Abstract
Background
Acute idiopathic chondrolysis in young adults is rare. The etiology often is unknown and outcomes can be devastating owing to rapid development of painful secondary osteoarthritis. There have been some recent reports of chondrolysis after arthroscopic shoulder procedures. Animal and laboratory data suggest chondrolysis is related to the use of intraarticular pain pumps, although there is no conclusive evidence that this is causative in patients.
Case description
We present two cases of young adults with chondrolysis of the humeral head after intraarticular pain pump use with humeral head resurfacing and biologic glenoid resurfacing.
Literature review
Several authors report glenohumeral chondrolysis after shoulder arthroscopy involving the use of bupivacaine pain pumps. In addition, experimental animal studies have confirmed the presence of chondrolysis after bupivacaine infusion.
Purposes and clinical relevance
These cases provide additional evidence of an important association between postarthroscopic chondrolysis of the glenohumeral joint and the use of bupivacaine pain pumps.
Introduction
Chondrolysis is defined as the disappearance of articular cartilage as the result of lysis or dissolution of the cartilage matrix and cells. Although the incidence of idiopathic chondrolysis remains to be elucidated, secondary chondrolysis with diseases, including slipped capital femoral epiphysis, is well documented [19, 20, 29]. The idiopathic and secondary varieties are rare [30]. Idiopathic chondrolysis is well-defined clinically, usually having its onset early in the second decade of life, with a marked female preponderance. An autoimmune etiology has been proposed [7, 30] but not confirmed. Postarthroscopic glenohumeral chondrolysis has been reported among secondary causes [22, 24]. Although these cases are reported temporally after arthroscopy, the actual cause of this process is unknown and the consequences are devastating. This condition currently has no effective treatment and most affected patients ultimately must consider some type of glenohumeral arthroplasty and/or biologic resurfacing [24]. Although the etiology remains unclear, some studies report patients had glenohumeral chondrolysis after arthroscopic shoulder surgery associated with bupivacaine pain pumps [9, 12]. Given the popularity and success of regional anesthesia and with the effectiveness of intraarticular pain pumps in controlling postoperative pain [23, 26], this finding poses a concern for patients who receive bupivacaine pain pumps after shoulder procedures.
We report two patients who had chondrolysis develop after arthroscopy with use of bupivacaine pain pumps. All information documented was obtained from the respective patients’ medical records.
Case Reports
Patient 1
A 19-year-old National Collegiate Athletic Association (NCAA) Division I gymnast was seen at another hospital for right shoulder pain, subluxation, and instability. Based on her history and presentation, a diagnosis of anterior shoulder instability was made. An arthroscopic capsular plication of her right shoulder was performed. Intraoperative findings revealed intact glenoid and humeral head articular cartilage. According to the operative report, her superior, anterior, posterior, and inferior labrum was intact. A positive anterior drive-through sign was noted. An anterior capsular plication was performed. A bupivacaine pain pump was placed intraarticularly and her incisions were closed. The record contained no information on the flow rate.
She continued to have pain after her index capsular placation without a pain-free period. Additionally, she experienced substantial shoulder stiffness that did not resolve after surgery despite physical therapy and abstinence from gymnastics. Her pain was continuous, severe, and present at rest preventing her from sleeping at night and interfering with her academic work. She was seen at our institution approximately 1 year after her initial surgery. On presentation, she had substantial pain with all shoulder motion and was unable to participate in gymnastics. She had no gross instability but had restricted shoulder motion. Specifically, she had painful forward flexion to 95°, abduction to 50°, external rotation to 30°, and internal rotation to the lumbar region. Her Penn shoulder score [17] was 13 of 100.
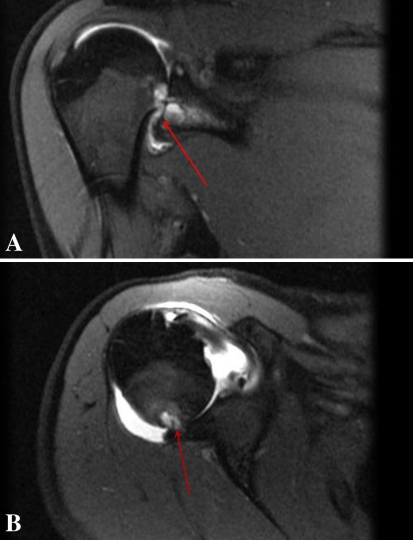
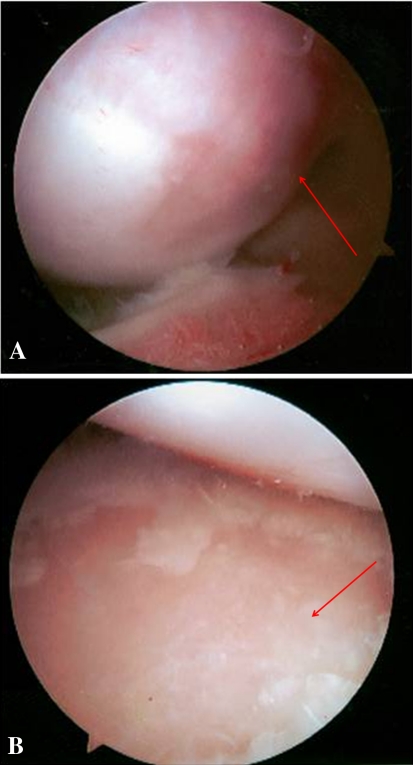
There were no radiographic studies available that postdated her index arthroscopic surgery. Plane radiographs obtained at our institution revealed early arthritic changes. An MR arthrogram of her shoulder revealed articular cartilage loss and subchondral cyst formation in the glenoid and humeral head (Fig. 1). To further evaluate the extent of chondral damage, she underwent a diagnostic arthroscopy of her shoulder. The humeral head (Fig. 2A) and glenoid surface (Fig. 2B) had focal cartilage defects in the central load-bearing area. Arthroscopic synovial biopsies showed no evidence of infection.
Fig. 1A–B.
(A) Coronal and (B) axial MR images of the left shoulder show chondrolysis with erosive changes of the glenoid and humeral head articular surfaces.
Fig. 2A–B.
Arthroscopic views from the posterior portal show chondral defects of the (A) humeral head and (B) glenoid.
Based on clinical presentation and radiographic and arthroscopic findings, she was treated with a hemicap right humeral resurfacing implant with a graft jacket interposition of the glenoid [8, 16]. At last followup, 18 months after reconstructive surgery, she had minimal pain at rest. On clinical examination, she had forward flexion to 130°, abduction to 100°, external rotation to 50°, and internal rotation to her thoracic level. Her Penn shoulder score was 66, and visual analog scale score for pain was 25 of 100. Her SF-36 [14, 28] physical functioning score was 85 of 100, general health average 80 of 100, and pain score 68 of 100 (100 being no pain). She had returned to competition in NCAA Division I gymnastics during her final year of college without difficulty.
Patient 2
A 26-year-old female childcare worker with a history of neurofibromatosis sustained a posterior glenoid labrum tear of her left shoulder while lifting some chairs at work. She was seen at an outside hospital and underwent a posterior glenoid labrum repair. A bupivacaine pain pump was placed for postoperative pain relief. Postoperatively, she had substantial shoulder pain and stiffness. The surgeon who performed her index surgery thought that her symptoms were related to postoperative adhesive capsulitis and therefore she underwent an arthroscopic débridement and capsular release. A bupivacaine pain pump again was placed after this second surgery. The record contained no information on the flow rate. She had no improvement in her symptoms and noted severe, constant pain in her shoulder at rest and with motion.
Twelve months after her initial surgery, she was seen at another tertiary center where an arthroscopic capsular release of her shoulder was planned. The treating surgeon documented advanced chondrolysis of the glenoid and humeral head articular surfaces and for this reason aborted the capsular release. Instead, this surgeon recommended reconstructive shoulder surgery as a more definitive treatment.
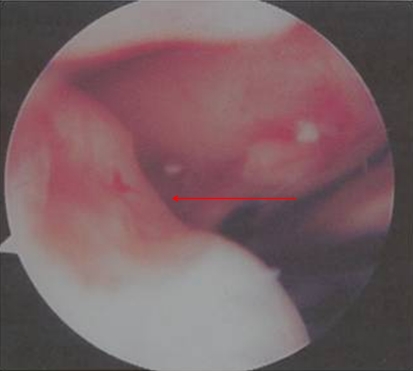
We saw the patient 1.5 years after her index surgery. On examination, she had limited active forward elevation to 90° with substantial pain. Abduction in the scapular plane was limited to 40°. She had external rotation to only 30° and internal rotation was limited to the sacrum. Her MR and arthroscopic images revealed chondrolysis of the humeral head and glenoid articular surfaces (Fig. 3). Given her young age and advanced arthritis, we performed a humeral head resurfacing and interposition arthroplasty of the glenoid with a graft jacket.
Fig. 3.
A chondral defect can be seen on the surface of the humeral head.
Sixteen months after shoulder arthroplasty, she had no pain at rest. She had passive forward flexion to 130°, passive abduction in the scapular plane to 80°, and passive neutral external rotation to 40°. She had good strength with internal and external rotation. She had returned to work full-time as a childcare provider, however she had difficulty reaching over shoulder height and had pain at the limits of her motion. Her Penn shoulder score was 38 of 100.
Discussion
The cause of chondrolysis is unknown, with various theories regarding its etiology. Some joints appear more prone to development of articular chondrolysis than others: chondrolysis is relatively common in the hip as compared with in smaller joints such as the shoulder or ankle [2]. Postarthroscopic chondrolysis has been reported in not only the shoulder but also the knee [6, 15, 27] and ankle [2].
van Huyssteen and Bracey [27] and Douw et al. [6] reported acute chondrolysis of the knee after arthroscopy involving accidental use of chlorhexidine. Douw et al. described three patients (four knees) who underwent knee arthroscopy; all their knees were accidentally irrigated with 1% aqueous chlorhexidine instead of plain saline. All three patients had chondrolysis of the knees and presented with increased knee pain and stiffness an average of 2.3 months after the index surgery [6].
Recently some authors have reported chondrolysis after bupivacaine administration via pain pump [12, 13, 24, 25]. In addition, various animal models and in vivo experiments have revealed acute chondrolysis after bupivacaine infusion [4, 9, 10]. Chu et al., using bovine knee models, compared articular cartilage damage after treatment with 0.5% bupivacaine compared with 0.9% saline [4]. Using flow cytometry to access chondrocyte viability for 1 week, they found greater than 99% chondrocyte death after bupivacaine treatment compared with 20% of cells treated with normal saline (p < 0.05) [4]. In another study Gomoll et al., using rabbit models, compared chondrocyte viability after infusion with bupivacaine with and without epinephrine compared with infusion with saline (all for 48 hours) [9]. They observed decreased chondrocyte viability in the samples treated with bupivacaine (p = 0.08) and bupivacaine with epinephrine (p = 0.02) compared with those treated with normal saline [9]. Gomoll et al. recently published their results of effects of bupivacaine on cartilage over a longer term than initial studies [10]. In this in vitro study, 36 rabbits were randomized in a control group (saline), bupivacaine group, or bupivacaine with epinephrine group. Their shoulders were infused with the respective solutions; they were sacrificed at 3 months. In contrast to previous studies, they did not note an increase in chondrocyte toxicity or cell death in the bupivacaine models after 3 months. In contrast, Gomoll et al. observed evidence of increased metabolism (proteoglycan synthesis) in the shoulders infused with bupivacaine; this increase was most notable in the bupivacaine with epinephrine group. They suggested the findings reflected a reparative process that occurs weeks after bupivacaine infusion [10]. More basic research is needed to provide more insight into these conflicting results.
Clinical reports of chondrolysis associated with pain pumps have been limited to the glenohumeral joint. Although commonly used in the treatment of knee disorders, there is no documented case of chondrolysis after use of pain pumps in the knees. Given most arthroscopic shoulder procedures using pain pumps are not complicated by chondrolysis [1, 3], other possible etiologies must be considered. Such possibilities include surgical and device placement techniques leading to chondral scuffing, use of intraarticular thermal devices, and a host predisposition for the development of chondrolysis, such as quality of native tissue, small size of the glenohumeral joint, and lack of joint fluid to dilute the bupivacaine or thinner shoulder articular cartilage compared with the knee [9].
Chondrolysis resulting after exposure to thermal and/or radiofrequency has been described [5, 11, 18, 21, 24]. Petty et al. [24] evaluated three cases of chondrolysis after shoulder arthroscopy, two of which involved the use of thermal energy. However, others have reported the occurrence of chondrolysis after arthroscopy without the use of thermal devices but with the use of pain pumps [12]. Hansen et al. [13] reported 10 patients (12 shoulders) who had chondrolysis develop received pain pumps for 48 hours; four of the patients had thermal devices used during the procedures. Neither of our patients had documentation of treatment with a thermal device.
For unclear reasons, chondrolysis associated with pain pumps and/or thermal device use tends to occur in younger females. Good et al. [11] reported that of the eight patients who had chondrolysis develop after thermal capsulorrhaphy, six were females and two were males with a mean age of 23 years for all patients. In the study by Hansen et al. [13], the average age of the patients was 28.9 years. The patients in our study were 20 and 26 years old and both were female.
With only two cases we cannot presume a direct cause and effect relationship between pain pumps and chondrolysis, only a possible association in keeping with other reports. In addition, we cannot be certain that our second patient did not have other predisposing factors or variables. It is possible that her chondrolysis was attributable to initial overtightening of the capsule during the labral repair. Furthermore it could have been caused by overtightening in the presence of the bupivacaine pain pump (decreasing the effective joint space).
Our cases add to the evidence of an association between pain pumps and glenohumeral chondrolysis. Additional research is necessary to understand why certain patients have chondrolysis develop and others do not. However, at this time, we do not encourage the use of pain pumps for shoulder cases.
Acknowledgments
We thank Norma Rendon BS, for help with the manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Barber FA, Herbert MA. The effectiveness of an anesthetic continuous-infusion device on postoperative pain control. Arthroscopy. 2002;18:76–81. doi: 10.1053/jars.2002.25976. [DOI] [PubMed] [Google Scholar]
- 2.Bojescul JA, Wilson G, Taylor DC. Idiopathic chondrolysis of the ankle. Arthroscopy. 2005;21:224–227. doi: 10.1016/j.arthro.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Busfield BT, Lee GH, Carrillo M, Ortega R, Kharrazi FD. Subacromial pain pump use with arthroscopic shoulder surgery: a short-term prospective study of complications in 583 patients. J Shoulder Elbow Surg. 2008;17:860–862. doi: 10.1016/j.jse.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Chu CR, Izzo NJ, Papas NE, Fu FH. In vitro exposure to 0.5% bupivacaine is cytotoxic to bovine articular chondrocytes. Arthroscopy. 2006;22:693–699. doi: 10.1016/j.arthro.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Coobs BR, LaPrade RF. Severe chondrolysis of the glenohumeral joint after shoulder thermal capsulorrhaphy. Am J Orthop. 2009;38:E34–E37. [PubMed] [Google Scholar]
- 6.Douw CM, Bulstra SK, Vandenbroucke J, Geesink RG, Vermeulen A. Clinical and pathological changes in the knee after accidental chlorhexidine irrigation during arthroscopy: case reports and review of the literature. J Bone Joint Surg Br. 1998;80:437–440. doi: 10.1302/0301-620X.80B3.8519. [DOI] [PubMed] [Google Scholar]
- 7.Eisenstein A, Rothschild S. Biochemical abnormalities in patients with slipped capital femoral epiphysis and chondrolysis. J Bone Joint Surg Am. 1976;58:459–467. [PubMed] [Google Scholar]
- 8.Elhassan B, Ozbaydar M, Diller D, Higgins LD, Warner JJ. Soft-tissue resurfacing of the glenoid in the treatment of glenohumeral arthritis in active patients less than fifty years old. J Bone Joint Surg Am. 2009;91:419–424. doi: 10.2106/JBJS.H.00318. [DOI] [PubMed] [Google Scholar]
- 9.Gomoll AH, Kang RW, Williams JM, Bach BR, Cole BJ. Chondrolysis after continuous intra-articular bupivacaine infusion: an experimental model investigating chondrotoxicity in the rabbit shoulder. Arthroscopy. 2006;22:813–819. doi: 10.1016/j.arthro.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Gomoll AH, Yanke AB, Kang RW, Chubinskaya S, Williams JM, Bach BR, Cole BJ. Long-term effects of bupivacaine on cartilage in a rabbit shoulder model. Am J Sports Med. 2009;37:72–77. doi: 10.1177/0363546508323748. [DOI] [PubMed] [Google Scholar]
- 11.Good CR, Shindle MK, Kelly BT, Wanich T, Warren RF. Glenohumeral chondrolysis after shoulder arthroscopy with thermal capsulorrhaphy. Arthroscopy. 2007;23:797.e1-5. [DOI] [PubMed]
- 12.Greis PE, Legrand A, Burks RT. Bilateral shoulder chondrolysis following arthroscopy: a report of two cases. J Bone Joint Surg Am. 2008;90:1338–1344. doi: 10.2106/JBJS.G.01004. [DOI] [PubMed] [Google Scholar]
- 13.Hansen BP, Beck CL, Beck EP, Townsley RW. Postarthroscopic glenohumeral chondrolysis. Am J Sports Med. 2007;35:1628–1634. doi: 10.1177/0363546507304136. [DOI] [PubMed] [Google Scholar]
- 14.Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med. 2001;33:350–357. doi: 10.3109/07853890109002089. [DOI] [PubMed] [Google Scholar]
- 15.Ishida K, Kuroda R, Sakai H, Doita M, Kurosaka M, Yoshiya S. Rapid chondrolysis after arthroscopic partial lateral meniscectomy in athletes: a case report. Knee Surg Sports Traumatol Arthrosc. 2006;14:1266–1269. doi: 10.1007/s00167-006-0091-0. [DOI] [PubMed] [Google Scholar]
- 16.Krishnan SG, Reineck JR, Nowinski RJ, Harrison D, Burkhead WZ. Humeral hemiarthroplasty with biologic resurfacing of the glenoid for glenohumeral arthritis: surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2, pt 1):9–19. doi: 10.2106/JBJS.G.01220. [DOI] [PubMed] [Google Scholar]
- 17.Leggin BG, Michener LA, Shaffer MA, Brenneman SK, Iannotti JP, Williams GR., Jr The Penn shoulder score: reliability and validity. J Orthop Sports Phys Ther. 2006;36:138–151. doi: 10.2519/jospt.2006.36.3.138. [DOI] [PubMed] [Google Scholar]
- 18.Levine WN, Clark AM, Jr, D’Alessandro DF, Yamaguchi K. Chondrolysis following arthroscopic thermal capsulorrhaphy to treat shoulder instability: a report of two cases. J Bone Joint Surg Am. 2005;87:616–621. doi: 10.2106/JBJS.D.02158. [DOI] [PubMed] [Google Scholar]
- 19.Lowe HG. Necrosis of articular cartilage after slipping of the capital femoral epiphysis: report of six cases with recovery. J Bone Joint Surg Br. 1970;52:108–118. [PubMed] [Google Scholar]
- 20.Lubicky JP. Chondrolysis and avascular necrosis: complications of slipped capital femoral epiphysis. J Pediatr Orthop B. 1996;5:162–167. doi: 10.1097/01202412-199605030-00005. [DOI] [PubMed] [Google Scholar]
- 21.Lubowitz JH, Poehling GG. Glenohumeral thermal capsulorrhaphy is not recommended: shoulder chondrolysis requires additional research. Arthroscopy. 2007;23:687. doi: 10.1016/j.arthro.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Nakagawa Y, Ueo T, Miki T, Kotani H, Onishi E, Nakamura T. Glenohumeral osteoarthritis following a “color test” during rotator cuff repair: a case report and a review of the literature. Bull Hosp Jt Dis. 1998;57:216–218. [PubMed] [Google Scholar]
- 23.Park JY, Lee GW, Kim Y, Yoo MJ. The efficacy of continuous intrabursal infusion with morphine and bupivacaine for postoperative analgesia after subacromial arthroscopy. Reg Anesth Pain Med. 2002;27:145–149. doi: 10.1053/rapm.2002.31209. [DOI] [PubMed] [Google Scholar]
- 24.Petty DH, Jazrawi LM, Estrada LS, Andrews JR. Glenohumeral chondrolysis after shoulder arthroscopy: case reports and review of the literature. Am J Sports Med. 2004;32:509–515. doi: 10.1177/0363546503262176. [DOI] [PubMed] [Google Scholar]
- 25.Piper SL, Kim HT. Comparison of ropivacaine and bupivacaine toxicity in human articular chondrocytes. J Bone Joint Surg Am. 2008;90:986–991. doi: 10.2106/JBJS.G.01033. [DOI] [PubMed] [Google Scholar]
- 26.Savoie FH, Field LD, Jenkins RN, Mallon WJ, Phelps RA., II The pain control infusion pump for postoperative pain control in shoulder surgery. Arthroscopy. 2000;16:339–342. doi: 10.1016/S0749-8063(00)90076-8. [DOI] [PubMed] [Google Scholar]
- 27.Huyssteen AL, Bracey DJ. Chlorhexidine and chondrolysis in the knee. J Bone Joint Surg Br. 1999;81:995–996. doi: 10.1302/0301-620X.81B6.9719. [DOI] [PubMed] [Google Scholar]
- 28.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Wilson PD, Jacobs B, Schecter L. Slipped capital femoral epiphysis: an end-result study. J Bone Joint Surg Am. 1965;47:1128–1145. [PubMed] [Google Scholar]
- 30.Yarbrough R, Gross R. Chondrolysis: an update. J Pediatr Orthop. 2005;25:702–704. doi: 10.1097/01.bpo.0000174379.65969.51. [DOI] [PubMed] [Google Scholar]