Abstract
Objective:
To determine the incidence and etiology of fever and the risk factors related to fever in adults with spinal cord injury (SCI) at the rehabilitation stage.
Design/Subjects:
A retrospective examination of records of 392 consecutive adult patients with traumatic SCI who received inpatient rehabilitation program.
Setting:
A national rehabilitation center in Turkey.
Outcome Measures:
Incidence and etiology of fever, period of hospitalization (days).
Results:
A total of 187 patients (47.7%) had fever at least once during their rehabilitation program. The most common etiology was urinary tract infection. The rate of fever occurrence was significantly higher in patients with complete SCI (P = 0.001). In patients with fever, the use of an indwelling catheter was significantly higher compared with clean intermittent catheterization and spontaneous voiding (P = 0.001). The hospitalization period of patients with fever was significantly longer than that of patients without fever (P = 0.006).
Conclusions:
A high rate of fever was seen in patients with SCI during rehabilitation. Fever was caused by various infections, of which urinary tract infection was the most common. Patients with motor complete injuries and those with permanent catheters constituted higher risk groups. Fever prolonged the length of rehabilitation stay and hindered active participation in the rehabilitation program.
Keywords: Spinal cord injuries, complete, incomplete; Fever, etiology; Rehabilitation, physical; Urinary tract infection; Bladder management
INTRODUCTION
Fever is a frequent complication in patients with spinal cord injury (SCI) and may be an early sign of morbidity (1). Infectious causes hold the first rank among the etiologic factors, the most common being urinary tract infections (UTIs) and respiratory tract infections (2–5). Noninfectious conditions, such as thromboembolic disease, heterotopic ossification, and thermoregulatory dysfunction, can also cause fever in patients with SCI (6–8). However, the cause of fever may not always be easy to determine in these patients. Symptoms and findings of the infection may differ according to the neurologic level and completeness of injury (1).
The incidence of fever is reported to be 60% to 85% in patients with SCI in various studies (1,4,5). However, such studies reporting the incidence of fever were generally conducted during the acute phase, and the data are very limited on incidence of fever during the rehabilitation period. The only study on this particular subject in the literature was conducted by McKinley et al (1) in 40 patients with traumatic SCI during the rehabilitation stage, in which the reported incidence of fever was 50%.
Determining the cause of fever and understanding risk factors in the rehabilitation stage are very important in terms of preventing fever and planning an appropriate treatment. Fever may prolong the hospitalization period by adversely affecting progress in rehabilitation (9). Prolonged rehabilitation stay means additional costs for these patients, who already have high treatment costs (9).
The objectives of this study were to determine (a) the incidence of fever, (b) the etiology of fever, and (c) the risk factors related to fever occurring during rehabilitation in patients with traumatic SCI.
METHODS
The study was performed retrospectively by evaluating the records of 392 consecutive adults with traumatic SCI who had undergone an inpatient rehabilitation program from 2000 to 2005 at the Ankara Physical Medicine and Rehabilitation Training and Research Hospital, which is, with a capacity of 250 beds, one of the largest national rehabilitation centers in Turkey. Patients with SCI, which constitute approximately one fourth of the total patient population, are admitted to our hospital from all over the country, either by physician referral or by personal application. Admitted patients are generally at the subacute or chronic stage, are clinically stable, and have already received necessary surgical interventions at the acute stage. Thus, this study included patients at the subacute or chronic stage of SCI who were admitted to the clinic for an inpatient rehabilitation program. Average time since injury on admission was 198.42 ± 82.75 days. The study protocol was approved by the review committee of our institution.
Demographic data, duration of disease (days), etiologic causes of injury, and hospitalization periods (days) were recorded for all patients included in the study. Neurologic level was defined using ASIA (10). During the analysis, the patients were divided into 2 groups: complete (ASIA A) and incomplete (ASIA B-C-D-E) (10). Adults with fever on admission and children were excluded from the study.
Presence of fever during the rehabilitation period was determined from medical and nursing records. Initially, 405 patients were analyzed in the study, with 13 patients excluded due to fever on admission. Core temperature measurement requires invasive techniques in the tympanic membrane, esophagus, or pulmonary artery, which are the gold standards (11). In routine practice, it is impractical to use invasive techniques to achieve the gold standard. Although rectal temperature readings are considered most representative of core temperature of the conventional temperature recording methods (12), this method could not be used in our study because of concerns over patient discomfort and rejection. In our clinical practice, we measure axillary temperature with standard mercury thermometers. The routine procedure on the ward is to measure axillary temperature 4 times daily. The number of measurements is increased during febrile periods. Body temperature of 36°C to 37.5°C was regarded as normal and >37.5°C as elevated (13). An increase in body temperature at least twice in 24 hours was considered fever (3). Maximum and minimum body temperature values were noted. The number of febrile days and the number of days during which the rehabilitation program was paused because of the fever were recorded. General practice in our clinic is to have the patients perform passive range-of-motion exercises during the period they have fever, and to resume active exercise programs when the temperature drops below 37.5°C. Recurring fever during the rehabilitation program and its causes were also noted.
Etiologic causes of fever were determined by evaluation of physical examination findings, laboratory results (eg, complete blood count, urinalysis, urine, wound and blood cultures), and radiologic imaging results (eg, chest radiograph, ultrasonography, Doppler). Cases in which the cause could not be determined were noted as fever of unknown origin (1). Causes of fever were classified as UTI, upper respiratory tract infection, pneumonia, wound infection, abscess, and other (eg, heterotopic ossification, deep vein thrombosis, gastrointestinal infection, sepsis). Whether treatment had been started and, if so, the treatment method used (oral, parenteral) were also recorded. Bladder evacuation methods were recorded (indwelling catheter, clean intermittent catheterization, spontaneous emptying).
Statistical Analysis
All data were entered into a database for later analysis (SPSS version 10.0 for Windows; SPSS Inc, Chicago, IL). The results were presented as descriptive statistics for categoric data, and the independent samples t test was used to compare continuous variables. The X2 test was employed to compare categoric data, such as the gender of patients with and without fever. Significance was set at P = 0.05.
RESULTS
Demographic Data
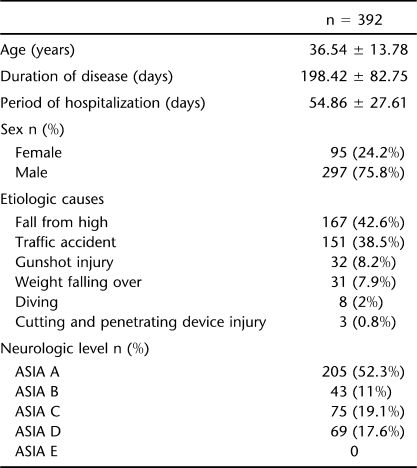
Demographic data of 392 patients included in the study are given in Table 1. Closer examination of Table 1 indicates that the most common etiologic cause of SCI was fall from height (42.6%) followed by traffic accidents (38.5%). The lesion level was thoracic in 236 patients (60.2%), cervical in 80 (20.4%), and lumbar in 76 (19.4%).
Table 1.
Distribution of Demographic Properties, Duration of Disease, Average Hospitalization Period, Etiologic Causes, and Neurologic Level
Of the 392 patients, SCI was complete in 205 (52.3%) and incomplete in 187 (47.7%). The number of patients with complete lesions was significantly higher in patients with thoracic lesions than among those with cervical or lumbar lesions (X2 = 99.95, P = 0.001). Respectively, 194 (77.9%) of the 236 patients with thoracic lesions, 38 (15.3%) of the 80 patients with cervical lesions, and 17 (6.8%) of the 76 patients with lumbar lesions had complete injuries.
Incidence of Fever, Etiologic Causes, and Risk Factors
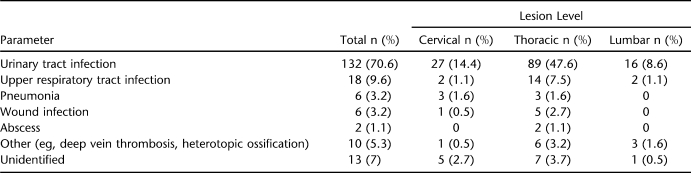
Incidence of fever was 47.7%. Fever occurred at least once in 187 (47.7%) patients, twice in 35 (18%) patients, and 3 times in 7 (3.7%) patients during the inpatient rehabilitation period. Distribution of the etiologic causes in febrile patients is given in Table 2. The most common cause of fever was UTI (70.6%). UTI was also the most common cause in patients with recurrent fever. Etiologic causes in patients with twice-recurring fever were UTI (68.6%), upper respiratory tract infection (14.3%), pneumonia (2.9%), wound infection (2.9%), other causes (8.6%), and fever of unknown origin (7%). The highest body temperature recorded was 41°C, with the lowest being 35.4°C. The average number of febrile days was found to be 3.51 ± 1.14 days in patients with fever, and the average number of days that the rehabilitation program was suspended was 3.25 ± 1.48 days.
Table 2.
Distribution of Etiologic Causes by Lesion Level in Patients With Fever
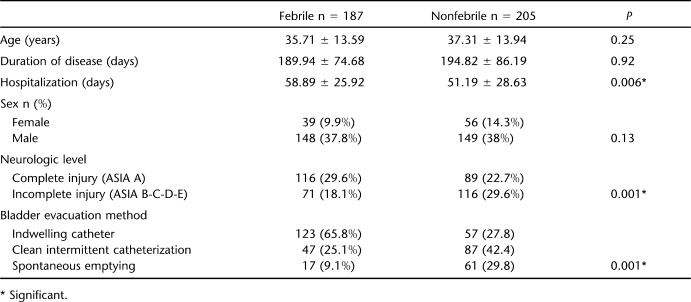
Differences Between Febrile and Nonfebrile Patients
There were no differences between febrile (n = 187) and nonfebrile (n = 205) patients with respect to age, mean duration of disease, and sex (Table 3). However, it was determined that febrile patients stayed in the hospital significantly longer (58.89 ± 25.92 days) than nonfebrile patients (51.19 ± 28.63 days) (P = 0.006). Similarly, the length of rehabilitation stay for patients with complete injury (60.95 ± 24.13 days) was significantly longer than for patients with incomplete injury (51.11 ± 29.40 days) (t = 3.63 P = 0.001). Besides, febrile patients with complete injury (64.40 ± 25.35 days) stayed in the hospital significantly longer than nonfebrile patients with complete injury (56.46 ± 21.77 days) (t = 2.36, P = 0.01). Febrile patients with incomplete injury also stayed in the hospital significantly longer (57.57 ± 22.30 days) than nonfebrile patients with incomplete injury (47.15 ± 32.46 days) (t = 2.38, P = 0.01).
Table 3.
Differences Between Febrile and Nonfebrile Patients
The incidence of fever was significantly higher in patients with complete SCI (ASIA A) compared with patients with incomplete SCI (X2 = 13.58, P = 0.001). Of 187 febrile patients, 116 (62%) had complete SCI and 71 (38%) had incomplete SCI.
The incidence of fever was significantly higher in patients with thoracic lesions compared with those with cervical or lumbar lesions (X2 = 13.81, P = 0.001). Fever was encountered in 126 (67.4%) of 236 patients with thoracic lesions, 39 (20.9%) of 80 patients with cervical lesions, and 22 (11.8%) of 76 patients with lumbar lesions. Distribution of the causes of fever by lesion level is given in Table 2.
It was also observed that indwelling catheters were used significantly more frequently than clean intermittent catheterization application or spontaneous emptying as the bladder evacuation method in febrile patients (X2 = 60.26, P = 0.001). Of 187 febrile patients, 123 (65.8%) used an indwelling catheter, 47 (25.1%) employed clean intermittent catheterization, and 17 (9.1%) had spontaneous urination.
Antibiotic therapy was started orally in 104 (55.6%) of the 187 febrile patients and parenterally in 60 (32.1%), for a total of 164 patients.
DISCUSSION
Main data obtained in this study show that the incidence of fever is high (47.7%) during the rehabilitation stage in SCI, that the most common etiologic factor is UTI, and that fever increases length of rehabilitation stay by compromising the rehabilitation program. It also demonstrates that the fever incidence is higher in patients with complete lesions and in those with indwelling catheters. This study is significant in that it is one of the few investigating fever incidence during the rehabilitation period and that it is a large series of Turkish patients treated in one of the largest rehabilitation centers in Turkey.
Fever is a common complication in patients with SCI (1). However, most of the data on fever pertains to acute SCI. Colachis et al (4) reported the incidence of fever to be 85% in a study conducted on 156 patients with acute traumatic SCI, and Sugarman et al (5) reported the incidence to be 67% in another study. McKinley et al (1) reported the incidence of fever in their study of traumatic SCI to be 60.4% during the acute stage and 50% during the rehabilitation period. However, this study was conducted on a relatively small patient population, with 48 in the acute stage and 40 in the rehabilitation stage. In our study, the incidence of fever was investigated in a larger series of patients at the subacute and chronic stage, and a very close incidence rate (47.7%) was found.
The etiology of fever in SCI must be investigated because the underlying pathology may be an important cause of morbidity. Infections, the most common cause of fever, are a significant cause of morbidity and mortality in individuals with SCI (3). Factors such as prolonged immobilization, respiratory muscle weakness, surgical interventions, prolonged hospitalization, and neurogenic bladder increase the tendency toward infections in patients with SCI (1). The most common causes of fever in SCI have been reported by various authors as follows: UTIs and soft-tissue infections by Sugarman et al (4), UTIs and respiratory tract infections by Colachis et al (5), and respiratory tract infections in the acute stage and UTIs at the rehabilitation stage by McKinley et al (1). UTIs (70.6%) were also the most common cause of fever at the rehabilitation period in our study. The risk of UTI is increased in SCI due to incontinence, increased intravesical pressure, reflux, and neurologic obstruction (14,15). In addition, the use of indwelling catheters in these patients also increases the risk for UTI (15,16). In fact, we found higher rates of fever in patients with indwelling catheters. We therefore believe that control of the factors causing UTI is important to prevent fever development. Use of clean intermittent catheterization should be the preferred bladder evacuation method in suitable patients because, compared with indwelling catheter, it reduces the risk of UTI (14).
Respiratory tract infections were second among infectious causes. We also observed that most of the patients with respiratory tract infections had cervical or thoracic lesions. Cotton et al (17) evaluated 596 patients with thoracic SCI and reported a high incidence of intubation, pneumonia, and mortality in patients with T1-T6 lesions. Muscle weakness in primary or accessory respiratory muscles depending on lesion level increases risk for respiratory tract infection in both the acute and the rehabilitation stages (1,18). Pulmonary rehabilitation should therefore be given priority, especially in patients with cervical or high thoracic lesions, because pulmonary complications rank the first among the causes of mortality after SCI (19).
We determined that wound infections and abscesses were third and fourth, respectively, among the most common etiologic factors of fever and that all such cases in our study were in patients with cervical or thoracic SCI. Beraldo et al (3) reported soft-tissue–related fever (pressure ulcer, abscess) in 11.4% of fever episodes. McKinley et al (1) reported wound infection as the cause of fever in 5% of the patients during the rehabilitation period. The percentage of wound infections as an etiologic factor was as low as 3.2% in our study. This may be associated with the better clinical care and early mobilization provided during recent years. The patient and the caregivers should be informed about preventive measures, adequate and proper nutrition should be provided, and early mobilization should be achieved to prevent pressure ulcer development (1,2).
We also found that noninfectious causes, such as deep vein thrombosis and heterotopic ossification, were underlying causes of fever in 5.3% of the cases. Therefore, noninfectious reasons along with infectious causes should be taken into account in fever etiology in patients with SCI. However, sometimes it may not be possible to determine the cause of fever, despite numerous tests and diagnostic methods. A study evaluating 129 patients (85 with paraplegia and 44 with tetraplegia) has reported the incidence of fever of unknown origin as 8% (3). Similarly, we found an incidence of fever of unknown origin of 7%.
Identification of risk factors associated with fever is important to prevent fever. McKinley et al (1) have reported a higher incidence of fever in patients with complete spinal lesions and in those with SCI associated with gunshot wounds. However, Beraldo et al (3) found no relation between lesion level and fever. We found a higher incidence of fever in patients with complete injury and thoracic lesions. Patients with complete SCI have a higher risk of secondary complications related to the SCI. This may explain the higher fever incidence in patients with complete SCI. Furthermore, etiologic factors causing fever may be more prevalent during the rehabilitation period of patients with complete SCI, because their rehabilitation lasts longer compared with that of patients with incomplete SCI. In fact, we found that the duration of inpatient care of patients with complete SCI was significantly longer than for patients with incomplete SCI.
In contrast to previously published studies, we found a significantly higher incidence of fever in patients with thoracic lesions than among those with cervical lesions. One explanation may be that the patients with thoracic lesions had a higher rate of complete SCI, compared with patients with cervical or lumbar lesions.
We found that patients with fever were unable to participate actively in their rehabilitation program during their febrile periods and that their hospitalization period increased significantly compared with that for nonfebrile patients. In addition, we also determined that the length of rehabilitation stay for febrile patients with complete SCI was significantly higher than for nonfebrile patients with complete SCI. These data indicate that fever is associated with a longer rehabilitation period for patients with complete lesions than with incomplete lesions. Fever prevents the patient from actively participating in the rehabilitation program and prolongs the hospitalization period. By understanding fever etiology, determining risk groups, and starting appropriate treatment in the early period, rehabilitation programs will be beneficial and patient costs will decrease. Controlled studies on this subject are needed.
CONCLUSIONS
Fever is frequently seen in patients with SCI, both in the acute and rehabilitation stages. Infections, especially UTIs, rank as the first etiologic causes of fever. Patients with complete injury and those using indwelling catheters are high-risk groups with respect to fever. Fever prevents active participation in rehabilitation programs and prolongs duration of hospitalization. We therefore believe that factors causing infection in patients with SCI, especially in high-risk groups, should be identified and addressed to prevent fever and its adverse effects on rehabilitation and recovery.
REFERENCES
- McKinley W, McNamee S, Meade M, Kandra K, Abdul N. Incidence, etiology, and risk factors for fever following acute spinal cord injury. J Spinal Cord Med. 2006;29(5):501–506. doi: 10.1080/10790268.2006.11753899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomerie JZ. Infections in patients with spinal cord injuries. Clin Infect Dis. 1997;25(6):1285–1290. doi: 10.1086/516144. [DOI] [PubMed] [Google Scholar]
- Beraldo PS, Neves EG, Alves CM, Khan P, Cirilo AC, Alencar MR. Pyrexia in hospitalised spinal cord injury patients. Paraplegia. 1993;31(3):186–191. doi: 10.1038/sc.1993.35. [DOI] [PubMed] [Google Scholar]
- Sugarman B, Brown D, Musher D. Fever and infection in spinal cord injury patients. JAMA. 1982;248(1):66–70. [PubMed] [Google Scholar]
- Colachis SC, 3rd, Otis SM. Occurrence of fever associated with thermoregulatory dysfunction after acute traumatic spinal cord injury. Am J Phys Med Rehabil. 1995;74(2):114–119. [PubMed] [Google Scholar]
- Chen D, Apple DF, Jr, Hudson LM, Bode R. Medical complications during acute rehabilitation following spinal cord injury: current experience of the Model Systems. Arch Phys Med Rehabil. 1999;80(11):1397–1401. doi: 10.1016/s0003-9993(99)90250-2. [DOI] [PubMed] [Google Scholar]
- Subbarao JV, Garrison SJ. Heterotopic ossification: diagnosis and management, current concepts and controversies. J Spinal Cord Med. 1999;22(4):273–283. doi: 10.1080/10790268.1999.11719580. [DOI] [PubMed] [Google Scholar]
- Schmidt KD, Chan CW. Thermoregulation and fever in normal persons and in those with spinal cord injuries. Mayo Clin Proc. 1992;67(5):469–475. doi: 10.1016/s0025-6196(12)60394-2. [DOI] [PubMed] [Google Scholar]
- Eastwood EA, Hagglund JK, Ragnarsonn TK, Gordon WA, Marino RJ. Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury: 1990–1997. Arch Phys Med Rehabil. 1999;80(11):1457–1463. doi: 10.1016/s0003-9993(99)90258-7. [DOI] [PubMed] [Google Scholar]
- Kirshblum SC, Groah SL, McKinley WO, Gittler MS, Stiens SA. Spinal cord injury medicine. 1. Etiology, classification, and acute medical management. Arch Phys Med Rehabil. 2002;83(3 suppl 1):50–57. doi: 10.1053/apmr.2002.32156. [DOI] [PubMed] [Google Scholar]
- Jensen BN, Jensen FS, Madsen SN, Løssl K. Accuracy of digital tympanic, oral, axillary and rectal thermometers compared with standard rectal mercury thermometers. Eur J Surg. 2000;166(11):848–851. doi: 10.1080/110241500447218. [DOI] [PubMed] [Google Scholar]
- Fulbrook P. Core temperature measurements in adults: a literature review. J Adv Nurs. 1993;18(9):1451–1460. doi: 10.1046/j.1365-2648.1993.18091451.x. [DOI] [PubMed] [Google Scholar]
- Essiet A, Onuba O. Hyperpyrexia in spinal injury patients. Paraplegia. 1992;30(5):339–342. doi: 10.1038/sc.1992.79. [DOI] [PubMed] [Google Scholar]
- Siroky MB. Pathogenesis of bacteriuria and infection in the spinal cord injured patient. Am J Med. 2002;113(suppl 1A):S67–S79. doi: 10.1016/s0002-9343(02)01061-6. [DOI] [PubMed] [Google Scholar]
- National Institute on Disability and Rehabilitation Research (NIDRR) Consensus Statement The prevention and management of urinary tract infections among people with spinal cord injuries J Am Paraplegia Soc 1992153194–207.1500945 [Google Scholar]
- Cardenas DD, Hooton TM. Urinary tract infection in persons with spinal cord injury. Arch Phys Med Rehabil. 1995;76(3):272–280. doi: 10.1016/s0003-9993(95)80615-6. [DOI] [PubMed] [Google Scholar]
- Cotton BA, Pryor JP, Chinwalla I, Wiebe DJ, Reilly PM, Schwab CW. Respiratory complications and mortality risk associated with thoracic spine injury. J Trauma. 2005;59(6):1407–1409. doi: 10.1097/01.ta.0000196005.49422.e6. [DOI] [PubMed] [Google Scholar]
- McKinley W, Gittler M, Kirshblum S, Stiens S, Groah S. Medical complications after SCI. Arch Phys Med Rehabil. 2002;83(suppl 1):S58–S64. doi: 10.1053/apmr.2002.32159. [DOI] [PubMed] [Google Scholar]
- DeVivo MJ, Kartus PL, Stover SL, Rutt RD, Fine PR. Cause of death for patients with spinal cord injuries. Arch Intern Med. 1989;149(8):1761–1766. [PubMed] [Google Scholar]