Abstract
Background
Individual home characteristics have been associated with indoor allergen exposure; however, the influence of neighborhood-level characteristics has not been well-studied. We defined neighborhoods as community districts determined by the New York Department of City Planning.
Objective
We examined the relationship between neighborhood-level characteristics and the presence of dust mite (Der f 1), cat (Fel d 1), cockroach (Bla g 2), and mouse (MUP) allergens in the household.
Methods
Using data from the Puerto Rican Asthma Project, a birth cohort of Puerto Rican children at risk of allergic sensitization (n=261) we examined associations between neighborhood characteristics (percent tree canopy, asthma hospitalizations per 1000 children, roadway length within 100 meters of buildings, serious housing code violations per 1000 rental units, poverty rates, and felony crime rates) and the presence of indoor allergens. Allergen cutpoints were used for categorical analyses and defined as follows: dust mite: >0.25 μg/g; cat: >1 μg/g; cockroach: >1 U/g; mouse: >1.6 μg/g.
Results
Serious housing code violations were statistically significantly positively associated with dust mite, cat and mouse allergens (continuous variables), adjusting for mother's income and education, and all neighborhood-level characteristics. In multivariable logistic regression analyses, medium levels of housing code violations were associated with higher dust mite and cat allergens (1.81, 95%CI: 1.08, 3.03 and 3.10, 95%CI: 1.22, 7.92, respectively). A high level of serious housing code violations was associated with higher mouse allergen (2.04, 95%CI: 1.15, 3.62). A medium level of housing code violations was associated with higher cockroach allergen (3.30, 95%CI: 1.11, 9.78).
Conclusions
Neighborhood-level characteristics, specifically housing code violations, appear to be related to indoor allergens, which may have implications for future research explorations and policy decisions.
Keywords: indoor allergens, dust mite, cat, cockroach, mouse, asthma, neighborhoods, community districts, housing code violations, policy, New York City, Puerto Rican
Introduction
In the United States, there is a large body of literature showing an association between neighborhood characteristics and health outcomes. (1) For instance, both neighborhood poverty and negative social climate contribute to child behavior problems. (2, 3) Yet, favorable neighborhood characteristics can also result in positive health outcomes. For example for adolescents, living in a neighborhood with a higher concentration of organizations or services for children and adults was associated with lower levels of youth aggression. (4) Asthma, a chronic disease of the lungs characterized by narrowing airways and recurrent breathing problems, affects 22.9 million Americans. (5-7) Despite the breadth of work concerning neighborhoods and health, only a few studies have examined the relationship between neighborhood-level characteristics and asthma. Previous research demonstrated that neighborhood-level characteristics such as neighborhood violence (8, 9) and pollution (10-14) are related to asthma morbidity (15-19). Also, not only do African Americans and Hispanics have a much higher risk of preventable asthma hospitalization than non-Hispanic Whites (20) but the racial composition of a neighborhood (i.e. proportion of African American and Hispanics) is associated with asthma hospitalization rates. (16) In addition, low-income areas have a disproportionate prevalence of childhood asthma. (21, 22)
Indoor allergen exposure is a risk factor for allergic sensitization, asthma development, and asthma morbidity. Although, previous work indicates that neighborhood characteristics are related to asthma morbidity, and asthma morbidity is related to indoor allergens, to our knowledge, no studies have specifically examined the association of neighborhood-level characteristics and the presence of indoor allergens. (21-25)
Neighborhood-Level
Asthma triggers, such as allergens, at the household or housing unit level have been widely investigated in the public health literature (23-48). Sensitization to cockroach allergen is widely known to be associated with asthma. (49-51) High exposure to cockroach allergen and concomitant cockroach allergy is a risk factor for asthma medication use and asthma-related hospitalizations. (30) Sensitization to indoor allergens (e.g. from to dust mites, cats, cockroaches, and mice) can be related to airway hyperresponsivesness (52), and wheezing. (53) Increased exposure to allergens, particularly dust mites and cockroaches, is related to an increased likelihood of developing asthma. (29, 54, 55)
Some indoor allergens (e.g., cockroach and mouse) are more prevalent in low-income inner-city areas; this suggests the possible role of both housing deterioration and disadvantaged neighborhood conditions concerning the presence of indoor allergens. (56-63) In low-income urban neighborhoods such as the Bronx and East Harlem, asthma morbidity is associated with high-levels of indoor allergens. (25, 30, 35, 40) We explored the association between neighborhood-level characteristics (environmental and social neighborhood exposures) and the following indoor allergens: dust mite (Der f 1), cat (Fel d 1), cockroach (Bla g 2), and mouse (MUP) in a birth cohort of Puerto Rican children in the Bronx, New York.
Specifically, we explored the following neighborhood characteristics: percent tree canopy, asthma hospitalization rates, mean roadway length, serious housing code violations, poverty rate, and felony crime rate. Neighborhood poverty (64, 65), and neighborhood violence are related to asthma. (8, 9, 45, 66-68). The proportion of tree canopy or trees, a measure of surface area covered by overhanging vegetation, is often recognized for its health benefits (69), though this is not always the case. (70) Neighborhood asthma hospitalization rates may signal differential access to health care, neighborhood resources, or polluting sources. (16) Considerable literature in environmental health explains that proximity to concentrations of noxious particles released by vehicles may exacerbate asthma development and severity (12, 68, 71-75); GIS traffic measures are often used as proxies to capture exposure to traffic-related pollutants associated with asthma. (76-79) Lastly, research suggests that housing violations may be related to asthma morbidity. (35, 80)
We hypothesized that these neighborhood-level characteristics are associated with the presence of indoor allergens in the household.
Methods
We examined the relationship between neighborhood-level characteristics and indoor allergens using data from the Puerto Rican Asthma Project (PRAP). Puerto Ricans are one of the racial/ethnic groups most severely affected by asthma in the United States. (40, 81-90) The PRAP is a prospective birth cohort of Puerto Rican children born in New York City (NYC) – primarily in the Bronx – who were at risk for development of childhood asthma. Full study details have been discussed previously. (91) Briefly, 274 mothers, and their newborns, completed the initial baseline home visit (the source of allergen measurements for this paper) which occurred within a few weeks after the birth of their child. Participant mothers answered questions on behalf of her household and child in either Spanish or English. A team of two technicians, one of whom was bilingual (Spanish/English), collected environmental samples and administered a questionnaire to the mother. During this baseline visit, the surface of the mother's bed was vacuumed for three minutes and samples were analyzed for dust mite (Der f 1), cockroach (Bla g 2), cat (Fel d 1), and mouse (MUP) allergens as previously described by Acosta, et al (2008).
At baseline, 12 participants were excluded because they were not available in OASIS (New York City Open Accessible Space Information System Cooperative). Of these 12, eight lived outside the five NYC boroughs and four addresses could not be located in OASIS. An additional participant was dropped from analyses because a sibling was already enrolled in the study. Thus, at baseline, 261 participants remained for analysis. The Human Subjects Committee at the Harvard School of Public Health and at Columbia University Medical Center approved this study.
Allergen Outcome Measures
Allergen levels were ln-transformed to approximate normality in linear regression models that examined associations with neighborhood-levels characteristics. Categorical analysis (logistic regression) was also used to explore previously published allergen level thresholds for allergic sensitization, when possible (cockroach >1 U/g [1 unit = 40 ng] and mouse > 1.6 μg/g); and if this was not possible, the detection limits of the relevant immunoassay were used (dust mite > 0.25 μg/g; cat > 1 μg/g). (29, 30, 39, 41, 49, 92)
Neighborhood Exposure Measures
Neighborhood was defined as a NYC community planning district, a spatial unit created by the New York Department of City Planning used to organize new and redeveloping projects. NYC has 59 community districts, and the average population in each community district was 135, 734. The Bronx, where the majority of study participants lived, has 12 community districts. (93) The average population of community districts in the Bronx was 106,775. Neighborhood-level data were collected from the OASIS database (www.oasisnyc.net) from March-April 2007 using participants’ addresses. (69) The neighborhood characteristics from OASIS were percent tree canopy (measure of tree canopy cover: amount of surface area covered by overhanging vegetation) and asthma hospitalizations per 1000 children. OASIS is a web-based Geographic Information Systems (GIS) mapping resource for NYC. It is a partnership of more than 30 federal, state, and local agencies, private companies, academic institutions, and nonprofit organizations, creating a one-stop, interactive mapping and data analysis application via the Internet. Each participant address was entered into the OASIS mapping system to collect neighborhood characteristics data. Each address was entered a minimum of three different times, when necessary. If the address still could not be located, the participant was dropped from the analysis. All study participant addresses were geocoded by the commercial geocoding firm, Mapping Analytics. (94) Neighborhood characteristics data were also collected from The State of New York City's Housing and Neighborhoods, 2006 (The Furman Center for Real Estate and Urban Policy). (95) These characteristics were serious housing code violations per 1000 rental units (a serious violation is a Class C [immediately hazardous] assigned by the NYC Department of Housing Preservation and Development), poverty rate (calculated by the NYC Housing and Vacancy Survey using income data, and income cutoffs or “poverty thresholds”), and the felony crime rate per 1000 people (the seven major felony crimes used are: burglary, larceny, motor vehicle theft, murder, rape, robbery, and assault). (69, 95) In ArcGIS 9.2, using StreetMap USA, we calculated distance to nearest highway from residences, and congestion (96) and mean roadway length within a 100 meter radius of participants’ residences. (97) These measurements were not available at the community district level. In this study, participants’ traffic exposures were standardized across measures, and the one with the best variability for this cohort was used; here, this was mean roadway length within a 100 meter radius of participants’ residences. (79) For both roadway length and serious housing code violations, we created three categories for analysis, spreading the data out as evenly as possible across the three groups. We reached an even spread with roadway length, achieving tertiles (n=87, 87, 87); however serious housing code violations could not be divided into tertiles due to the number participants who had the same amount of violations, overlapping across categories. Therefore, as a category, serious housing violations, was grouped as follows: n=70, 91, 99.
Covariates
Mother's education and household income were measured in the baseline interview survey and were dichotomized: education (≤ high school graduate (referent) or ≥ some college); household income ((≤ $39,999 (referent) or ≥ $40,000+). Building-level violations for each address were collected by linking to the NYC Department of Buildings (DOB), Property Profile Overview to obtain the number and type of violation for each address. (98) An Environmental Control Board (ECB) violation is a notice that a property does not comply with a provision of the NYC Building Code and/or NYC Zoning Resolution, and such violations are resolved at the Environmental Control Board, an administrative law court where a violator must (a) pay a civil penalty and correct the violating condition, and (b) file a Certificate of Correction with the DOB. (99) Violations were standardized by building age and number of units in the building, and then multiplied by 100 for ease of interpretability.
Sociodemographic Variables
During the baseline interview survey, participants’ mothers were asked their about marital status (married, divorced, separated, widowed, never been married), birth place (Mainland, USA, Puerto Rico, Dominican Republic, Mexico, Other), and how long they had been in the U.S. (number of years).
Analysis
We evaluated the association (p<0.05) between neighborhood exposures and allergen levels, using bivariate and multivariable linear regression, as well as logistic regression for allergen threshold levels as specified earlier. Possible confounders (income and education) were included in all subsequent analyses.
In initial bivariate linear models we examined the relationship of each neighborhood exposure to the allergen levels. The first set of multivariable linear models examined the same relationships, while also adjusting for income and education. The next set of multivariable analyses examined social neighborhood exposures, and then environmental neighborhood exposures, in relation to the allergen levels. We then explored fully adjusted multivariable models, where each parameter estimate was adjusted for all other predictor variables in the model, including income and education. All ratios and 95% confidence intervals for linear models were back-transformed to represent the original allergen scales instead of log-scales.
We also fitted multivariable logistic models for each allergen according to its limit of detection or allergic sensitization cutpoint, as found in the literature (dust mite: >0.25 μg/g; cat: >1 μg/g; cockroach: >1 U/g [40 ng/g]; mouse: >1.6 μg/g). (29, 30, 39, 41, 49, 92) In addition to following the modeling strategy described above for multivariable linear regression, in multivariable logistic models, we also adjusted for building-level violations (ECB + DOB violations). Lastly, we examined spatial representations of neighborhood characteristics and the outcomes in ArcGIS 9.2. All other analyses were performed in SAS 9.1 and JMP 7.0. (100, 101)
Results
Sample
Most mothers had never been married (64.8%) and were born on the Mainland USA (73.6%), while 20.7% were born in Puerto Rico. In addition, 56.3% of mothers had a high school education or less and 80.8% lived in households where the combined family income was less than $39,999/year. In participants’ neighborhoods, the average percent of tree canopy was 10.3, and the average asthma hospitalization rate per 1000 children was 16.7. Participants’ buildings had an average of 555.3 meters of roadway within a 100 meter radius of their buildings. Participants’ neighborhoods were also characterized by an average of 106.4 serious housing code violations per 1000 rental units, a neighborhood poverty rate of 30.2%, and a felony crime rate of 31.2% per 1000 people. (Table 1) NYC community districts where participants lived were compared to NYC community districts where no study participants lived to examine study exposures. We found that community districts where study participants lived generally shared a higher burden of neighborhood-level characteristics that have been shown to relate to asthma in the neighborhood literature. (8, 35, 65, 67-70, 72, 79, 80, 102) Study participants lived in community districts that had 4% more tree canopy, a 136% higher asthma hospitalization rate, a 164% higher housing code violations rate, a 68% higher poverty rate, and an 11% higher felony crime rate than those community districts where there were no study participants. (Table 2)
Table 1.
Demographic and Neighborhood-Level Characteristics (n=261)
| Built Environment Neighborhood Exposures | Mean | SD | Missing |
|---|---|---|---|
| % Tree Canopy | 10.33 | 5.26 | -- |
| Asthma Hospitalization Rate per 1000 children | 16.67 | 4.88 | -- |
| Mean Roadway Length within 100 meter radius of bldg | 555.30 | 146.30 | -- |
| Mean Roadway Length within 100m (meters) | 396.41 | 69.68 | |
| Mean Roadway Length within 100m (meters) | 556.18 | 35.94 | |
| Mean Roadway Length within 100m (meters) | 713.32 | 88.05 | |
| Housing Code Violations per 1000 people | 106.36 | 61.63 | 1 |
| Housing Code Violations per 1000 people | 39.04 | 17.79 | |
| Housing Code Violations per 1000 people | 78.79 | 18.95 | |
| Housing Code Violations per 1000 people | 179.29 | 13.03 |
| Social Environment Neighborhood Exposures | Mean | SD | Missing |
|---|---|---|---|
| Poverty Rate | 30.23 | 9.93 | 1 |
| Felony Crime Rate per 1000 people | 31.24 | 7.40 | 1 |
| Mother's Demographic Characteristics | N | % | Missing |
|---|---|---|---|
| Marital Status | -- | ||
| Married | 75 | 28.74 | |
| Divorced | 7 | 2.68 | |
| Separated | 9 | 3.45 | |
| Widowed | 1 | 0.38 | |
| Never been married | 169 | 64.75 | |
| Maternal Birthplace | -- | ||
| Mainland USA | 192 | 73.56 | |
| Puerto Rico | 54 | 20.69 | |
| Dominican Republic | 10 | 3.83 | |
| Mexico | 2 | 0.77 | |
| Other | 3 | 1.15 | |
| Education | -- | ||
| High school grad or equivalent, or less | 147 | 56.32 | |
| Some college or more | 114 | 43.68 | |
| Income | -- | ||
| ≤ $39,999 | 211 | 80.84 | |
| $40,000+ | 50 | 19.16 |
| Mean | SD | Missing | |
|---|---|---|---|
| Maternal Years in Mainland U.S. | 23.44 | 7.12 | -- |
Table 2.
Comparisons between New York City (NYC) and Puerto Rican Asthma Project Community District Weighted Averages
| All NYC Community Districts (59) | Non Puerto Rican Asthma Project Community Districts (42) | Puerto Rican Asthma Project Commuity Districts (17) | Puerto Rican Asthma Project Bronx Only Community Districts (12) | |
|---|---|---|---|---|
| NYC Community District Exposures | ||||
| % Tree Canopy | 12.93 | 12.8 | 13.34 | 11.81 |
| Asthma Hospitalization Rate per 1000 children | 8.91 | 6.69 | 15.76 | 15.83 |
| Housing Code Violations per 1000 rental units | 50.96 | 36.38 | 96.03 | 102.85 |
| Poverty Rate | 17.94 | 15.38 | 25.83 | 28.58 |
| Felony Crime Rate per 1000 people | 27.26 | 26.55 | 29.48 | 29.35 |
Descriptive statistics of the indoor allergens are presented in Table 3. When dust mite allergen was detected, the concentrations were low compared with those of cockroach, mouse and cat allergens. The variation in cat allergen was markedly greater than that of the other allergens. Some homes were missing dust samples, primarily because not enough dust was collected from the bed surface.
Table 3.
Indoor Allergens at Baseline
| N | Median | Missing | Geometric Mean | Geometric SD | |
|---|---|---|---|---|---|
| Der f 1 μg/g (dust mite) | 245 | 0.125 | 16 | 0.20 | 2.98 |
| Fel d 1 μg/g (cat) | 253 | 0.48 | 8 | 0.64 | 7.66 |
| Bla g 2 U/g* (cockroach) | 221 | 0.50 | 40 | 1.46 | 4.10 |
| MUP μg/g (mouse) | 241 | 0.38 | 20 | 0.63 | 2.81 |
Bla g 2 U/g [40 ng/g]
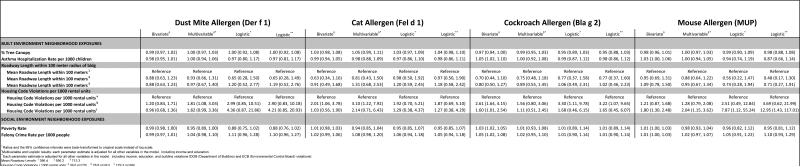
Multivariable Analysis
Dust mite (Der f 1)
As can be seen in Table 4, no statistically significant associations were found in any bivariate models between dust mite and neighborhood-level characteristics. In fully-adjusted models, a statistically significant association was found between a medium level of serious housing code violations and the presence of dust mite allergen (1.81, 95%CI: 1.08, 3.03). When dust mite allergen was dichotomized into a level of detectable vs. not detectable, it was no longer associated with a medium level of serious housing code violations in fully adjusted models.
Table 4.
Bivariate and multivariable associations of neighborhood characteristics and indoor allergens: Puerto Rican Asthma Project (n=261)
|
Cats (Fel d 1)
As can be seen in Table 5, a bivariate statistically significant relationship was found between a medium level of housing code violations and cat allergen (2.01, 95%CI: 1.06, 3.78). This association was maintained in fully adjusted models (3.10, 95%CI: 1.22, 7.92). When at allergen was dichotomized using as a cutpoint levels >1 μg/g, it was no longer associated with medium levels of serious housing code violations in fully adjusted models.
Cockroaches (Bla g 2)
As can be seen in Table 6, in bivariate models, statistically significant associations were found between the asthma hospitalization rate per 1000 children (1.05, 95%CI: 1.02, 1.10), a medium (2.61, 95%CI: 1.64, 4.15) and a high (1.60, 95%CI: 1.01, 2.54) level of serious housing code violations, the poverty rate (1.03, 95%CI: 1.02, 1.05), and the felony crime rate (1.05, 95%CI: 1.02, 1.08), and the presence of cockroach allergen. None of these associations remained statistically significant in fully adjusted analyses. In logistic regression analysis, a medium level of housing code violations was associated with cockroach allergen at levels >1 U/g [40 ng/g] in fully adjusted models (3.30, 95%CI: 1.11, 9.78).
Mice (MUP)
As can be seen in Table 7, statistically significant associations were found in bivariate models between the asthma hospitalization rate (1.03, 95%CI: 1.00, 1.06), a high level of serious housing code violations (1.80, 95%CI: 1.30, 2.48), and the poverty rate (1.01, 95%CI: 1.00, 1.03) and mouse allergen levels. Only the association between a high level of serious housing code violations mouse allergens persisted in fully adjusted models (2.04, 95%CI: 1.15, 3.62). In logistic regression analysis, a high level of serious housing code violations was associated with mouse allergen at levels >1.6 μg/g in fully adjusted models (7.87, 95% CI: 1.12, 55.24).
Adjusting for Building-Level Violations
As can be seen in Tables 4-7, in multivariable logistic models, statistically significant associations between neighborhood-level housing violations and indoor allergens persisted after adjusting for building-level violations A medium level of neighborhood serious housing code violations was statistically significantly associated with cockroach allergen after adjusting for DOB and ECB building level housing violations separately. A high level of serious neighborhood housing code violations was statistically significantly associated with mouse allergen after adjusting for building level housing code violations.
Discussion
Our primary objective was to determine if any relationship existed between neighborhood characteristics and the presence of indoor allergens, since this had not been previously studied. We examined the relationship between various neighborhood-level predictors and the presence of indoor allergens in the household, even after adjusting for building-level housing code violations. Previous studies have explored the relationship between housing conditions and indoor allergens. Concerning dust mite and cat allergen, previous literature has been inconsistent in its reporting of the relationship between housing conditions and the presence of these allergens. Therefore it is difficult to assess whether our results demonstrating an association between neighborhood-level housing code violations and dust mite/cat allergens in multivariate linear models is consistent with previous findings concerning the housing unit level. (103)
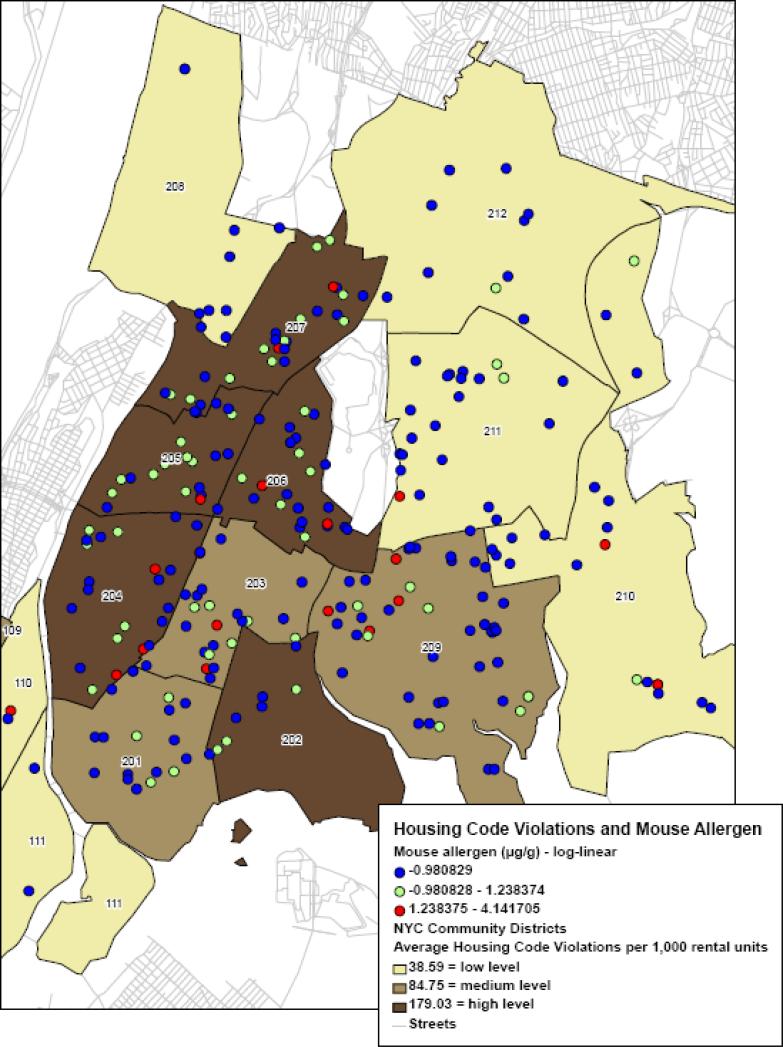
Previous studies have found a relationship between poor housing conditions and the presence of cockroach allergen (35, 58, 104) and elevated mouse allergen. (58, 104) We demonstrated an association between cockroach and mouse allergen, and the prevalence of housing code violations at the neighborhood level even after adjusting for building level housing code violations. Graphically, the relationship between serious housing code violations and the presence of mouse allergen can be seen in Figure 1, which shows neighborhoods with high levels of housing code violations to overlap neighborhoods with higher levels of mouse allergen. Overall, these relationships suggest that, where many of the leading indoor allergens are concerned, we may need to consider prevention and treatment options at the neighborhood-level. Though more work is needed to determine the relationship between neighborhood factors and the presence of allergens, it seems that reducing serious housing code violations may decrease exposure to allergens, which are related allergic sensitization and asthma.
Figure 1.
Housing Code Violations and Mouse Allergen (MUP), Bronx, New York
This study had a few limitations. First, while this was a prospective birth cohort, we only assessed allergen measurements and neighborhood-level characteristics cross-sectionally. Therefore, no causal statements can be made. Furthermore, these analyses were limited to a small baseline cohort sample (N=261) of Puerto Rican participants with a history of mother inhalant allergy or asthma. Therefore, we can not generalize beyond this population. Furthermore, limitations existed in the actual measurement of exposures. Many neighborhood-level exposures were proxy variables, (e.g. mean roadway length), while still other relevant variables were unavailable (e.g. specific types of neighborhood housing code violations). Since one of our major findings was the importance of neighborhood-level housing code violations, it seemed important to adjust for building-level violations to see if this mediated any of the neighborhood level effect. It did not, and in fact, adjusting for building-level violations strengthened the neighborhood effect.
However, it is clear that the neighborhood-level and building-level housing code violations were not drawn in the same way in the New York City data systems we used for this analysis. Furthermore, even though we did not achieve perfect tertiles with the serious housing code violations variable, the amount of violations in the medium and high categories were so egregious that such findings seem plausible given previous literature, and subsequent analyses controlling for building-level house code violations. Lastly, since some participants were missing dust samples, because not enough dust was drawn, results could be biased. Yet allergen levels in this study were comparable to other New York City studies examining indoor allergens. (39, 58) Compared to other non New York City-specific studies measuring indoor allergens, our levels of cat and dust allergen were generally low, while levels of cockroach and mouse allergen were generally high. The levels in our study are not comparable to national data, since such data are less representative of urban areas with high population density and high density of high-rise buildings. (37, 41, 46, 105)
Despite these limitations, this work suggests avenues for additional research. First, future research should further explore the association between neighborhood-level characteristics and the presence of indoor allergens. Currently, neighborhood-level factors are not considered in asthma prevention strategies. For example, the most recent “Guidelines for the Diagnosis and Management of Asthma” from the National Asthma Education and Prevention Program does not discuss neighborhood-level factors. (106) However, Wright and colleagues have discussed neighborhood factors in terms of asthma prevention. (8, 67, 107, 108)
Increasingly, urban planning and public health researchers and practitioners are aware of the need for collaboration between these two fields. (16, 109-114) This study suggests some ways in which such collaborations may happen. For example, the New York City Department of City Planning can target “high-risk” community districts (those with high levels of housing code violations, for example). The Department could include a health objective on future building and planning bids, and require future projects to discuss how a new project would solve, prevent, or alleviate health concerns. For example, if a developer is interested in creating a new mixed-use space in the Bronx near the Cross-Bronx Expressway, she would need to explain how the firm is taking measures to mitigate the harmful air and noise pollution byproducts of the expressway that might be experienced by future commercial and residential tenants. In addition, she might explain how the project would prevent dust from spreading into neighboring areas while the project is being constructed, and how the project plans to minimize construction noise. In partnership with the NYC Department of Mental Health and Hygiene, and the Department of City Planning, the City of New York could be a model for consciously combining these issues of the built environment and health into its work practice. The Furman Center has several data indicators at the community district level which can be helpful to projects which consider both built environment and health issues; these indicators include elevated blood lead levels, infant mortality rate, low birth weight rate, severe crowding rate, tax delinquencies, racial diversity index, rental units that are subsidized, and residential units within ¼ mile of a park. (95)
Future studies should incorporate a larger city-wide, or nationally, representative sample of U.S. participants to further clarify the relationship between neighborhood characteristics and asthma morbidity and mortality. The focus on Puerto Ricans in this study was important, since the asthma burden is so high in this population, but future studies should aim to clarify the relationship of neighborhood-level issues and asthma morbidity in a representative sample. The use of multilevel modeling will help to isolate neighborhood, building and individual level effects. (115)
Such future studies should also further extend the measurement of neighborhood characteristic variables, which was not possible in this study. Though it is certainly positive that the area level data used in this study was publicly available, we need to continue working toward fuller measurement. Future studies might more precisely examine the relationship between neighborhood traffic pollutants (116-119), specific types of housing code violations (35, 80) and asthma morbidity. For example, available data on serious housing code violations may have actually underestimated the relationship with asthma-related allergens since it only pertained to one class of housing violations, and did not include NYC public housing. (120) Future studies should both collect their own neighborhood-level data, and request more publicly available data from governmental entities, e.g. housing and planning agencies.
The definition of neighborhood is also an important issue for future work. Two important concerns informed the decision to use community planning districts as the spatial unit in our work, although most current thought in spatial epidemiology suggests the use of smaller spatial areas (e.g. census tracts). (121) First, the sample size was too small to consider spatial areas aside from these districts; it would have been difficult to consider participants’ outcomes and area level issues if so few of them were within each spatial unit. (122) Second, the NYC Department of City Planning uses these districts to design and implement redevelopment as well as new building and neighborhood projects. Therefore, districts are spatial units with policy and planning relevance, and employing them in public health research may serve as a vehicle to link health issues to indicators regularly maintained by government officials, including information on housing types, parks, vacant land, commercial space, and facilities. (123-125)
City agencies, such as health departments, transportation and planning boards, the police, and housing authority, wield a good deal of power over the health of neighborhood residents. Community district policies regarding incentives for landlords for fewer housing violations and quicker remediation if violations occur might be useful remedies to reduce asthma burden. Likewise, planning boards might instruct architects and developers to explicitly incorporate health objectives into their design plans. A health lens needs could be used to assess the possible health effects of urban polices and programs, for example through the application of a methodology such as Health Impact Assessment.
Acknowledgments
We thank the Puerto Rican Asthma Project research participants and staff for their time and effort, especially Dr. Luis Acosta and Marianne Turner. We also thank Jeff Blossom for creating variables and maps in ArcGIS 9.2, and Amy Cohen for her SAS programming expertise. This work was supported by NIEHS grants R01 ES 10922 and P30 ES 009089.
Footnotes
Declaration of Interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Kawachi I, Berkman LF. Neighborhoods and Health. Oxford University Press; New York: 2003. [Google Scholar]
- 2.Caughy MO, Nettles SM, O'Campo PJ, Lohrfink KF. Neighborhood matters: racial socialization of African American children. Child Dev. 2006;77(5):1220–36. doi: 10.1111/j.1467-8624.2006.00930.x. [DOI] [PubMed] [Google Scholar]
- 3.Caughy MO, Nettles SM, O'Campo PJ. The effect of residential neighborhood on child behavior problems in first grade. Am J Community Psychol. 2008;42(1-2):39–50. doi: 10.1007/s10464-008-9185-9. [DOI] [PubMed] [Google Scholar]
- 4.Molnar B, Cerda M, Buka S, Roberts A. Effects of Neighborhood Resources on Agression and Delinquent Behaviors Among Urban Youths. American Journal of Public Health. 2008;98:1086–1093. doi: 10.2105/AJPH.2006.098913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akinbami L. The State of Childhood Asthma, United States, 1980-2005. CDC - Office of Analysis and Epidemiology; Atlanta, GA: 2006. [PubMed] [Google Scholar]
- 6.NCHS C-. CDC - NCHS - Fast Facts: Asthma (adult morbidity) Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2005, Tables 3 and 4, Appendix III, Table V: CDC. 2008 [Google Scholar]
- 7.NCHS C-. CDC - NCHS - Fast Facts: Asthma (child morbidity) Summary Health Statistics for U.S. Children: National Health Interview Survey, 2006, Table 1, Appendix III, Table IV: CDC. 2008 [Google Scholar]
- 8.Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, et al. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94(4):625–32. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeffrey J, Sternfeld I, Tager I. The association between childhood asthma and community violence, Los Angeles County, 2000. Public Health Rep. 2006;121(6):720–8. doi: 10.1177/003335490612100612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oyana TJ, Rogerson P, Lwebuga-Mukasa JS. Geographic clustering of adult asthma hospitalization and residential exposure to pollution at a United States-Canada border crossing. Am J Public Health. 2004;94(7):1250–7. doi: 10.2105/ajph.94.7.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heinrich J, Gehring U, Cyrys J, Brauer M, Hoek G, Fischer P, et al. Exposure to traffic related air pollutants: self reported traffic intensity versus GIS modelled exposure. Occup Environ Med. 2005;62(8):517–23. doi: 10.1136/oem.2004.016766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007;29(5):879–88. doi: 10.1183/09031936.00083406. [DOI] [PubMed] [Google Scholar]
- 13.Meng YY, Wilhelm M, Rull RP, English P, Ritz B. Traffic and outdoor air pollution levels near residences and poorly controlled asthma in adults. Ann Allergy Asthma Immunol. 2007;98(5):455–63. doi: 10.1016/S1081-1206(10)60760-0. [DOI] [PubMed] [Google Scholar]
- 14.McEntee JC, Ogneva-Himmelberger Y. Diesel particulate matter, lung cancer, and asthma incidences along major traffic corridors in MA, USA: A GIS analysis. Health Place. 2008 doi: 10.1016/j.healthplace.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 15.Cagney KA, Browning CR. Exploring neighborhood-level variation in asthma and other respiratory diseases: the contribution of neighborhood social context. J Gen Intern Med. 2004;19(3):229–36. doi: 10.1111/j.1525-1497.2004.30359.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corburn J, Osleeb J, Porter M. Urban asthma and the neighbourhood environment in New York City. Health Place. 2006;12(2):167–79. doi: 10.1016/j.healthplace.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Pearlman DN, Zierler S, Meersman S, Kim HK, Viner-Brown SI, Caron C. Race disparities in childhood asthma: does where you live matter? J Natl Med Assoc. 2006;98(2):239–47. [PMC free article] [PubMed] [Google Scholar]
- 18.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(5 Suppl):757S–769S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]
- 19.Gupta RS, Zhang X, Sharp LK, Shannon JJ, Weiss KB. Geographic variability in childhood asthma prevalence in Chicago. J Allergy Clin Immunol. 2008 doi: 10.1016/j.jaci.2007.11.036. [DOI] [PubMed] [Google Scholar]
- 20.Laditka JN, Laditka SB. Race, ethnicity and hospitalization for six chronic ambulatory care sensitive conditions in the USA. Ethn Health. 2006;11(3):247–63. doi: 10.1080/13557850600565640. [DOI] [PubMed] [Google Scholar]
- 21.Carr W, Zeitel L, Weiss K. Variations in asthma hospitalizations and deaths in New York City. Am J Public Health. 1992;82(1):59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Litonjua AA, Carey VJ, Weiss ST, Gold DR. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pediatr Pulmonol. 1999;28(6):394–401. doi: 10.1002/(sici)1099-0496(199912)28:6<394::aid-ppul2>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 23.Lanphear BP, Kahn RS, Berger O, Auinger P, Bortnick SM, Nahhas RW. Contribution of residential exposures to asthma in us children and adolescents. Pediatrics. 2001;107(6):E98. doi: 10.1542/peds.107.6.e98. [DOI] [PubMed] [Google Scholar]
- 24.Chaudhuri N. Interventions to improve children's health by improving the housing environment. Rev Environ Health. 2004;19(3-4):197–222. [PubMed] [Google Scholar]
- 25.Gruchalla RS, Pongracic J, Plaut M, Evans R, 3rd, Visness CM, Walter M, et al. Inner City Asthma Study: relationships among sensitivity, allergen exposure, and asthma morbidity. J Allergy Clin Immunol. 2005;115(3):478–85. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 26.Jaakkola N, Ruotsalainen R, Jaakkola JJ. What are the determinants of children's exposure to environmental tobacco smoke at home? Scand J Soc Med. 1994;22(2):107–12. doi: 10.1177/140349489402200205. [DOI] [PubMed] [Google Scholar]
- 27.Malveaux FJ, Fletcher-Vincent SA. Environmental risk factors of childhood asthma in urban centers. Environ Health Perspect. 1995;103(Suppl 6):59–62. doi: 10.1289/ehp.95103s659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Platt-Mills TA, Sporik RB, Chapman MD, Heymann PW. The role of indoor allergens in asthma. Allergy. 1995;50(22 Suppl):5–12. doi: 10.1111/j.1398-9995.1995.tb02729.x. [DOI] [PubMed] [Google Scholar]
- 29.Sarpong SB, Hamilton RG, Eggleston PA, Adkinson NF., Jr Socioeconomic status and race as risk factors for cockroach allergen exposure and sensitization in children with asthma. J Allergy Clin Immunol. 1996;97(6):1393–401. doi: 10.1016/s0091-6749(96)70209-9. [DOI] [PubMed] [Google Scholar]
- 30.Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336(19):1356–63. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 31.Yang CY, Tien YC, Hsieh HJ, Kao WY, Lin MC. Indoor environmental risk factors and childhood asthma: a case-control study in a subtropical area. Pediatr Pulmonol. 1998;26(2):120–4. doi: 10.1002/(sici)1099-0496(199808)26:2<120::aid-ppul8>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 32.Eggleston PA, Buckley TJ, Breysse PN, Wills-Karp M, Kleeberger SR, Jaakkola JJ. The environment and asthma in U.S. inner cities. Environ Health Perspect. 1999;107(Suppl 3):439–50. doi: 10.1289/ehp.99107s3439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gergen PJ, Mortimer KM, Eggleston PA, Rosenstreich D, Mitchell H, Ownby D, et al. Results of the National Cooperative Inner-City Asthma Study (NCICAS) environmental intervention to reduce cockroach allergen exposure in inner-city homes. J Allergy Clin Immunol. 1999;103(3 Pt 1):501–6. doi: 10.1016/s0091-6749(99)70477-x. [DOI] [PubMed] [Google Scholar]
- 34.Phipatanakul W, Eggleston PA, Wright EC, Wood RA. Mouse allergen. II. The relationship of mouse allergen exposure to mouse sensitization and asthma morbidity in inner-city children with asthma. J Allergy Clin Immunol. 2000;106(6):1075–80. doi: 10.1067/mai.2000.110795. [DOI] [PubMed] [Google Scholar]
- 35.Rauh VA, Chew GR, Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ Health Perspect. 2002;110(Suppl 2):323–7. doi: 10.1289/ehp.02110s2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vojta PJ, Friedman W, Marker DA, Clickner R, Rogers JW, Viet SM, et al. First National Survey of Lead and Allergens in Housing: survey design and methods for the allergen and endotoxin components. Environ Health Perspect. 2002;110(5):527–32. doi: 10.1289/ehp.02110527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arbes SJ, Jr., Cohn RD, Yin M, Muilenberg ML, Burge HA, Friedman W, et al. House dust mite allergen in US beds: results from the First National Survey of Lead and Allergens in Housing. J Allergy Clin Immunol. 2003;111(2):408–14. doi: 10.1067/mai.2003.16. [DOI] [PubMed] [Google Scholar]
- 38.Arbes SJ, Jr., Sever M, Archer J, Long EH, Gore JC, Schal C, et al. Abatement of cockroach allergen (Bla g 1) in low-income, urban housing: A randomized controlled trial. J Allergy Clin Immunol. 2003;112(2):339–45. doi: 10.1067/mai.2003.1597. [DOI] [PubMed] [Google Scholar]
- 39.Chew GL, Perzanowski MS, Miller RL, Correa JC, Hoepner LA, Jusino CM, et al. Distribution and determinants of mouse allergen exposure in low-income New York City apartments. Environ Health Perspect. 2003;111(10):1348–51. doi: 10.1289/ehp.6124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Findley S, Lawler K, Bindra M, Maggio L, Penachio MM, Maylahn C. Elevated asthma and indoor environmental exposures among Puerto Rican children of East Harlem. J Asthma. 2003;40(5):557–69. doi: 10.1081/jas-120019028. [DOI] [PubMed] [Google Scholar]
- 41.Arbes SJ, Jr., Cohn RD, Yin M, Muilenberg ML, Friedman W, Zeldin DC. Dog allergen (Can f 1) and cat allergen (Fel d 1) in US homes: results from the National Survey of Lead and Allergens in Housing. J Allergy Clin Immunol. 2004;114(1):111–7. doi: 10.1016/j.jaci.2004.04.036. [DOI] [PubMed] [Google Scholar]
- 42.Hynes HP, Brugge D, Osgood ND, Snell J, Vallarino J, Spengler J. Investigations into the indoor environment and respiratory health in Boston public housing. Rev Environ Health. 2004;19(3-4):271–89. [PubMed] [Google Scholar]
- 43.Berghout J, Miller JD, Mazerolle R, O'Neill L, Wakelin C, Mackinnon B, et al. Indoor environmental quality in homes of asthmatic children on the Elsipogtog Reserve (NB), Canada. Int J Circumpolar Health. 2005;64(1):77–85. doi: 10.3402/ijch.v64i1.17956. [DOI] [PubMed] [Google Scholar]
- 44.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26:89–113. doi: 10.1146/annurev.publhealth.26.021304.144528. [DOI] [PubMed] [Google Scholar]
- 45.Byrd RS, Joad JP. Urban asthma. Curr Opin Pulm Med. 2006;12(1):68–74. doi: 10.1097/01.mcp.0000199001.68908.45. [DOI] [PubMed] [Google Scholar]
- 46.Cohn RD, Arbes SJ, Jr., Jaramillo R, Reid LH, Zeldin DC. National prevalence and exposure risk for cockroach allergen in U.S. households. Environ Health Perspect. 2006;114(4):522–6. doi: 10.1289/ehp.8561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Warman K, Silver EJ, Wood PR. Asthma risk factor assessment: what are the needs of inner-city families? Ann Allergy Asthma Immunol. 2006;97(1 Suppl 1):S11–5. doi: 10.1016/s1081-1206(10)60779-x. [DOI] [PubMed] [Google Scholar]
- 48.Liu AH. Hygiene theory and allergy and asthma prevention. Paediatr Perinat Epidemiol. 2007;21(Suppl 3):2–7. doi: 10.1111/j.1365-3016.2007.00878.x. [DOI] [PubMed] [Google Scholar]
- 49.Call R, Smith TF, Morris E, Chapman MD, Platts-Mills TAE. Risk factors for asthma in inner city children. J Pediatr. 1992;121:862–866. doi: 10.1016/s0022-3476(05)80329-4. [DOI] [PubMed] [Google Scholar]
- 50.Gelber L, Seltzer LH, Bouzoukis JK, Pollart SM, Chapman MD, Platts-Mills TAE. Sensitization and exposure to indoor allergens as risk factors for asthma among patients presenting to hospital. Am Rev Respir Dis. 1993;147(573-578) doi: 10.1164/ajrccm/147.3.573. [DOI] [PubMed] [Google Scholar]
- 51.Arruda L, Vailes LD, Ferriani VPL, Santos ABR, Pomes A, Chapman MD. Cockroach allergens and asthma. J Allergy Clin Immunol. 2001;107:419–428. doi: 10.1067/mai.2001.112854. [DOI] [PubMed] [Google Scholar]
- 52.TePas E, Litonjua AA, Celedon JC, Sredl D, Gold DR. Sensitization to Aeroallergens and Airway Hyperresponsiveness at 7 Years of Age. Chest. 2006;129:1500–1508. doi: 10.1378/chest.129.6.1500. [DOI] [PubMed] [Google Scholar]
- 53.Erwin E, Wickens K, Custis NJ, Siebers R, Woodfolk J, Barry D, Crane J, Platts-Mills TAE. Cat and dust mite sensitivity and tolerance in relation to wheezing among chidlren raised with high exposure to both allergens. J Allergy Clin Immunol. 2005;115:74–79. doi: 10.1016/j.jaci.2004.10.030. [DOI] [PubMed] [Google Scholar]
- 54.Eggleston P, Rosenstreich D, Lynn H, Gergen P, Baker D, Kaltan M, et al. Relationship of indoor allergen exposure to skin test sensitivity in inner city children with asthma. J Allergy Clin Immunol. 1998;97(1393-1401) doi: 10.1016/s0091-6749(98)70272-6. [DOI] [PubMed] [Google Scholar]
- 55.Huss K, Adkinson NK, Eggleston PA, Dawson C, Van Natta ML, Hamilton RG. House dust mite and cockroach exposure are strong risk factors for positive allergy skin test responses in the Childhood Asthma Management program. J Allergy Clin Immunol. 2001;107:48–54. doi: 10.1067/mai.2001.111146. [DOI] [PubMed] [Google Scholar]
- 56.Prewitt E. Inner-City Health Care. Annals of Internal Medicine. 1997;126(6) [PubMed] [Google Scholar]
- 57.Karpati A, Kerker B, Mostashari F, Singh T, Hajat A, Thorpe L, Bassett M, Henning K, Frieden T. Health Disparities in New York City. New York City Department of Health and Mental Hygiene.; New York: 2004. [Google Scholar]
- 58.Chew GL, Carlton EJ, Kass D, Hernandez M, Clarke B, Tiven J, et al. Determinants of cockroach and mouse exposure and associations with asthma in families and elderly individuals living in New York City public housing. Ann Allergy Asthma Immunol. 2006;97(4):502–13. doi: 10.1016/S1081-1206(10)60942-8. [DOI] [PubMed] [Google Scholar]
- 59.Diette GB, Hansel NN, Buckley TJ, Curtin-Brosnan J, Eggleston PA, Matsui EC, et al. Home indoor pollutant exposures among inner-city children with and without asthma. Environ Health Perspect. 2007;115(11):1665–9. doi: 10.1289/ehp.10088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Peters JL, Levy JI, Rogers CA, Burge HA, Spengler JD. Determinants of allergen concentrations in apartments of asthmatic children living in public housing. J Urban Health. 2007;84(2):185–97. doi: 10.1007/s11524-006-9146-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Berg J, McConnell R, Milam J, Galvan J, Kotlerman J, Thorne P, et al. Rodent allergen in Los Angeles inner city homes of children with asthma. J Urban Health. 2008;85(1):52–61. doi: 10.1007/s11524-007-9232-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Peters JL, Muilenberg ML, Rogers CA, Burge HA, Spengler JD. Alternaria measures in inner-city, low-income housing by immunoassay and culture-based analysis. Ann Allergy Asthma Immunol. 2008;100(4):364–9. doi: 10.1016/S1081-1206(10)60600-X. [DOI] [PubMed] [Google Scholar]
- 63.Wang C, Abou El-Nour MM, Bennett GW. Survey of Pest Infestation, Asthma, and Allergy in Low-income Housing. J Community Health. 2008;33(1):31–9. doi: 10.1007/s10900-007-9064-6. [DOI] [PubMed] [Google Scholar]
- 64.Garg RKA, Leighton J, Perrin M, Shah M. Asthma Facts. Second Edition New York City Department of Health and Mental Hygiene; New York: 2003. [Google Scholar]
- 65.Babin SM, Burkom HS, Holtry RS, Tabernero NR, Stokes LD, Davies-Cole JO, et al. Pediatric patient asthma-related emergency department visits and admissions in Washington, DC, from 2001-2004, and associations with air quality, socio-economic status and age group. Environ Health. 2007;6:9. doi: 10.1186/1476-069X-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Graham-Bermann SA, Seng J. Violence exposure and traumatic stress symptoms as additional predictors of health problems in high-risk children. J Pediatr. 2005;146(3):349–54. doi: 10.1016/j.jpeds.2004.10.065. [DOI] [PubMed] [Google Scholar]
- 67.Wright RJ. Health effects of socially toxic neighborhoods: the violence and urban asthma paradigm. Clin Chest Med. 2006;27(3):413–21. v. doi: 10.1016/j.ccm.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 68.Clougherty JE, Levy JI, Kubzansky LD, Ryan PB, Suglia SF, Canner MJ, et al. Synergistic effects of traffic-related air pollution and exposure to violence on urban asthma etiology. Environ Health Perspect. 2007;115(8):1140–6. doi: 10.1289/ehp.9863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.OASIS-NYC . OASIS, New York City Open Accessible Space Information System Cooperative. OASIS, Center for Urban Research The Graduate Center/CUNY 365 Fifth Ave., Room 6202 New York, NY 10016; New York City: 2008. [Google Scholar]
- 70.Rundle A. Children Living in Areas with More Trees have Lower Asthma Prevalence. The Built Environment and Health Project; 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kinney PL, Aggarwal M, Northridge ME, Janssen NA, Shepard P. Airborne concentrations of PM(2.5) and diesel exhaust particles on Harlem sidewalks: a community-based pilot study. Environ Health Perspect. 2000;108(3):213–8. doi: 10.1289/ehp.00108213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nicolai T, Carr D, Weiland SK, Duhme H, von Ehrenstein O, Wagner C, et al. Urban traffic and pollutant exposure related to respiratory outcomes and atopy in a large sample of children. Eur Respir J. 2003;21(6):956–63. doi: 10.1183/09031936.03.00041103a. [DOI] [PubMed] [Google Scholar]
- 73.Zmirou D, Gauvin S, Pin I, Momas I, Sahraoui F, Just J, et al. Traffic related air pollution and incidence of childhood asthma: results of the Vesta case-control study. J Epidemiol Community Health. 2004;58(1):18–23. doi: 10.1136/jech.58.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Baxter LK, Clougherty JE, Laden F, Levy JI. Predictors of concentrations of nitrogen dioxide, fine particulate matter, and particle constituents inside of lower socioeconomic status urban homes. J Expo Sci Environ Epidemiol. 2007;17(5):433–44. doi: 10.1038/sj.jes.7500532. [DOI] [PubMed] [Google Scholar]
- 75.Meng YY, Wilhelm M, Rull RP, English P, Nathan S, Ritz B. Are frequent asthma symptoms among low-income individuals related to heavy traffic near homes, vulnerabilities, or both? Ann Epidemiol. 2008;18(5):343–50. doi: 10.1016/j.annepidem.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 76.Gehring U, Cyrys J, Sedlmeir G, Brunekreef B, Bellander T, Fischer P, et al. Traffic-related air pollution and respiratory health during the first 2 yrs of life. Eur Respir J. 2002;19(4):690–8. doi: 10.1183/09031936.02.01182001. [DOI] [PubMed] [Google Scholar]
- 77.Gordian ME, Haneuse S, Wakefield J. An investigation of the association between traffic exposure and the diagnosis of asthma in children. J Expo Sci Environ Epidemiol. 2006;16(1):49–55. doi: 10.1038/sj.jea.7500436. [DOI] [PubMed] [Google Scholar]
- 78.Maantay J. Asthma and air pollution in the Bronx: methodological and data considerations in using GIS for environmental justice and health research. Health Place. 2007;13(1):32–56. doi: 10.1016/j.healthplace.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 79.Clougherty J, Wright RJ, Baxter L, Levy JI. Land use regression modeling of intra-urban residential variability in multiple traffic-related air pollutants. Environ Health. 2008;7(17) doi: 10.1186/1476-069X-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.NYCDMHH NYCDoMHaH . HEALTH DEPARTMENT DETAILS ACTIONS IN RESPONSE TO ITS INVESTIGATION OF GREENWICH VILLAGE KFC/TACO BELL RODENT INFESTATION. Press Release; New York City: 2007. [Google Scholar]
- 81.Carter-Pokras OD, Gergen PJ. Reported asthma among Puerto Rican, Mexican-American, and Cuban children, 1982 through 1984. Am J Public Health. 1993;83(4):580–2. doi: 10.2105/ajph.83.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Crain EF, Weiss KB, Bijur PE, Hersh M, Westbrook L, Stein RE. An estimate of the prevalence of asthma and wheezing among inner-city children. Pediatrics. 1994;94(3):356–62. [PubMed] [Google Scholar]
- 83.Beckett WS, Belanger K, Gent JF, Holford TR, Leaderer BP. Asthma among Puerto Rican Hispanics: a multi-ethnic comparison study of risk factors. Am J Respir Crit Care Med. 1996;154(4 Pt 1):894–9. doi: 10.1164/ajrccm.154.4.8887582. [DOI] [PubMed] [Google Scholar]
- 84.Lara M, Morgenstern H, Duan N, Brook RH. Elevated asthma morbidity in Puerto Rican children: a review of possible risk and prognostic factors. West J Med. 1999;170(2):75–84. [PMC free article] [PubMed] [Google Scholar]
- 85.Homa DM, Mannino DM, Lara M. Asthma mortality in U.S. Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990-1995. Am J Respir Crit Care Med. 2000;161(2 Pt 1):504–9. doi: 10.1164/ajrccm.161.2.9906025. [DOI] [PubMed] [Google Scholar]
- 86.Diaz T, Sturm T, Matte T, Bindra M, Lawler K, Findley S, et al. Medication use among children with asthma in East Harlem. Pediatrics. 2000;105(6):1188–93. doi: 10.1542/peds.105.6.1188. [DOI] [PubMed] [Google Scholar]
- 87.Ledogar RJ, Penchaszadeh A, Garden CC, Iglesias G. Asthma and Latino cultures: different prevalence reported among groups sharing the same environment. Am J Public Health. 2000;90(6):929–35. doi: 10.2105/ajph.90.6.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Choudhry S, Burchard EG, Borrell LN, Tang H, Gomez I, Naqvi M, et al. Ancestry-environment interactions and asthma risk among Puerto Ricans. Am J Respir Crit Care Med. 2006;174(10):1088–93. doi: 10.1164/rccm.200605-596OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rose D, Mannino DM, Leaderer BP. Asthma prevalence among US adults, 1998-2000: role of Puerto Rican ethnicity and behavioral and geographic factors. Am J Public Health. 2006;96(5):880–8. doi: 10.2105/AJPH.2004.050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Carter-Pokras O, Zambrana RE, Poppell CF, Logie LA, Guerrero-Preston R. The environmental health of Latino children. J Pediatr Health Care. 2007;21(5):307–14. doi: 10.1016/j.pedhc.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Acosta LM, Acevedo-Garcia D, Perzanowski MS, Mellins R, Rosenfeld L, Cortes D, et al. The New York City Puerto Rican asthma project: study design, methods, and baseline results. J Asthma. 2008;45(1):51–7. doi: 10.1080/02770900701815784. [DOI] [PubMed] [Google Scholar]
- 92.Chew GL, Perzanowski MS, Canfield SM, Goldstein IF, Mellins RB, Hoepner LA, et al. Cockroach allergen levels and associations with cockroach-specific IgE. J Allergy Clin Immunol. 2008;121(1):240–5. doi: 10.1016/j.jaci.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 93.NYCDCP NYCDoCP . Community District Profiles. New York City: 2008. [Google Scholar]
- 94.Krieger NWP, Chen JT, Rehkopf DH, Subramanian SV. Geocoding and monitoring US socioeconomic inequalities in health: an introduction to using area-based socioeconomic measures -- The Public Health Disparities Geocoding Project monograph. Harvard School of Public Health; Boston, MA: [Google Scholar]
- 95.Armstrong A, Been V, Bhalla CK, Ellen IG, Ferraro CA, Greene SJ, Schuetz SJ, Voicur I. State of New York City's Housing and Neighborhoods. The Furman Center for Real Estate and Urban Policy; New York: 2006. 2006. [Google Scholar]
- 96.NYMTC NYMTC . Congestion Management System, 2005 Status Report. NYMTC; New York City: 2005. [Google Scholar]
- 97.ESRI . ArcGIS 9.2. ESRI; Redlands, CA: 2006. [Google Scholar]
- 98.NYCDOB NYC . Department of Buidlings. Property Profile Overview, Building Information System. New York: 2008. [Google Scholar]
- 99.Buildings NYCDo . New York City Department of Buildings, Buildings Information System: Environmental Control Board Violations. New York: 2005. [Google Scholar]
- 100.SAS Institute I. SAS 9.1. SAS Institute, Inc.; Cary, NC: 2002-2003. [Google Scholar]
- 101.SAS Institute I. JMP7.0. SAS Institute, Inc.; Cary, NC: 2007. [Google Scholar]
- 102.Levy JI, Baxter LK, Clougherty JE. The air quality impacts of road closures associated with the 2004 Democratic National Convention in Boston. Environ Health. 2006;5:16. doi: 10.1186/1476-069X-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Peterson EL, Ownby DR, Johnson CC. The relationship of housing and household characteristics to the indoor concentrations of Der f 1, Der p 1, and Fel d 1 measured in dust and air samples. Ann Allergy Asthma Immunol. 2003;90(5):564–71. doi: 10.1016/S1081-1206(10)61852-2. [DOI] [PubMed] [Google Scholar]
- 104.Bradman A, Chevrier J, Tager I, Lipsett M, Sedgwick J, Macher J, et al. Association of housing disrepair indicators with cockroach and rodent infestations in a cohort of pregnant Latina women and their children. Environ Health Perspect. 2005;113(12):1795–801. doi: 10.1289/ehp.7588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cohn RD, Arbes SJ, Jr., Yin M, Jaramillo R, Zeldin DC. National prevalence and exposure risk for mouse allergen in US households. J Allergy Clin Immunol. 2004;113(6):1167–71. doi: 10.1016/j.jaci.2003.12.592. [DOI] [PubMed] [Google Scholar]
- 106.NHLBI N, Heart, Lung, and Blood Institute Guidelines for the Diagnosis and Managment of Asthma, National Asthma Education and Preventon Program, Expert Panel Report 3. 2007 Summary Report 2007. [Google Scholar]
- 107.Boynton-Jarrett R, Ryan LM, Berkman LF, Wright RJ. Cumulative violence exposure and self-rated health: longitudinal study of adolescents in the United States. Pediatrics. 2008;122(5):961–70. doi: 10.1542/peds.2007-3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Clark C, Ryan L, Kawachi I, Canner MJ, Berkman L, Wright RJ. Witnessing community violence in residential neighborhoods: a mental health hazard for urban women. J Urban Health. 2008;85(1):22–38. doi: 10.1007/s11524-007-9229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Corburn J. Environmental justice, local knowledge, and risk: the discourse of a community-based cumulative exposure assessment. Environ Manage. 2002;29(4):451–66. doi: 10.1007/s00267-001-0013-3. [DOI] [PubMed] [Google Scholar]
- 110.Corburn J. Confronting the challenges in reconnecting urban planning and public health. Am J Public Health. 2004;94(4):541–6. doi: 10.2105/ajph.94.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Farhang L, Bhatia R, Scully CC, Corburn J, Gaydos M, Malekafzali S. Creating tools for healthy development: case study of San Francisco's Eastern Neighborhoods Community Health Impact Assessment. J Public Health Manag Pract. 2008;14(3):255–65. doi: 10.1097/01.PHH.0000316484.72759.7b. [DOI] [PubMed] [Google Scholar]
- 112.Bhatia R, Wernham A. Integrating human health into environmental impact assessment: an unrealized opportunity for environmental health and justice. Environ Health Perspect. 2008;116(8):991–1000. doi: 10.1289/ehp.11132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dannenberg AL, Bhatia R, Cole BL, Heaton SK, Feldman JD, Rutt CD. Use of health impact assessment in the U.S.: 27 case studies, 1999-2007. Am J Prev Med. 2008;34(3):241–56. doi: 10.1016/j.amepre.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 114.Wier M, Weintraub J, Humphreys EH, Seto E, Bhatia R. An area-level model of vehicle-pedestrian injury collisions with implications for land use and transportation planning. Accid Anal Prev. 2009;41(1):137–45. doi: 10.1016/j.aap.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 115.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–21. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Weisel CP. Assessing exposure to air toxics relative to asthma. Environ Health Perspect. 2002;110(Suppl 4):527–37. doi: 10.1289/ehp.02110s4527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Soliman AS, Jacko RB, Palmer GM. Development of an empirical model to estimate real-world fine particulate matter emission factors: the traffic air quality model. J Air Waste Manag Assoc. 2006;56(11):1540–9. doi: 10.1080/10473289.2006.10464566. [DOI] [PubMed] [Google Scholar]
- 118.Ozkaynak H, Palma T, Touma JS, Thurman J. Modeling population exposures to outdoor sources of hazardous air pollutants. J Expo Sci Environ Epidemiol. 2008;18(1):45–58. doi: 10.1038/sj.jes.7500612. [DOI] [PubMed] [Google Scholar]
- 119.Rosenlund M, Forastiere F, Stafoggia M, Porta D, Perucci M, Ranzi A, et al. Comparison of regression models with land-use and emissions data to predict the spatial distribution of traffic-related air pollution in Rome. J Expo Sci Environ Epidemiol. 2008;18(2):192–9. doi: 10.1038/sj.jes.7500571. [DOI] [PubMed] [Google Scholar]
- 120.New York City DoHPaD . HPD Online, HPD Online Glossary. New York City: 2008. [Google Scholar]
- 121.Elliott P, Wartenberg D. Spatial Epidemiology: Current Approaches and Future Challenges. Environ Health Perspect. 2004;112:998–1006. doi: 10.1289/ehp.6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Brady JE, Weitzman BC. Inconsistencies in place definition: How different operational place definitions affect estimates of adolescent smoking and drinking risk. Health Place. 2007;13(2):562–8. doi: 10.1016/j.healthplace.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 123.Fleischman AR, Barondess JA. Urban health: a look out our windows. Acad Med. 2004;79(12):1130–2. doi: 10.1097/00001888-200412000-00002. [DOI] [PubMed] [Google Scholar]
- 124.Vlahov D, Gibble E, Freudenberg N, Galea S. Cities and health: history, approaches, and key questions. Acad Med. 2004;79(12):1133–8. doi: 10.1097/00001888-200412000-00003. [DOI] [PubMed] [Google Scholar]
- 125.Galea S, Vlahov D. Urban health: evidence, challenges, and directions. Annu Rev Public Health. 2005;26:341–65. doi: 10.1146/annurev.publhealth.26.021304.144708. [DOI] [PubMed] [Google Scholar]