Abstract
Background/Objective:
Intervertebral disk herniation is relatively common. Migration usually occurs in the ventral epidural space; rarely, disks migrate to the dorsal epidural space due to the natural anatomical barriers of the thecal sac.
Design:
Case report.
Findings:
A 49-year-old man presented with 1 week of severe back pain with bilateral radiculopathy to the lateral aspect of his lower extremities and weakness of the ankle dorsiflexors and toe extensors. Lumbar spine magnetic resonance imaging with gadolinium revealed a peripheral enhancing dorsal epidural lesion with severe compression of the thecal sac. Initial differential diagnosis included spontaneous hematoma, synovial cyst, and epidural abscess. Posterior lumbar decompression was performed; intraoperatively, the lesion was identified as a large herniated disk fragment.
Conclusions:
Dorsal migration of a herniated intervertebral disk is rare and may be difficult to definitively diagnose preoperatively. Dorsal disk migration may present in a variety of clinical scenarios and, as in this case, may mimic other epidural lesions on magnetic resonance imaging.
Keywords: Vertebral disk, herniation; Back pain, radiculopathy; Abscess, epidural; Hematoma, epidural; Laminectomy; Decompression, lumbar
INTRODUCTION
Herniated nucleus pulposus arising from intervertebral disk degeneration is a common condition. Reviews estimate that 35% to 72% of lumbar disk herniations manifest fragment migration, predominantly in the ventral and anterolateral epidural space (1–3). Few cases of disk fragment migration into the dorsal epidural space have been reported (Table 1). A report of dorsal fragment migration with unusual radiographic findings and a review of the pertinent published literature are presented.
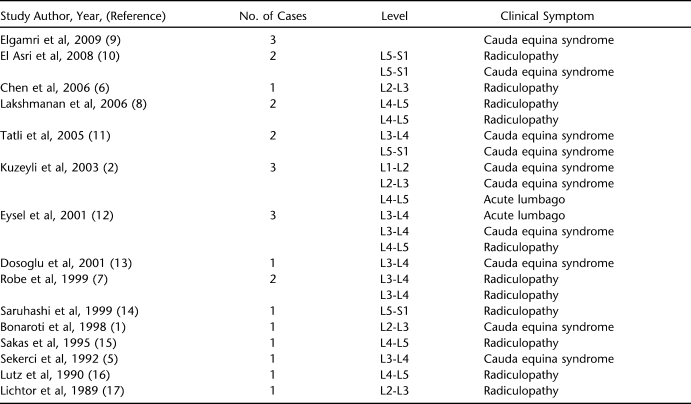
Table 1.
Review of Reported Cases of Migration of Intervertebral Disk Fragment to the Dorsal Epidural Space
CASE REPORT
A 49-year-old steel worker presented with 1 week of severe lower back pain radiating into the lateral aspect of both lower extremities. The pain was described as “excruciating” and was recalcitrant to oral pain medications. Onset of these symptoms occurred acutely after physical exertion at his workplace. A trial of conservative therapy utilizing oral nonsteroidal anti-inflammatory drugs and bed rest provided minimal relief. The patient noted bilateral lower extremity weakness but denied bowel and bladder symptoms. Neurologic examination found muscle strength of 4/5 in the tibialis anterior and extensor hallucis longus in both lower extremities and 5/5 in all other muscles groups; sensation was intact in all dermatomes, and reflexes were 2/2. The remainder of the neurologic examination was normal.
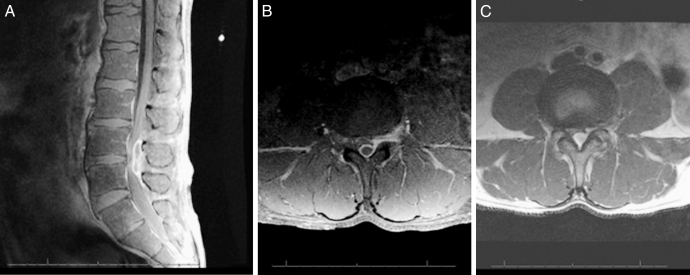
Plain radiographs of the lumbar spine revealed minimal degenerative spurring. Computed tomography demonstrated a dorsal epidural collection at L4-L5, with moderate central canal stenosis. Lumbar spine magnetic resonance imaging with gadolinium revealed a mass in the dorsal epidural space. The lesion was heterogeneously hyperintense on T1-weighted images with a rim of enhancement after gadolinium injection; the lesion was isointense to hyperintense on T2-weighted images. The imaging was consistent with spontaneous epidural hematoma or epidural abscess. The degree of disk degeneration at the L4-L5 level was mild (Figure 1). Laboratory values included an erythrocyte sedimentation rate of 8.0 and a C-reactive protein of 0.6 mg/L, making an infectious process unlikely.
Figure 1.
Magnetic resonance image of the lumbar spine showing a large dorsal epidural lesion. (A) Sagittal T1-weighted images after gadolinium injection. (B) Axial T1-weighted image after gadolinium injection show rim enhancement. (C) Axial T2-weighted images show severe thecal sac compression.
The patient underwent an L4-L5 central laminectomy. A large, solid epidural disk material was identified dorsally, with significant compression of the thecal sac. Dissection along the lateral margin of the spinal canal revealed tracking of the disk fragment ventral to the L4-L5 disk space, as well as a significant annular defect along the lateral aspect of the disk space. These operative findings were confirmed by histopathologic analysis of the intraoperative specimen.
Clinically the patient had immediate complete recovery of motor function and resolution of radicular pain. He did well postoperatively and had complete recovery of motor function to 5/5 in all muscle groups on the first postoperative day. After a few sessions with the in-hospital physical therapists, he was deemed stable for discharge home.
DISCUSSION
Migration of herniated intervertebral disk fragments into the dorsal epidural space is an infrequent event. Disk fragments typically follow a path of least resistance through the fissure in the posterior annulus. Due to the strength of the posterior longitudinal ligament, fragments usually remain ventral and infrequently lateral to the thecal sac. Cephalad migration is more common with lateral disk herniation, whereas caudal displacement may be more common in central disk extrusion (4). Lateral and dorsal migration is thought to be limited by a sagittal midline septum than spans the posterior longitudinal ligament and vertebral bodies. This thin connective tissue membrane connects the posterior longitudinal ligament to the medial and lateral wall of the spinal canal (3). The nerve roots may also act as an anatomical barrier limiting migration disk fragments to the dorsal epidural space.
Review of the literature illustrates that the clinical presentation in dorsal epidural disk herniation is variable, from low back pain without objective neurologic deficits to cauda equina syndrome. Authors have posited that due to disk fragment migration to the dorsal epidural space, several neural structures may be compromised. Hence, these patients may more often present with clinically significant neurologic deficits (1,5). However, a review of the published literature clearly delineates a wide spectrum of symptoms (Table 1).
Definitive diagnosis of a dorsal herniated disk fragment may be difficult. Conventional axial and sagittal magnetic resonance imaging has been the method of choice for radiologic diagnosis of lumbar degenerative conditions. However, it may not always absolutely differentiate similar processes, such as herniated disk, epidural hematoma, and abscess. Herniated disks are usually hypointense on T1-weighted images and hyperintense on 80% of T2-weighted images (2,3,6). Herniated disk fragments sequestered in the dorsal epidural space may appear similar to other dorsal epidural pathologies, such as abscess, hematoma, and malignancy. As disk fragments migrate dorsally, they become surrounded by a vascular layer of epidural fat, which can induce an inflammatory response, and the formation of a granulation tissue around the disk fragment (7,8). The presence of circumferential contrast enhancement raises the possibility of abscess or epidural metastasis.
This patient's magnetic resonance images revealed a lesion with rim enhancement. The absence of diskitis and osteomyelitis on imaging in addition to unremarkable infectious laboratory markers (erythrocyte sedimentation rate, C-reactive protein) decreases the potential for epidural abscess; however, they do not eliminate it absolutely. Our patient also presented with a clear history of physical exertion followed promptly by onset of symptoms. Although a sequestered disk fragment was high upon our list of preoperative differential diagnoses, the severity of patient symptoms and our diagnostic uncertainty equally mandated operative exploration.
CONCLUSIONS
The rare dorsal migration of sequestered lumbar herniated disks may be difficult to definitively diagnose. Dorsal disk migration may present in a variety of clinical scenarios and may mimic other more common dorsal epidural lesions on magnetic resonance imaging. Dorsal migration of herniated lumbar disk fragments should be considered in the differential diagnosis of dorsal epidural enhancing lesions in patients with appropriate clinical histories.
References
- Bonaroti EA, Welch WC. Posterior epidural migration of an extruded lumbar disk fragment causing cauda equina syndrome: clinical and magnetic resonance imaging evaluation. Spine. 1998;23(3):378–381. doi: 10.1097/00007632-199802010-00018. [DOI] [PubMed] [Google Scholar]
- Kuzeyli K, Cakir E, Usul H, et al. Posterior epidural migration of lumbar disk fragments: report of three cases. Spine. 2003;28(3):E64–E67. doi: 10.1097/01.BRS.0000042272.17850.49. [DOI] [PubMed] [Google Scholar]
- Schellinger D, Manz HJ, Vidic B, et al. Disk fragment migration. Radiology. 1990;175(3):831–836. doi: 10.1148/radiology.175.3.2343133. [DOI] [PubMed] [Google Scholar]
- Ebeling U, Reulen HJ. Are there typical localisations of lumbar disk herniations? A prospective study. Acta Neurochir. 1992;117(3–4):143–148. doi: 10.1007/BF01400611. [DOI] [PubMed] [Google Scholar]
- Sekerci Z, Ildan F, Yuksel M, Gul B, Kilic C. Cauda equina compression due to posterior epidural migration of extruded lumbar disk. Neurosurg Rev. 1992;15(4):311–313. doi: 10.1007/BF00257813. [DOI] [PubMed] [Google Scholar]
- Chen CY, Chuang YL, Yao MS, Chiu WT, Chen CL, Chan WP. Posterior epidural migration of a sequestrated lumbar disk fragment: MR imaging findings. AJNR Am J Neuroradiol. 2006;27(7):1592–1594. [PMC free article] [PubMed] [Google Scholar]
- Robe P, Martin D, Lenelle J, Stevenaert A. Posterior epidural migration of sequestered lumbar disk fragments: report of two cases. J Neurosurg. 1999;90(2 suppl):264–266. doi: 10.3171/spi.1999.90.2.0264. [DOI] [PubMed] [Google Scholar]
- Lakshmanan P, Ahuja S, Lyons K, Howes J, Davies PR. Sequestrated lumbar intervertebral disk in the posterior epidural space: a report on two cases and review of the literature. Spine J. 2006;6(5):583–586. doi: 10.1016/j.spinee.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Elgamri A, Sami A, Aqqad A, et al. Posterior migration of a lumbar disk herniation as a cause of cauda equina syndrome. J Radiol. 2009;90(6):731–733. doi: 10.1016/s0221-0363(09)74728-6. [DOI] [PubMed] [Google Scholar]
- El Asri AC, Naama O, Akhaddar A, et al. Posterior epidural migration of lumbar disk fragments: report of two cases and review of the literature. Surg Neurol. 2008;70(6):668–671. doi: 10.1016/j.surneu.2007.06.034. discussion 671. [DOI] [PubMed] [Google Scholar]
- Tatli M, Guzel A, Ceviz A, Karadag O. Posterior epidural migration of sequestered lumbar disk fragment causing cauda equina syndrome. Br J Neurosurg. 2005;19(3):257–259. doi: 10.1080/02688690500208593. [DOI] [PubMed] [Google Scholar]
- Eysel P, Herbsthofer B. Dorsal compression of the epidural cord due to free sequestral lumbar prolapse: diagnostic problems in magnetic resonance imaging and computed tomography. Arch Orthop Trauma Surg. 2001;121(4):238–240. doi: 10.1007/s004020000213. [DOI] [PubMed] [Google Scholar]
- Dosoglu M, Is M, Gezen F, Ziyal MI. Posterior epidural migration of a lumbar disk fragment causing cauda equina syndrome: case report and review of the relevant literature. Eur Spine J. 2001;10(4):348–351. doi: 10.1007/s005860100300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saruhashi Y, Omura K, Miyamoto K, Katsuura A, Hukuda S. A migrated lumbar disk herniation simulating a dumbbell tumor. J Spinal Disord. 1999;12(4):307–309. [PubMed] [Google Scholar]
- Sakas DE, Farrell MA, Young S, Toland J. Posterior thecal lumbar disk herniation mimicking synovial cyst. Neuroradiology. 1995;37(3):192–194. doi: 10.1007/BF01578256. [DOI] [PubMed] [Google Scholar]
- Lutz JD, Smith RR, Jones HM. CT myelography of a fragment of a lumbar disk sequestered posterior to the thecal sac. AJNR Am J Neuroradiol. 1990;11(3):610–611. [PMC free article] [PubMed] [Google Scholar]
- Lichtor T. Posterior epidural migration of extruded lumbar disk. Surg Neurol. 1989;32(4):311–312. doi: 10.1016/0090-3019(89)90236-x. [DOI] [PubMed] [Google Scholar]