing excluding those with evidence of an adverse local reaction to a metal-on-metal bearing
| Patient number | Age | Gender | Reason for revision | Original procedure | Time to revision | Revision procedure | Types of implants revised |
|---|---|---|---|---|---|---|---|
| 1 | 30 | F | Aseptic loosening of acetabular component | THA | 11 months | Acetabular component | Wright Medical Conserve |
| 2 | 58 | F | Aseptic loosening of acetabular component | RTHA for instability | 14 months | Acetabular component, trochanteric advancement | Zimmer Durom |
| 3 | 55 | F | Aseptic loosening of acetabular component | RTHA for leg length inequality | 17 months | Acetabular component | Wright Medical Conserve |
| 4 | 57 | F | Aseptic loosening of acetabular component | THA | 52 months | Acetabular component | Biomet M2a |
| 5 | 66 | F | Aseptic loosening of acetabular component | THA | 18 months | Acetabular component | DePuy Ultamet |
| 6 | 45 | M | Aseptic loosening of acetabular component | THA | 48 months | Acetabular component | Biomet M2a |
| 7 | 56 | F | Aseptic loosening of acetabular component | RTHA for aseptic loosening of cup | 27 months | Acetabular component | Biomet M2a |
| 8 | 41 | F | Aseptic loosening of acetabular component | THA | 15 months | Acetabular component | Zimmer Durom |
| 9 | 51 | M | Infection | THA | 24 months | Resection followed by two stage revision | Wright Medical Conserve |
| 10 | 60 | M | Infection | THA | 6 months | I&D, acetabular component only | Biomet M2a |
| 11 | 44 | F | Infection | THA | 18 months | I&D, resection of all components | Wright Medical Conserve |
| 12 | 51 | F | Infection | RTHA for previous infection | 4 months | I&D, liner exchange | DePuy Ultamet |
| 13 | 64 | M | Infection | THA | 2 months | Resection followed by two stage revision | DePuy ASR |
| 14 | 57 | M | Infection | THA | 22 months | Resection followed by two stage revision | DePuy ASR |
| 15 | 45 | F | Infection | THA | 30 months | Resection followed by two stage revision | Biomet M2a |
| 16 | 52 | F | Femoral neck fracture following HRA | HRA | 1 month | Conversion to THA (femoral side only) | DePuy ASR HRA |
| 17 | 48 | M | Femoral neck fracture following HRA | HRA | 6 months | Conversion to THA (all components) | Wright Medical Conserve Plus HRA |
| 18 | 53 | M | Femoral neck fracture following HRA | HRA | 3 months | Conversion to THA (femoral side only) | DePuy ASR HRA |
| 19 | 51 | F | Component malposition | THA | 17 months | All components | DePuy Ultamet |
| 20 | 55 | M | Component malposition | RTHA for aseptic loosening | 1 month | All components | Biomet M2a |
| 21 | 65 | F | Component malposition | THA | 18 months | Acetabular component | Wright Medical Conserve |
| 22 | 63 | F | Iliopsoas impingment | THA | 36 months | Acetabular component, iliopsoas tendon release | DePuy ASR |
| 23 | 64 | F | Iliopsoas impingment | THA | 14 months | Acetabular component, iliopsoas tendon release | DePuy ASR |
| 24 | 34 | M | Recurrent instability | Hip fusion takedown with THA | 2 weeks | Acetabular component | DePuy Ultamet |
| 25 | 60 | F | Recurrent instability | THA | 7 months | Conversion to constrained liner, abductor reconstruction | DePuy Ultamet |
| 26 | 83 | M | Periprosthetic fracture with loose femoral stem | THA | Unknown1 | All components | Unknown1 |
| 27 | 66 | F | Aseptic loosening of both components | THA for femoral neck fracture | 27 months | All components | Biomet M2a |
THA = total hip arthroplasty; RTHA = revision total hip arthroplasty; I&D = irrigation and debridement.
1Date of primary total hip arthroplasty and manufacturer of implants could not be verified.
Ten patients were revised for a presumed adverse response to the metal-on-metal bearing (Table 2). Three of these patients had already undergone revision in which a metal-on-metal bearing was used (one failed hip resurfacing, one aseptic cup loosening, one two-stage revision for infection), whereas the remainder of patients had failed primaries. Seven patients had large-diameter metal-on-metal bearings, including one hip resurfacing.
Table 2.
Clinical and intraoperative findings of 10 patients revised for adverse local reaction to a metal-on-metal bearing
| Patient number | Age (years) | Gender | Original procedure | Onset of symptoms | Clinical presentation | Clinical exam | Cup position | ESR/CRP* |
|---|---|---|---|---|---|---|---|---|
| 1 | 54 | F | Primary THA | Since surgery | GP, NR, L, TP | L, St | 57 abd, 0 ante | 17, 3.6 |
| 2 | 63 | F | Primary THA | Since surgery | NR, GP, I, M (catching), SP, Sit | St, Pex | 38 abd, 20 ante | 13, 0.3 |
| 3 | 62 | F | Primary THA | Never recovered | GP, SP, Sit, | L, Pex | 44 abd, 18 ante | 37, 26.7 |
| 4 | 56 | M | Primary THA | Since surgery | F/C, NR, responded to prednisone | L | 47 abd, 20 ante | 34, 6.4 |
| 5 | 59 | F | Revision THA for failed HRA | Since surgery | M (clunk), GP, PWB | L, Pex | 43 abd, 49 ante | Within normal limits |
| 6 | 69 | M | Primary HRA | Never recovered | NR, L, PWB | Palp fluid collection, abductor weakness, swelling | 50 abd, 45 ante | 20, 10.6 |
| 7 | 55 | F | Primary THA | Since surgery | M (audible clunk), PWB | Audible clunk | 56 abd, 43 ante | 3, 3.4 |
| 8 | 61 | F | Revision THA for infection | Since surgery | L, PWB | Pex | 48 abd, 39 ante | 7, 3.8 |
| 9 | 60 | F | Revision THA for aseptic loosening cup | Never recovered | M (clicking), GP | Pex, crutches, St | 60 abd, 1 ante | 7, <3 |
| 10 | 55 | M | Primary THA | Since surgery | L, M (audible squeak) | L, swelling, audible squeak | 43 abd, 30 ante | 46, 53.5 |
| Aspiration | Time to revision | Intraoperative findings | Pathology | Implants revised | Revision performed | Followup after revision | Clinical outcome |
|---|---|---|---|---|---|---|---|
| N/A | 36 months | Yellow fluid, greenish membrane | ALVAL | Biomet M2a | Revision cup with MOP | 6 months | Excellent (no pain, limp resolved) |
| N/A | 10 months | Large benign-appearing fluid collection | ALVAL | DePuy ASR | Revision cup with MOP | 28 months | Fair (preop pain resolved, developed femoral loosening 2 yrs postop) |
| 202 nucleated cells, CN | 17 months | Cloudy fluid, synovial proliferation | ALVAL | Biomet M2a | Cemented poly liner | 6 months | Good (occasional groin ache) |
| CN | 42 months | Milky fluid, synovitis | ALVAL | DePuy Ultamet | Modular poly liner exchange | 15 months | Fair (persistent buttock pain, limp) |
| CN | 48 months | Shaggy synovium, dark fluid, wear | Fibrous, extensive necrosis | Stryker Optimom | Revision cup with MOP | 2 months | Good (mild residual ache) |
| 988 nucleated cells, CN | 46 months | Large milky fluid collection with whitish tissue | ALVAL | Stryker Cormet | Revision cup with COP | 5 months | Excellent (no pain or limp) |
| N/A | 24 months | Osteolysis femur, fibrous cup, metallosis, wear, synovitis | ALVAL | DePuy ASR | Revision cup with MOP | 12 months | Excellent (no pain, no clunk) |
| N/A | 24 months | Loose cup, metallosis, cystic fluid mass | Dense chronic inflammation | Wright Medical Conserve | Revision cup with MOP | 3 months | Good (recovering as expected) |
| 37191 nucleated cells, CN | 15 months | Milky fluid, wear | ALVAL | Biomet M2a | Revision cup with MOP | 18 months | Excellent (no pain, radiolucencies around cup) |
| 260 nucleated cells, CN | 5 months | Necrosis, metallosis, fluid | Acellular, extensive necrosis | DePuy ASR | Cemented poly liner | 27 months | Poor (limp, developed acute hematogenous infection at 2 yrs postop) |
* Institutional normal values for ESR are 0-22 mm/hour and CRP are less than 8.0 mm/L; ESR = erythrocyte sedimentation rate (units mm/hour); CRP = C-reactive protein (units mm/L); F = female; M = male; HRA = hip resurfacing arthroplasty; ALVAL = lymphocytic infiltration; NR = never recovered from index procedure; GP = groin pain; TP = thigh pain; F/C = fevers/chills; I = feeling of instability; M = mechanical symptoms; SP = startup pain; Sit = pain with prolonged sitting; PR = pain at rest; NP = night pain; L = limp; PWB = pain with weight bearing; St = Stinchfield test; Pex = pain at extremes of motion; Abd = abduction angle; Ante = anteversion angle; CN = culture negative; MOP = metal-on-polyethylene bearing surface; COP = ceramic-on-polyethylene; poly = polyethylene.
The clinical presentation of these patients was varied. The majority of the patients (seven of 10) were female. All patients reported some degree of symptoms since the time of the index arthroplasty. A majority of patients described symptoms that were clearly not present preoperatively, although some felt that they had just never recovered from the hip replacement. The majority of patients described groin pain aggravated by weightbearing activities. Difficulty with stairs and standing from a seated position was common. Patients commonly felt they were no better clinically than before their hip arthroplasty. The discomfort tended to be localized to the groin and progressive in nature, usually aggravated by the Stinchfield maneuver (resisted straight leg raise). Four patients described mechanical symptoms (clunking or catching), and one patient had a loud audible squeak that could be heard throughout the room. Four patients had elevated inflammatory markers, one presented with fever, and one aspiration revealed over 37,191 nucleated cells with negative cultures. Only two of the patients presented with large effusions and an associated cystic fluid-filled mass consistent with a pseudotumor (Table 2; patients 6 and 8). One patient underwent skin testing, which revealed an allergic response to cobalt. In vitro testing (lymphocyte transformation test) was not performed. No patient presented with a rash.
Radiographs revealed some degree of component malposition in five patients (excessive abduction > 55 degrees and/or anteversion > 40 degrees). Radiographic evidence of osteolysis in Gruen Zones 1 and 7 of the proximal femur was noted on analysis of the radiographs by the treating surgeon in one patient. One acetabular component appeared radiographically loose and was confirmed to lack bony ingrowth at the time of revision. There was one case of component size mismatch, in which a femoral head was used that was larger than recommended by the manufacturer (Table 2; patient 10).
All patients who underwent revision had clinical failure with substantial pain and functional limitation. Revision was undertaken when the patient felt their symptoms warranted surgical treatment, although it was recommended strongly in patients with mechanical derangement as evidenced by clunking or squeaking given concerns about accelerated metal wear and long-term durability. Surgical intervention was also recommended when concern existed for progressive bone or soft tissue destruction. Prior to surgery, an adverse reaction to metal debris was either suspected or considered a possibility in eight of the 10 patients; the other two were thought to have component malposition and soft tissue irritation. Infection was considered preoperatively in several patients owing to systemic symptoms of fever and chills (one patient), elevated inflammatory markers (four patients), and high synovial fluid cell count (one patient); two patients in this series whose presentation mimicked a deep seated hip infection have been previously reported in detail [16].
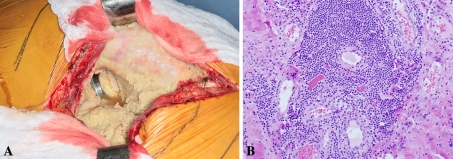
Notable effusions were found intraoperatively in all patients with metal sensitivity. These fluid collections varied in size and gross appearance. The most common presentation was creamy “milk-stained” fluid with tissue necrosis and metallosis (Fig. 2), although four patients did have a more benign-appearing, watery yellowish brown effusion. The characteristics of the fluid varied from thin and translucent to thick, cloudy, and caseous. Brown, yellow, green, and white discolorations were all noted. The fluid was commonly under pressure. A fluid mass consistent with a pseudotumor was seen in two patients. Shaggy, ragged synovial proliferation was frequently encountered. Evidence of excessive metal wear, with gross damage and pitting or scratching of the bearing surfaces, was seen in three patients. Metallosis was common, particularly in patients with a predominantly necrotic component that lacked an inflammatory component on subsequent histological analysis. Varying degrees of tissue necrosis was observed.
Fig. 2A–B.
(A) An intraoperative photograph at the time of revision shows a patient with an adverse reaction to a metal bearing surface demonstrating whitish tissue, a large fluid-filled collection, and milky fluid. (B) A photomicrograph demonstrates the histologic findings of marked lymphocytic inflammation, predominantly perivascular in location (×200 magnification).
All patients were treated with revision of the bearing surface to highly crosslinked polyethylene and a cobalt-chromium (9 patients) or ceramic (1 patient) head. The acetabular component was revised in seven patients to allow for insertion of a modular polyethylene liner. A polyethylene liner was cemented directly into a well-fixed monoblock cup in two patients after scoring the acetabular component surface with a burr. The final case involved a modular cup which allowed the metal liner to be swapped for a polyethylene component. Necrotic tissue was débrided in all instances.
Histologic examination revealed lymphocytic aggregation in the periprosthetic tissues consistent with an ALVAL reaction in seven patients. One case was seen to have a lymphocytic infiltration but lacked clear perivascular aggregation. Tissues obtained from the remaining two patients consisted only of fibrous or acellular tissue with extensive necrosis but no major inflammation. No organisms grew on culture of intraoperative tissue in any of the 10 cases described.
Discussion
There is growing recognition that metal-on-metal hip arthroplasties may fail early from novel mechanisms of failure in addition to the conventional mechanisms well described for all bearing surfaces. In reviewing all metal-on-metal hip arthroplasties revised at our institution over the past 3 years, our purpose was to document and describe the clinical and intraoperative findings in patients with early failures that appear to be unique to these particular implants.
We recognize limitations to our study. First, the study was not designed to provide information about the incidence or prevalence of the failure mechanisms that we encountered. We have attempted to put this failure mechanism into an overall clinical context by reviewing all revisions with a metal-on-metal bearing. However, as the majority of patients were referred to our institution, we do not know the denominator when it comes to the number of metal-on-metal implants that had been used in our referral area during the time of this study. Second, many available diagnostic modalities were not routinely or consistently employed in the workup of these patients. It is important to note that there is no clear consensus for the diagnosis of an adverse metal reaction, and individual laboratory and imaging studies may be useful (but not mandatory) adjuncts in the evaluation and treatment of these patients. Serum and joint ion levels reportedly correlate with in vivo wear and metal debris-related failures [6, 13] and may find routine use in clinical practice when the implications of these levels are better defined. Advanced imaging (MRI, CT, or ultrasound) was obtained in select patients on an individual basis when concern existed for pseudotumor or soft tissue destruction, but we do not have extensive cross sectional imaging data for all patients. Patch testing is unreliable and clinical validation of the accuracy of in vitro lymphocyte testing is lacking at the present time [10]. Third, retrieval analysis was not performed in these patients, limiting our ability to comment on the role of wear of the bearing surfaces in the development of adverse immune responses.
The clinical presentation of patients with an adverse metal reaction was varied and often nonspecific. The majority of patients were women, consistent with previous reports in the literature [17, 18], although this phenomenon did not completely exclude males. One universal complaint in these patients was the feeling that they had either never fully recovered from the procedure or had experienced a new pain sensation since the hip replacement was performed. No patients reported being fully satisfied after the operation, which differs from previous reports that suggest early satisfaction with later development of pain [13]. Stiffness and groin pain was typical when first arising from a chair or getting out of a car, nonspecific complaints that have also been reported with aseptic loosening of large-diameter metal-on-metal acetabular monoblock components [14]. Several patients presented with features concerning for infection, including fevers, elevated inflammatory markers, and an elevated nucleated cell count on aspiration. On average, patients underwent revision around two years after the index procedure, although we noted substantial variability. This is consistent with previous reports suggesting that metal-related complications may take several years to progress to reoperation [13, 18].
The evaluation of patients with a painful metal-on-metal joint can be difficult with an expanded differential diagnosis including metal hypersensitivity and wear. In our experience, the presumptive reason for early failure in patients with an adverse reaction to metal included infection, component malposition and soft tissue irritation, and fibrous fixation of the acetabular component without osseointegration. Our approach to the diagnosis of adverse metal reaction requires exclusion of other well-defined causes of failure. It appears that the inflammatory reaction to the metal debris may increase serum markers and mimic a low grade infection with systemic symptoms [16, 18]. As such, inflammatory markers do not appear to adequately distinguish between an adverse metal reaction and infection, and all patients with abnormal values undergo aspiration with cultures. A high nucleated cell count was present in one of our patients; we therefore consider a positive culture off antibiotics to be more reliable. Furthermore, while component malposition has been suggested to play a role in patients with metal hypersensitivity [13], only a minority of our patients had excessive abduction or anteversion. Early osteolysis has been also associated with metal hypersensitivity [19], although this finding was not prevalent in our experience and seen in only one of our patients. The technetium Tc-99 m white blood cell/colloid study, which labels polymorphonuclear cells but not lymphocytes, may have some intuitive appeal but is of unknown clinical utility [3].
We did not identify any pathognomonic intraoperative findings. Effusion was universal, metallosis was common, and the synovium often appeared shaggy. Obvious macroscopic wear and damage of the components was seen in three patients, suggesting that wear may play a role in the pathophysiology of the adverse metal response, although the majority of implants did not show any macroscopic damage. It is clear from our experience and others that encountering purulent-appearing fluid intraoperatively is not necessarily indicative of infection [7, 16]. Reports exist of two-stage revision for presumed infection with subsequent tissue pathology suggestive of a metal reaction and negative cultures [7]. Frozen specimen analysis was used in all patients to exclude acute inflammation. In our series, the treatment for all patients with clinical, intraoperative, and frozen specimen findings consistent with metal hypersensitivity was single stage revision to a metal-on-polyethylene bearing couple.
The majority of patients had histologic findings consistent with a chronic inflammatory response. We observed perivascular lymphocytic infiltration similar to previously reported histological findings and consistent with ALVAL [5, 21]. Two patients did not appear to have an inflammatory component, but rather had extensive necrosis. These findings are consistent with previous reports suggesting a role for both cytotoxicity and delayed hypersensitivity in the pathogenesis of these reactions [15]. While our experience corroborates previous findings, histopathologic testing continues to have unknown sensitivity and specificity for metal hypersensitivity. The prevalence of these histologic changes in well-functioning metal-on-metal hip arthroplasties is unknown.
The clinical response to revision procedures with a diagnosis of metal hypersensitivity has not been extensively reported. Revision surgery for pseudotumors with massive soft-tissue destruction has a poor reported outcome with substantial challenges [9, 18]. Grammatopolous et al. experienced a 50% incidence of major complications and described lower Oxford hip scores and UCLA activity scores following revision of a failed hip resurfacing in patients pseudotumors compared to matched controls undergoing total hip arthroplasty [9]. Our patients have generally reported pain relief with revision of the bearing surface to a polyethylene insert. While the preoperative limp was seen to improve in many patients, one patient with major damage to the abductor musculature had a persistent severe limp. The amount of soft tissue destruction appeared to generally correlate with subsequent functional outcome. Following revision, there was one case of deep infection, one of femoral component loosening, one with radiolucencies around the acetabular component in an asymptomatic patient, and one case of persistent disabling pain.
While the main focus of our paper is to describe our clinical experience with adverse reactions to metal debris, review of our entire metal-on-metal revision population also suggests a substantial number of early failures of large-diameter metal-on-metal articulations are related to early acetabular component loosening [12]. Technical issues with a steep learning curve have been suggested as a potential reason for these failures [12], although other studies have suggested implant design features may be responsible [14]. Our study is not designed to answer these questions. However, the solid stiff cobalt-chrome shells may be technically more challenging to implant correctly compared with traditional titanium acetabular components and do not allow for supplemental screw fixation.
The majority of revisions of metal-on-metal articulations at our institution were not specific or unique to this bearing couple. However, an adverse local reaction to metal must be considered when evaluating a failed metal-on-metal bearing surface. Consideration of this possibility, along with recognition of the varied clinical and intraoperative findings, should help guide treatment decisions.
Acknowledgments
We thank Dr. Rafael J. Sierra and Dr. Robert T. Trousdale for providing cases and documentation.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in research was obtained.
References
- 1.Amstutz HC, Campbell PA, Le Duff MJ. Fracture of the neck of the femur after surface arthroplasty of the hip. J Bone Joint Surg Am. 2004;86:1874–1877. doi: 10.2106/00004623-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Aroukatos P, Repanti M, Repantis T, Bravou V, Korovessis P. Immunologic adverse reaction associated with low-carbide metal-on-metal bearings in total hip arthroplasty. Clin Orthop Relat Res. 2009 Dec 18. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 3.Biant LC, Bruce WJ, van der Wall H, Walsh WR. Infection or allergy in the painful metal-on-metal total hip arthroplasty? J Arthroplasty. 2009 Feb 23. [Epub ahead of print]. [DOI] [PubMed]
- 4.Bozic KJ, Kurtz S, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:1614–1620. doi: 10.2106/JBJS.H.01220. [DOI] [PubMed] [Google Scholar]
- 5.Davies AP, Willert HG, Campbell PA, Learmonth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am. 2005;87:18–27. doi: 10.2106/JBJS.C.00949. [DOI] [PubMed] [Google Scholar]
- 6.Smet K, Haan R, Calistri A, Campbell PA, Ebramzadeh E, Pattyn C, Gill HS. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am. 2008;90(Suppl 4):202–208. doi: 10.2106/JBJS.H.00672. [DOI] [PubMed] [Google Scholar]
- 7.Engh CA Jr, Ho H, Engh CA. Metal-on-metal hip arthroplasty: does early clinical outcome justify the chance of an adverse local tissue reaction? Clin Orthop Relat Res. 2009 Sep 1. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 8.Ghelman B, Kepler CK, Lyman S, Della Valle AG. CT outperforms radiography for determination of acetabular cup version after THA. Clin Orthop Relat Res. 2009;467:2362–2370. doi: 10.1007/s11999-009-0774-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grammatopolous G, Pandit H, Kwon YM, Gundle R, McLardy-Smith P, Beard DJ, Murray DW, Gill HS. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br. 2009;91:1019–1024. doi: 10.1302/0301-620X.91B8.22562. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs JJ, Hallab NJ. Loosening and osteolysis associated with metal-on-metal bearings: a local effect of metal hypersensitivity? J Bone Joint Surg Am. 2006;88:1171–1172. doi: 10.2106/JBJS.F.00453. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs JJ, Urban RM, Hallab NJ, Skipor AK, Fischer A, Wimmer MA. Metal-on-metal bearing surfaces. J Am Acad Orthop Surg. 2009;17:69–76. doi: 10.5435/00124635-200902000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Kim PR, Beaulé PE, Laflamme GY, Dunbar M. Causes of early failure in a multicenter clinical trial of hip resurfacing. J Arthroplasty. 2008;23(Suppl 1):44–49. doi: 10.1016/j.arth.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 13.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. J Bone Joint Surg Br. 2010;92:38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 14.Long WT, Dastane M, Harris MJ, Wan Z, Dorr LD. Failure of the Durom Metasul(R) acetabular component. Clin Orthop Relat Res. 2010;468:400–405. doi: 10.1007/s11999-009-1071-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N. Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties. Acta Orthop. 2009;80:653–659. doi: 10.3109/17453670903473016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mikhael MM, Hanssen AD, Sierra RJ. Failure of metal-on-metal total hip arthroplasty mimicking hip infection. A report of two cases. J Bone Joint Surg Am. 2009;91:443–446. doi: 10.2106/JBJS.H.00603. [DOI] [PubMed] [Google Scholar]
- 17.Ollivere B, Darrah C, Barker T, Nolan J, Porteous MJ. Early clinical failure of the Birmingham metal-on-metal hip resurfacing is associated with metallosis and soft-tissue necrosis. J Bone Joint Surg Br. 2009;91:1025–1030. doi: 10.1302/0301-620X.91B8.21701. [DOI] [PubMed] [Google Scholar]
- 18.Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90:847–851. doi: 10.1302/0301-620X.90B7.20213. [DOI] [PubMed] [Google Scholar]
- 19.Park YS, Moon YW, Lim SJ, Yang JM, Ahn G, Choi YL. Early osteolysis following second-generation metal-on-metal hip replacement. J Bone Joint Surg Am. 2005;87:1515–1521. doi: 10.2106/JBJS.D.02641. [DOI] [PubMed] [Google Scholar]
- 20.Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg Br. 2005;87:463–464. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 21.Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Köster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28–36. doi: 10.2106/JBJS.A.02039pp. [DOI] [PubMed] [Google Scholar]