Abstract
Objective
To evaluate the roles of spouse- versus self-rated health as predictors of all cause mortality among older adults over the age of 50.
Design
Cross sectional and longitudinal data from 2000 through 2006.
Setting
The Health and Retirement Study (HRS) is a national sample of Americans over the age of 50 and their spouses.
Participants and Measurements
673 dyads of married couples randomly selected to participate in an HRS module examining spouse-rated health. For each couple, one member was asked to rate his or her overall health status, and his or her spouse was asked to report their partner's overall health status. Mortality data were available through the year 2006.
Results
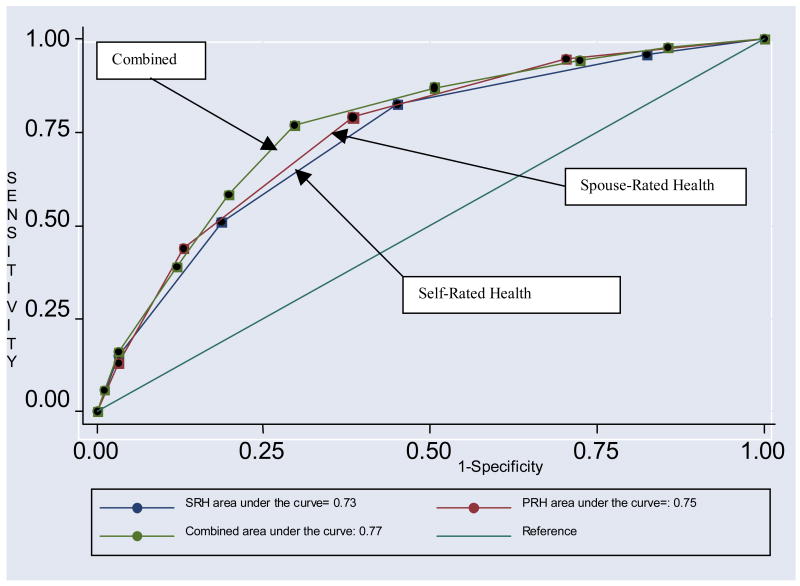
Our findings demonstrate that spouse-rated health (area under the curve=.75) is as strong a predictor of mortality status as self-rated health (area under the curve=.73; chiˆ2[1]=.36, p=.54). Combining spouse- and self-rated health together predicts mortality better than self-rated health alone (area under the curve=.77; chiˆ2[1]=6.72, p=.009).
Conclusions
Spouse ratings of health are at least as strongly predictive of mortality as self-rated health. This suggests that when self-rated health is used as a prognostic indicator, spouse ratings can be used when self-ratings are unavailable. Both measures together may be more informative than either measure alone.
Keywords: epidemiology, mortality risk, proxy, concordance, prognostic indicators
Introduction
There is ample research demonstrating that self-rated health is an excellent predictor of mortality that often outperforms objective indicators of health and mental health status 1. Even after controlling for age, sex, and other demographic variables, the predictive power of self-rated health remains stable over time 1, 2. To account for the strong predictive value of self-rated health, it has been hypothesized that self-rated health either measures health status data that cannot be captured by existing technology, such as respondents' inner biological and physiological health processes or serves as a self fulfilling prophecy 1, 3. Others have suggested that maintaining positive health habits leads one to perceive his or her health more positively than expected based on objective measures alone or that optimism, as manifested in a more positive self-rated health is beneficial in itself. Finally, self-rated health has also been proposed as a proxy of emotional status, such as depression or other emotional problems, which are known to account for mortality 2.
To date, there has been no research on the utility of spouse-rated health as a predictor of all cause mortality. Nonetheless, it is possible that the way individuals perceive the health of their spouse is also of prognostic value. Only one study has evaluated the utility of proxy report against mortality data. This study found that after adjustment for health and sociodemographic data, spouse rated limitations and life expectancy were predictive of husbands' mortality, but not of wives' mortality, arguing that wives are more astute judges of their husbands' mortality risk than the other way around 4.
The majority of research concerning proxy reports has, instead, focused on concordance between proxy and respondent with regard to reports of quality of life 5-11 and activities of daily living 12-14. These studies have shown that degree of concordance between proxy and respondent is moderate at best, with proxies tending to view respondents' quality of life as lower and functional impairment as greater than respondents do 5, 7, 15. Only a small fraction of these studies has also evaluated proxy-respondent concordance concerning medical status, with most12, 14, 15, but not all 16, studies reporting a reasonable agreement.
The present study evaluates spouse- versus respondent-reports of health status as predictors of mortality amongst older adults over the age of 50. Given past research on degree of concordance between respondent and proxy; we expected to find moderate agreement with regard to respondent's health status. We further expected spouse-rated health to capture not only self-rated health, but also other sociodemographic and clinical characteristics of both respondent and spouse. Finally, we expected both self-rated health and spouse-rated health to serve as independent risk factors for respondents' mortality.
Methods
The Health and Retirement Study (HRS) is a nationally representative sample of individuals 50 years and older living in the United States 17. The HRS is sponsored by the National Institute of Aging and is conducted by the University of Michigan. The study is reviewed and approved by the University of Michigan's Health Sciences IRB. Participants take part in a biennial interview that covers a range of topics including income, wealth, work, retirement, health, health care utilization, etc. Most interviews are conducted over the phone.
Baseline data for the present study were collected in the year 2000. Overall, 18,167 individuals responded to the 2002 HRS questionnaire. In addition to the core interview, each wave of the HRS includes additional modules on selected topics that are administered to randomly selected participants. Randomization is computerized and is conducted by the University of Michigan. The potential analytic sample for this study was the 3,008 participants who were randomly selected to participate in a module designed to evaluate feelings of loneliness using three items selected from the UCLA-Loneliness Scale based on their ???.
Measures
Outcome Variable
Mortality
Mortality status (alive/dead) was available through the year 2006 based on HRS tracking efforts. Respondents were classified by HRS into 1 of 5 categories: a) alive in 2006; b) presumed alive as of 2006; c) death reported in 2006; d) death reported in past waves; e) vital status unknown. In the present study, the first two categories were collapsed as alive, the next two categories were collapsed as dead and the latter category was classified as missing (1.1% of the sample).
Predictors
Spouse-rated health
Proxies were asked to rate the health status of their spouse on a five-point scale (recoded as excellent=5, very good=4, good=3, fair=2, poor=1).
Self-rated health
All participants were asked to rate their own health status on a five-point scale (excellent=5 through poor=1).
Covariates
Medical Status
Number of chronic medical conditions out of six common conditions (e.g., cancer, diabetes, stroke) was gathered based on self-report. We dichotomized subjects into those with 0-1 medical conditions versus >1 conditions.
Functional Impairments
Participants were asked to indicate the presence or absence of impairments in 9 activities (e.g., difficulties stooping, difficulties sitting). Participants were then asked whether they provide assistance with activities of daily living/instrumental activities of daily living (ADL/IADL) to their spouse.
Depression
The CES-D is a common measure of depressive symptomatology that has been used in a variety of population-based studies 18. The HRS uses 8 items from the CES-D. A cutoff of 3 and higher was used to represent depression 19. However, it is important to note that this is only a measure of depressive symptomatology and not of clinical depression.
Cognitive Functioning
We used the HRS cognitive scale, a test of overall cognitive functioning that includes subtests of immediate- and delayed word recall, subtraction, and backward count. The tests were modeled after the Mini-Mental Status Exam, a standard geriatric dementia screen 20, 21. Because scores are highly correlated with each other, we used a composite score ranging from 0 to 26, with 26 representing perfect performance.
Health Behaviors
Participants were asked whether they participate in any vigorous physical activity (yes/no), smoke cigarettes (yes/no), or drink alcohol (yes/no).
Sociodemographic Data
Age (<65, 65-74, 75+), gender, education (0-12, 13+), and ethnicity (White, Black, Latino, other) were gathered based on self-report.
Statistical Analysis
We conducted chi-square analyses to compare spouses and respondents on a variety of categorical demographic and clinical characteristics. T-test analyses for dependent samples were conducted to compare the two parties on continuous variables. We also used Wilcoxon signed-rank test to compare spouses' and respondents' reports of health status 22. We then evaluated the degree of concordance between spouse-rated health (of respondent) and self-rated health, using chi-square analysis and the weighted kappa statistic 23, employing a linear set of weights (e.g., 1 .75 .5 .25 0). The Kappa statistic examines the degree of agreement beyond what would occur by chance. A kappa statistic of 0 indicates that the level of agreement is no more than would be expected by chance alone, while a Kappa statistic of 1.0 indicates a perfect agreement. Next, we identified the unique association of the various covariates with spouse-rated health, over and above its associations with self-rated health. We first assured all variables complied with the proportional odds assumption and then conducted a series of proportional odds regression analyses with spouse-rated health as an outcome variable, each sociodemographic and clinical correlate as a potential predictor, and self-rated health as a control variable. We then conducted logistic regression analyses comparing self-rated health to spouse-rated health as potential predictors of mortality status. We repeated the same logistic regression analyses while adjusting for a variety of demographic and clinical characteristics (e.g., respondents' age, gender, education, medical status, functional impairment, depression, cognitive status, physical activity, smoking, alcohol drinking, and cognitive functioning as well as for spouse's depression, cognitive status, and caregiving status). Finally, we calculated receiver-operating curves (ROC) 24, to compare the predictive ability of spouse-rated health against self-rated health as well as their combined predictive ability (i.e., a sum of both health ratings) 25, 26. An area under the curve of 1.0 represents perfect predictive ability, whereas an area of .5 represents worthless predictive ability. The statistical comparison between the two curves was conducted using the roccomp command in STATA, which relies on logistic models for estimating the curves26.
Results
Overall 673 dyads participated in this analysis. The majority of spouses were female (54%). The majority of both spouses and respondents were White (87%, 86%; respectively). See Table 1. Whereas differences between respondents and spouses were statistically significant for some characteristics, in most cases, the magnitude of the difference was small.
Table 1. Demographic and Clinical Characteristics of the Sample1.
| Spouse (n=672) |
Respondent (n=672) |
p-value | |
|---|---|---|---|
| Age | <.001 | ||
| <65 | 369(54.9%) | 349(51.9%) | |
| 65-74 | 200(29.8%) | 201(29.9%) | |
| 75+ | 103(15.3%) | 122(18.2%) | |
| Gender | <.001 | ||
| Female | 367(54.0%) | 305(45.3%) | |
| Education | <.001 | ||
| 13+ | 278(41.3%) | 297(44.1%) | |
| Ethnicity | <.001 | ||
| White | 564(83.9%) | 554(82.4%) | |
| Latino | 46(6.8%) | 52(7.7%) | |
| Black | 49(7.3%) | 51(7.6%) | |
| Other | 13(1.7%) | 15(2.2%) | |
| Medical Conditions | .09 | ||
| >2 | 175(22.9%) | 191(25.7%) | |
| Functional Impairment (0-9) | 1.71(.11) | 1.77(.09) | .66 |
| Providing Assistance with ADL/IADL to Partner | .78 | ||
| Yes | 50(6.6%) | 57(7.8%) | |
| Depression | <.001 | ||
| Depressed | 137(19.9%) | 152(22.5%) | |
| Cognitive Status (0-26) | 14.60(.25) | 14.08(.19) | .11 |
| Vigorous Exercise | <.001 | ||
| Yes | 297(44.5%) | 310(48.9%) | |
| Smoking Cigarettes | <.001 | ||
| Yes | 96(15.6%) | 88(14.0%) | |
| Drinking Alcohol | <.001 | ||
| Yes | 96(15.6%) | 88(14.0%) | |
| Self Rated Health2 | <.001 | ||
| Poor | 35(3.5%) | 40(4.9%) | |
| Fair | 101(13.5%) | 108(15.5%) | |
| Good | 203(32.3%) | 204(29.3) | |
| Very Good | 228(34.0%) | 219(35.4) | |
| Excellent | 94(16.5%) | 89(14.5) | |
Chi-square analyses were conducted to compare spouse to respondent on categorical variables. T-test analyses for dependent samples were conducted to compare spouse to respondent on continuous variables.
For spouse, refers to their own health
As can be seen in Table 2, degree of concordance between spouse-rated health and respondent self-rated health was moderate, weighted kappa=.48, p<.001. This suggests the level of agreement between respondents and spouses was about the midpoint between being no better than chance and perfect. Wilcoxon signed-rank test showed that spouses tended to rate respondents' health (Mean [SD=.05] =3.22[.05]) slightly worse than respondents did (Mean [SD] = 3.37[.05]; z=4.3, p<.001).
Table 2. Self- versus Spouse-Rated Health1.
| Spouse-rated health | Total | ||||||
|---|---|---|---|---|---|---|---|
| Poor | Fair | Good | Very Good | Excellent | |||
| Self-rated health | Poor | 27 | 9 | 4 | 0 | 0 | 40(4.9%) |
| Fair | 22 | 51 | 30 | 3 | 2 | 108(15.5%) | |
| Good | 6 | 44 | 96 | 45 | 13 | 204(29.3%) | |
| Very Good | 1 | 14 | 71 | 105 | 28 | 219(35.5%) | |
| Excellent | 1 | 0 | 20 | 34 | 34 | 89(15.5%) | |
| Total | 57(7.0%) | 118(17.2%) | 221(32.4%) | 187(32.0%) | 77(11.2%) | 660 | |
Weighted Kappa was calculated to evaluate the degree concordance between spouse and respondent. To identify differences between spouse and respondent, chi-square analysis was conducted. Weighted Kappa=.48, p<.001; Chi-square[16]=461.8, p<.001
Correlates of spouse-rated health after controlling for self-rated health
Employing a p<.01 as a criterion for statistical significance in order to account for the large sample size and the multiple comparisons 27, all variables met the proportional odds assumption. In a series of proportional odds regression analyses, we found several respondents'- and spouses'- level variables to be associated with spouse-rated health even after controlling for self-rated health; respondents' of younger age, of better education, of fewer medical conditions, of better cognitive functioning, of less functional impairments, and those who engaged in physical activity were more likely to be rated by their spouse as enjoying better health. In addition, non-depressed spouses and spouses of better cognitive functioning also were more likely to rate their partner's health as better, unrelated to their partner's self-rated health. Hence, these various demographic and clinical characteristics of both respondent and spouse contribute to spouse perception of respondent's health even after respondent's self-rated health is taken into consideration.
Spouse-rated health versus self-rated health as predictors of mortality status
Overall, 94 (12.3%) respondents died over the 6-year period. As can be seen in table 3, using logistic regression analysis, better self-rated health is associated with lower mortality risk (F [4,47]=12.5, p<.001). Similar results were obtained for spouse-rated health (F [4,47]=18.0, p<.001). Both self- and spouse-rated health remained significant predictors of mortality even after adjusting for a variety of demographic and clinical characteristics (e.g., respondents' age, gender, education, medical status, functional impairment, depression, cognitive status, health behaviors, and cognitive functioning as well as for spouse's depression, cognitive status, and caregiving status).
Table 3. Correlates of Spouse-rated health after Adjustment for Self-rated health1.
| OR | 95% CI | |
|---|---|---|
| Age | ||
| <65 (reference) | ||
| 65-74 | .63 | .44-.92 |
| 75+ | .50 | .31-.79 |
| Gender | ||
| Male (reference) | ||
| Female | 1.11 | .79-1.54 |
| Education | ||
| 0-12 (reference) | ||
| 13+ | 1.67 | 1.17-2.37 |
| Medical Conditions | ||
| 0-1 (reference) | ||
| >2 | .53 | .38-.74 |
| Functional Impairment | .76 | .67-.82 |
| Depression | ||
| Not Depressed (reference) | ||
| Depressed | .68 | .44-1.06 |
| Vigorous Exercise | ||
| No (reference) | ||
| Yes | 1.47 | 1.07-2.03 |
| Smoking Cigarettes | ||
| No (reference) | ||
| Yes | .79 | .52-1.20 |
| Drinking Alcohol | ||
| No (reference) | ||
| Yes | .79 | .52-1.20 |
| Cognitive Status | 1.05 | 1.02-1.08 |
| Spouse's Depression | ||
| Not Depressed (reference) | ||
| Depressed | .43 | .28-.64 |
| Spouse's Cognitive Status | 1.06 | 1.02-1.10 |
| Providing Assistance with ADL/IADL to Respondent | ||
| No (reference) | ||
| Yes | .69 | .32-1.46 |
A series of proportional odds regressions, with spouse-rated health as an outcome and self-rated health of respondent as a control variable were conducted to identify correlates of spouse-rated health.
Areas under the curve indicated moderate predictive ability for both self-rated and spouse-rated health. The area under the curve of spouse-rated health (.75) was not significantly better than the area under the curve of respondent-rated health (.73; chiˆ2[1] =.36, p=.54). Combining self-rated health and spouse-rated health provided the best predictive value (area under the cure= .77), which was significantly better than self-rated health alone (Chiˆ2[1] =6.72, p=.01), but not significantly better than spouse-rated health alone (Chiˆ2 [1] =2.91, p=.08). See Figure 1.
Figure 1. Receiver Operating Characteristics (ROC) Comparing Self-, Spouse-, and Combined- Rated Health as Predictors of Mortality Status1.
1 For this analysis, spouse and self-rated health were recoded accordingly: (1=excellent)(2=very good)(3=good)(4=fair)(5=poor). Self-rated health vs. spouse-rated health: chiˆ2[1]=.36, p=.54; self rated health vs. combined: chiˆ2[1]=6.72, p=.01; spouse-rated health vs. combined: chiˆ2[1]=2.91, p=.08
Discussion
To date, many studies have evaluated the role of self-rated health as a predictor of all-cause mortality and its predictive ability has been demonstrated in a variety of epidemiological studies 1, 2, 28-30. This is the first study, however, to show that among older adults, spouse-rated health is as predictive of respondent mortality as self-rated health is. This is despite the fact that the two are not synonymous. Our findings indicate only moderate levels of concordance between self-rated health and spouse-rated health. Further, the study demonstrates that spouse-rated health is correlated with other respondent- and spouse- level variables in addition to self-rated health; spouse-rated health captures respondents' medical status, demographic characteristics, cognitive status, health behaviors, and mental status. As has been demonstrated in past research 31, it also is correlated with proxies' cognitive status and mental status; so that more depressed or cognitively impaired proxies tend to report their spouse's health lower, even after controlling for self-rated health.
Similarly to the case of self-rated health, however, it still remains unclear what accounts for the strong predictive value of spouse-rated health. Are spouses more attuned to certain biological and physiological processes in their partner that remain otherwise unnoticed? Is it the mental condition of the spouse that has such an important impact on respondent mortality prospects? Or is it the relationship between the two partners and the expectations that spouses hold regarding their partner that impact their partner's mortality prospects? At this point, the exact mechanism behind the predictive ability of spouse-rated health remains unclear. Nonetheless, our study shows that combining self-rated health with spouse-rated health provides a better prognostic indicator of all cause mortality than self-rated health alone.
The present study has several limitations that should be acknowledged. First, the study was limited to married couples. Research has shown that the quality of the relationship between proxy and respondent plays a major role in determining degree of concordance between respondent- and proxy-rated variables 8. Hence, the present results may not be generalized to other types of proxies. Further, the HRS is a representative sample of individuals over 50, hence, results may not be representative of individuals younger than 50. Second, the study was limited to cognitively intact proxies and respondents. Thus, results cannot be generalized to cognitively impaired participants. Third, no blinding measures were in place and it is possible that spouses were present during their partner's interview. While we can't be sure how this might have impacted the results, we think it is unlikely it had a major impact. The administration of the HRS interview takes a fairly long time, and many of the questions have similar response choices. While a spouse may have heard their partner providing answers, it is unlikely they would have known which specific question was being answered. Perhaps more importantly, our results emphasize that spouse ratings of health are often discordant. As a result, any bias resulting from awareness of partner response would bias our results towards the null, suggesting that our results are even more conservative. Fourth, it is important to note that the study did not evaluate the predictive ability of spouse-rated health for other purposes other than mortality. Finally, we acknowledge that there are no standards for how to recognize the clinical significance of differences in ROC curves. However, many would view the ROC difference of .04 (self-rated health compared to combined self-spouse-rated health) as clinically meaningful. Consider a situation where you have pairs of patients, one of whom survived longer than the other. Using self-rated health only, you would correctly identify the longer surviving patient 73% of the time. Using the combined self-spouse-rated health model, you would correctly identify the longer surviving patient 77% of the time. We believe this is meaningful, and that most would choose to incorporate both self- and spouse- rated health based on this information.
Nonetheless, this is the first study to evaluate the role of spouse-rated health as a predictor of mortality status. Our findings demonstrate that spouse-rated health is at least as strong a predictor of mortality status as self-rated health, even though the two measure different things; spouse-rated health is correlated not only with self-rated health, but also captures the sociodemographic and medical status of respondents, as well as spouses' own cognitive and mental status. Spouse-rated health can be used as a predictor of mortality either when self-rated health is unavailable, or as an additional source of data that complements self-rated health. Health care practitioners working with older adults may attempt to obtain not only patients' self-report of their health status, but when available also their spousal reports as the combination of spouse-self-rated health provides a more accurate estimate of respondents' mortality risk.
Table 4. Self-rated health versus Spouse-rated health as Predictors of Mortality Status1.
| Overall Incidence | Unadjusted OR | 95% CI | Adjusted OR2 | 95% CI | |
|---|---|---|---|---|---|
| Self-rated health3 | |||||
| Poor | 16(36.1%) | ||||
| Fair | 34(29.4%) | .72 | .30-1.76 | 1.06 | .32-3.48 |
| Good | 24(11.0%) | .22 | .09-.48 | .37 | .12-1.16 |
| Very Good | 14(5.3%) | .09 | .03-.25 | .25 | .07-.87 |
| Excellent | 3(2.3%) | .04 | .009-.18 | .16 | .03-.86 |
| Spouse-rated health4 | |||||
| Poor | 28(45.6%) | ||||
| Fair | 30(25.0%) | .39 | .19-.79 | .45 | .14-1.44 |
| Good | 23(9.7%) | .12 | .06-.23 | .31 | .09-1.02 |
| Very Good | 9(3.6%) | .04 | .01-.12 | .12 | .02-.59 |
| Excellent | 4(3.6%) | .04 | .01-.16 | .17 | .03-.81 |
Logistic regression analyses were conducted to identify the role of self-rated health vs. spouse-rated health as predictors of mortality status.
Logistic regression analyses were conducted to identify the role of self-rated health vs. spouse-rated health as predictors of mortality status after adjusting for respondents' age, gender, education, medical status, functional impairment, depression, cognitive status, exercise, smoking, alcohol drinking, and cognitive functioning as well as for spouse's depression, cognitive status, and caregiving status.
Unadjusted model F[4,47]=12.5, p<.001; Adjusted model F[18,33]=7.06, p<.001
Unadjusted model F[4,47]=18.0, p<.001; Adjusted model F[18,33]=7.35, P<.001
Acknowledgments
Dr. Covinsky was supported by grants 5K24AG029812 and 5R01AG023626 from the National Institute on Aging.
References
- 1.Strawbridge WJ, Wallhagen MI. Self-Rated Health and Mortality Over Three Decades: Results from a Time-Dependent Covariate Analysis. Research on Aging. 1999 May 1;21(3):402–416. [Google Scholar]
- 2.Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982 Aug;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel M, Bradley EH, Kasl SV. Self-rated life expectancy as a predictor of mortality: evidence from the HRS and AHEAD surveys. Gerontology. 2003 Jul-Aug;49(4):265–271. doi: 10.1159/000070409. [DOI] [PubMed] [Google Scholar]
- 4.van Doorn C. Spouse-rated limitations and spouse-rated life expectancy as mortality predictors. J Gerontol B Psychol Sci Soc Sci. 1998 May 1;53(3):S137–143. doi: 10.1093/geronb/53b.3.s137. [DOI] [PubMed] [Google Scholar]
- 5.Ball AE, Russell EM, Seymour DG, Primrose WR, Garratt AM. Problems in using health survey questionnaires in older patients with physical disabilities. Can proxies be used to complete the SF-36? Gerontology. 2001 Nov-Dec;47(6):334–340. doi: 10.1159/000052824. [DOI] [PubMed] [Google Scholar]
- 6.Berwig M, Leicht H, Gertz HJ. Critical Evaluation of Self-Rated Quality of Life in Mild Cognitive Impairment and Alzheimer's Disease - Further Evidence for the Impact of Anosognosia and Global Cognitive Impairment. J Nutr Health Aging. 2009;13(3):226–230. doi: 10.1007/s12603-009-0063-4. [DOI] [PubMed] [Google Scholar]
- 7.Gundy CM, Aaronson NK. The influence of proxy perspective on patient-proxy agreement in the evaluation of health-related quality of life: an empirical study. Med Care. 2008 Feb;46(2):209–216. doi: 10.1097/MLR.0b013e318158af13. [DOI] [PubMed] [Google Scholar]
- 8.Huang HL, Chang MY, Tang JS, Chiu YC, Weng LC. Determinants of the discrepancy in patient- and caregiver-rated quality of life for persons with dementia. J Clin Nurs. 2008 Dec 12; doi: 10.1111/j.1365-2702.2008.02537.x. [DOI] [PubMed] [Google Scholar]
- 9.McPhail S, Beller E, Haines T. Two perspectives of proxy reporting of health-related quality of life using the Euroqol-5D, an investigation of agreement. Med Care. 2008 Nov;46(11):1140–1148. doi: 10.1097/MLR.0b013e31817d69a6. [DOI] [PubMed] [Google Scholar]
- 10.Muus I, Petzold M, Ringsberg KC. Health-related quality of life after stroke: reliability of proxy responses. Clin Nurs Res. 2009 May;18(2):103–118. doi: 10.1177/1054773809334912. [DOI] [PubMed] [Google Scholar]
- 11.Pickard AS, Johnson JA, Feeny DH, Shuaib A, Carriere KC, Nasser AM. Agreement Between Patient and Proxy Assessments of Health-Related Quality of Life After Stroke Using the EQ-5D and Health Utilities Index. Stroke. 2004 February 1;35(2):607–612. doi: 10.1161/01.STR.0000110984.91157.BD. [DOI] [PubMed] [Google Scholar]
- 12.Long K, Sudha S, Mutran EJ. Elder-proxy agreement concerning the functional status and medical history of the older person: the impact of caregiver burden and depressive symptomatology. J Am Geriatr Soc. 1998 Sep;46(9):1103–1111. doi: 10.1111/j.1532-5415.1998.tb06648.x. [DOI] [PubMed] [Google Scholar]
- 13.Shaw C, McColl E, Bond S. Functional abilities and continence: the use of proxy respondents in research involving older people. Qual Life Res. 2000;9(10):1117–1126. doi: 10.1023/a:1016660724376. [DOI] [PubMed] [Google Scholar]
- 14.Weinberger M, Samsa GP, Schmader K, Greenberg SM, Carr DB, Wildman DS. Comparing proxy and patients' perceptions of patients' functional status: results from an outpatient geriatric clinic. J Am Geriatr Soc. 1992 Jun;40(6):585–588. doi: 10.1111/j.1532-5415.1992.tb02107.x. [DOI] [PubMed] [Google Scholar]
- 15.Magaziner J, Bassett SS, Hebel JR, Gruber-Baldini A. Use of Proxies to Measure Health and Functional Status in Epidemiologic Studies of Community-dwelling Women Aged 65 Years and Older. Am J Epidemiol. 1996 February 1;143(3):283–292. doi: 10.1093/oxfordjournals.aje.a008740. [DOI] [PubMed] [Google Scholar]
- 16.Lerner-Geva L, Frenkel Y, Lusky A, Farhi A, Rabinovici J. An assessment of the validity of reporting by proxy to women's health questionnaire: a pilot study. Eur J Obstet Gynecol Reprod Biol. 2008 May;138(1):80–82. doi: 10.1016/j.ejogrb.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Health and Retirement Study, (2006 Core, Early, V2.0) public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740) Ann Arbor, MI: 2007. [Google Scholar]
- 18.Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977 June 1;1(3):385–401. [Google Scholar]
- 19.Steffick DE. Documentation of affective functioning measures in the Health and Retirement Study: HRS Documentation Report DR-005. 2000. [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatry Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 21.Brandt J, S Miriam, Folstein Marshal. The Telephone Interview for Cognitive Status. Neuropsychiatry, Neuropsychology, & Behavioral Neurology. 1988;1(2):111–117. [Google Scholar]
- 22.Wilcoxin F. Probability tables for individual comparisons by ranking methods. Biometrics. 1947 Sep;3(3):119–122. [PubMed] [Google Scholar]
- 23.Fleiss JL, Cohen J. The Equivalence of Weighted Kappa and the Intraclass Correlation Coefficient as Measures of Reliability. Educational and Psychological Measurement. 1973 October 1;33(3):613–619. [Google Scholar]
- 24.Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. 1993 Apr;39(4):561–577. [PubMed] [Google Scholar]
- 25.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983 Sep;148(3):839–843. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 26.Cleves MA, Rock L. From the help desk: Comparing areas under receiver operating characteristic curves from two or more probit or logit models. The Stata Journal. 2002;2:301–313. [Google Scholar]
- 27.Williams R. Generalized Ordered Logit/ Partial Proportional Odds Models for Ordinal Dependent Variables. The Stata Journal. 2006;6(1):58–82. [Google Scholar]
- 28.Miller TR, Wolinsky FD. Self-rated health trajectories and mortality among older adults. J Gerontol B Psychol Sci Soc Sci. 2007 Jan;62(1):S22–27. doi: 10.1093/geronb/62.1.s22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh-Manoux A, Gueguen A, Martikainen P, Ferrie J, Marmot M, Shipley M. Self-Rated Health and Mortality: Short- and Long-Term Associations in the Whitehall II Study. Psychosom Med. 2007 February 1;69(2):138–143. doi: 10.1097/PSY.0b013e318030483a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sei JL, Sandra YMA, Landefeld CS, et al. The Relationship Between Self-Rated Health and Mortality in Older Black and White Americans. Journal of the American Geriatrics Society. 2007;55(10):1624–1629. doi: 10.1111/j.1532-5415.2007.01360.x. [DOI] [PubMed] [Google Scholar]
- 31.Pickard AS, Lin HW, Knight SJ, et al. Proxy assessment of health-related quality of life in african american and white respondents with prostate cancer: perspective matters. Med Care. 2009 Feb;47(2):176–183. doi: 10.1097/MLR.0b013e31818475f4. [DOI] [PMC free article] [PubMed] [Google Scholar]