Abstract
A 38-year-old Iranian woman was found to have a huge ovarian cystic mass. Her presenting symptom was vague abdominal pain and severe abdominal distention. She underwent laparotomy and after surgical removal, the mass was found to be mucinous cystadenoma on histology.
Key Words: Mucinous cystadenoma, Abdominal masses, Abdominal distention, Ovarian cysts, Ovarian tumors
Introduction
Ovarian cysts rarely grow immense. Ultrasonography scanning permits early detection and appropriate treatment. Occasionally, ovarian cysts reach enormous dimensions without raising any symptom. A few cases of giant ovarian cysts have been sporadically reported in the literature [1,2,3,4].
Case Presentation
The patient is a 38-year-old Iranian married and multiparous female who presented at our surgical department with a gradually increasing abdominal swelling first noticed 1 year ago. The swelling was accompanied by vague abdominal pain since 6 months before admission. There was no history of colicky pain, fainting attacks, vomiting or other gastrointestinal attacks. She had no previous history of any illnesses, allergies or operations. She is P5L4D4, has been married for 20 years and had normal regular menses. Based on sonographic examinations, a huge abdominal cystic mass that occupied all of the abdomen and pelvic cavity was noted. On general examination, she was slim and undernourished. She weighed 52 kg. Pallor was present and vital signs were normal. There was no icterus, edema, or lymphadenopathy. Abdominal examination showed general distension (fig. 1). The liver and spleen were not palpable. Percussion note was dull all over the abdomen with positive fluid thrill. Abdominal bowel sounds were heard normally. Vaginal examination showed only cystocele grade 1. Hemoglobin was 11 g/dl, and other hematological or biochemical serum tests were normal. Chest X-ray was normal.
Fig. 1.
Generalized distension of the abdomen is evident.
Abdominal ultrasonography was suggestive of a huge abdominal cystic mass. Uterus was normal and seen separate from the mass. Abdominal organs were compressed by the mass, and a mild right hydronephrosis was seen. Abdominopelvic computerized tomography (CT) findings were consistent with a large abdominopelvic cystic mass (fig. 2). The patient underwent laparotomy with a low midline incision, extending up to the umbilicus. After opening the layers, a large tense, smooth surfaced cystic mass was noted (fig. 3). The mass was so large that it could not be excised without a large abdominal incision, so we drained the intra-cystic fluid with creation of a small hole in the mass, and 6 liters of clear fluid were drained, until we could excise the cyst with its remaining fluid (fig. 4). The cyst measured 65 × 45 × 35 cm, extended up to the undersurface of the diaphragm, and totally weighted 12 kg. The mass originated from the right ovarian region. So we excised the cyst with the ipsilateral fallopian tube and ovary. The right ovary was included in the mass. The right fallopian tube was adherent to the surface of the cyst. There was no free fluid in the abdomen. Pathology confirmed serous cystadenoma of the ovary. The postoperative period was uneventful and the patient was discharged on the fourth day after operation. After 3 months, in order to decrease the possibility of recurrence and malignant transformation, total abdominal hysterectomy with left salpingo-oophorectomy was performed. The patient has been regularly followed up for a period of 1 year, and she has remained healthy with no recurrence of the disease.
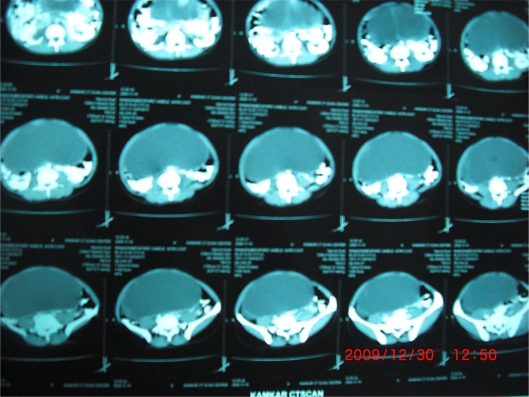
Fig. 2.
Abdominopelvic CT scan of the patient.
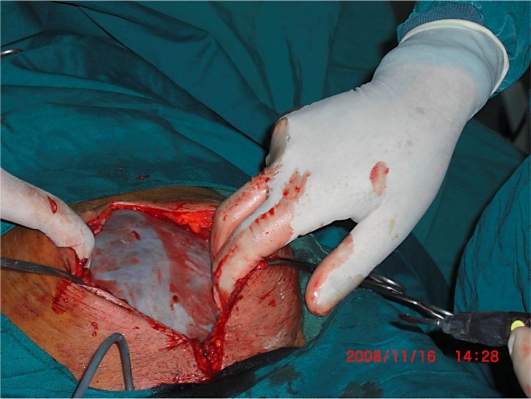
Fig. 3.
The mass just after opening of the abdominal layers.
Fig. 4.
The excised mass after draining 6 liters of fluid.
Written informed consent was obtained from the patient for publication of this case report.
Discussion
Mucinous cystadenomas (MCAs) of the ovary are known for their potential to grow to massive proportions and are often incidentally diagnosed. They are typically benign tumors accounting for 15% of ovarian neoplasms and up to 80% of all mucinous tumors [5]. Ovarian MCAs are characteristically unilateral, only 5% presenting bilaterally, and the peak incidence occurs among women who are between 30 and 50 years of age [6]. Ovarian neoplasms may be divided according to original cell types into 3 main groups: epithelial, stromal, and germ cell. Taken as a group, the epithelial tumors are by far the most common type. The single most common benign ovarian neoplasm is the benign cystic teratoma; however, according to some studies, it is serous cystadenoma. The most common types of epithelial neoplasms encountered were benign cystadenoma, of which 75% were serous cystadenomas and 25% were MCAs. Mucinous tumors of the ovary occur principally in middle adult life and are extremely rare prior to menarche. The histopathological groups of mucinous tumors are described as follows: (1) MCA, (2) mucinous tumor of uncertain malignant potential (borderline), and (3) mucinous carcinoma [7]. MCA appears as a large cystic mass, is often multiloculate, and contains sticky gelatinous fluid. Microscopically, the tumor consists of cystic spaces lined by tall columnar epithelium with mucinous differentiation. In general, ovarian MCAs tend to present with abdominal distention. The vast majority of mucinous tumors are benign (75%), 10% borderline, and 15% carcinomas [8]. One of the major differential diagnoses of ovarian cysts are omental cysts. Omental cysts occur in all age groups, but most often they present in children and young adults [9]. These masses may be simple or multiple, may be huge, and simulating ascites. Ascites is another entity that must be included in the list of differential diagnoses. Other diagnoses may be mesenteric cysts, cysts arising from retroperitoneal structures like pancreatic pseudocysts, urinary retention, bladder diverticulum, hydronephrosis, cystic lymphangiomas, choledochal cysts, splenic cysts, multicystic dysplastic kidney, gastrointestinal duplication cysts and large uterine tumors [10,11,12,13,14,15,16]. Management of ovarian cysts depends on the patient's age, the size and structure of the cyst and menopausal status [17]. Surgical management of cysts is by laparotomic or laparoscopic cyst excision or cystectomy with oophorectomy.
Conclusion
There has been no report of a mass of this weight in our institution before, and it is one of the largest tumors reported in Iran in the literature.
References
- 1.Menahem S, Shvartzman P. Giant ovarian cyst mimicking ascites. J Fam Pract. 1994;39:479–481. [PubMed] [Google Scholar]
- 2.Lombardo L, Babando GM. Giant ovarian cyst mimicking ascites. Gastrointest Endoc. 1986;32:245–246. doi: 10.1016/s0016-5107(86)71829-4. [DOI] [PubMed] [Google Scholar]
- 3.Farinetti A, Butazzi A, Tazzioli G, Saviano L, Saviano M. Giant ovarian cyst. A case weighing 23 kg. Literature review. Minerva Chir. 2003;58:261–265. [PubMed] [Google Scholar]
- 4.Hunter DJ. Management of massive ovarian cyst. Obstet Gynecol. 1980;56:254–255. [PubMed] [Google Scholar]
- 5.Malakan AD, Singh-Braich P, Dudrick SJ. Mucinous cystadenoma of the ovary presenting as unilateral lower extremity edema. Conn Med. 2009;73:517–519. [PubMed] [Google Scholar]
- 6.Hart WR. Mucinous tumors of the ovary: a review. Int J Gynecol Pathol. 2005;24:4–25. [PubMed] [Google Scholar]
- 7.Sri Paran T, Mortell A, Devaney D. Mucinous cystadenoma of the ovary in perimenarchal girls. Pediatr Surg Int. 2006;22:224. doi: 10.1007/s00383-005-1624-1. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez IM, Part J. Mucinous tumors of the ovary. A clinicopathologic analysis of 75 borderline tumors (of intestinal type) and carcinomas. Am J Surg Pathol. 2002;26:139. doi: 10.1097/00000478-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Walker AR, Putham TC. Omental, mesenteric and retroperitoneal cyst. A clinical study of 33 new cases. Ann Surg. 1973;178:13–19. doi: 10.1097/00000658-197307000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Semchyshyn S, Strickler RC, Gerulath AH. Giant ovarian cyst in a dwarf. Can J Surg. 1977;20:153–155. [PubMed] [Google Scholar]
- 11.Zanini P, Cavalca A, Benatti E, Drei B. Benign giant ovarian cystadenoma. Description of a clinical case. Minerva Ginecol. 1996;48:215–219. [PubMed] [Google Scholar]
- 12.Rattan KN, Budhiraja S, Pandit SK, Yadav RK. Huge omental cyst mimicking ascites. Indian J Pediatr. 1996;63:707–708. doi: 10.1007/BF02730829. [DOI] [PubMed] [Google Scholar]
- 13.Zamir D, Yuchtman M, Amar M, Shoemo U, Weiner P. Giant mesenteric cyst mimicking ascites. Harefuah. 1996;130:683–684. [PubMed] [Google Scholar]
- 14.Chen SS. A large retroperitoneal cyst mimicking ascites. A case report. J Reprod Med. 1979;22:261–263. [PubMed] [Google Scholar]
- 15.Grobe JL, Kozarek RA, Sanowski RA, Earnest DL. ‘Pseudo-ascites’ associated with giant ovarian cysts and elevated cystic fluid amylase. Am J Gastroenterol. 1983;78:421–424. [PubMed] [Google Scholar]
- 16.Wootton-Gorges SL, Thomas KB, Harned RK, Wu SR, Stein-Wexler R, Strain JD. Giant cystic abdominal masses in children. Pediatr Radiol. 2005;35:1277–1288. doi: 10.1007/s00247-005-1559-7. [DOI] [PubMed] [Google Scholar]
- 17.Ishioka S, Sagae S, Ito E, Kudo R. Ultrastructural study of benign, low-malignant potential (LMP), and malignant ovarian tumors. Med Electron Microsc. 2004;37:37–44. doi: 10.1007/s00795-003-0189-0. [DOI] [PubMed] [Google Scholar]