Abstract
Objectives
The antischistosomal properties of the marketed antiandrogens bicalutamide, flutamide, nilutamide and cyproterone acetate were studied both in vivo and in vitro.
Methods
Schistosoma mansoni-infected mice were treated orally with 50–400 mg/kg of the antiandrogens 3 and 7 weeks post-infection. In addition, three drug combinations of nilutamide and praziquantel (200/100, 100/100 and 100/50 mg/kg) were administered to mice harbouring adult S. mansoni. Drug effects were also monitored in vitro following exposure to antiandrogen concentrations of 1, 10 and 100 µg/mL.
Results
Low total worm burden reductions (5%–37%) and low to moderate female worm burden reductions (13%–75%) were achieved with the antiandrogens in the S. mansoni juvenile infection model. While flutamide and cyproterone acetate lacked activity against adult S. mansoni in vivo, low to moderate total and female worm burden reductions (0%–47%) were observed with bicalutamide. The highest total and female worm burden reductions (85% and 71%, respectively) (P < 0.001) were documented following a single 400 mg/kg dose of nilutamide. Statistically significant total (91%) and female (85%) worm burden reductions were achieved with the combination of nilutamide (200 mg/kg) and praziquantel (100 mg/kg). Schistosomes incubated with 100 µg/mL cyproterone acetate in vitro died after 15 h. Incubation with bicalutamide, nilutamide and flutamide at 100 µg/mL resulted in decreased movement of S. mansoni adults.
Conclusions
Our data indicate that the hydantoin derivative nilutamide has interesting antischistosomal properties, confirming previous results of schistosomicidal activities of this drug class.
Keywords: schistosomiasis, bicalutamide, nilutamide, flutamide, cyproterone acetate
Introduction
Schistosomiasis, caused by fluke worms of the genus Schistosoma, continues to be an important cause of parasitic morbidity and mortality, affecting >200 million individuals worldwide, with a further 579 million living at risk of infection.1 Even though praziquantel is an effective treatment for the chronic stage of infection, it only has moderate activity against juvenile schistosomes. In addition, drug resistance remains a concern; hence, the development of novel treatment options is desirable.2,3
The schistosomicidal activities of hydantoins, such as 5,5-diphenylhydantoin (phenytoin), were described in the early 1950s. However, these drugs lacked oral activity and multiple treatment courses were necessary in Schistosoma mansoni-infected mice.4 In the early 1980s, a series of 3-arylhydantoins were tested for their antischistosomal properties in the framework of the antischistosomal drug discovery programme carried out by Hoffmann–La Roche.5 Meta- and/or para-halogen-substituted 3-phenyl-5,5-dimethylhydantoins showed high antischistosomal activities. For example, administration of a single 38 mg/kg oral dose of 5,5-dimethyl-3-[4-fluoro-3-(trifluoromethyl)phenyl]-2,4-imidazolidinedione (Ro 13-3978) resulted in a worm burden reduction of 50% in mice harbouring adult S. mansoni.5
Nilutamide, a closely related 4-nitro-3-(trifluoromethyl)phenylhydantoin derivative, and the structurally related toluidides (flutamide and bicalutamide) are marketed antiandrogens useful for the treatment of metastatic prostate cancer. These drugs block the binding of testosterone and dihydrotestosterone at the androgen receptor.6
The aim of this study was to elucidate the antischistosomal properties of bicalutamide, flutamide and nilutamide in vitro and in mice harbouring juvenile and adult S. mansoni. Cyproterone acetate, a structurally unrelated steroidal antiandrogen, was included as a control.
Materials and methods
Drugs
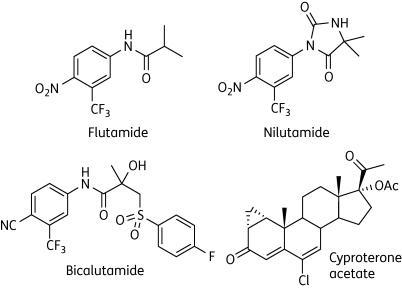
Bicalutamide, flutamide, nilutamide and cyproterone acetate (Figure 1) were purchased from Sigma–Aldrich. All drugs were suspended in 7% (v/v) Tween 80% and 3% (v/v) ethanol shortly before oral treatment of mice (10 mL/kg). For the in vitro studies, stock solutions of 10 mg/mL were prepared in DMSO (Fluka, Buchs, Switzerland).
Figure 1.
Chemical structures of flutamide, nilutamide, bicalutamide and cyproterone acetate.
Animals and parasites
In vivo studies were carried out in accordance with Swiss animal welfare regulations. This work was carried out under licences granted by the Cantonal Veterinary Office, Basel Stadt. Female mice (NMRI strain, n = 165, weight ∼20–22 g) were purchased from Harlan (Horst, The Netherlands), maintained under environmentally controlled conditions and acclimatized for 1 week before infection. Cercariae of S. mansoni were obtained from infected Biomphalaria glabrata maintained in our laboratories, as described previously.3
In vivo studies
Each mouse was infected subcutaneously with ∼80 S. mansoni cercariae. Twenty-one days (pre-patent infection) and 49 days (patent infection) after infection, groups of five mice were treated orally with the antiandrogens (single doses of 50–400 mg/kg). For the combination chemotherapy experiments, groups of mice were treated with praziquantel monotherapy (50 and 100 mg/kg) or combinations of nilutamide and praziquantel (200 mg/kg nilutamide plus 100 mg/kg praziquantel, 100 mg/kg nilutamide plus 100 mg/kg praziquantel and 100 mg/kg nilutamide plus 50 mg/kg praziquantel). Four groups of eight or nine untreated mice served as controls.
At 21 days post-treatment, animals were killed by the CO2 method, dissected and worms were sexed and counted, as described in previous publications.3
In vitro studies
Two male and two female schistosomes were placed in each well of a 48-well plate containing RPMI 1640 culture medium supplemented with 5% fetal calf serum, 100 U/mL penicillin and 100 µg/mL streptomycin. Concentrations of 100, 10 or 1 µg/mL of the drugs were added. Schistosomes incubated with 0.1% DMSO served as controls. Worms were kept in an incubator at 37°C and 5% CO2 for up to 66 h. Worm motility, phenotypic changes and death were recorded shortly after drug exposure and at 15, 22, 45 and 66 h post-incubation. Each assay was carried out in duplicate.
Statistical analysis
The Kruskal–Wallis (KW) test was used to compare the medians of the worm burdens in the treatment and control groups or in the monotherapy versus combination chemotherapy treatment groups (version 2.4.5 Statsdirect, Cheshire, UK). The significance level was P ≤ 0.05.
Results
In vitro findings
In the presence of antiandrogen concentrations of 1 and 10 µg/mL, no effect was observed on the viability and morphology of adult schistosomes.
Schistosomes incubated with 100 µg/mL cyproterone acetate died after 15 h. Incubation with 100 µg/mL bicalutamide, nilutamide and flutamide resulted in decreased movement of S. mansoni adults; however, schistosomes were still alive after 66 h and no morphological changes were observed.
Dose–response relationships of antiandrogens against juvenile S. mansoni
Total worm burden reductions of 5.1%–35.6% (P > 0.05) were achieved with nilutamide. The highest female worm burden reduction of 75.4% was observed with a 200 mg/kg dose of nilutamide, while moderate female worm burden reductions of 22.5%–27.5% were observed following 50, 100 and 400 mg/kg nilutamide doses. The female worm burden reductions in nilutamide-treated mice were statistically significant (KW = 4.15, P = 0.042). In contrast, flutamide effected only low total and female worm burden reductions of 3.7%–27.5% (P > 0.05). Similarly, administration of 100–400 mg/kg bicalutamide to mice infected with juvenile S. mansoni resulted in statistically insignificant total and female worm burden reductions of 17.3%–46.4%. A 400 mg/kg dose of cyproterone acetate achieved low, statistically insignificant, total and female worm burden reductions of 10.2% and 12.9%, respectively (Table 1).
Table 1.
Effect on worm burden of four antiandrogens administered as single oral doses ranging from 50 to 400 mg/kg to mice harbouring a 21- or 49-day-old S. mansoni infection
| Mean number of worms (SD) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Infection | Drug | Dose (mg/kg) (single) | total | females | Total worm burden reduction (%) | P value | Female worm burden reduction (%) | P value |
| — | Control 1 | — | 27.4 (10.9) | 13.8 (5.6) | — | — | — | — |
| Control 2 | — | 25.3 (9.5) | 12.0 (2.8) | — | — | — | — | |
| Control 3 | — | 27.0 (12.6) | 11.6 (7.4) | — | — | — | — | |
| Control 4 | — | 25.6 (5.0) | 12.4 (3.3) | — | — | — | — | |
| Juvenile infection | nilutamide | 50a | 24.4 (8.4) | 10.0 (3.3) | 11.0 | 0.189 | 27.5 | 0.042 |
| 100a | 26.0 (8.3) | 10.2 (3.8) | 5.1 | 26.1 | ||||
| 200a | 21.4 (5.1) | 3.4 (1.5) | 21.9 | 75.4 | ||||
| 400b | 16.3 (12.7) | 9.3 (6.7) | 35.6 | 22.5 | ||||
| flutamide | 50a | 25.8 (7.3) | 12.0 (4.1) | 5.8 | 0.324 | 13.1 | 0.151 | |
| 100a | 20.8 (11.1) | 10.0 (4.5) | 24.1 | 27.5 | ||||
| 200a | 26.4 (4.1) | 11.8 (3.6) | 3.7 | 14.5 | ||||
| bicalutamide | 100a | 17.4 (8.1) | 7.4 (3.6) | 36.5 | 0.022 | 46.4 | 0.092 | |
| 200c | 21.4 (12.4) | 9.6 (6.8) | 20.8 | 17.3 | ||||
| 400c | 18.6 (6.3) | 9.2 (3.9) | 31.1 | 36.2 | ||||
| cyproterone acetate | 400d | 23.0 (10.1) | 10.8 (4.6) | 10.2 | 0.502 | 12.9 | 0.543 | |
| Adult infection | nilutamide | 50a,e | 30.0 (6.1) | 12.8 (3.0) | 0 | 0.001 | 7.3 | 0.0007 |
| 100a | 19.0 (4.3) | 8.0 (2.3) | 30.7 | 42.0 | ||||
| 200a,f | 13.8 (4.5) | 7.0 (2.2) | 49.6 | 49.3 | ||||
| 400b,g | 5.5 (2.5) | 5.0 (2.4) | 84.8 | 71.3 | ||||
| flutamide | 50a | >27 | >14 | 0 | ND | 0 | ND | |
| 100a | >27 | >14 | 0 | 0 | ||||
| 200a,h | 31.7 (6.7) | 15.7 (3.2) | 0 | 0 | ||||
| bicalutamide | 100a | 30.8 (5.3) | 12.8 (3.8) | 0 | 0.148 | 7.2 | 0.131 | |
| 200c | 14.3 (8.0) | 7.5 (4.6) | 47.0 | 35.4 | ||||
| 400c,i | 16.0 (4.1) | 6.5 (1.3) | 40.8 | 44.0 | ||||
| cyproterone acetate | 400d | 32.2 (7.6) | 16.2 (3.7) | 0 | ND | 0 | ND | |
ND, not done.
aVersus Control 1.
bVersus Control 2.
cVersus Control 3.
dVersus Control 4.
eOne mouse died 20 days post-treatment.
fOne mouse died 3 days post-treatment.
gOne mouse died 1 day post-treatment.
hOne mouse died 14 days post-treatment.
iOne mouse died 6 days post-treatment.
Dose–response relationships of antiandrogens against adult S. mansoni
At 50 mg/kg, nilutamide showed no effect on adult schistosomes. Moderate worm burden reductions (30.7%–49.6%) were observed with doses of 100 and 200 mg/kg. At 400 mg/kg, nilutamide reduced total and female worm burdens by 84.8% and 71.3%, respectively. The total (KW = 6.78, P = 0.001) and female (KW = 11.38, P = 0.0007) worm burden reductions in the nilutamide-treated mice were statistically highly significant. No effects on female and total adult worm burdens were observed for flutamide at any dose tested. Bicalutamide at 100 mg/kg failed to show schistosomicidal activity, although higher doses of 200–400 mg/kg showed moderate (35.4%–47.0%) total and female worm burden reductions; however, these were not statistically significant. Cyproterone acetate given at 400 mg/kg had no effect on worm burden (Table 1).
Combinations of nilutamide plus praziquantel against adult S. mansoni in vivo
Low total worm burden reductions of 16.0% and 17.8% were achieved with praziquantel at 50 or 100 mg/kg, respectively. Combinations of nilutamide (100 mg/kg) and praziquantel (50 or 100 mg/kg) revealed an increase in worm survival, above the level observed with praziquantel or nilutamide monotherapy. However, a combination of nilutamide (200 mg/kg) and praziquantel (100 mg/kg) produced statistically significant total (90.6%; P = 0.013) and female (85.1%; P = 0.018) worm burden reductions (Table 2).
Table 2.
Effect on worm burden of praziquantel/nilutamide combinations given to mice harbouring a 49-day-old S. mansoni infection
| Mean number of worms (SD) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Treatment | Drug | Dose (mg/kg) (single) | total | females | Total worm burden reduction (%) | P value | Female worm burden reduction (%) | P value |
| — | Control 2 | — | 25.3 (9.5) | 12.0 (2.8) | — | — | — | — |
| Control 4 | — | 25.6 (5.0) | 12.4 (3.3) | — | — | — | — | |
| Monotherapy | praziquantel | 50a | 21.5 (10.5) | 11.5 (7.2) | 16.0 | 0.164 | 7.3 | 0.138 |
| praziquantel | 100a | 21.0 (9.5) | 9.5 (3.8) | 17.8 | 0.344 | 23.4 | 0.311 | |
| nilutamide | 100b | 19.0 (4.3) | 8.0 (2.3) | 30.7 | 0.06 | 42.0 | 0.027 | |
| nilutamide | 200b | 13.8 (4.5) | 7.0 (2.2) | 49.6 | 0.008 | 49.3 | 0.01 | |
| Combination chemotherapy | nilutamide plus praziquantel | 200/100c | 3.4 (3.2) | 2.6 (1.5) | 90.6 | 0.013 | 85.1 | 0.018 |
| 100/100d | 24.8 (10.0) | 13.0 (4.7) | 3.1 | 0.389 | 0 | ND | ||
| 100/50d | 22.6 (11.2) | 11.0 (4.3) | 11.7 | 0.753 | 11.3 | 0.293 | ||
ND, not done.
aVersus Control 4.
bVersus Control 2.
cVersus nilutamide 200 mg/kg.
dVersus nilutamide 100 mg/kg.
Discussion
Identification of marketed drugs as antischistosomals streamlines drug development, which can be accomplished with relative speed and economy.7
In this study, we examined the schistosomicidal activities of single oral doses of selective androgen receptor antagonists in mice, one steroid (cyproterone acetate) and three non-steroidal antiandrogens (bicalutamide, flutamide and nilutamide), marketed for the treatment of male hypogonadism, muscle wasting, anaemia, benign prostate hyperplasia and prostate cancer.6 Androgen receptor modulators are often associated with adverse events, such as hepatotoxicity, flushing and loss of libido or virilizing effects, since multiple doses for several months are necessary for treatment of these serious conditions.6,8 The rationale for selecting these compounds for testing against S. mansoni arose from the striking structural similarity of the hydantoins nilutamide and Ro 13-3978, the latter of which has potent antischistosomal activity in rodent models.5
A high total worm burden reduction (85%) was achieved with nilutamide at 400 mg/kg against adult S. mansoni, confirming the interesting antischistosomal properties of this structural class, in particular of the trifluoromethyl-substituted 3-arylhydantoins.5 However, the 4-nitro-3-(trifluoromethyl)phenyl-substituted nilutamide is much less effective than the 4-fluoro-3-(trifluoromethyl)phenyl-substituted Ro 13-3978, the latter of which has a reported ED50 of 38 mg/kg in the S. mansoni mouse model.5
Disappointingly, nilutamide achieved only low worm burden reductions against juvenile S. mansoni in vivo. High worm burden reductions observed against all development stages of schistosomes would be a valuable attribute of a new antischistosomal drug and an important differentiation from praziquantel. Praziquantel is characterized by only moderate activity against juvenile schistosomes, requiring frequent retreatment of patients to remove the schistosome burden of the continuously developing adult worms.2
Since drug combinations can enhance therapeutic effects and reduce adverse events, we studied nilutamide/praziquantel combinations. Simultaneous administration of nilutamide (200 mg/kg) and praziquantel (100 mg/kg) resulted in high worm burden reductions, suggesting an additive effect of the drugs. Interestingly, when the nilutamide dose was lowered further (100 mg/kg), a high worm survival, above the level seen with praziquantel and nilutamide monotherapy, was observed.
While cyproterone acetate and flutamide lacked activity in mice harbouring adult S. mansoni, moderate activities were observed with bicalutamide at doses of ≥200 mg/kg. Variations in the interaction with the androgen receptors might play a role in the difference in the antischistosomal activities observed among the four drugs tested. Indeed, cortisol and dehydroepiandrosterone have been reported to have a profound effect on the growth and survival of schistosomes, and hence the onset, establishment and pathogenesis of schistosomiasis.9 Classical nuclear receptors for steroids have been identified in schistosomes.9 The varying affinities of these drugs for androgen receptors in vitro and in vivo10 might also partially explain the differences in the antischistosomal properties observed in our in vitro and in vivo studies.
In conclusion, high in vivo schistosomicidal activity was observed for single oral doses of the marketed antiandrogen drug nilutamide. It would be worthwhile to investigate further analogues of this molecule that have been synthesized over the past years or that have even already emerged as leads, such as BMS564929.6
Funding
This work was supported by the Swiss National Science Foundation (project no. PPOOA-114941) and the U.S. National Institutes of Health (grant number R21AI076783).
Transparency declarations
None to declare.
Acknowledgements
We thank Yvette Endriss for maintenance of the S. mansoni life cycle and Dr Jacques Chollet for expert help with the S. mansoni mouse model.
References
- 1.Steinmann P, Keiser J, Bos R, et al. Schistosomiasis and water resources development: systematic review, meta-analysis, and estimates of people at risk. Lancet Infect Dis. 2006;6:411–25. doi: 10.1016/S1473-3099(06)70521-7. doi:10.1016/S1473-3099(06)70521-7. [DOI] [PubMed] [Google Scholar]
- 2.Caffrey CR, Williams DL, Todd MJ, et al. Chemotherapeutic development strategies for schistosomiasis. In: Selzer PM, editor. Antiparasitic and Antibacterial Drug Discovery. Weinheim: Wiley–Blackwell; 2009. pp. 301–21. [Google Scholar]
- 3.Keiser J. In vitro and in vivo trematode models for chemotherapeutic studies. Parasitology. 2010;137:589–603. doi: 10.1017/S0031182009991739. doi:10.1017/S0031182009991739. [DOI] [PubMed] [Google Scholar]
- 4.Luttermoser GW, Bond HW. Results of laboratory screening tests of compounds for possible schistosomicidal agents. I. Rhodanidines and hydantoins. J Parasitol. 1954;40:33. [Google Scholar]
- 5.Link H, Stohler HR. 3-Arylhydantoine, eine substanzklasse mit schistosomizider wirkung. Eur J Med Chem. 1984;19:261–5. [Google Scholar]
- 6.Gao W, Dalton JT. Expanding the therapeutic use of androgens via selective androgen receptor modulators (SARMs) Drug Discov Today. 2007;12:241–8. doi: 10.1016/j.drudis.2007.01.003. doi:10.1016/j.drudis.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nwaka S, Ramirez B, Brun R, et al. Advancing drug innovation for neglected diseases—criteria for lead progression. PLoS Negl Trop Dis. 2009;3:e440. doi: 10.1371/journal.pntd.0000440. doi:10.1371/journal.pntd.0000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahler C, Verhelst J, Denis L. Clinical pharmacokinetics of the antiandrogens and their efficacy in prostate cancer. Clin Pharmacokinet. 1998;34:405–17. doi: 10.2165/00003088-199834050-00005. doi:10.2165/00003088-199834050-00005. [DOI] [PubMed] [Google Scholar]
- 9.Escobedo G, Roberts CW, Carrero JC, et al. Parasite regulation by host hormones: an old mechanism of host exploitation? Trends Parasitol. 2005;21:588–93. doi: 10.1016/j.pt.2005.09.013. doi:10.1016/j.pt.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Migliari R, Muscas G, Murru M, et al. Antiandrogens: a summary review of pharmacodynamic properties and tolerability in prostate cancer therapy. Arch Ital Urol Androl. 1999;71:293–302. [PubMed] [Google Scholar]